Neurosurgery is a highly competitive residency, with few positions available to many applicants.Reference Lubelski, Healy, Friedman, Ferraris, Benzel and Schlenk 1 Despite the nearly universal high motivation, impressive academic record, and good medical school ranking of accepted trainees, programs have historically been plagued with a 43% attrition rate.Reference Cusimano, Yonke and Tucker 2 , Reference Nadeem, Effendi and Hammad Ather 3 Among the potential risk factors identified were dissatisfaction with lifestyle,Reference Cusimano, Yonke and Tucker 2 female gender,Reference Lynch, Nieto and Puthenveettil 4 and attitude of senior residents and staff.Reference Nadeem, Effendi and Hammad Ather 3 As admissions in Canadian programs were increased to compensate an anticipated shortage in the workforce,Reference Hugenholtz 5 neurosurgery itself became much more subspecialized,Reference Toyota 6 challenging the adequacy of surgical exposure for each trainee.Reference Haji and Steven 7 In the end, workforce shortage never materialized and, combined with the decision of the American Board of Neurological Surgeons to stop recognizing Canadian residency training, graduates recently found themselves worrying about unemployment.Reference Kondro 8 , Reference Woodrow, O’Kelly, Hamstra and Wallace 9
Neurosurgery residents therefore face a unique combination of challenges including a high-workload, high-stakes specialty following a 6-year long residency with uncertain employment prospects. To identify characteristics of such individuals, we performed a cross-sectional survey of Canadian neurosurgery residents and fellows assessing three domains: demographics, interests and career goals, as well as happiness and well-being.
Methods
Study Population
All neurosurgery residents or fellows enrolled in a Canadian postgraduate program as of April 1, 2016, were eligible for participation. Residents who had been accepted at but had not yet started their neurosurgical residency program were excluded from the study. Potential respondents were identified through the Canadian Neurosurgery Research Collaborative (CNRC), which includes a local resident representative at 12 of the 14 neurosurgery programs in Canada.Reference Dakson, Tso and Ahmed 10 Potential respondents from the remaining institutions were reached through a contact with one of the institution’s residents. The study took the form of an online survey to be completed at the participant’s convenience within 8 weeks of study start.
Survey Development
A 40-question online survey was developed by the first author. The survey specifically explored three domains: (1) demographics, (2) interests and career goals, and (3) happiness and well-being. A meeting of the CNRC members was held to assess face and content validity. The survey was improved and the final version approved by all authors. The distributed survey is available as Supplementary Material 1.
Most questions consisted of either multiple choice questions or five-level Likert scales. Overall quality of life and satisfaction with choice of specialty and work-life balanced were specifically assessed in this way to match reports from other specialties.Reference Linn, Yager, Cope and Leake 11 - Reference Pulcrano, Evans and Sosin 15 Responses to Likert questions were condensed to three levels for the analysis (i.e. “strongly agree” and “agree” grouped together and “strongly disagree” and “disagree” grouped together).
Survey Administration
All Canadian residents and fellows received an invitation to participate in the study and a link to the survey website. A general e-mail reminder was sent after 2 and 4 weeks. After 6 weeks, nonrespondents were contacted directly by their local CNRC representative to encourage participation. Response collection was stopped after 8 weeks.
Statistical Analysis
As per the guidelines of the American Association for Public Opinion Research, surveys were considered completed if more than 80% of the questions were answered. 16 Only completed surveys were included in the analysis.
Survey answers are presented using frequency tables with the number of respondents to each answer and valid percentages. Continuous variables are reported using the median and range. The independence of categorical variables was assessed using the chi-square test. All statistical analyses were performed in IBM SPSS Statistics, version 24.0.0.0 (IBM, Armonk, NY). Figures were produced using Prism 6.0 (GraphPad Software Inc., La Jolla, CA) and Adobe Illustrator CS6, version 16.0.4 (Adobe Systems, San Jose, CA).
Ethics, Consent, and Permissions
This study was approved by the Research Ethics Board of the Centre Hospitalier Universitaire de Sherbrooke and by the CNRC steering committee. Consent to publish anonymized, aggregated data was obtained as part of the general consent for study participation.
