CLINICIANS CAPSULE
What is known about the topic?
Patients with atrial fibrillation and flutter (AFF) and an underlying condition are at risk of iatrogenic events.
What did this study ask?
Can a decision tool identify ED AFF patients with underlying illness early in the evaluation?
What did this study find?
Of patients with potential underlying illness, 93% arrive by ambulance; present with chest pain, dyspnea, or weakness; or have CHA2DS2-VASc > 2.
Why does this study matter to clinicians?
Physicians have a decision tool to evaluate undifferentiated AFF patients for underlying illness.
INTRODUCTION
Atrial fibrillation accounts for 0.5% of Canadian emergency department (ED) visits.Reference Atzema, Austin, Miller, Chong, Yun and Dorian1 A proportion of these patients will have an acute underlying illness,Reference Atzema, Lam and Young2,Reference Scheuermeyer, Pourvali and Rowe3 and the use of dysrhythmia-specific therapies such as rate or rhythm control is associated with a higher risk of adverse outcomes along with a low rate of success. In 416 ED atrial fibrillation and flutter (AFF) patients with an acute underlying condition (32% sepsis, 28% heart failure, 11% acute coronary syndrome), physicians administered rate or rhythm control in nearly one-third, and the median time of administration was 90 minutes after registration,Reference Scheuermeyer, Pourvali and Rowe3 illustrating that, in many cases, rate or rhythm control was likely administered before completion of diagnostic investigations.
Identification of such high-risk patients early in the ED assessment remains a challenge, and unfortunately there is little evidence to assist clinicians. The Canadian Association of Emergency Physicians 2018 guidelinesReference Stiell, Scheuermeyer and Vadeboncoeur4 recommend that these patients be identified and treatment directed at the underlying cause. Both patients and physicians would benefit from a tool to rapidly identify such patients: if a patient was deemed high-risk, physicians should investigate for the presence of an underlying illness, rather than administering early AFF-specific therapies.
We sought to develop a decision aid that could quickly identify undifferentiated ED AFF patients who might have an acute underlying illness, who would then merit further investigations to confirm or refute this illness. We also sought to describe patients the decision had missed and ascertain how they could have been identified.
METHODS
Study design and setting
This was a health record review at two Canadian university-affiliated teaching EDs whose setting and patients have been previously described.Reference Scheuermeyer, Pourvali and Rowe3,Reference Scheuermeyer, Grafstein and Stenstrom5–Reference Scheuermeyer, Grafstein and Heilbron7 St Paul's Hospital is an inner-city referral center with 70,000 annual ED visits and comprehensive cardiology services, while Mount St Joseph's Hospital is a community ED with 25,000 yearly visits and a general medicine ward. The University of British Columbia ethics review approved this study. During the study period, emergency physicians managed AFF patients at their discretion.
Patient selection
This dataset has been previously described.Reference Scheuermeyer, Pourvali and Rowe3 We identified all ED patients who with AFF identified on an electrocardiogram (ECG) from January 1, 2009, to December 31, 2009. ECGs are generally performed in any patient with chest pain, palpitations, a history of arrhythmia, syncope or dizziness, weakness, or dyspnea, and in any patient over 50 with abdominal complaints. Every ECG was stored in the MUSE (GE Healthcare Clinical Systems, Waukesha, WI, USA) database, and cardiologists confirmed results within 24 hours. We retained the patients’ unique identifier, date, and time of acquisition, and conducted a structured chart review of the ED encounter. We excluded patients with cardiac arrest, ST-elevation myocardial infarction, or stroke symptoms, because these require non-AFF related management; those with cardiac procedures in the prior 7 days because cardiac specialists typically direct care; those referred for direct admission; those from out-of-region because no follow-up was available; and those evaluated solely for adjustments to anticoagulation.
Data collection
The sites share an electronic database that records patient demographics, arrival mode, triage level,Reference Beveridge, Ducharme, Janes, Beaulieu and Walter8 chief complaint,Reference Grafstein, Unger and Bullard9 and initial vitals, and the results of all ED and hospital investigations, consultations, and discharge summaries.
