Introduction
Falling is a major problem in today’s society leading to injuries and secondary morbidities. Reference Do, Chang, Kuran and Thompson1 Independent of acute illnesses causing dizziness and neurological disorders characterized by imbalance, many other physical factors contribute to falling. Reference Do, Chang, Kuran and Thompson1–Reference Kenny, Rubenstein and Tinetti3 Fall risk assessment includes comprehensive neurological examination focusing on balance and gait, lower limb strength, tone, sensation and coordination, and cognition. Reference Thurman, Stevens and Rao2 Not infrequently, patients present with symptoms of dizziness and imbalance, but without evidence of pathology related to these typical fall-risk factors. Instead, they exhibit static axial deformities which can also cause imbalance, Reference Gauchard, Lascombes, Kuhnast and Perrin4–Reference Hayashi, Aizawa, Nagase and Ohara6 or suffer acute neck pain which causes imbalance through disruption of cervical proprioceptive signals. Reference Karlberg, Johansson, Magnusson and Fransson7–Reference Uthaikhup, Jull, Sugnkarat and Treleaven9
In order to maintain balance and successfully navigate our environment, we must be able to accurately assess the speed, accuracy, and trajectory of our own movements through space (self-motion), identify targets of interest and avoid obstacles through tight coordination of visual, vestibular, and neck proprioceptive signals. The vestibulo-ocular reflex (VOR) stabilizes gaze by producing eye movements equal in amplitude and velocity, and opposite in direction to head movements. When undertaking gaze redirection, the vestibular system incorporates inputs from neck proprioceptors to suppress the VOR, allowing the eyes to rotate in the same direction as the head, enhancing gaze and postural stability. Reference Cullen10 Chronic cervical immobility prolongs VOR suppression during combined eye–head movements because coactivation of cervical muscles causes non-veridical sensory signals from neck proprioceptors. This in turn causes diminished gaze accuracy, Reference Johnston, Daye and Thomson11 potentially impairing navigation through complex visual environments where it is essential to accurately redirect gaze to novel targets. We determined these abnormalities of saccade metrics and VOR suppression to be consistent and robust findings in patients with chronically restricted cervical mobility. We hypothesized that these abnormalities would lead to imbalance and falls in this cohort of patients, who do not otherwise have quantitative evidence of vestibulopathy. Reference Johnston, Daye and Thomson11
To date, there has been little written about fall risk in those with chronically restricted neck mobility. Gabell et al. Reference Gabell, Simons and Nayak12 examined 100 individuals aged 65–85 years and found that restricted neck movements increased the probability of falling twofold. They did not examine coexistent neck pain or define neck motion restriction either in amplitude or in rotational plane. Accordingly, we sought to determine if chronically restricted cervical motion is associated with increased fall frequency or fear of falling. Likewise, we examined the contribution of abnormal cervicothoracic spinal morphology in fall causality and whether these static and dynamic axial abnormalities contribute differentially to falls, depending on age.
