CLINICIAN'S CAPSULE
What is known about the topic?
The Herreros bladder stimulation technique to obtain clean-catch urine is effective in approximately 50% of infants <6 months of age.
What did this study ask?
What was the impact of using point-of-care ultrasound (POCUS) prior to clean-catch collection in infants regarding the success rate of the procedure?
What did this study find?
This study found no benefit of using POCUS before attempting stimulated urine clean-catch sampling in infants.
Why does this study matter to clinicians?
Implementation of POCUS for clean-catch collection would have limited usefulness to improve the success rate of the procedure.
BACKGROUND
Urinary tract infection is the most common serious bacterial infection in febrile infants.Reference Shaikh, Morone, Bost and Farrell1 Until recently, urethral catheterization and suprapubic aspiration were considered the standard methods of obtaining urine samples from children who are not yet toilet trained, but these techniques are invasiveReference Robinson, Finlay and Lang2,Reference Roberts3 and painful.Reference Kozer, Rosenbloom and Goldman4,Reference El-Naggar, Yiu and Mohamed5 A new, quick, and safe technique to obtain clean-catch urine has recently been described for newborns.Reference Herreros Fernández, González Merino and Tagarro García6 This procedure involves combining fluid intake and non-invasive bladder stimulation manoeuvres, repeated until micturition starts. In previous studies, success rates for this technique varied with age ranging from 86% (<1 month)Reference Herreros Fernández, González Merino and Tagarro García6 to 58% (0–3 months)Reference Labrosse, Levy, Autmizguine and Gravel7 and around 25% (3–24 months).Reference Tran, Fortier and Giovannini-Chami8 This technique's low success rate in older children is a limitation to its use in the emergency department (ED). The original stimulated clean-catch urine technique described by Herreros et al. recommended a 25-minute delay after an obligatory feeding period prior to stimulation that could delay urine collection and increase the risk of voiding during the waiting period.Reference Herreros Fernández, González Merino and Tagarro García6,Reference Herreros, Tagarro and García-Pose9,Reference Herreros, Tagarro and García-Pose10
A potential reason for failure to obtain urine using the stimulated clean-catch procedure may be an empty bladder. Previous studies reported that emergency point-of-care ultrasound (POCUS) could identify infants for whom urinary catheterization was unlikely to be successful.Reference Milling, Van Amerongen and Melville11 Two other studies showed that the use of POCUS significantly improved success rates of bladder catheterization.Reference Chen, Hsiao, Moore, Dziura and Santucci12, Reference Witt, Baumann and McCans13 Accordingly, performing a POCUS prior to a stimulated clean-catch urine sampling could potentially increase the success rate by identifying children who have an empty bladder and require a feeding period prior to collection.
To our knowledge, there has been no study evaluating whether a POCUS-based clean-catch urine collection protocol improves success rates compared with standard bladder stimulation manoeuvres. The primary objective of this study was to evaluate if a POCUS-guided feeding protocol prior to stimulated clean-catch urine collection increases the rate of success of the procedure by 20% in children aged less than six months who need a urine sample, compared with children for whom POCUS was not used.
METHODS
Study design and population
This was a randomized controlled trial. Recruitment occurred between August 2016 and June 2017 at the ED of a tertiary care pediatric hospital with an annual census of more than 80,000 patient-visits.
All infants less than six months of age, who needed a urinalysis and/or urine culture according to the attending ED physician, presenting to the ED during the working hours of the research assistants were eligible for recruitment. Patients with any medical condition in which obtaining a clean-catch urine sample was impossible (e.g., urostomy and anuria for 24 hours), any serious illness or unstable infant (e.g., sepsis), any medical situation in which the infant could not be fed, and inability to obtain parental informed consent were excluded from the study.
The study protocol has been registered on the clinicaltrials.gov website (study number: NCT02751671).
Intervention
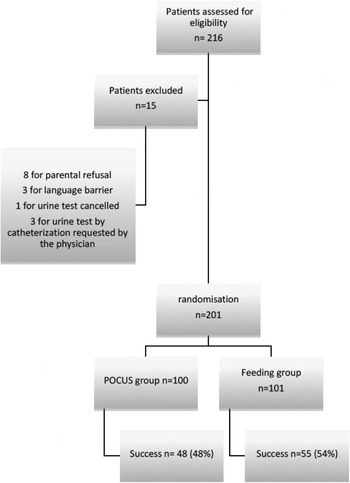
All participants were randomized into either a POCUS group or a mandatory feeding group. In the feeding group, a 20-minute feeding period (breastfeeding or formula) was enforced prior to clean-catch urine, as suggested in the publication of Labrosse et al.Reference Labrosse, Levy, Autmizguine and Gravel7 In the POCUS group, a clean-catch urine procedure was performed (without a feeding period) only if the transverse diameter of the bladder measured was ≥2 cm (Figure 1). If the bladder diameter was <2 cm, a 20-minute feeding period was enforced prior to a second POCUS. A stimulated clean-catch urine procedure was performed if the bladder diameter measured ≥2 cm at the second POCUS. If not, a second and last 20-minute feeding period was permitted prior to a third POCUS. A clean-catch urine procedure was performed following the third POCUS regardless of the bladder diameter. The genital areas of the infant were cleaned prior to the POCUS, and the research assistant was ready to collect urine if the child voided during the ultrasound exam.
