Introduction
Emergency tourniquet application to arrest hemorrhage in major limb trauma, particularly in the military context, has been shown to be a life-saving manoeuvre.Reference Kragh, Beebe and O’Neill 1 – Reference Kragh, Littrel and Jones 3 Due to the potential for significant complications (including clots, myonecrosis, pain, palsy, abscess, blisters, contusions, abrasions, renal failure, compartment syndrome, and amputation)Reference Kragh, O’Neill and Walters 4 and the paucity of evidence of its role in the non-military context, controversy persists regarding tourniquet use. We describe a civilian case in which improvised tourniquets were applied to an extremity for 17 hours following a penetrating lower limb injury in a remote area of Quebec.
Case Report
A 38-year-old man was involved in a shooting in a small remote Quebec village. The patient sustained a gunshot wound to the left thigh at 8:15 pm and was immediately transported to the community clinic where a nurse applied compression over the bleeding wound. Following application of the dressing, medical consultation was sought over the phone from a physician of a nearby village. The nurse was instructed to apply a tourniquet proximal to the bleeding wound and a pressure dressing. Because the first tourniquet (a leather belt) failed to control the bleeding, another improvised tourniquet (a seatbelt) was placed distal to the first one. The two tourniquets were in place by 8:30 pm, and hemostasis was achieved.
At 9:15 pm, the patient’s hemodynamic status deteriorated (blood pressure 90/50 mmHg, heart rate 113 beats/min). Because no blood products were available, the patient was administered crystalloids. At 10:20 pm, the trauma team leader at our institution was contacted by the local physician in the closest village, and, at 2:30 am, the local physician had arrived at the patient’s bedside with blood products. Due to continued hemodynamic compromise and agitation, the patient was intubated, started on a norepinephrine infusion, and administered five units of packed red blood cells and three units of fresh frozen plasma. The left lower extremity distal to the tourniquets was reportedly cold, cyanotic, and edematous, at this time. The patient responded to fluid resuscitation, and the norepinephrine was gradually weaned.
The patient was transported from the remote village to the nearest community hospital, arriving at 6:00 am. The first venous blood gas measurement showed a pH of 6.91, pCO2 of 51 mmHg,HCO310 mEq/L, lactate 8.5 mmol/L, and hemoglobin 122 g/L. At 8:30 am, the repeat venous blood gas measurement showed pH 7.15, pCO2 54 mmHg, HCO3 18 mEq/L, base excess of −9.2, and lactate 6.2 mmol/L. At 9:00am, the patient was transported by fixed-wing air ambulance to our tertiary trauma care facility, 1633 km away.
The patient remained hemodynamically stable during transport and arrived at our facility at 1:00pm. On arrival, the left lower limb was edematous, cold, cyanotic, and pulseless (Figures 1 and 2). A venous blood gas measurement showed pH 7.41, pCO2 29 mmHg, HCO3 18 mEq/L, lactate 2.1 mmol/L, hemoglobin 112 g/L, and an international normalized ratio of 1.27. Plain radiography of the pelvis and left femur did not show a bullet or fracture. The patient was immediately taken to the operating theatre, and both tourniquets were sequentially removed (total tourniquet time was more than 17 hours). The leg appeared to be demarcated at the knee joint down. Therefore, the femoral artery and vein were suture-ligated just above the knee, and an above-knee amputation was undertaken. Then, the two tourniquets and pressure dressings were removed, and anterior and posterior thigh penetrating wounds were identified. A counter incision was made at the injury site on the medial aspect of the thigh. The femoral superficial artery and vein were transected approximately half of their circumferences. Both vessels were oversewed. After this, complete hemostasis was achieved. The patient was transferred to the intensive care unit and treated with hemofiltration for rhabdomyolysis (serum creatine kinase 103,649 IU/L). The patient subsequently made an uneventful recovery and was transferred to a rehabilitation centre.

Figure 1 The patient lower limbs on arrival at our trauma center. Note the “paramedic belt” used as an improvised tourniquet. Part of the leather belt used as another improvised tourniquet can also be seen.

Figure 2 Anatomic cross section of the left thigh. The two wounds are illustrated.
Discussion
This case illustrates the potential use of tourniquets as a life-saving measure in civilian settings. It also highlights the challenges faced by local health care providers in remote locations.
To control exsanguination, tourniquets have been used for centuries. Since World War II, their utility in the military context has suggested a role in the civilian, prehospital context. When compared to manual compression, the advantages of tourniquets are 1) relative ease of application, 2) freedom for the medical provider’s hands to perform other tasks, and 3) provision of more reliable pressure over time. There exist inherent disadvantages: 1) interference with both arterial and venous circulation, 2) risk of nerve injuries and skin necrosis, and 3) limb ischemia and possible reperfusion injury if in situ for a prolonged period of time.
