CLINICIAN'S CAPSULE
What is known about the topic?
Early access of trauma patients to trauma centres and definitive care improves patient outcomes.
What did this study ask?
This study examines risk factors for non-optimal air transport of trauma patients via a provincial air medical transport organization.
What did this study find?
Nursing station as a sending facility, advance/primary care paramedics, and transport between 08:00 and 00:00 were risk factors for non-optimal transport.
Why does this study matter to clinicians?
These risk factors can be studied to attempt to minimize them and decrease time to definitive care for trauma patients.
BACKGROUND
Early access to definitive care at a lead trauma centre has been shown to improve patient outcomes.Reference MacKenzie, Rivara and Jurkovich1–Reference Nolan, Tien and Sawadsky5 The use of air ambulance has become an integral part of many trauma systems and helps alleviate geographic barriers to rapid trauma centre access. Although the literature regarding the mortality benefit of air ambulance is mixed, there are multiple studies showing improved patient outcomes in the Canadian system.Reference Haas, Stukel and Gomez4–Reference Thomas, Wisham, Clemmer, Orme and Larsen11 Speed is often cited as the greatest benefit of air medical transport; however, multiple studies have shown improved outcomes despite no time benefit.Reference Brown, Gestring and Guyette7,Reference Taylor, Stevenson and Jan8 These studies suggest a higher level of care that includes advanced procedures such as airway management, blood transfusion, and vasopressor use in conjunction with expedited transfer to trauma centres as part of this benefit.Reference Chen, Gestring and Rosengart6–Reference Taylor, Stevenson and Jan8,Reference Thomas, Wisham, Clemmer, Orme and Larsen11
There are several reasons why a severely injured patient may initially be brought to the non-trauma hospital, including inappropriate triage and identification of injuriesReference Brown, Forsythe, Stassen and Gestring12,Reference Lehmann, Arthurs and Cuadrado13 ; also, there may not be a trauma centre within an acceptable safe distance to transport. Patients initially brought to a non-trauma centre undergo an interfacility transfer to be taken to a specialized trauma centre for advanced care. Air ambulance services play an integral role in facilitating the interfacility transport. Delays during the interfacility transfer process resulting in delays to definitive care can have negative impacts on patient outcomes.Reference MacKenzie, Rivara and Jurkovich1−Reference Nolan, Tien and Sawadsky5 Previous studies have identified modifiable delays to interfacility transfer including the sending physician doing a procedure, waiting to meet a land emergency medical service (EMS) crew, and delays for diagnostic imaging.Reference Nolan, Tien and Sawadsky5
Often, there are times when the closest aircraft or most optimal type of resource (i.e., fixed wing or rotor wing) for transport is unavailable. This can occur for multiple reasons such as the optimal resource being already busy with another patient transport or is unavailable because of weather or maintenance.Reference Nolan, Tien and Sawadsky5 When a non-optimal resource is used, there is an inherent delay to the transport of that patient; as such, there may be critically ill or injured patients who deteriorate as a result of this delay.
The objective of this study was to identify patient-, institutional-, and paramedic-level characteristics associated with non-optimal resource utilization for injured adult patients undergoing emergent interfacility transfer to a trauma centre. A better understanding of patient, institutional, and paramedic characteristics that have non-optimal resource utilization may assist with targeted interventions to reduce any delays and expedite transfer of injured patients to definitive care.
METHODS
Setting
Ornge is the sole provider of air ambulance and critical care transport in Ontario, Canada. Ornge operates a total of 12 bases, 9 of which operate fixed- or rotor-wing aircrafts (Figure 1). Ornge provides service to more than 14 million people over an area of operations that spans more than one million square kilometres. Ornge transports injured patients to and from a multitude of health care facilities varying from nine tertiary trauma centres to small remote nursing stations. Most nursing stations are serviced by fixed-wing resources and have longer transport times, often more than 1–2 hours each way and require a land ambulance transport from the landing site to the nursing station. Ornge has the largest fleet of air ambulances in Canada and includes eight fixed-wing Pilatus Next Generation PC-12 airplanes and 12 Leonardo AW-139 helicopters. In addition, Ornge operates 13 Crestline Commander land ambulances. Aircrafts are staffed with two paramedics and two pilots. A transport medicine physician is also available and provides online medical control using direct telecommunication with paramedics. Paramedic staff include critical care paramedics, who are trained to administer vasopressors, blood products, and sedation, as well as to provide complex interventions including intubation, needle thoracostomy, and cricothyrotomy.

