INTRODUCTION
Fractures of the distal forearm are among the most common injuries presenting to the pediatric emergency department (PED). Forearm fractures represent nearly 25% of all childhood fractures, and approximately 19% of these require a closed reduction.Reference Landin 1 , Reference Kramhoft and Bodtker 2 A closed reduction is most often performed in the PED setting with analgesia for manipulation provided using procedural sedation (PS). While generally well tolerated, the agents used for PS can be associated with post-procedural emesis, psychotomimetic recovery reactions, and adverse airway events.Reference Green, Roback and Krauss 3 , Reference Green, Roback and Krauss 4 Moreover, patients undergoing PS require ongoing post-procedural monitoring until they return to a pre-procedural level of alertness,Reference Evered 5 prolonging length of stay and increasing associated costs.Reference Aarons, Fernandez and Willsey 6
Intravenous (IV) regional anesthesia, or Bier block (BB), is a safe and effective alternative to PS for forearm fracture reduction. The procedure consists of isolating the circulation of the affected limb with a pneumatic cuff and infusing lidocaine for rapid and complete anesthesia of the tourniquet-injured extremity. Patients remain awake throughout the procedure, without risk of central nervous system depression and/or respiratory effects. BB requires no pre-procedural fasting or post-procedural observation periods. Consequently, this technique is associated with reduced PED time and resource utilization.Reference Aarons, Fernandez and Willsey 6 Furthermore, several studies have demonstrated the efficacy of BB for forearm fracture reduction, with very infrequently reported adverse events.Reference Blasier and White 7 - Reference Mohr 10 One large Canadian retrospective review of 1816 adult and pediatric BB procedures reported zero-failed reductions, no major adverse events, and a minor adverse event rate of only 0.5%.Reference Mohr 10
Despite the many advantages offered by the use of BB, it remains an infrequently used technique. In a survey of 44 North American pediatric emergency medicine fellowship program directors, only 19% of respondents reported that BB was ever used for forearm fracture reductions at their centres.Reference Constantine, Steele and Eberson 11 The most common reason cited for not using local anesthesia techniques (including BB) was the efficacy of PS, and the authors further suggested decreased physician comfort level as a barrier to more widespread use of this regional technique.
In June 2012, our tertiary PED introduced BB as an analgesic alternative to PS for forearm fracture reductions, becoming the first Canadian PED to successfully implement a BB program. Prior to the implementation of the BB program, we designed and administered a novel simulation and Web-based training course for PED staff, and undertook a survey-based assessment of attitudes regarding BB. In parallel, we prospectively evaluated the clinical use of BB in the PED following course delivery. We hypothesized that a multimodal training course would increase staff comfort and willingness to use BB, and ultimately lead to increased use of this technique for closed forearm fracture reductions in the PED. The specific objectives of this study were to 1) assess PED staff attitudes regarding BB before and following a multimodal training course, and 2) prospectively determine the in vivo clinical uptake of BB in the PED following course participation.
METHODS
Study design, setting, and participants
We designed and administered an interdisciplinary, multimodal BB training course in June 2012, and used a pre-/post-questionnaire study design to survey course participants at four time points: immediately prior to and following course participation, and at 2 and 6 months following course completion. The study population included PED physicians and nurses at The Montreal Children’s Hospital, an urban Canadian tertiary pediatric centre serving children defined as<18 years of age, with an annual census of over 84,000 visits. Study participants were asked to complete a one-page, paper questionnaire, which was previously piloted for clarity by individuals not included in the study.Reference Bretholz, Graham and Cheng 12 The questionnaire consisted of multiple-choice questions designed to assess 1) previous experience with BB, 2) comfort with and willingness to use BB, and 3) the value added by the BB training course. Attitudes regarding BB and the BB training course were assessed using a 4-point Likert scale. Study participant demographic data were also collected. This study was approved by the Research Ethics Board of the McGill University Health Centre, and informed written consent was obtained from all participants.