Results
Survey Response Rate
A total of 146 residents and 25 fellows were identified as potentially eligible for study participation by CNRC representatives. We received surveys from 77 (53%) residents and four (16%) fellows. Given the poor response rate among fellows, we decided to exclude them from the analysis and focus exclusively on residents. One resident survey was incomplete and was excluded (Figure 1), leading to a final analysis of 76 completed resident surveys (52% response rate). Response rate varied between programs, ranging from 0% to 83%. All provinces and residency training levels were proportionally represented.
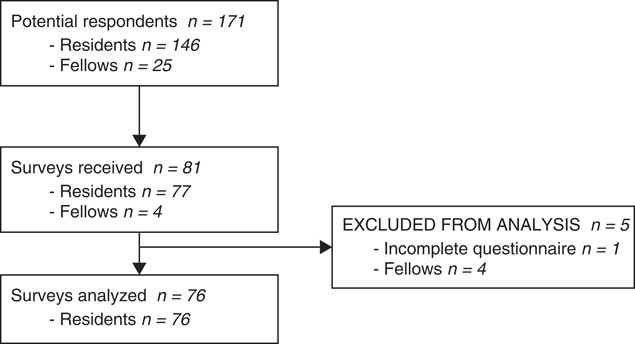
Figure 1 Flow diagram of survey respondents.
Demographics
The demographics of respondents are presented in Table 1. Briefly, 75% were male, 38% were married, and 71% had no children. The median age was 29 years. During their respective Canadian Resident Matching Service application, neurosurgery was the first choice of specialty for 96% of respondents, and 75% were matched to their first-ranked neurosurgical program (Table 2). Most respondents had some research experience before beginning residency, but their prior research exposure was not associated with a higher chance of matching in their first choice of program (73.4% vs 87.5% for residents with or without prior research experience, respectively; Pearson chi-square (3)=.911, p=0.823).
Table 1 Demographics of survey respondents (Canadian neurosurgery residents and fellows)
PGY=postgraduate year.
Table 2 Residency matching statistics
CaRMS=Canadian Resident Matching Service.
Interests and Career Planning
Following residency training, 86% indicated that they plan to complete a fellowship (Table 3), with the most popular subspecialties being spine, oncology, and open vascular neurosurgery (Figure 2). The United States was the most popular anticipated site for fellowship training. Seventy-five percent of respondents stated they plan to incorporate research as part of their practice, with 57% planning to pursue advanced research training (masters of science or doctorate) during residency. The majority of respondents (80%) would endeavor to practice in an academic institution, with 59% ideally practicing in Canada. Twenty-five percent were unsure in which country they would like to practice and only 37% felt confident in finding a job. Interestingly, a nonstatistically significant trend was observed in which pursing an additional research degree was associated with a lack of confidence in finding a job (28% vs 52% feeling confident among the respondents planning vs not planning an additional degree, Pearson chi-square (2)=5.843, p=0.054).
Table 3 Career planning
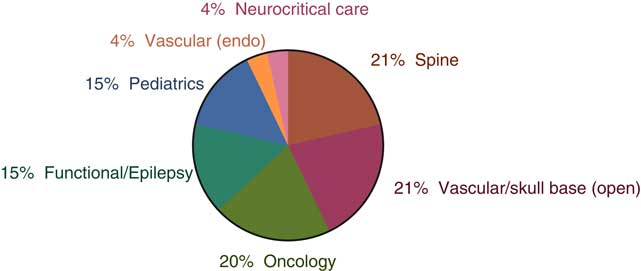
Figure 2 First choice of fellowship.
Workload
The most frequent self-reported number of worked hours per week (including calls) was the 80- to 89-hour range, with 21% stating they typically worked more than100 hours per week (Figure 3). This workload was deemed reasonable by 58% and too much by 41% of respondents. The median number of days on call per month was 7 (range, 0-12), with most feeling this number was reasonable (66%) or too high (34%).
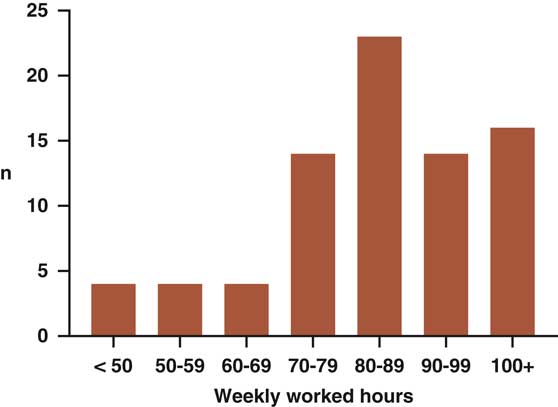
Figure 3 Self-reported worked hours in a typical week (including calls).