Health record review
We adhered to accepted methodological criteria for health record reviews.Reference Worster, Bledsoe and Cleve10 Two emergency physicians and two final-year medical students, blinded to study hypotheses and outcomes, independently abstracted records onto electronic spreadsheets, documenting vital signs, comorbidities, and all ED-based laboratory testing and imaging. We trained reviewers on the first 10 health records and they submitted data at regular intervals, which were examined for obvious errors. We clarified missing or discrepant data by looking for clinic visits, ED visits, hospitalizations, discharge summaries, laboratory testing, and procedures back to 1999. We recorded conflicting information and reconciled this at regular meetings. An independent reviewer blinded to the first abstraction assessed a random 10% of records, and we calculated inter-rater reliability for the variable “prior AFF.”
Outcomes
The a priori outcome was the presence of an acute underlying medical illness. Separate from the above analysis, two emergency physicians also blinded to study hypothesis and outcomes independently reviewed charts to identify patients with an acute underlying medical illness. We defined the following acute underlying conditions a prioriReference Scheuermeyer, Pourvali and Rowe3,Reference Scheuermeyer, Grafstein and Stenstrom5–Reference Scheuermeyer, Grafstein and Heilbron7 (Appendix 1): sepsis (including pneumonia), acute coronary syndrome, acute decompensated heart failure, pulmonary embolism, exacerbation of chronic obstructive pulmonary disease, thyrotoxicosis, hypertensive emergency, acute valvular disease, hypothermia, acute renal failure, or acute bleeding. Characteristics that defined the presence of an acute underlying condition had to be present during the ED encounter, so a medical event or diagnostic abnormality occurring days later would not constitute an acute underlying illness. In case the two emergency physician reviewers did not agree whether there was an underlying illness, the health record was referred to two additional physicians, a cardiologist and a hematologist, who were unaware of study hypothesis or outcomes, for adjudication of underlying illness and the diagnosis. If the two adjudicators could not agree, the primary investigator provided the final determination.
Model development
We collected potential predictor variables including demographics (age, sex, ambulance arrival) presenting complaints and timing, initial vital signs, and comorbidities, including prior AFF, hypertension, diabetes, acute coronary syndrome, stroke, and vascular disease. Given that our decision aid should be useful early in the ED evaluation, and that patients did not undergo standardized investigations, we omitted all diagnostic testing from the model.
We calculated the unadjusted odds ratio for underlying illness versus no underlying illness. We used a data-splitting approachReference Arboretti and Salmaso11 and randomly used 75% of the dataset to fit the model (derivation set) and 25% for the validation set. From the derivation set, we developed multivariable logistic regression models to predict the presence or absence of acute underlying illness using the following potential predictor variables: ambulance arrival, time in AF (either greater or less than 48 hours), presenting complaint (palpitations, chest pain, dyspnea, weakness, other), arrival heart rate, systolic and diastolic blood pressure, CHA2DS2-VASc scoreReference Lip, Nieuwlaat, Pisters, Lane and Crijns12 (this incorporates age and sex), and pre-existing comorbidities (prior AFF, hypertension, diabetes, prior acute coronary syndrome, stroke, or vascular disease). We compared models by stepwise forward selection and retained only those with an adjusted odds ratio (aOR) of >2.0. We calculated sensitivity and specificity, predictive values, and likelihood ratios, all with 95% confidence intervals (CIs). We also assessed the receiver-operating characteristic curve and used the Hosmer-Lemeshow goodness of fit test to calculate model performance.
Model evaluation
After model development, we assessed performance of the decision aid using area under the receiver-operating characteristic curve (AUC) as the measure of interest. We used bootstrapping with 1,000 resamples to obtain a fitting and validation distribution of all AUC values.
We also analyzed the data using different cutoffs of the CHA2DS2-VASc score. Finally, we conducted the same analysis in the subgroup of patients with an initial heart rate >100 beats per minute, because these patients are more likely to undergo rate or rhythm control and, therefore, potentially be more at risk for treatment-related adverse events.
Data analysis
We used Microsoft Excel 2008 (Microsoft Corp, Redmond, WA, USA) for data entry, and R (R Foundation for Statistical Computing, Vienna, Austria) for analysis. We reported discrete variables as percentages and presented continuous variables as means with standard deviations if normally distributed, or medians with interquartile ranges (IQR).
RESULTS
We collected 1,083 ED AFF patients with 400 (36.9%) having an acute underlying medical illness (Figure 1). For the chart review, inter-rater agreement was 0.74 (95% CI, 0.70–0.79) for the variable of “prior atrial fibrillation.” Overall, 23/1,083 patients (2.1%) required adjudication to ascertain “underlying illness”; the primary investigator was required for final determinations in five patients.