Methods
In order to fully evaluate upper body musculoskeletal complaints and potential relationships to fall risk, we examined 435 patients presenting with soft tissue musculoskeletal complaints to a tertiary rheumatology clinic over a 3-year period between July 2012 and July 2015 with the approval of the CIADS Research Institutional Review Board in compliance with the Declaration of Helsinki and after obtaining informed written consent. Patients with work-related injuries or Worker’s Compensation Board claims were excluded as were individuals with trauma from motor vehicle or other accidents. Individuals meeting criteria for fibromyalgia were excluded. Other exclusions included those with prominent lower limb weakness and pain, significant peripheral sensorimotor neuropathies, or decreased range of motion in the hips, knees, ankles, and feet, which produced antalgic gait. No patient had clinical, serological, or radiological evidence of inflammatory arthritis or connective tissue disorders, both of which may be associated with increased fall risk. Reference Stanmore, Oldham, Skelton, O’Neill, Pilling and Campbell13,Reference Alkan Melikoğlu and Bağcıer14 Patients with stroke, Parkinson’s disease, ataxia, or cognitive impairment were also excluded. Fifteen patients were excluded because of past or current history of vertigo. In total, 376 patients met the criteria and completed the Falls Efficacy Scale-International (FES-I) 16-item balance questionnaire. The FES-I questionnaire provides a validated, quantitative measure of fear of falling. Reference Yardley, Beyer, Hauer, Kempen, Piot-Ziegler and Todd15 It assesses concerns about falling during simple and challenging physical tasks. Reference Delbaere, Close, Mikolaizak, Sachdev, Brodaty and Lord16 Individuals with both past history of falling and those at greater fall risk have higher scores, indicating heightened fear of falling (low concern: 16–22/64; high concern: 23–64/64). Reference Delbaere, Close, Mikolaizak, Sachdev, Brodaty and Lord16
Symptoms of cervical mobility restriction and thoracic kyphoscoliosis consisted of chronic neck, shoulder, upper back, and forearm discomfort. Pain at end range of motion is frequently associated with restriction of range of motion in these regions and discomfort in shoulders and forearms is referred from cervical and upper thoracic spine. Reference Bland17 Duration was based on when the patient first recalled experiencing musculoskeletal pain or restriction of motion. Each patient was systematically examined for evidence of visual impairment (reduced vision or diplopia), peripheral neuropathy, foot pain, and lower limb osteoarthritis or joint replacement. Patients were segregated by fall frequency in the prior year (no falls, one fall, two or more falls) and by age (less than 65 years or 65 years and older).
Anatomical Measurements
Static Measurements
Cervical tilt was defined as static lateral inclination of head and neck in roll measured by goniometer. Thoracic scoliosis was measured using a scoliometer (Orthopedic Systems, Inc., Union City, CA, USA). High scoliosis was defined as cervicothoracic scoliosis with the apex of the curve rostral to T4; mid-thoracic scoliosis apex between T4 and T9 and low thoracic scoliosis apex between T9 and T12. Complex scoliosis was any scoliosis with at least two thoracic curves of opposite orientation. Kyphosis was excessive posterior curvature of the thoracic spine and was either present or absent. Reference Bland17
Kinetic Measurements (Figure 1)
All head and neck rotations were active and measured by goniometer. Measurements for sagittal movements around the interaural X axis were made from a vertical reference line between vertex and sternal notch (Y axis) (Figure 1A). Head and neck extension were attempted nose-up postures. Measurements were negative if the active range of motion of head and neck was posterior to the Y axis and positive if head and neck could not extend back beyond the Y axis. Flexion was forward, nose-down rotation of head and neck from the Y axis. Total range of motion in pitch was calculated as range of flexion minus range of extension. Full head and neck lateral flexion was total rotation around the naso-occipital Z axis in roll, from right ear down to left ear down position (Figure 1B). Horizontal neck rotation in yaw was measured as left and right rotations around the Y axis with full horizontal neck rotation as their sum (Figure 1C).