Happiness and Well-Being
Happiness and well-being measures are presented in Table 4. Overall, the majority of respondents reported both a high level of happiness as well as stress. Sense of accomplishment and fatigue were reported as average to high. Overall quality of life was low for 18%, average for 49%, and high for 33%. Satisfaction with work-life balance was average for 46% of respondents and was the only tested domain in which significant dissatisfaction was identified (17%). Overall, respondents were highly satisfied with their choice of specialty, choice of program, surgical exposure, and work ambiance.
Table 4 Wellbeing, quality of life, and satisfaction with residency
Of note, 35% of respondents reported having been victim of intimidation during residency. Depression was experienced by 17%, and 4% considered suicide. Intimidation was statistically significantly associated with depression (Pearson chi-square (4)=19.107, p=0.001).
Discussion
Demographics and Career Planning
The demographics of Canadian neurosurgery residents was remarkably similar to that of their AmericanReference Fargen, Dow, Tomei and Friedman 17 and EuropeanReference Stienen, Netuka and Demetriades 18 colleagues, with an average age of 30 years, the majority being male (75% of Canadians vs 79% of Americans vs 76% or Europeans), married (38% of Canadians vs 51% of Americans), and without children (71% of Canadians vs 68% of Americans). The interest in subspecialty training was significant and appears grossly proportional to the current Canadian staff positions, with spine, oncology, and vascular being the most represented. This contrasts with a survey conducted in 1996 in which the majority of practicing neurosurgeon worked as general neurosurgeons in academic centersReference Hugenholtz 5 and further confirms the trend toward a subspecialization within the field.Reference Toyota 6
Workload
With regard to work hours, 69% of Canadian residents reported working more than 80 hours/week, compared with 6% of Europeans,Reference Stienen, Netuka and Demetriades 19 in whom the European Working Time Directive 2003/88/EC theoretically limits work hours to 48 per week. Recent data were not available for the American programs, although a survey performed 1 year after the 2011 introduction of American work hour restrictions reported that 36% of neurosurgery residents violated the 80-hour regulation on an occasional or regular basis.Reference Fargen, Dow, Tomei and Friedman 17
The issue of work hour regulation is controversial. Proponents argue that an excessive workload negatively affects residents’ physical and mental health and are associated with increased complications and unfavorable patient outcomes.Reference Landrigan, Rothschild and Cronin 20 - Reference Weinger and Ancoli-Israel 22 Opponents stress that imposing work hour restrictions impedes continuity of care by increasing the number of caregivers, limits surgical exposure, and decreases resident performance with a detrimental effect on patient safety and resident employability.Reference Schaller 23 , Reference Stienen, Netuka and Demetriades 24
In our survey, although the majority of respondents felt that their workload was reasonable, a significant proportion of respondents (42.5%) disagreed. Work-life balance was the only consistent source of dissatisfaction (17% of respondents) among our cohort, with a rate comparable to that reported for practicing US neurosurgeons (14%).Reference Klimo, DeCuypere, Ragel, McCartney, Couldwell and Boop 25 Although less dramatic than the 32% and 38.9% reported for American and Canadian general surgery residents, respectively,Reference Antiel, Reed and Van Arendonk 26 , Reference Ginther, Dattani, Miller and Hayes 27 dissatisfaction with work-life balance was higher than the 8.8% national average for residents across specialties. 28 This phenomenon is not new. Indeed, an analysis of attrition in Canadian neurosurgery residency programs revealed a total attrition rate of 42.6% in the years 1980 through 1992, with 65% of the affected residents voluntarily withdrawing from training mostly for lifestyle reasons.Reference Cusimano, Yonke and Tucker 2 Moreover, a 2015 survey reported a 56% rate of burnout among American practicing neurosurgeons.Reference McAbee, Ragel and McCartney 29 Although data for neurosurgery residents are not available, a rate of 51.5% was reported for American internal medicine residents in 2011Reference West, Shanafelt and Kolars 14 and 58% for general surgery residents in 2004.Reference Ishak, Lederer and Mandili 30 Burnout was not directly assessed in our survey, although no respondent reported extending his or her residency for health reasons. It would be surprising, however, that burnout was nonexistent in neurosurgery, and this may reflect a response bias to the survey. We did, however, collect anecdotal evidence that research rotations are sometimes used to give residents “a break” from the workload of on-service rotations. Strategically placed research could perhaps represent a coping mechanism in the face of a demanding residency while also fulfilling academic objectives.
