CASE PRESENTATION
A previously healthy 23-year-old man presented to the emergency department (ED) during the night, seven days after sustaining a left ankle injury during a soccer match when another player inadvertently kicked him. His vital signs at triage were as follows: heart rate 75beats/minute, blood pressure 177/101 mm Hg, respiratory rate 22breaths/minute, O2 sat 98% on room air, temperature 36.6°C. He complained of severe pain. The patient did not recall any specific inversion or eversion mechanism during the injury; he described it as an “ankle-to-ankle collision” while running. He was unable to continue playing or to weight-bear. He had attended a sports medicine clinic the day after the injury. At that time, the ankle/foot were described as markedly swollen but neurovascularly intact, with both medial and lateral ankle tenderness. X-rays completed there did not show any fracture, and he was diagnosed with an ankle sprain. Initial treatment consisted of immobilization in a below-knee back slab, crutches, and oral naproxen for pain control. The patient had been compliant with treatment, and denied any weight-bearing on the injured limb at home. He reported that his symptoms, including local swelling, had been steadily improving all week until the sudden onset of severe ankle pain while watching television with his foot elevated, approximately four hours before his ED presentation. He was not experiencing fever, shortness of breath, chest pain, or paresthesia. He also denied any chronic medical conditions, allergies, or illicit drug use.
On examination, the patient was pale, diaphoretic, and experiencing severe pain. He remained hypertensive with a blood pressure of 168/98 mm Hg; vital signs were otherwise normal. The anterolateral aspect of the left ankle was markedly swollen, with extensive purple contusions extending over the posterolateral ankle and lateral foot (Figure 1). The dorsalis pedis and posterior tibialis pulses were present; the skin of the foot and toes was pink, warm, and well-perfused with normal capillary refill. Skin temperature was not appreciably different than the contralateral foot. No marked erythema, lymphangitis, pustules, abrasions or other skin lesions were noted. There was extreme hyperalgesia with testing of light touch over the dorsum of the ankle and foot, roughly corresponding to the distal distribution of the superior peroneal nerve. Sensation in the lower extremity was otherwise grossly normal. The patient was able to actively flex and extend his left toes, and demonstrate small degrees of active plantar- and dorsiflexion, inversion, and eversion of the left ankle. However, complete assessment of motor function during this initial examination was precluded by significant patient discomfort.

Figure 1 Clinical image of patient’s affected ankle, with surface location of pseudoaneurysm marked with large X.
Initial ED management consisted of oral and parenteral analgesia with acetaminophen, ketorolac, and morphine, as well as intravenous ceftriaxone. X-rays revealed significant soft tissue swelling over and around the lateral malleolus, with a few well-corticated ossific densities in the swollen tissue. No fracture or air in the tissue was identified. Laboratory tests were unremarkable. The differential diagnosis included an expanding hematoma secondary to vascular injury, abscess, DVT, and complex regional pain syndrome.
Duplex ultrasound performed in the radiology suite the following morning (eighth day after initial injury) revealed a left anterior tibial artery pseudoaneurysm at the level of the ankle measuring 2.94×1.86 cm, with a 5.6×1.9 cm hematoma overlying the lateral ankle (Figures 2 and 3). Diagnostic ultrasound images of the lesion were obtained by scanning over skin marked with the large X (Figure 1), corresponding to the area of maximal swelling and pain. Distal flow was identified within the dorsalis pedis artery. The diagnosis was confirmed with CT angiography, which demonstrated a large pseudoaneurysm arising from the dorsal-lateral aspect of the proximal dorsalis pedis artery. Of note, after imaging the patient was re-examined and found to have an easily audible bruit in the area of the anterolateral ankle and dorsum of the foot, overlying the pseudoaneurysm.
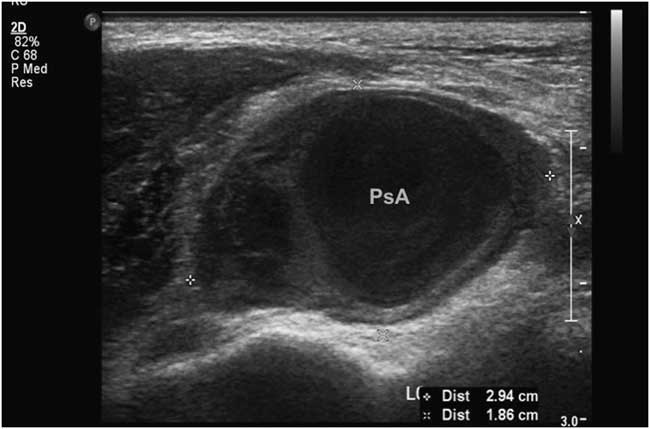
Figure 2 2D ultrasound image showing maximal diameter of anterial tibial pseudoaneurysm.