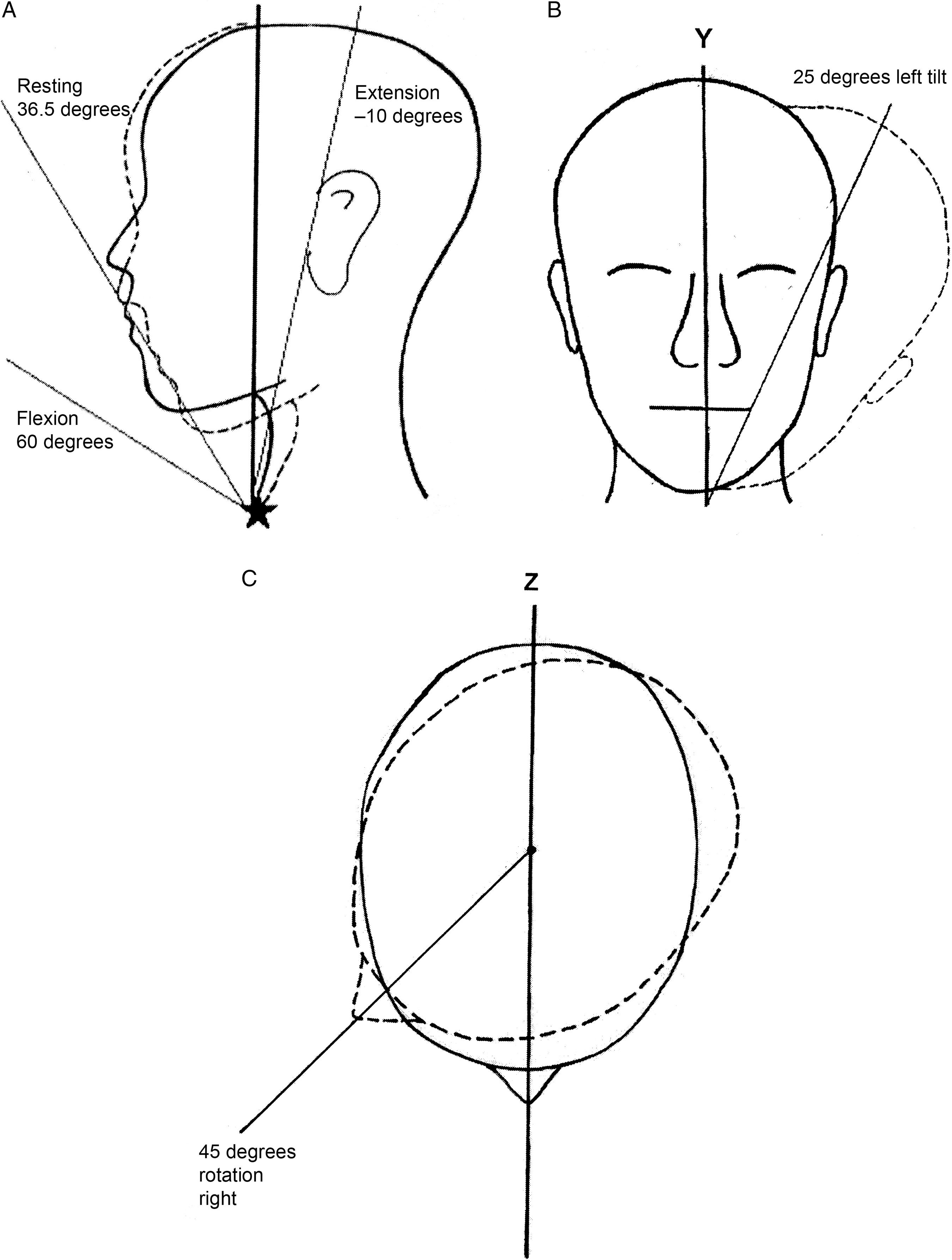
Figure 1: Measurements of Head and Neck Mobility. (A) Pitch: Measurements for head and neck movements in pitch were made from a vertical reference line between the vertex and the sternal notch (star). Resting postures (dashed outline) were typically forward flexion (36.5 degrees; SD 5.1) and did not vary between groups or with age. Extension measurements were negative if the active range of motion of the head and neck was posterior to the vertical reference line (−10 degrees in this example). Flexion was active forward rotation of the head and neck from the vertical reference line (measuring 60 degrees in this diagram). Total active range of motion in pitch was calculated as flexion minus extension. In this example, total active pitch rotation is 70 degrees [60 degrees – (−10 degrees)]. (B) Lateral Flexion: Full head and neck lateral flexion was total rotation around the naso-occipital Z axis in roll, from right ear down to left ear down position. In this example, head and neck lateral flexion to the left measures 25 degrees. (C) Horizontal Rotation: Horizontal neck rotation in yaw was measured as left and right rotations around the Y axis with full horizontal neck rotation as their sum. In this example, head and neck horizontal rotation measures 45 degrees to the right.