Satisfaction and Quality of Life
Respondent’s satisfaction with their program (88%) was higher than the 2013 national Canadian average across specialties (62%). 28 Neurosurgery residents’ satisfaction in their choice of specialty (92%) was comparable to rates reported for practicing American neurosurgeons (95%)Reference Klimo, DeCuypere, Ragel, McCartney, Couldwell and Boop 25 and substantially higher than orthopedic residents (69%) and most surveys of attending surgeons from other surgical specialties including ear, nose, throat (ENT) (74%); obstetrics and gynecology (76%-89%); plastics (67%-80%); and vascular (36%).Reference Pulcrano, Evans and Sosin 15 This might be related to a higher sense of accomplishment amongst neurosurgery residents. Indeed, only 8% of our respondents reported having a low sense of accomplishment relative to 13% to 40% of obstetrics and gynecology residents and 21% to 55% of ENT residents.Reference Pulcrano, Evans and Sosin 15
Quality of life was reported as low by 18% of respondents. This was similar to general surgery residents’ 18%Reference Antiel, Reed and Van Arendonk 26 and ENT surgeons’ 20.9%Reference Balch, Shanafelt, Sloan, Satele and Freischlag 31 and higher than internal medicine residents’ 14.5%.Reference West, Shanafelt and Kolars 14 Yet, only 4% of respondents reported being unhappy. This discrepancy between quality of life and happiness might seem contradictory. We believe it reflects the temporary nature of residency in which quality of life is sacrificed until training is complete, competency is demonstrated, and a job is found. This overarching goal likely sustains happiness despite challenging circumstances.Reference Davenport, Henderson, Hogan, Mentzer and Zwischenberger 32
Intimidation
Intimidation is a longstanding problem in residency training and workplace environment in general. A recent literature review reported that 45% to 93% of residents experienced some form of inappropriate behavior during trainingReference Karim and Duchcherer 33 ; “intimidation or bullying,” when specifically named as such, was reported by 30.8% of Canadian residents across specialties in 2013. 28 A total of 44.7% of family medicine residents who graduated between 2001 and 2005 from two Canadian programs reported having experienced intimidation or harassment during residency training,Reference Crutcher, Szafran, Woloschuk, Chatur and Hansen 34 and such behavior was reported by 16.7% of Canadian general surgery residents as a reason for considering leaving training.Reference Ginther, Dattani, Miller and Hayes 27 With a rate of 35% in our survey, neurosurgical programs are clearly affected by this problem as well. The well-known association between intimidation and depression is further confirmed by our data and highlights the importance of proactively fighting this problem.
Limitations
With a 52% response rate, our survey captured a sizeable sample of Canadian neurosurgery residents, and respondents were evenly distributed throughout training levels and provinces.
As an e-mail survey, our results do remain vulnerable to voluntary response bias. If, for example, residents with more time and energy proved more susceptible to answer, results could be skewed toward optimism. Concerns regarding respondents’ anonymity could have further exacerbated this phenomenon because residents may have feared identification in small training programs with only one resident per year. Although participants were assured that only anonymous, aggregated data would be published, personal questions such as satisfaction with the program, intimidation, depression, and suicide could have acted as deterrents. On the other hand, the opposite could also be true and dissatisfaction might have motivated some residents to complete the survey.
Conclusions
The average, prototypical neurosurgery resident is a 29-year-old single male with an interest in research. He works 80 to 89 hours per week with 7 nights on call per month, which he finds reasonable. Although he reports having a high level of stress and fatigue because of the high workload, he is generally happy and feels rewarded for his work. He is highly satisfied with his choice of specialty and considers a fellowship in spine, oncology, or open vascular surgery. He remains uncertain about his future employability.
Acknowledgments
This study was made possible by the joint efforts of the Canadian Neurosurgery Research Collaborative (CNRC) steering committee members.
Disclosures
All authors declare having no conflict of interest.
Statement of Authorship
All authors contributed to the study design and implementation. CI-M collected the results, performed the statistical analysis, and drafted the manuscript. All authors critically revised the manuscript and approved the final version.
Supplementary Material
To view the supplementary material for this article, please visit https://doi.org/10.1017/cjn.2017.263.