Figure 1. Map of Ontario showing Ornge fixed- and rotor-wing bases.
Study design
This was a retrospective cohort study of data collected in an internal Ornge database. Ethics approval was given by the Sunnybrook Health Sciences Research Ethics Board.
Study participants
Patients were identified from an Ornge database over a five-year period from January 1, 2013, to December 31, 2017. Patients were included as outlined below (Figure 2). All adult (aged 18 years and older) patients who underwent emergent interfacility transport for traumatic injuries during this time period were assessed for inclusion. Patients were excluded from the study if they were under 18 years of age, were transported for medical reason, were an urgent or non-urgent priority, were transported by an aircraft that was mobile at the time of request, or had an optimal resource determined to be a land resource.
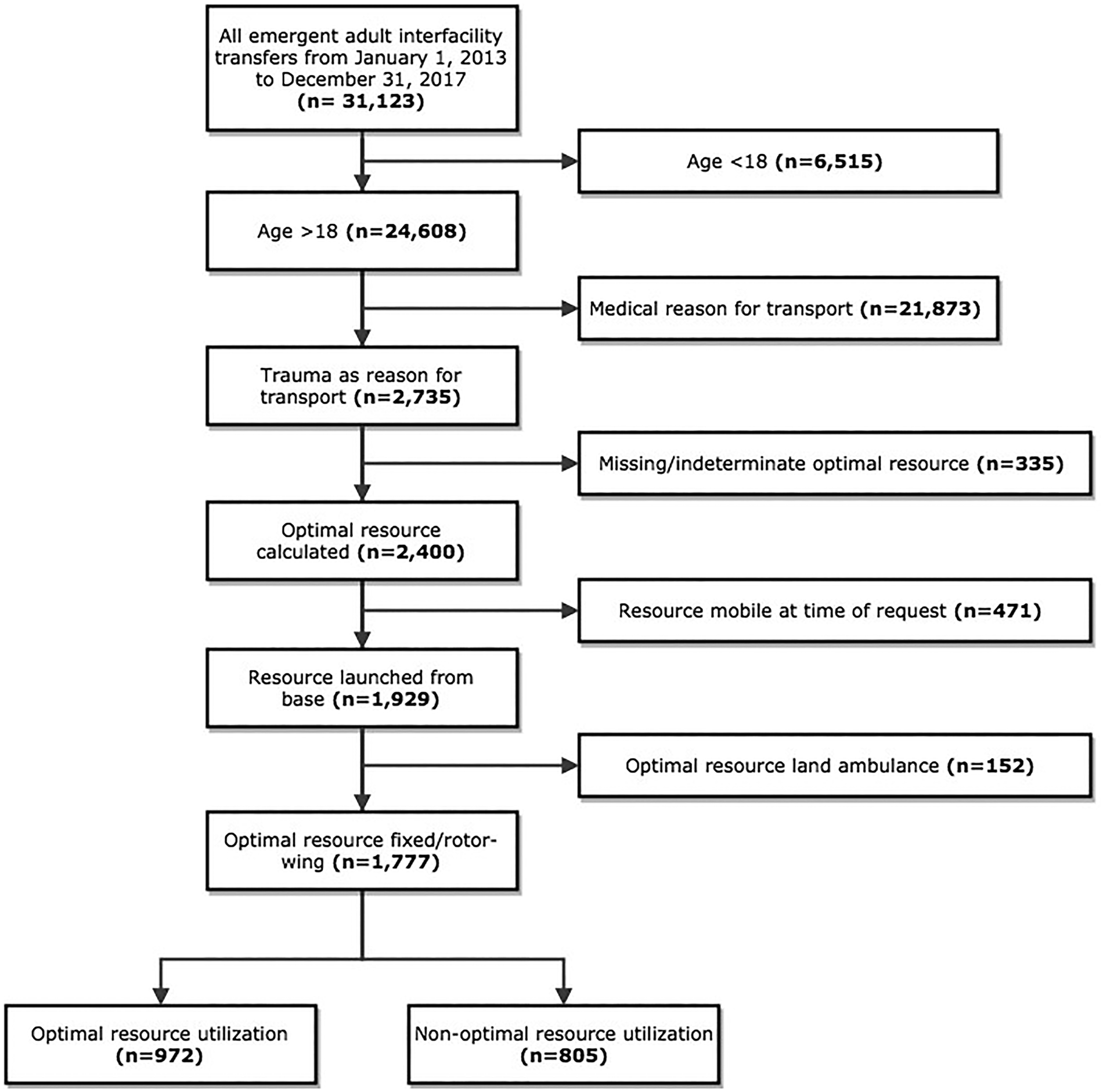
Figure 2. Cohort creation.