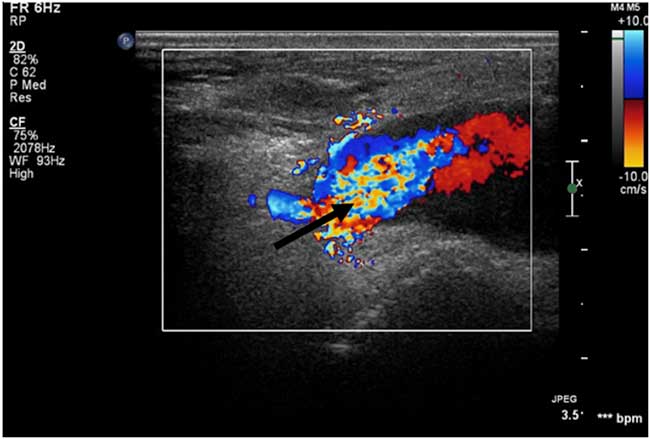
Figure 3 Colour Doppler ultrasound image of this patient’s pseudoaneurysm. Blue = blood flow toward probe, Red = blood flow away from probe, Arrow = area of high-velocity swirling.
Definitive management, consisting of embolization of the pseudoaneurysm with platinum microembolization coils, was performed in the interventional radiology suite the same day (Figure 4).

Figure 4 Angiogram image taken in the Interventional Radiology suite, showing saccular pseudoaneurysm located anterolateral to the talocrural joint.
DISCUSSION
Lower extremity arterial injuries are uncommon, affecting an estimated 0.39% of patients admitted to hospital with traumatic injuries.Reference Franz, Shah and Halaharvi 1 The majority of these patients have suffered significant lower extremity trauma. In one recent retrospective review, 78.4% of patients with lower extremity arterial injuries had other lower extremity injuries, and 35.4% had injured other body regions.Reference Franz, Shah and Halaharvi 1 Predictably, patients presenting with severe lower extremity trauma remain at high risk of associated arterial injury, with an incidence of 57.1% reported in this patient population.Reference Haddock, Weichman and Reformat 2 The anterior tibial artery is most commonly injured (31.9% of patients).Reference Haddock, Weichman and Reformat 2 , Reference Lädermann, Stern and Bettschart 3
In ambulatory patients, injury of the anterior tibial artery can occur as the result of routine procedures, minor trauma, or concomitant medical disease. Such injuries, particularly pseudoaneurysms, are rare but well-recognized complications of ankle arthroscopy, with a reported incidence of 0.008%.Reference Jacobs, Groot and Das 4 - Reference Mariani, Mancini and Tara 7 Rarely, pseudoaneurysm of the anterior tibial artery has been described as a result of endocarditis, connective tissue disease, biopsy, and, as in our case, sports injury.Reference Murashita, Yasuda and Takigami 8 - Reference Marron, McKay and Johnston 13
Pseudoaneurysms may occur when all 3 layers of the arterial wall—intima, media, and adventitia—are damaged. This allows for extravascular hematoma collection, with formation of a surrounding fibrous wall, which communicates directly with the intra-arterial lumen.Reference Lädermann, Stern and Bettschart 3 , Reference Shah, Fischman and Marin 11 Complications of arterial pseudoaneurysms include infection, compression of surrounding neurovascular structures, limb ischemia, necrosis of overlying skin, and rupture. 14 - Reference Webber, Jang and Gustavson 16 Pseudoaneurysms carry a higher risk of rupture than true arterial aneurysms.Reference Lädermann, Stern and Bettschart 3 , 14 - Reference Webber, Jang and Gustavson 16 We suspect that the suddenly escalating pain experienced by our patient, one week after the traumatic event, occurred when the pseudoaneurysm began to leak and/or expand, resulting in a high-pressure collection of blood. Branches of the superficial peroneal nerve passing through the anterolateral ankle may have been compressed, explaining the exquisite hyperalgesia noted to the dorsum of the foot.
