A 45-year-old Caucasian man with X-linked hypophosphataemic rickets (XLHR), and no other risk factors for ossification of the posterior longitudinal ligament (OPLL), presented with a 3-week history of progressive right hand and leg weakness. This was noticed when weight-bearing, 5 weeks after a right total knee replacement. Examination revealed right upper limb and right lower limb weakness and bilateral lower limb spasticity with extensor plantar responses, compatible with a cervical myelopathy. CT cervical spine revealed coarse calcification of the posterior longitudinal ligaments (PLL), from C4 to C7, and of the ligamentum flavum (LF), from T3 to T4, causing severe central canal stenosis (Figure 1). MRI spine showed extensive abnormal ossification of the PLL at C2-C6, and confirmed compressive myelopathy of the cervical cord, with spinal cord oedema at this level (Figure 2). The patient declined surgery (Figure 2).
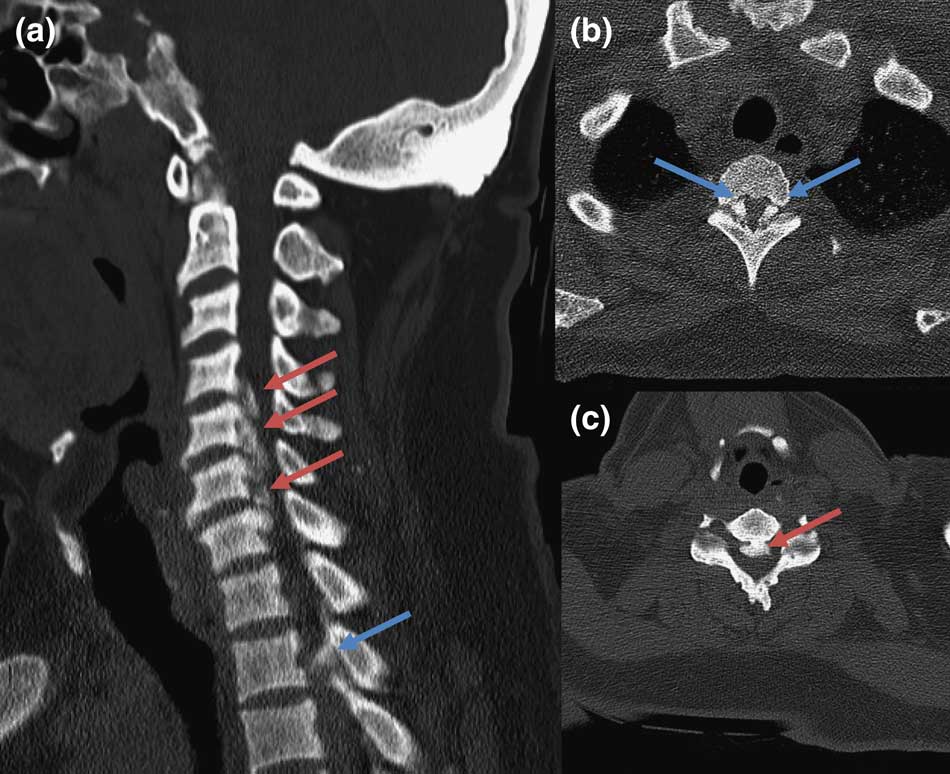
Figure 1 CT cervical spine, sagittal (A) and axial (B, C): marked ossification of posterior longitudinal ligament (red arrows) and ligamentum flavum (blue arrows), causing severe central canal stenosis.