Data sources
Data were collected from two health administrative databases at Ornge. The first database used, Flight Vector, contains all information related to sending and receiving facilities, dispatch times, vital signs at time of request to transport, reason for transport, and patient age and sex. The second database used was the electronic patient care record (ePCR), which is a computerized charting system for the paramedics. Data captured in this database include patient's vital signs while under the care of paramedics, interventions done by paramedics, time to complete patient transport, reason for transport, and a narrative text of the patient transport. Classification of a resource as optimal or non-optimal was done using time data collected in Flight Vector. This is further described below.
Patient, institutional, and paramedic characteristics that were examined included: age, sex, transporting base (name), sending facility/hospital (name), date and time of transport request, date and time paramedics arrive at patient bedside, season of transport, time of transport (day, evening, and night), vital signs on arrival of paramedics, and paramedic interventions (intubation, vasopressor use, cardiopulmonary resuscitation [CPR], and blood transfusion). Additionally, classification of sending facility (academic, community >100 beds, community <100 beds, and nursing station) was done by manually identifying the number of beds available at each sending hospital.
Defining optimal resource
The process of defining optimal resource utilization is outlined in Figure 3. All possible interfacility transfers were determined using the study cohort by grouping all patient transfers that had identical sending and receiving facilities.

Figure 3. Optimal resource utilization categorization.
A unique resource was defined as a specific type of aircraft (rotor or fixed wing) that was attached to a specific base; however, multiples of the same type of aircraft within a single base were considered one resource. For example, in the Thunder Bay base, there are two fixed-wing resources and a single rotor-wing resource. In these methods, there was a distinction between fixed-wing and rotor-wing resources, but two fixed-wing resources were considered the same “unique resource” for this methodology. Then, each unique resource that transported the sending-receiving pair was identified. Resources were considered unique if they differed in base or mode of transport (rotor wing, fixed wing, or land). For each unique sending-receiving pair, estimated transfer times for each resource were calculated using a modular method by breaking down the total time to definitive care into intervals based on the major steps of the transfer process.Reference Giang, Donmez, Fatahi, Ahgari and MacDonald15 The median times for these intervals was then calculated and summed for each unique resource. The fastest resource was the one that had the minimum sum of medians. This modular process of the sum of median time intervals has been used in previous studies to estimate optimal resource use for air ambulance services.Reference Giang, Donmez, Fatahi, Ahgari and MacDonald15 Furthermore, the same methodology has been used internally at Ornge as a decision support tool to aid planning of resource utilization.
The optimal resource was determined to be the fastest asset (rotor-wing, fixed-wing, or land ambulance) from the closest base. If the distance between sending and receiving was less than 100 km and the mean time difference between land and air resources was less than 10 minutes, then the fastest land resource was considered the optimal resource. These distance cut-offs are used internally at Ornge for flight planning and resource allocation. If the resource that serviced the transfer was mobile at the time of call request, it was removed from the study cohort since time comparisons would be unreliable without an accurate acceptance location. If an optimal resource was determined to be a land resource, they were removed from the final study cohort.
Statistical methods
Descriptive statistics
Descriptive statistics were used to assess the distribution for all variables of interest in each group. Continuous factors were assessed for normality by evaluating kurtosis and skewness and are summarized as means and standard deviations (SD) or medians and interquartile range (IQR) for normal and non-normally distributed data, respectively, and categorical variables are displayed as counts and percentages.
Unadjusted bivariate analyses were performed to assess differences between patients with a non-optimal transfer strategy and patients with an optimal transfer strategy. Continuous variables were compared using the independent samples Student's t-test for normally distributed variables and Wilcoxon rank-sum test for non-normally distributed variables. Categorical variables were compared using the Chi-square test. Two-sided p-values were reported in all cases, and p-values <0.05 were considered significant for all analyses.