A high index of suspicion is necessary to diagnose anterior tibial artery pseudoaneurysm in the absence of major trauma. A tender or pulsatile mass of the lower leg, signs or symptoms of neurovascular insufficiency, or disproportionate pain or swelling after any lower limb injury or invasive medical procedure should prompt consideration of this diagnosis. Presentation may be delayed by months, following the initial insult.Reference Lädermann, Stern and Bettschart 3 , Reference Verbrugghe, Vandekerkhof and Baeyens 5 , Reference Ramavath, Cornish and Ganapathi 17 As in our case, the differential diagnosis often includes infectious processes such as abscess formation. Varying degrees of swelling, fluctuance, erythema, pain, leukocytosis and other non-specific findings may lead the clinician to consider empiric incision and drainage of an arterial lesion presumed to be an abscess. Auscultation for a bruit during the initial assessment—which was present and easily audible upon subsequent examination of our patient—would have confirmed our initial suspicion of a vascular problem. We propose that bedside ultrasound, employed by a trained emergency physician, may be helpful in avoiding this potentially serious iatrogenic complication. Other advantages of this approach include decreased time to diagnosis and definitive therapy, and decreased ED length of stay.Reference Goksu, Kucukyilmaz and Soyuncu 18
While angiography remains the gold standard for diagnosis and treatment planning, duplex ultrasound is the accepted modality for initial non-invasive imaging.Reference Shah, Fischman and Marin 11 , Reference Webber, Jang and Gustavson 16 Sensitivity and specificity of duplex ultrasonography in the diagnosis of pseudoaneurysm are estimated at 94% and 97%, respectively.Reference Coughlin and Paushter 19 Bedside diagnosis of post-traumatic arterial pseudoaneurysms of the face and lower limb, using point-of-care ultrasonography performed by the ED physician, has indeed been described in a few case reports of single patients.Reference Goksu, Kucukyilmaz and Soyuncu 18 , Reference Goksu, Yuruktumen and Kaya 20 - Reference Jenq, Panebianco and Lee 22 The bedside technique most commonly described consists of linear ultrasound probe placement directly over the area of maximal swelling (or bruit/thrill, if present).Reference Goksu, Kucukyilmaz and Soyuncu 18 , Reference Goksu, Yuruktumen and Kaya 20 The anechoic pseudoaneurysm cavity may be pulsatile and is commonly surrounded by hypoechoic thrombus (Figure 2).Reference Goksu, Kucukyilmaz and Soyuncu 18 , Reference Jenq, Panebianco and Lee 22 This sonographic appearance may closely resemble that of an abscess cavity with debris.Reference Abdi, Armijo and Seif 21 The use of color Doppler is particularly valuable in differentiating the two. Characteristic findings of pseudoaneurysm include bidirectional blood flow in the pseudoaneurysm neck, pulsatile flow in the cavity (Figure 3), and the “yin-yang sign” (swirling blood in the pseudoaneurysm resembling the ancient symbol).Reference Goksu, Yuruktumen and Kaya 20 The accuracy of bedside ultrasound in the diagnosis of arterial pseudoaneurysms has not yet been elucidated.
Current first-line therapies for arterial pseudoaneurysm include ultrasound-guided thrombin injection, and endovascular procedures including embolization and coiling, as described in our patient.Reference Jacobs, Groot and Das 4 , Reference Webber, Jang and Gustavson 16 , Reference Mavili, Donmez and Ozcan 23 , Reference Pan, Medina and Suarez de Lezo 24 First-attempt success rates with these procedures are high (>90%) and complication rates are low.Reference Webber, Jang and Gustavson 16 , Reference van Hensbroek, Ponsen and Reekers 25 Ultrasound-guided compression therapy is also reported to be effective and safe, though more resource intensive.Reference Jang, Kwak and Song 6 , Reference Webber, Jang and Gustavson 16 , Reference Fellmeth, Roberts and Bookstein 26 A minority of patients require open surgical resection, particularly those with infected or rapidly expanding pseudoaneurysms, skin necrosis, limb ischemia, or neurovascular compromise.Reference Webber, Jang and Gustavson 16 , Reference Lumsden, Miller and Kosinski 27 , Reference Saad, Saad and Davies 28 The literature also documents successful conservative management, i.e., observation only, of painless arterial pseudoaneurysms measuring <2 cm.Reference Shah, Fischman and Marin 11 One year after coiling of his pseudoaneurysm, our patient is asymptomatic and has no functional limitations. He remains active and plays sports regularly.
CONCLUSION
Disproportionate pain and/or swelling after lower limb injury, even when the insult is apparently innocuous or the presentation is delayed, should raise the clinician’s index of suspicion for these uncommon vascular lesions. Duplex ultrasound is well established as the initial gateway to definitive diagnosis. Bedside ultrasound is rapidly becoming a vital extension of the emergency physician’s physical examination. The indications for, and applications of, ED targeted ultrasound are expanding. Imaging findings in this case suggest that the lesion may have been detectable by an ED physician using ultrasound at the bedside. As with other conditions, this has the potential to facilitate more timely diagnosis and definitive treatment for patients. More research is needed to establish the diagnostic accuracy and utility of point-of-care ultrasound in the evaluation of suspected lower limb vascular lesions.
Competing Interests: This research received no specific grant funding from any funding agency, commercial or not-for-profit sectors. No conflict of interest declared.