Training course design
The BB training course content was developed in consultation with experts, according to consensus-based guidelines and using best-evidence practice recommendations.Reference Kam, Kavanagh and Yoong 13 - 16 Participants completed a pre-course, self-directed, Web-based learning module prior to attendance of a complementary simulation-based training session. The online learning component provided an overview of the BB technique and reviewed potential adverse events using text, illustrations, and video. This online pre-course tutorial was developed to complement the simulation-based sessions in order to maximize participant learning and retention. Following completion of the online pre-course tutorial, subjects participated in a standardized, half-day course with simulation-based training and debriefing, which commenced with a 30-minute, evidence-based didactic session. A checklist outlining the critical steps required to safely perform BB was developed a priori and was distributed and referenced during the course. Participants were provided a pocket card memory aid outlining the signs, symptoms, and management of lidocaine toxicity. Simulations incorporated standardized patients and both high- and low-fidelity mannequins for a hands-on opportunity to practice the BB technique, as well as to recognize and respond to potential complications. Scenarios and standardized patient roles were tightly scripted to ensure a consistent educational experience for all learners.Reference Cheng, Auerbach and Hunt 17 A total of four 10-minute simulation scenarios were delivered during the course, all involving forearm fractures following various injuries (simulation curriculum available in Online Supplement 1). Scenario one involved obtaining pre-procedural consent with a 17-year-old patient. Scenario two required the use of distraction techniques and medical management for an anxious 16-year-old patient undergoing BB. Scenario three was a case of an 8-year-old patient with equipment failure and seizure. Scenario four was a case of a 10-year-old patient with a local anesthetic medication error and cardiac arrest. All simulation scenarios used the same automatic tourniquet system for BB that was available to participants in the PED of their clinical practice (A.T.S 3000, Zimmer Inc.). The four simulation facilitators had previous training in the use of BB, as well as prior experience in simulation-based education and debriefing ranging from 2 to 10 years. Debriefing sessions were conducted using a mix of Plus-Delta and Advocacy-Inquiry methods of debriefing,Reference Cheng, Eppich and Grant 18 without the use of video review, and limited to a maximum of 10 minutes per debriefing. Two identical, English-language training courses were offered over 2 consecutive days by the same instructors. Following course completion, participants were tracked to record BB procedures performed for maintenance of competency.
Determination of clinical Bier block utilization
Beginning in May 2012, prior to BB training course administration, all patients presenting to the PED with displaced forearm fractures were captured daily by a research assistant in a prospectively maintained database for research purposes.Reference Dubrovsky, Kempinska and Bank 19 In June 2012, following delivery of the BB training course, our PED implemented BB for the first time as an alternative to PS for children of 6 to 18 years of age presenting with forearm fractures requiring closed reduction. An interprofessional protocol was developed for the safe use of BB in the PED and was approved by the institutional Clinical Practice Review Committee (protocol available in Online Supplement 2). Patients were not eligible for BB if they presented with one of the following contraindications: lidocaine allergy, seizure disorder, blood dyscrasia, compromised circulation, bilateral forearm fractures, open fracture, or if they were non-verbal. Reductions using BB were performed by pediatric emergency physicians and offered at the discretion of the treating physician with consideration of patient/family preferences. Patients undergoing either BB or PS for fracture reduction were identified by the research assistant, and patient identification numbers were used to access the electronic patient charts as well as standardized BB and sedation monitoring forms. Charts were reviewed by a single investigator (EFL), and data were extracted to determine the number of BBs performed, and the number of physicians using BB for forearm fracture reductions. We included all closed forearm fracture reductions for children greater than 6 years old and eligible for both BB and PS, performed between June 2012 and June 2014 by all pediatric emergency physicians trained during the pre-implementation course.
Statistical analysis
Categorical variables are expressed as proportions and were analysed by McNemar testing for paired data (GraphPad Prism software, v6.03). A minimum sample size of 5 was calculated to achieve 90% power for detecting a change from 20% to 80% on questionnaire responses. A two-tailed p-value<0.05 was considered statistically significant.
RESULTS
Overall, 38 subjects (N=26 physicians, 12 nurses) participated in the Web- and simulation-based training course. Demographics of the study participants are shown in Table 1. All participants completed pre- and post-course surveys, and the survey response rate at both 2 and 6 months remained at 100%.