Statistical Analysis
Analysis of variance (ANOVA)/chi-square test for trend was used to examine for differences in continous/categorical data between nonfallers, patients who had fallen once, and those who had fallen twice or more (multiple fallers). Student’s t-test/ Pearson chi-square test was used to compare differences between continuous/categorical risk factors for nonfallers compared to all fallers (single + multiple fallers) and between younger and older nonfallers and fallers. Odds ratios (OR) for fall risk factors were calculated using binary logistic regression [Exp (B)] with any fall event as the outcome. Normative data was based on the lower 95% CI of the mean of total neck rotation (85.9 degrees) and total pitch (66.6 degrees) for fallers as a group.
Hierarchical multiple regression assessed the ability of anatomical factors to predict FES-I scores in fallers. Least absolute shrinkage and selection operator (forward criterion: probability of F to enter ≤ 0.05) was used to determine which of the other variables known to contribute to increased fall risk were relevant; these included age, impaired vision, number of psychotropic medications, total number of medications, lower limb osteoarthritis and joint replacement, peripheral neuropathy, foot pain, fatigue, and other comorbidities. Of these, age, pain, number of psychotropic medications, peripheral neuropathy, and fatigue were significant independent contributors to FES-I scores, depending on the age of the group being analyzed. Preliminary analyses did not show any violations of normality, linearity, multicollinearity (VIF > 10), and homoscedasticity.
Partial correlation assessed any relationship between duration of symptoms and kinetic and static axial measurements and between duration of symptoms and FES-I scores, for both young and older fallers, controlling for age. For all statistical analyses, a two-sided value of p ≤ 0.05 was considered significant. Statistical analysis was performed with IBM SPSS, version 25. SQUIRE reporting guidelines were utilized in the preparation of this manuscript. Reference Ogrinc, Davies, Goodman, Batalden, Davidoff and Stevens18
Results
Subject Characteristics (Table 1)
Of the 376 patients, 254 did not suffer any falls over the year prior to assessment. In total, 61 patients fell once and a further 61 patients suffered multiple falls. There was no significant difference between mean ages for nonfallers compared to fallers, and age did not confer additional risk of falling (OR 1.00; 95% CI 0.99–1.02; p = 0.888). There was a female predominance of 2.4:1 in the group as a whole, and 4.1:1 among multiple fallers, but no gender effect was detected with respect to fall risk (OR 1.40; 95% CI 0.87–2.25; p = 0.168).
Table 1: Subject Characteristics

* Student’s t-test; † Chi square/Chi square for trend; ‡ ANOVA
The occurrence of symptoms of neck and upper back pain and stiffness due to cervical mobility restrictions and thoracic kyphoscoliosis was significantly greater for fallers compared to their nonfalling counterparts. The presence of symptoms more than doubled the risk of falling (OR 2.34; 95% CI 1.39–3.93; p = 0.001). Fallers had significantly longer mean symptom durations than nonfallers.
FES-I questionnaire scores were significantly greater in fallers compared to nonfallers for the group of fallers as a whole and for younger fallers. There was no significant difference in FES-I questionnaire scores between older nonfallers and older fallers. Mean FES-I scores for younger fallers and both older nonfallers and fallers showed high concern regarding fall risk (>23). Younger nonfallers had mean FES-I scores which showed low concern regarding the risk of falling (<23).