Risk factors associated with non-optimal resource use
Patient, institutional, and paramedic characteristics were examined to assess association with non-optimal resource use. These included patient age, sex, vital signs (heart rate, respiratory rate, systolic blood pressure, Glasgow Coma Scale [GCS], and oxygen saturation), ventilator dependence, sending facility type, season, time of day, and paramedic level of care. As this model was exploratory, there was no single key predictor variable; thus, all the above characteristics were all assessed for possible inclusion in the final model. A backward selection technique using a p-value cut-off of 0.2 was used to determine which variables to include in the final analysis.
An adjusted logistic regression model was used to explore factors associated with a non-optimal transfer strategy. Patients with any missing data for one or more of the predictor variables of interest were excluded from the final model. Missing data resulted in exclusion of <5% of observations. Lastly, a generalized estimating equation (GEE) logistic regression model accounting for clustering by sending facility was performed.
Assumptions for logistic regression were then assessed, including adequate model fit and absence of influential observations. Model fit was assessed with c-statistic. Multicollinearity was assessed using a variation inflation factor (VIF) of four as the cut-off for exclusion. A 50-50 split sample technique comparing difference in c-statistics was used to assess internal validity.
All statistical analyses were conducted using SAS Studio, version 3.4 (SAS Institute, North Carolina, USA).
Missing data
All data were reviewed for completeness and to ensure there were no implausible values. If the optimal resource was missing or unable to be calculated or if the resource was mobile at the time of transfer request, they were removed. Lastly, if the optimal resource was deemed to be a land resource, they were also removed from further analysis.
RESULTS
There were a total of 31,123 adult emergent interfacility transports with Ornge between January 1, 2013, and December 31, 2017. Of these, 24,608 were older than 18 years of age, with 2,735 of those being trauma patients. Of these patients, a total of 1,777 had fixed- or rotor-wing transport as their optimal method, with 972 receiving optimal transport and 805 receiving non-optimal resource use (Figure 2).
The patients receiving optimal resource use were older, with a median age of 48, as compared with 45 (Table 1). A higher percentage of patients who underwent optimal resource utilization were mechanically ventilated, as compared with those who underwent non-optimal resource utilization (24.4% v. 17.4%, respectively) and had a GCS of less than 8 (30.3% v. 24.2%, respectively).
Table 1. Baseline characteristics of study cohort

IQR = interquartile range; Missing = values missing in original dataset.
*Student's t-test
Wilcoxon rank sum
‡Chi-square
An adjusted logistical regression model accounting for clustering by sending facility was used to determine which factors were associated with higher odds of non-optimal transport (Table 2). Patients being transported from a nursing station had higher odds of non-optimal resource use, as compared with an academic centre (odds ratio [OR] 1.94). Transport with primary or advanced care paramedics had a higher odds of non-optimal resource use, as compared with critical care paramedics (OR 6.57 and 1.44, respectively). As compared with time of transport between 00:00 and 08:00, both daytime (08:00–17:00) and evening (17:00-00:00) times of transport had higher odds of non-optimal resource use (OR 1.40 and 1.54, respectively). There was no significant difference in OR for age, sex, need for mechanical ventilation or time of year.
Table 2. Adjusted logistic regression models of odds of having non-optimal transfer strategy with and without accounting for clustering by sending facility

CI = confidence internal; OR = odds ratio; ref = reference category.
Only 32.9% of patients transported from a nursing station were brought directly to a trauma centre for assessment, as compared with more than 90% of all transports from academic and community hospitals. Most of the time patients transported from a nursing station were transported to a facility with computed tomography (CT) scanning capabilities if they were not transported to a trauma centre. Patients transported from academic and community centres who were not transported to a trauma centre were transported to centres with neurosurgical capabilities for isolated head injuries. The median delay to arrival to receiving facility if a patient had a non-optimal resource use was 40 minutes (IQR 18–47 min).
DISCUSSION
Multiple studies have shown that early transport of trauma patients to definitive care improves patient outcomes.Reference MacKenzie, Rivara and Jurkovich1–Reference Haas, Stukel and Gomez4,Reference Baxt, Moody and Cleveland16–Reference Doucet, Bulger and Sanddal18 In Ontario, air ambulance covers a massive land mass, with the majority of tertiary centres in its southern region.Reference Baxt, Moody and Cleveland16,Reference Galvagno, Haut and Zafar17 Previous studies have examined when delays occurred during transport for the various types of Helicopter Emergency Medical Services transports of trauma patients; some of the major delays included weather, refueling and mechanical checks, and procedures at the sending facility and land EMS transport to the sending facility from the aircraft.Reference Nolan, Tien and Sawadsky5 Our study adds to this existing literature by identifying patient-, institutional-, and paramedic-level factors associated with non-optimal resource use.