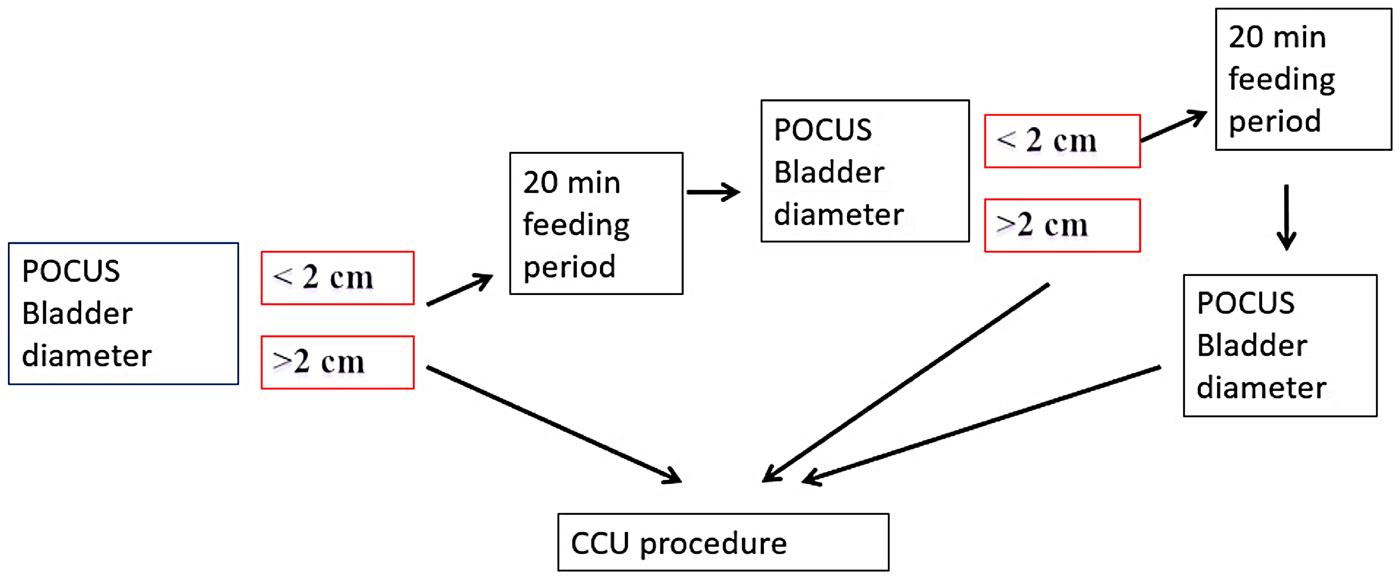
Figure 1. Intervention diagram for study procedure in POCUS group.
Two studies on POCUS prior to catheterization suggested that a transverse bladder measurement of less than 2 cm corresponded to a bladder volume of less than 2.5 cm.Reference Roberts3,Reference Witt, Baumann and McCans13,Reference Riccabona, Nelson, Pretorius and Davidson14 Consequently, the author of these studies suggested postponing catheterization until a repeated measurement reached or exceeded a transverse measurement of 2 cm.
In both groups, infants underwent clean-catch urine manoeuvres as described by Herreros Fernández et al.Reference Herreros Fernández, González Merino and Tagarro García6 Examiners alternated between bladder stimulation manoeuvres, which consisted of gentle tapping in the suprapubic area at a frequency of 100 taps per minute for 30 seconds and lumbar paravertebral massage manoeuvres for 30 seconds. The two stimulation manoeuvres were repeated until micturition began or for a maximum of 300 seconds. Clean-catch urine samples were collected in sterile wide-mouth containers.
Outcome measures and independent variables
The primary outcome was the rate of successful clean-catch urine sample collection. Success was defined by the collection of a sample of urine of at least 2 mL, obtained within 300 seconds of bladder stimulation manoeuvres, while cleansing, or again during POCUS prior to the manoeuvres. Secondary outcomes were times to collect the urine sample: from randomization to sample collection (T1); from the beginning of the manoeuvres to sample collection (T2); and the total time the research assistants spent with the patients (T3). We also aimed to determine the transverse bladder dimension associated with at least an 80% success rate for the procedure. Independent variables measured as a potential confounder were age, sex, low oral intake, and voiding in the previous hour.