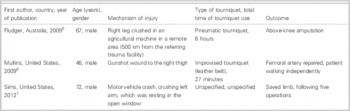
A review of tourniquet use in the civilian prehospital setting during the last 5 years identified three prior case reports (Table 1). Fludger and BellReference Fludger and Bell 5 described a civilian case with a prolonged tourniquet time: a 67-year-old man who sustained an above-knee amputation after his right foot was caught in an agricultural machine. A pneumatic tourniquet was applied until the patient was transported by helicopter to the referring trauma centre 500km away. On arrival, the limb was clearly not salvageable. The tourniquet had stayed in place for 6 hours.
Table 1 Result of MEDLINE search via PubMed—civilian use of the prehospital tourniquet
Recent literature from the military environment includes a case-control retrospective study of military casualties with significant traumatic injury to an extremity during Operation Freedom in Iraq by Beekley et al.Reference Beekley, Sebesta and Blackbourne 8 They identified 67 patients who arrived at the hospital with prehospital tourniquets and did not find a survival benefit, although they reported that 85% of the tourniquets had achieved hemostasis. The relatively short tourniquet time (average of 70 minutes) may explain, in part, the absence of any adverse effects of tourniquet use in their report. Kragh et al.Reference Kragh, O’Neill and Walters 4 conducted an observational study over 1 year in Iraq and included 499 patients with tourniquet placement either in the prehospital setting or emergency department (86% v. 14%). The overall survival rate was 87%, and survival was higher with prehospital tourniquet application (89% v. 78%) and with application before onset of shock (96% v. 4%); 1.5% of patients sustained palsies at the level of the tourniquet, and 0.4% had a major limb shortening secondary to the tourniquet. A prospective observational study in Afghanistan identified that 97% of the military tourniquets applied prior to hospital arrival were deemed indicated and that 94% had been placed correctly.Reference Lairet, Bebarta and Burns 9 In 2012, the Eastern Association for the Surgery of Trauma Guidelines made the use of tourniquet a level-3 evidence when compression measures are not able to control the bleeding.Reference Fox, Rajani and Bokhari 10 Finally, in the ninth edition of the Advanced Trauma Life Support (ATLS) book, the American College of Surgeons Committee on Trauma states that, in the context of major arterial bleeding, “the judicious use of a tourniquet may be helpful and life-saving.” 11
Recently, this committee published guidelines for prehospital tourniquet use, based mostly on data from military studies. The committee made a strong recommendation (quality of evidence: moderate) for the use of tourniquets in the prehospital setting for the control of significant extremity hemorrhage if direct pressure is ineffective or impractical.Reference Bulger, Snyder and Schoelles 12 There are no absolute contraindications to tourniquet placement. Improvised tourniquets tend to apply pressure unevenly and often have sharp edges. These increase the risk for underlying tissue injury and may partially occlude arterial flow and increase venous pressure, which may increase hemorrhage.Reference Doyle and Taillac 13 Examples of suboptimal improvised tourniquets include belts and similar straps, elastic bandages, or sphygmomanometer cuffs. We believe that commercial tourniquets should be used when available because they are easy to apply in less than 1 minute and are not prone to loosening. Tourniquets should be placed 5–8 cm above the most proximal bleeding wound and should never be placed over an articulation or an impaled object. Based on pneumatic tourniquet use in elective orthopaedic surgery, tourniquet times less than 2 hours are generally safe.Reference Wakai, Winter and Street 14 , Reference Lee, Porter and Hodgetts 15 In the military context, tourniquet times longer than 4, or sometimes even 8, hours has not necessarily resulted in amputation.Reference Kragh, Walters and Baer 16 – Reference Kragh, Baer and Walters 19 Although no guidelines exist regarding the safe duration of tourniquet application, we recommend that tourniquets be removed as soon as possible.
If used for a prolonged period, the use should be reassessed frequently (every 30 minutes). Unless the patient is still hemodynamically unstable, the situation is unstable, or insufficient personnel are available, direct pressure or pressure dressing can be applied to the wounds and the tourniquets released but left in place. If significant bleeding reappears, the tourniquet can be retightened.
Tourniquets should be removed in a controlled and monitored setting, especially after prolonged application. Before removal, physicians should be cognizant of the possibility of a sudden cardiovascular collapse attributed to reperfusion and the release into the systemic circulation of toxic cytokines.
Conclusion
Tourniquet use in civilian prehospital setting remains highly debated, but it may be life-saving. In the case reported here, two improvised tourniquets were needed to control a hemorrhage but at the cost of an above-knee amputation.
Competing interests: None declared.