In our study, resource was defined as a two-level variable: originating base and category of aircraft (fixed wing v. rotor wing). Further, the variable “category of aircraft” was not independent of the variable “base,” as certain bases had only specific categories of aircraft. Thunder Bay has two fixed-wing aircrafts and one rotor-wing aircraft; Timmins and Sioux Lookout operate only one fixed-wing aircraft each. Kenora, Toronto, London, Sudbury, Ottawa, and Moosonee operate only a rotor-wing aircraft.
Our study identified three factors associated with non-optimal resource use to emergent interfacility transfer of injured patients by air ambulance: size of sending facility, paramedic level of care, and time of day.
The type of sending facility was associated with non-optimal resource use. In comparison with academic centres, patients being transferred from nursing stations had a higher odds of non-optimal resource use. This is likely multifactorial. Many of the nursing stations in Ontario are remote, with long distances and, thus, long transport times for patients undergoing interfacility transport. Because of this, once an asset is engaged in transporting a patient, it is likely to be unavailable for a number of hours to complete that initial patient transport. As this resource would then be unavailable to transport another patient during this period, a non-optimal resource would be deployed. Furthermore, most nursing stations are further north and more prone to inclement weather than southern Ontario. It is possible that a non-optimal resource was deployed as it was able to transport that patient as the optimal resource was unable to do so because of weather conditions along that route.
A non-optimal resource was used for 45% of all emergent interfacility transports. Advanced and critical care resources are limited across the province, with the same resources being used to transport emergent transports (i.e., going for life-saving interventions or higher-level care) and non-urgent transports (i.e., repatriation to closer hospital with no escalation of care). Currently, if there are no emergent transports pending, advanced and critical care resources are deployed to service these non-urgent transports when they require a higher level of care during transport. These non-urgent transports may prevent an asset from being available to transport an emergent patient, resulting in a non-optimal resource being used. One strategy to mitigate this may be to reserve advanced and critical care resources for emergent transports only. This could be done by not sending an available resource on a non-urgent transport if it is the only resource available in a select area of the province. Additionally, partnering with local hospitals to send nurse escorts to provide a higher level of care during transports may allow patients to be transported with primary paramedic crews safely, again allowing for advanced and critical care paramedics to prioritize emergent patient transports.
Not all patients were transported directly to a trauma centre. As mentioned earlier, some injured patients are transported for advanced diagnostic imaging such as a CT scan that is unavailable at their current health care facility. For many of these patients, it may be reasonable to have them transported for a CT scan at a non-trauma centre to assess them for significant injuries rather than transport them all directly to a trauma centre to avoid overburdening the regional trauma centre.
Time of day was also associated with optimal resource use with transports between 08:00–17:00 and 17:00–00:00 having more non-optimal transports. This may be because of fewer new transports booked overnight, resulting in higher aircraft availability and optimal resources being assigned.
There were several limitations for our study. The first being that this was a retrospective study that can often lead to missing data and exclusion of participants. Because of the retrospective aspect of our analysis, we were unable to determine the location of a resource at the time a transfer was requested unless that resource was at the base. Therefore, if a resource was mobile at the time of request, we were unable to include these transfers in our study as we could not reliably identify whether they would have been the optimal resource. Another limitation of this study was that we were unable to identify the specific reasons why a non-optimal resource was used. Unfortunately, the databases used do not provide reason for resource assignment or make note of inclement weather or mechanical or staffing issues. Lastly, our data was limited to a prehospital database; we are unable to report other variables of interest such as severity of illness or injuries identified. This also limited our ability to explore the impact of non-optimal resource use on in-hospital outcomes and mortality. However, it can be inferred from the literature that severely injured patients have increased mortality when they experience delays to definitive care and transport to a trauma centre.Reference MacKenzie, Rivara and Jurkovich1–Reference Haas, Stukel and Gomez4
CONCLUSION
In conclusion, there were three factors associated with non-optimal resource use to emergent interfacility transfer of injured patients by air ambulance. These included the size of sending facility, paramedic level of care, and time of day. Further research is required to explore specific causes of non-optimal resource use of air ambulance and to assess for any impact on patient-centred outcomes.
Acknowledgements
Meetings presented at: Canadian Association of Emergency Physicians Annual Conference 2019.
Competing interest
None.