Other Fall Risk Factors (Table 2)
Among other fall risk factors, psychotropic drug use was significantly greater in fallers for the group as a whole (p = 0.023) and in both younger (p = 0.007) and older (p = 0.003) fallers compared to their nonfalling counterparts. For the group as a whole, the presence of fatigue and mild peripheral neuropathy was no greater among fallers than nonfallers, but for younger fallers, fatigue (p = 0.038) and peripheral neuropathy (p = 0.050) were greater than in younger nonfallers. Lower limb joint replacements were more common among fallers, but this was strictly a function of younger fallers (p = 0.028). Similarly, significant increases in total medication numbers and visual impairments in all fallers were due entirely to older fallers. Older fallers also had greater numbers of comorbidities (p = 0.020) than older nonfallers. Otherwise, for the group as a whole, the number of comorbidities, presence of lower limb osteoarthritis, and foot pain were no greater in fallers than in nonfallers.
Table 2: Other fall risk factors

* Student’s t-test.
† Chi square.
Anatomical Risk Factors (Tables 3A and 3B)
Falling
No static anatomical measurement showed any relationship to fall frequency in the group as a whole or in younger and older patients. These included amplitudes of cervical tilt or high, mid, and low thoracic scoliosis, and presence or absence of kyphosis or complex thoracic scoliosis. All patients had stationary flexed-forward resting postures of head and neck that did not vary among groups (Figure 1A). Of dynamic axial movements, neck flexion, full neck pitch movements, and leftward neck rotations had reduced amplitudes in patients who fell compared to nonfallers. While both older and younger fallers tended to have reduced dynamic head and neck movement amplitudes compared to older and younger nonfallers respectively, these did not reach statistical significance. Rightward, leftward, and total horizontal neck rotations were reduced in older fallers and nonfallers compared to their younger counterparts.
Table 3A: Dynamic measurements segregated by fall frequency

*Student’s t-test.
Table 3B: Dynamic measurements segregated by age

*Student’s t-test.
†Chi square/chi square for trend.
‡ANOVA.
The risk of falling doubled for patients with limited cervical motility for both total rotation in yaw (<85.9 degree) and pitch (<66.6 degree) compared to those who had normally sized rotations in both (OR 2.101; 95% CI 1.27–3.47; p = 0.005).
FES-I
When assessing the contribution of risk factors to the variance in FES-I scores among fallers, other fall risk factors which significantly and independently contributed to fall risk (age, pain, number of psychotropic medications, and peripheral neuropathy) explained 35.6% of the total 48.3% variance in FES-I scores within the group of fallers as a whole (F (7, 96) = 12.810, p < 0.0001). The presence of mid-thoracic kyphoscoliosis and leftward neck rotation were the most robust anatomical risk factors, contributing another 12.7% of the variance in FES-I scores in fallers. When older fallers were analyzed separately, fatigue was the only significant independent risk factor, accounting for all of the 43.6% total variance in FES-I scores (F (1, 15) = 11.614, p = 0.004).
Symptom Duration
For fallers as a group, duration of symptoms correlated negatively with total horizontal neck rotation (r = −0.230; p = 0.014) and positively with mid-thoracic scoliosis amplitudes (r = 0.191; p = 0.042), controlling for age. This was similar for younger fallers; axial rotations to right (r = −0.146, p = 0.014) and left (r = −0.149, p = 0.012) were both negatively correlated with duration and mid-thoracic scoliosis amplitudes positively correlated with symptom duration (r = 0.133, p = 0.025). In the older faller cohort, total pitch amplitude and more specifically, neck flexion amplitudes, were negatively correlated with symptom duration (r = −0.268; p = 0.012). For all nonfallers, there were no significant correlations between any static or dynamic anatomical measurements and duration of symptoms.