Randomization
Allocation was based on a 1:1 ratio. An independent statistician generated the randomization scheme using a computer-generated sequence with blocks of variable sizes. To maintain blinding, the randomization allocation of each participant was concealed in an opaque envelope that was opened only following signature of the informed consent.
Study procedure
Before initiating the study, research assistants were trained to measure the transverse bladder diameter by a pediatric emergency physician with considerable experience using POCUS. The research assistants were one fellow in pediatric emergency medicine, two nurses, and one medical student. This training consisted of a 15-minute standardized theoretical training session, followed by supervised POCUS of the bladder in five children younger than six months of age. All sonographers were deemed able to measure the bladder width according to the experienced practitioner (MPD) before patient recruitment. Research assistants were experienced and trained to perform stimulation manoeuvre techniques as described by Herreros Fernández et alReference Herreros Fernández, González Merino and Tagarro García6 because they collaborated in a previous study.Reference Labrosse, Levy, Autmizguine and Gravel7
After obtaining parental informed consent, multiple variables were collected including demographics, feeding, and clinical characteristics. Patients were then randomized to their study group. Transverse bladder dimensions were measured for patients in the intervention group. Time was measured by a research assistant using a digital chronometer.
Data analysis
Data were entered in an Excel database (Microsoft Inc., Richmond, WA) and analyzed using SPSS, v24 software (IBM Software Group Inc.). To assess the adequacy of randomization, randomized patients were compared between arms for baseline sociodemographic characteristics. The primary analysis compared the proportion achieving success between the two groups. Secondary analyses compared the delay in obtaining the urine sample from randomization to sample collection (T1); the stimulation time required to obtain the sample in participants in whom success was achieved (T2); and the time spent by the research assistants with the patient to obtain the sample (T3). Another secondary analysis was the correlation between the transverse bladder diameter and success. For exploratory purposes, predictive factors of success were assessed using a multivariate logistic regression. These factors were identified a priori as age, sex, low oral intake, and voiding in the previous hour. A 95% confidence interval (CI) was calculated for each measurement. An intention-to-treat analysis was carried out for all analysis.
The sample size was calculated based on a previous study demonstrating a success rate of 49% for clean-catch urine technique in children aged less than six months in our setting.Reference Labrosse, Levy, Autmizguine and Gravel7 To assess the minimal difference that would be considered clinically significant; we surveyed 23 pediatric emergency physicians. The main consensus of this survey suggested that an improvement of 20% would be clinically significant enough to change the current practice and use POCUS before clean-catch urine. Since this was the first study on POCUS involving a clean-catch urine technique, there was no evidence to support specific increases in success rates that would be beneficial for use in other institutions. Based on this, and assuming β=0.8 and α=0.05, a total of 188 patients were necessary for recruitment. Expecting a very low proportion of loss to follow-up, we planned to recruit a total of 200 children.
RESULTS
Between August 2016 and June 2017, a urine sample specimen was ordered for a total of 216 children in the presence of research assistants. Among those, 201 (93%) patients were recruited, with 100 in the POCUS group and 101 in the obligatory feeding group. All completed the study (Figure 2). The main reason for non-inclusion was parental refusal to participate. No patient was lost to follow-up during the study period, and no patient was excluded from the analysis. The study population included 104 boys and 97 girls, with a median age of two months (Table 1). Although parents reported that children had low oral intake prior to the procedure in 54%, only 2% seemed to be dehydrated according to the physician in charge. In addition, 64% of the children had voided in the hour prior to the procedure.

Figure 2. Flow diagram for the study cohort.
Table 1. Baseline characteristics

IQR = interquartile range.
*Unless stated otherwise.
A total of 110 (55%) infants provided a urine sample within five minutes of the stimulation procedure, including 103 (51%) who provided an adequate quantity of urine. The procedure was equally successful in the POCUS group (48 of 100 patients; 48%) and feeding group (55 of 101 patients; 54%) (difference 6.5%, 95% CI -7.3 to 19.8%). In the intervention group, eight patients voided during POCUS, but the quantity of urine caught was ≥2 mL in only four patients.
The mean time to collect a urine sample from randomization to sample collection (T1) was similar in the POCUS group (11.9 minutes) compared with the feeding group (16.7 minutes) (difference 4.8 minutes, 95% CI -1.0 to 10.6 minutes). The time from the beginning of the manoeuvres to sample collection (T2) did not differ significantly (93 seconds [POCUS] v. 121 seconds [feeding group], difference 28 seconds, 95% CI -7 to 62 seconds). The time spent by the research assistant with the patient (T3) for the procedure was also similar in both groups (9.0 minutes [POCUS] v. 7.8 minutes [feeding group], difference 1.2 minutes, 95% CI -0.2 to 2.2 minutes). (Table 2). However, 36 of the 101 children randomized to the feeding group had been fed recently when the research assistant came for consent. Consequently, the 20-minute post-feeding period was considered already ongoing at randomization, and this decreased the delays in that group.