Figure 1. Study flow diagram.
Patients with an acute underlying medical illness were older; more likely to arrive by means of ambulance; more likely to have a chief complaint of chest pain, dyspnea, or weakness; to have altered vital signs; and to have cardiovascular comorbidities. New AFF diagnoses were made in 42.2% and 35.6% of patients with and without underlying illness, respectively (Table 1).
Table 1. Patient characteristics stratified by presence of acute underlying illness (n = 1083)

CHA2DS2-VASc = stroke risk stratification score (Congestive heart failure, Hypertension, Age, Diabetes, Stroke, Vascular disease, Sex, where age is 0, 1, or 2 points, stroke is 2 points, and female is 1 point); EMS = ambulance; eGFR = estimated glomerular filtration rate; Hb = hemoglobin; TSH = thyroid stimulating hormone.
For the clinical investigations, the first line is the number of patients in each group who had the investigation, and the second is the number of abnormal investigations. Crude ORs are calculated for both having the test performed (and cannot be obtained if zero or all patients had a test, or if zero or all test results were normal) and for an abnormal result. “Signs of ischemia” is new onset ST-segment elevation, or ST-segment depression, or new T-wave inversions, or dynamic ST-segment changes during sequential ECG.
Univariate analysis showed the strongest potential predictor variables were ambulance arrival (aOR, 3.5; 95% CI, 2.6–4.7); chief complaint of weakness, chest pain, or dyspnea (aOR, 4.7; 95% CI, 3.2–7.0); no prior history of AFF (aOR, 1.2; 95% CI, 0.9–1.5); prior history of hypertension (aOR, 4.0; 95% CI, 2.9–5.8), heart failure (aOR, 6.4; 95% CI, 4.1–10.0), diabetes (aOR, 2.7; 95% CI, 1.8–4.4), vascular disease (aOR, 2.9; 95% CI, 1.9–4.5), or stroke (aOR, 2.8; 95% CI, 1.8–5.0).
The most accurate derived multivariable predictive model combined ambulance arrival (aOR, 3.5; 95% CI, 2.6–4.7) and presenting complaint of chest pain, weakness, or dyspnea (aOR, 4.7; 95% CI, 3.2–7.0) and CHA2DS2-VASc score greater than 2 (aOR, 4.6; 95% CI, 2.9–7.0) (Table 2). This model was 93% sensitive (372/400; 95% CI, 91–96%) and 54% specific (366/683; 95% CI, 50–58%) for identifying patients with acute underlying illness. The positive predictive value was 0.54 (95% CI, 0.50–0.58), negative predictive value was 0.93 (95% CI, 0.90–0.95), positive likelihood ratio was 2.0 (95% CI, 1.8–2.2), and negative likelihood ratio was 0.13 (95% CI, 0.09–0.18) (Table 3). The Hosmer-Lemeshow goodness of fit was 0.16, and the AUC was 0.79.
Table 2. Performance of decision aid
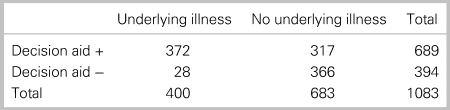
Table 3. aORs in the final model

CHA2DS2 – VASc =; A composite measure of stroke risk; the constituent variables are age, sex, hypertension, diabetes, heart failure, stroke, and vascular disease. Note that age, hypertension, diabetes, heart failure, stroke, and vascular disease were significant in the univariate analysis and incorporated into this single risk score.
For assessment of model performance over 1000 iterations, the AUC fitting had a median of 0.79 (IQR, 0.77–0.81) and AUC validation had a median of 0.79 (IQR, 0.72–0.85). Changing CHA2DS2-VASc cutoffs provided the following results. A score > 1 had a sensitivity of 95% (95% CI, 92–97%) with specificity of 48% (95% CI, 43–53%). A score > 3 had a sensitivity of 89% (95% CI, 86–92%) with specificity of 60% (95% CI, 56–64%). In both cases, the AUC was 0.77 (IQR, 0.75–0.79).