Table 1 Participant demographics
Participants’ pre- and post-training attitudes regarding BB are shown in Figure 1. Prior to the course, 10% of participants indicated that they felt comfortable (score≥3) performing BB for fracture reduction, compared to 89% (p<0.001) at the time of course completion. Comfort with BB reportedly fell to 66% at 6 months (p=0.02 v. post-course), although it remained significantly higher than baseline (p<0.001). Willingness to perform BB was similarly increased by course participation (score≥3; 51% pre-course v. 95% post-course, p<0.001) and remained elevated at 6 months (92%, p<0.001).
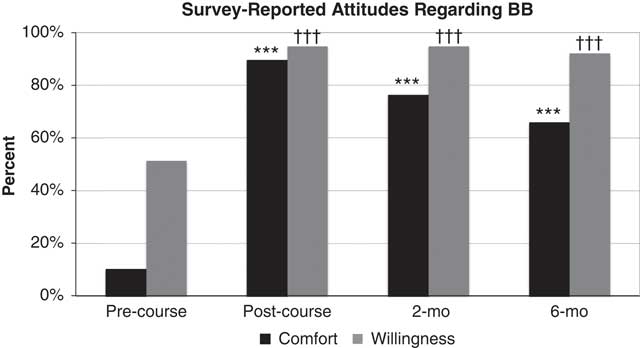
Figure 1 Responses from course participants during pre-course, post-course, 2 and 6 months’ post-training regarding comfort with (black bars) and willingness to perform (grey bars) Bier blocks; ***p<0.001 v. pre-course comfort, ††† p<0.001 v. pre-course willingness.
Immediately following the course, all of the participants either agreed (42%) or strongly agreed (58%) that the course addressed their learning objectives. At 2 months, 45% (17/38) of participants indicated that they felt a refresher course was necessary. Comparatively at 6 months, 66% (25/38) of respondents favoured a refresher course, with a majority of these participants (14/25) endorsing a semiannual review emphasizing simulation-based learning.
We assessed self-reported experience with BB before and following BB training (Figure 2). To ascertain baseline experience prior to the course, 6% of participants reported having previously performed BB in a PED setting other than in our institution. Respondents reported a significant increase in their clinical experience with BB at 2 months (37%, p=0.02) and at 6 months (53%, p<0.001 v. pre-course; p=0.04 v. 2 months).
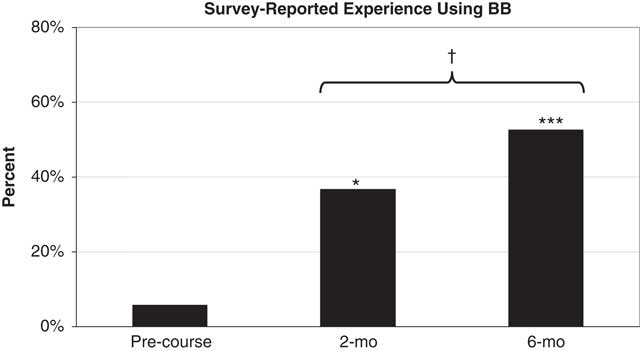
Figure 2 Self-reported responses from course participants pre-course, 2 and 6 months’ post-training regarding experience with Bier block; *p<0.05 and ***p<0.001 v. pre-course, † p<0.05 v. 2 months.
To assess the clinical uptake of BB by pre-implementation course-trained physicians, we quantified the clinical use of BB for fracture reductions in the 24-month period following course delivery (Figure 3). Prior to the training course and BB implementation in the PED, no BB had been performed at our centre. In the period immediately following course completion, there was a sustained increase in the use of BB, with 79 BB reductions performed at 24 months by physicians in the study population. Similarly, BB-assisted forearm reductions were performed by an increasingly diverse number of these physicians, with 50% (13/26) of physicians using BB at 24 months, 46% (6/13) of whom performed≥5 BB by this time. Relative use of BB in comparison to PS over time is depicted in Figure 4. At 24 months, 37% of all forearm reductions performed by course-trained physicians used BB (79 BB v. 137 PS).