Discussion
In our population of patients with chronic soft-tissue rheumatic complaints, increased fall frequency and fear of falling occurred in patients who had reduced cervical mobility and increased mid-thoracic kyphoscoliosis. With chronic neck and upper back pain, horizontal head rotations become smaller, slower, longer, and more delayed over time, Reference Johnston, Daye and Thomson11 as evidenced by negative correlations between head rotations and symptom duration in all faller cohorts. The consequence is head-on-trunk stability at the expense of gaze accuracy when making large unpredictable horizontal head-free gaze shifts. Reference Johnston, Daye and Thomson11 In the sagittal plane, head angular displacements remain small during ambulation Reference Pozzo, Berthoz and Lefort19 and continuously move within a range of flexion. Reference Cromwell, Aadland-Monahan, Nelson, Stern-Sylvestre and Sede20 Stability in the head-flexed forward position may improve reliability of otolithic signals by providing consistent gravitational orientation for the vestibular system. Reference Pozzo, Berthoz and Lefort19,Reference Pierrot-Deseilligny and Milea21 Our population of fallers had significantly reduced neck flexion amplitudes when compared to nonfallers, even though resting amplitudes were identical.
Our data showed greater restriction of head and neck mobility in fallers for both horizontal rotations and for flexion-extension movements in the sagittal plane. While this will not affect gaze stability and balance when ambulating and maintaining a fixed line of sight, if active gaze redirection is required, limited neck mobility may cause impaired perception of self-motion, Reference Cullen10 reduced gaze accuracy, Reference Johnston, Daye and Thomson11 problems navigating a complex visual environment, inability to adjust rapidly to perturbations, Reference Kavanagh, Barrett and Morrison22 and falls. It also contributed to increased fear of falling in fallers. Finally, while mobile, older adults require more time to react to and avoid obstacles in their path. Reference Cao, Ashton-Miller, Schultz and Alexander23 Delay in precisely acquiring the image of an obstacle because of reduced head-free motion and inaccurate gaze will further prolong reaction time and increase fall risk.
Of further interest is the consistent asymmetry between leftward head and neck rotations compared to rightward rotations. Leftward rotations were reproducibly larger in all groups and were significantly reduced in fallers compared to nonfallers, while rightward head rotations, although reduced in fallers, did not achieve statistical significance. The reasons for these differences are not readily apparent, but may be a function of most patients being right-side dominant. Additionally, our patients were exclusively Canadian, and almost all were automobile drivers. Leftward shoulder-checking in vehicles and when crossing streets may constitute long-term exercise, resulting in increased range of motion.
When considering static axial abnormalities in fallers, mid-thoracic kyphoscoliosis contributed to the variance in FES-I, but not to falling, suggesting that these individuals had greater concern regarding the possibility of falls, but they did not necessarily fall. One theory regarding development of adolescent idiopathic scoliosis concerns vestibular dysfunction. Inner ear lesions in animals induce spinal rotations of thoracic vertebrae similar to idiopathic scoliosis. Reference De Waele, Graf, Josset and Vidal24 Studies in humans with scoliosis have shown asymmetric otolithic vestibular responses Reference Wiener-Vacher and Mazda25,Reference Pollak, Shlamkovic, Minewicz and Mirovsky26 and altered perception of visual vertical, indicating imbalance in the roll plane. Reference Cakrt, Slabý, Viktorinová, Kolář and Jeřábek27 In patients with large Cobb angles (a radiological measure of lateral spinal curvature), the sum total of these abnormalities is static and dynamic imbalance. Reference Gauchard, Lascombes, Kuhnast and Perrin4 Our patients had much smaller thoracic scoliosis angles (only seven patients had the equivalent of Cobb angles of 20 degrees or more) and although we did not undertake vestibular studies, no patient had vertigo. Likewise, prior investigation of the VOR in a population of patients with chronic restrictions of cervical motion showed normal vestibular function. Reference Johnston, Daye and Thomson11 Thus we would not expect these small thoracic deviations to have vestibular origins. Nonetheless, mid-thoracic kyphoscoliosis did contribute to the fear of falling, more so in younger fallers. In younger individuals, the trunk modulates gait-induced oscillations minimizing the need for additional control from neck muscles, especially at faster gait speeds. Reference Kavanagh, Barrett and Morrison28 Although our young fallers were typically unaware of their thoracic kyphoscoliosis (only two individuals knew of adolescent thoracic scoliosis), it suggests that they were unconsciously mindful of the need to increase trunk muscle coactivation in order to maintain stability. Older individuals have less trunk muscle coactivation, correlating with slower gait and greater instability. Reference Lee, Chang, Choi, Ryu and Kim29 They do not use trunk muscles to modulate gait-induced oscillations and rely more on neck muscles to enhance head stability by locking neck to trunk motion. This is manifested by lower head accelerations in older compared to younger individuals Reference Menz, Lord and Fitzpatrick30 and may explain why thoracic kyphoscoliosis did not contribute to fear of falling in our older cohort of fallers.