Table 2. Outcomes

CI = confidence interval; T1 = delay in obtaining the urine sample from randomization to sample collection; T2 = stimulation time required to obtain the sample in successful participants; T3 = time spent by the research assistants with the patient to obtain the sample.
*n = 50 for group 1 and 55 for group 2.
Only 12 of the 100 patients did not reach the two-centimetre bladder diameter size upon the first POCUS. Of those, 9 of the 12 attained the mandatory two-centrimetre bladder size after the second feeding period, and 3 of the 12 needed three feeding periods. Fifty percent (6 of 12) was finally achieved success.
A univariate logistic regression analysis showed that for each one-centimetre increase in bladder size, the odds ratio (OR) of a successful clean-catch urine increased by 1.22 (95% CI 0.58–2.56). After adjusting for age, the association remained non-significant (OR 1.44, 95% CI 0.67–3.17). For two patients, the bladder diameter was not documented because the child voided at the beginning of the ultrasound. The association between bladder size and success is graphically represented in Figure 3 (web appendix).
A secondary univariate logistic regression analysis (web appendix, Table 3) showed that success rates of the clean-catch urine procedure were significantly higher in the 0–29 day (OR 2.75, 95% CI 1.03–7.36) and 30–59 day (OR 3.59, 95% CI 1.67–7.69) age groups compared with children older than 89 days of life. The success rate in the 60–89 day age group was not different from that of the group older than 89 days (OR 1.43, 95% CI 0.66–3.12). Sex of the patient, low oral intake according to the parents, and last urine in the previous hour were not associated with the success rate of the procedure.
DISCUSSION
This study did not find that the use of POCUS improves the success rate of stimulated clean-catch urine manoeuvres in children less than six months of age. Children randomized to the POCUS group had no difference in time to obtain the urine specimen, as compared with the control group, and there was no impact on the nursing time involved in the procedure. Further, we failed to find an association between the bladder diameter and success rate. An important and unexpected finding in our study was the absence of a relationship between the bladder size and success rates. Unlike other urine sampling methods, success of the clean-catch urine procedure for children with a measured bladder size of >2 cm is probably more linked to the ability of the child to relax his or her sphincter than to the actual quantity of urine in the bladder. This procedure is based on manoeuvres described for patients with bladder dysfunctions to stimulate bladder emptying through reflex contraction of the detrusor muscle.Reference Prasad, Smith and Wright15 It probably also explains why this technique seems to be more effective in younger infants. Another interesting finding is that the 20-minute feeding period did not seem to be necessary prior to clean-catch urine manoeuvres to reach a bladder size of ≥2 cm. To save time in the ED, this 20-minute feeding period could be reserved only if the first clean-catch failed prior to a second attempt. This could be of potential interest and should be assessed in future studies.
The impact of a POCUS protocol seems different for clean-catch urine in comparison with both bladder catheterizationsReference Milling, Van Amerongen and Melville11–Reference Witt, Baumann and McCans13 and suprapubic aspirations.Reference Gochman, Karasic and Heller16, Reference Kiernan, Pinckert and Keszler17 These previous studies demonstrated an increased probability of success with POCUS. The use of a bladder scan is another potential choice; however, POCUS is increasingly available in most EDs.Reference Marin and Lewiss18 In addition, the success of clean-catch urine procedures seems to be unrelated to the bladder size.
LIMITATIONS
Our study had limitations. The relatively small sample size of our study may have underpowered our ability to detect differences between both groups that may be perceived as clinically significant to other institutions. Another limitation is that many children in the control group were already fed at randomization and did not wait 20 minutes for further feeding. This may have biased results toward a smaller difference in delays for the two groups. Finally, the study was conducted at a single site, and only four research assistants were involved in measuring the bladder size. This small number of POCUS users allows for reduced interrater variability but limits the generalizability of the study. Further, these research assistants had variable experience in POCUS.
CONCLUSION
Our study did not demonstrate any benefit in using a POCUS algorithm to improve the success rates of stimulated clean-catch urine. Assuring a bladder size of >2 cm with POCUS prior to stimulated clean-catch urine had no clinical impact on success rates in our study population. In addition, our study confirms that a stimulated clean-catch urine procedure is effective in about one-half of infants younger than six months of age. Finally, a feeding period may be unnecessary prior to the first clean-catch urine collection attempts and could be reserved for patients requiring a second attempt. Future studies should explore this issue further.
Acknowledgements
The study team would like to thank Maryse Lagacé, RN, and Ramona Cook, RN, for their contribution to the data collection and coordination of the research assistants.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.30
Competing interests
None.