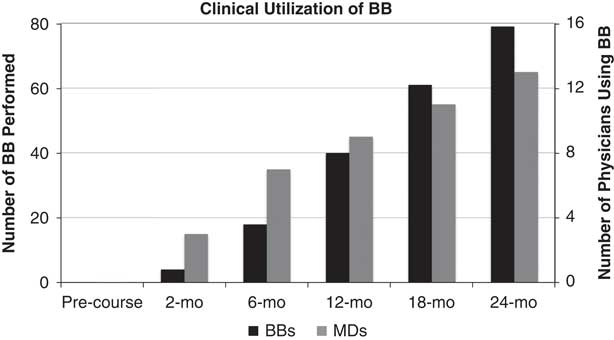
Figure 3 Absolute number of Bier blocks (black bars, left axis) and course-trained PED physicians (grey bars, right axis) performing Bier blocks at intervals following training course delivery.
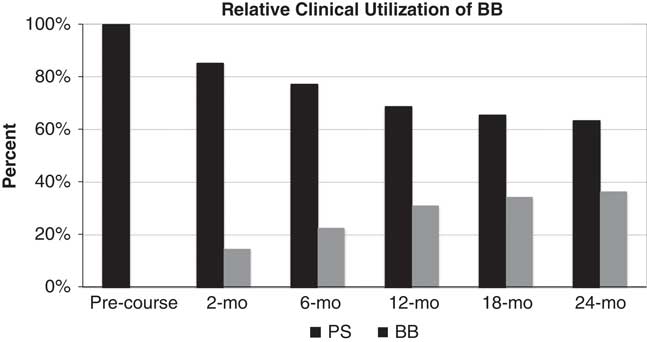
Figure 4 Relative use over time of Bier block (grey bars) and procedural sedation (black bars) for forearm fracture reductions by course-trained PED physicians.
DISCUSSION
For the present study, we have designed and administered an interdisciplinary, simulation, and Web-based training course to instruct novice users the technique of BB for pediatric forearm fracture reductions. Findings demonstrate that the multimodal training course was an effective method for increasing PED staff comfort with, and willingness to use BB for forearm fracture reductions. Moreover, completion of the training course was associated with increased use of BB in clinical practice, despite low participant comfort and experience with BB prior to training.
BB for closed reduction of pediatric forearm fractures has been well described in the literature but remains infrequently used in the PED.Reference Constantine, Steele and Eberson 11 Although the efficacy of PS for pediatric fracture reductions is well established, side effects of sedating agents and the considerable resource utilization associated with PS make BB an attractive alternative. There are several theoretical barriers that have thus far potentially limited a more widespread adoption of BB. For example, perceived difficulty placing an IV in an injured extremity might bias against the use of BB in children; however, this occurred in only 3 of 470 children ages 2 to 19 years in one large case series.Reference Blasier and White 7 The theoretical lack of muscle relaxation that is thought to facilitate fracture reduction with PS does not appear to compromise reduction success when using BB.Reference Blasier and White 7 - Reference Mohr 10 Pain that may be associated with the high-pressure cuff can be minimized by the use of now readily available dual bladder tourniquet systems, which also provide an increased safety margin to reduce the theoretical risk of lidocaine toxicity.Reference Henderson, Warriner and McEwen 20 A systematic review of studies from 1950 to 2007 identified just eight major adverse events among pediatric patients receiving BB, all of which resulted from toxic dosing of local anesthetics and/or unreliable tourniquets; the review highlighted the low incidence of complications and concluded that BB is a safe anesthetic technique.Reference Guay 21
Despite the advantages offered by the use of BB, staff comfort level remains an important obstacle to more widespread uptake of this technique. Our multimodal training course was developed to increase PED staff comfort with BB and support the safe implementation of a BB program. The course was designed to maximize participant learning, and we elected to incorporate both simulation and Web-based learning modalities. There is significant literature supporting the use of both computer-assisted and simulation-based education to facilitate the acquisition of procedural skills.Reference Ricks, Ratnapalan and Jain 22 , Reference Sawyer, White and Zaveri 23 A meta-analysis by Lam-Antoniades et al. reviewed 15 studies evaluating education interventions and found that multicomponent interventions were effective at changing health-care professionals’ practice patterns and improving their knowledge.Reference Lam-Antoniades, Ratnapalan and Tait 24 White et al. have demonstrated that a combination of didactic, video, and simulation-based training can augment resident confidence and knowledge for pediatric lumbar puncture procedures.Reference White, Jones and Zinkan 25 To our knowledge, this is the first description of a training course to teach the use of BB for fracture reduction. Participants in our study unanimously indicated that the multimodal training course addressed their learning objectives. It is not possible from our study design, however, to compare this multimodal training, in particular, to another style of training, or to determine the added incremental value of either online or simulation-based training alone.