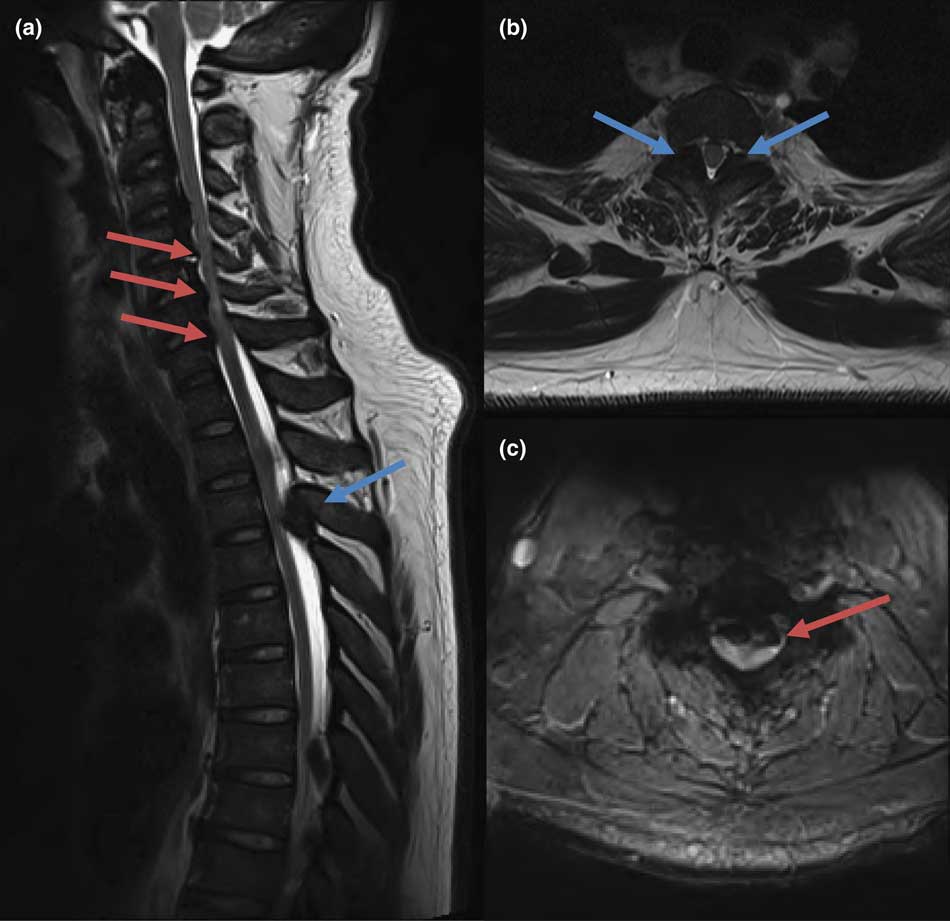
Figure 2 T2-weighted MRI spine, sagittal (A) and axial (B, C): diffuse hypointense bone marrow signal abnormality (also shown on T1 sequence; likely a treatment effect), mass-like T2-hypointensities within posterior longitudinal ligament at C4-C7 (red arrows), which causes cord oedema at these levels; focal and expanded T2-hypointensities in ligamentum flavum at T3-T4 and T7-T8 (blue arrows).
X-linked hypophosphataemic rickets is a common genetic cause of hypophosphataemia due to mutations in the PHEX gene (Phosphate-regulating gene with Homologies to Endopeptidases on the X-chromosome). Affected individuals have a short stature that is usually limited to the lower extremities, with associated leg bowing. It is rarely a cause of spinal cord compression. Neuroradiological findings in XLHR reported in the literature include thickening of the vertebral laminae, facet joint hypertrophy, and ossification of the intervertebral discs, PLL, and/or LF.Reference Soehle and Casey 1
Ossification of the posterior longitudinal ligament is rare in Caucasians (0.16%) compared with Asian populations (2.4%).Reference Choi, Song and Chang 2 CT of the spine is the imaging modality of choice for detecting ossification of the PLL and LF. A recent case study showed evidence for the use of three-dimensional CT to be superior than lateral radiographic approaches in detecting small calcifications.Reference Izumi, Hirano and Watanabe 3 Ossified lesions in MRI are hypointense on T1-weighted and T2-weighted images, which can be difficult to distinguish from the adjacent soft tissues and ligaments. MRI is generally superior to CT in detecting soft tissue abnormalities, such as concurrent disc protrusions and resultant spinal cord compression (as in this case).Reference Tan, Siew and Wong 4 Radiographic predictors for the development of myelopathy in patients with OPLL include >60% spinal canal stenosis; large range of motion of the cervical spine; and lateral deviated-type OPLL.Reference Matsunaga, Nakamura and Seichi 5 It is important to consider compressive myelopathy in patients with XLHR. We demonstrate the classical findings of ossification of the PLL and LF, leading to spinal cord compression.
Disclosures
CF, AA, SAR, SJF, and SL do not have anything to disclose.
Statement of Authorship
CF prepared the first draft of the manuscript and helped with the corrections. AA, SAR, and SJF reviewed the manuscript and helped with the corrections. SL reviewed the manuscript, and was involved in corrections, image selection, and description.