In total, 88.5% of multiple fallers were patients less than 65 years of age. The reason for this trend is unknown; however repeated falls in younger individuals may lead to injuries, worsening musculoskeletal complaints and with aging, cause greater impairments in mobility. Reference Kenny, Rubenstein and Tinetti3 With persistence of musculoskeletal symptoms, over time there is greater reduction in neck rotation amplitudes as evidenced in older fallers. This enhanced head-on-trunk stability is a possible mechanism for cervical vertigo due to prolonged VOR suppression and reduced gaze saccade accuracy, and can occur at any age. Reference Johnston, Daye and Thomson11 It may also underlie the increased falling seen in our older cohort. Enhanced VOR suppression may be a function of the chronicity of their disorder and the result of anti-Hebbian plasticity in the cerebellum, which, over time induces synaptic changes to further reduce the vestibular response to head movement during head-free gaze shifts. Reference Cullen10 Moreover, chronic suppression of the VOR may cause visual-vestibular mismatch and evoke brainstem mechanisms for additional VOR suppression. Reference Carcaud, França de Barros and Idoux31 Finally, increased fear of falling may cause additional neck immobility through cervical muscle coactivation in a flawed attempt to improve stabilization.
The individuals in this study did not present with concerns regarding imbalance or falls; however, a large number of both young and older patients had fallen in the prior year. As we relied on recollection of falls, there may have been errors in patient estimation of fall frequency. However, it is important to recognize that individuals who complain of chronic upper body soft tissue discomfort have a twofold likelihood of falling, perhaps similar to imbalance seen with acute neck pain. Reference Karlberg, Johansson, Magnusson and Fransson7–Reference Uthaikhup, Jull, Sugnkarat and Treleaven9
In patients who have fallen or are at risk for falls, it is imperative to assess for neck mobility restriction in addition to comprehensive neurological examination. Impaired cervical movement may cause dizziness and increased falls in the absence of vestibulopathy, structural lower limb abnormalities or other neurological, and non-neurological conditions typically associated with falling. Reference Thurman, Stevens and Rao2 This was a small study, and there was great variability in the range of cervical mobility; nonetheless, patients with total sagittal rotations less than 70 degrees and total horizontal rotations less than 90 degrees should be considered as being at greater fall risk, and their restrictions are typically obvious to the clinician. In assessing patients for restricted cervical mobility at the bedside, this translates into horizontal head and neck rotations from primary position midway to shoulder tip in both directions. For sagittal rotations, patients should be able to look up to the ceiling (extension) and down to the floor (flexion) with the chin touching the chest.
Conclusion
Patients presenting with restricted dynamic cervical rotations are at increased fall risk and have greater fear of falling, independent of other conventional fall risk factors. Static axial abnormalities do not influence fall risk, but mid-thoracic kyphoscoliosis amplitudes contribute to fear of falling. As part of a comprehensive neurological fall risk evaluation, dynamic and static cervicothoracic biomechanical assessment should be undertaken, along with more conventional vestibular, lower limb sensorimotor, and cognitive examination.
Disclosures
The authors report no financial disclosures or conflicts of interest that could bias the results of the study.
Statement of Authorship
JJ and GT conceived the study. GT examined the patients. GT and GF undertook the measurements. GT, JJ, and SH carried out the statistics and wrote and edited the manuscript.