We found that 37% of all eligible reductions at 24 months were performed using BB by half of the course-trained physicians. Additionally, at 6 months, nearly all participants in our study remained willing to use BB but reported a moderate yet significant attrition in comfort with BB. Several factors can influence physician comfort and use of BB, including clinical opportunity, patient/family preferences, and department logistics. It is also reasonable to hypothesize that both the number of physicians not using BB and the reported decline in comfort could relate to a decline in skill retention over time. Skill retention is a well-recognized concern in procedural skill training, and decline of physician knowledge and performance following initial simulation-based training are well described.Reference Semeraro, Signore and Cerchiari 26 , Reference Chamberlain, Smith and Woollard 27 Several studies have emphasized the importance of refresher courses to maintain critical skill competency.Reference Niles, Sutton and Donoghue 28 , Reference Nishiyama, Iwami and Murakami 29 The question of refresher frequency and timing is likely to vary, depending on the psychomotor complexity of the skill being learned as well as how routinely that skill is revisited by an individual in clinical practice. The majority of participants in our study population were in favour of a refresher course at 6 months following course completion. It is possible that refresher course administration would have attenuated the decline in comfort and increased the number of physicians using BB at 24 months. It remains to be determined the appropriate interval for refresher courses to maintain greater comfort with BB in the PED.
Several limitations of the present study are inherent to the pre-post study design. Our training course was administered concurrently with the implementation of BB at our centre, such that it is not possible to isolate effects that result solely from training course delivery. Importantly, our study cohort began with minimal baseline comfort and experience using BB, and we have attempted to determine the extent to which course participation altered participant attitudes towards BB by conducting surveys both immediately before and following course completion. Despite utilization of BB by half of the study physicians for more than a third of all forearm fracture reductions, our survey did not specifically explore the reasons why some physicians were not using BB post-course. Because all study participants completed pre-post surveys, the study cohort had no true control for the training intervention. Findings from this study can be generalized only among novice BB users. It is of note, however, that a survey of 44 North American pediatric emergency medicine fellowship program directors reported that BB was seldom used at their centres.Reference Constantine, Steele and Eberson 11 Reported comfort with BB decreased among our study population by 6 months. It is not possible to know what factors specifically account for this attrition, although it is plausible that the temporal distance from the training intervention plays an important role and could be mitigated by refresher courses, as suggested by survey results. We have attempted to mitigate recall bias of participant self-reported experience with BB by prospectively evaluating the clinical uptake of this technique in the PED following course delivery. We found that the experience reported by participants was corroborated by the sustained parallel increase in both the documented number of BB procedures and the diversity of physicians using this technique at 6 months and beyond. Importantly, the multimodal training course offered has not been externally validated. However, to our knowledge, no other BB training course has been described previously, and we have used consensus-based guidelines and best-evidence practice recommendations to guide course content.Reference Kam, Kavanagh and Yoong 13 - 16 Finally, our study did not assess patient-centered and orthopedic quality measures in the post-implementation period. Although these outcomes are beyond the scope of the current study, they remain an important area of future research.
CONCLUSIONS
We have described a novel multimodal training course, which increased participant comfort with BB for forearm fracture reduction and was associated with an increased use of this technique in clinical practice. At present, BB is not routinely employed for closed fracture reduction in the PED setting. Course administration achieved the goal of increasing knowledge of this technique and promoting conditions conducive to change in clinical practice. The course design allowed skill acquisition without patient risk, and with the benefit of repeated trials in a safe learning environment. It is our recommendation and hope that this novel training course be adapted to implement the BB at other institutions to support the safe adoption of an effective alternative to PS for forearm fracture reductions. Future work should be directed at assessing orthopedic and patient-centered outcomes following BB-assisted fracture reductions.
Acknowledgements
The authors wish to thank Rami Rezk, Gabrielle Allard, Elise Mok, and Albert Ho for technical assistance, as well as the McGill University’s Steinberg Centre for Simulation and Interactive Learning and the Whistler Health Care Centre’s staff and leadership.
Competing interests: None declared.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2016.392