Among 541 patients with initial heart rate ≥ 100 beats per minute, 185 (34.2%) had an underlying illness. The above model had an aOR of 3.7 (95% CI, 2.4–5.7) for ambulance arrival; an aOR of 7.9 (95% CI, 4.4–14.5) for presenting complaint of weakness, chest pain, or dyspnea; and an aOR of 4.0 (95% CI, 2.3–6.9) for CHADS-VASC > 2. This model was 87% sensitive (161/185; 95% CI, 83–92%) and 66% specific (235/356; 95% CI, 61–72%) for identifying patients with acute underlying illness. The positive predictive value was 0.57 (95% CI, 0.51–0.63), negative predictive value was 0.91 (95% CI, 0.88–0.95), positive likelihood ratio was 2.6 (95% CI, 2.2–3.0), and negative likelihood ratio was 0.19 (95% CI, 0.13–0.28). The Hosmer-Lemeshow goodness of fit was 0.49, and the AUC was 0.84.
Overall, of the 28 (7.0%; 95% CI, 4.7–10.0%) patients in whom the model was falsely negative, 8 had sepsis, 7 had a gastrointestinal bleed, 5 had acute heart failure, 2 each had thyrotoxicosis, an acute coronary syndrome, and an acute kidney injury, and 1 had a pulmonary embolus. All 28 patients were identified with a combination of basic physical examination, simple blood testing, and chest radiography (Appendix 2).
DISCUSSION
In 1,083 consecutive ED patients with AFF, with nearly 40% having an acute underlying illness, we demonstrate that a parsimonious decision aid based upon presentation characteristics and comorbidities can identify most patients at high risk of an underlying illness within minutes of assessment. Our decision aid missed few patients, and straightforward testing identified these within an hour of assessment. The subgroup of tachycardic patients showed similar results. This assists emergency physicians by providing a reliable aid to quickly select patients who may be at high risk of an acute medical illness from a cohort of undifferentiated ED AFF patients. Given that the presence of an acute underlying illness is likely a relative contraindication to AFF-specific therapies, such as rate and rhythm control,Reference Scheuermeyer, Grafstein and Stenstrom5 our decision aid should allow clinicians to consider diagnostic investigations in potentially high-risk patients before empirical AFF therapies.
These high-risk patients were acknowledged in the 2018 CAEP guidelinesReference Stiell, Scheuermeyer and Vadeboncoeur4 as a critical early decision node. The consensus expert opinion identified risk factors for an acute underlying illness, including permanent AF; prescription for oral anticoagulants; absence of prior cardioversion; a heart rate less than 150 beats per minute; or presenting symptoms of fever, dyspnea, or pain. Our study confirms the importance of some of these and provides clinicians with a tool to help identify these potentially high-risk AFF patients within minutes of arrival.
The few patients our decision aid incorrectly labeled as having no underlying illness were all identified early in the ED evaluation through physical findings, including fevers or rectal examination, basic laboratory investigations, or plain chest radiography. All tests should be routinely available and quickly available in any ED, ensuring that most patients can undergo timely investigations before administration of AFF-specific therapies.
This review at two urban Canadian sites may not be applicable elsewhere and the proportion of AFF patients with an acute underlying illness may vary. While presenting complaints are standardized,Reference Lip, Nieuwlaat, Pisters, Lane and Crijns12 inter-rater reliability is unknown. Because emergency physician-directed testing was instrumental in defining an acute underlying diagnosis, both ascertainment or incorporation bias must be considered, although the direction of bias is unclear and the overall number of affected patients may be small. We did not include diagnostic testing because our goal was to construct a decision rule applicable early during the ED evaluation.
Seven percent of the patients were misclassified by the rule, but rather by basic laboratory and imaging tests within the first hour of ED evaluation. The retrospective nature of the study, as well as the data analysis, ensures that an external validation will likely underperform this model. We were unable to test our decision aid directly against physician judgment.Reference Schriger, Elder and Cooper13 However, given that the same dataset reported that physicians used rate or rhythm control in 135/416 patients with underlying illness, often shortly after arrival,Reference Scheuermeyer, Pourvali and Rowe3 we propose that our decision aid may assist physicians in more careful selection of patients with potential underlying illness before administration of AFF-specific therapies.
CONCLUSION
We have developed a decision tool with sensitive criteria for identifying AFF patients who may have acute underlying condition and who should undergo further evaluation before empiric administration of rate or rhythm control.
We suggest the following clinical approach: First, there is a very small group of unstable AFF patients who require immediate conversion.Reference Stiell, Scheuermeyer and Vadeboncoeur4 However, the vast majority of ED AFF patients could be stratified upon initial assessment. Patients with none of the high-risk criteria we have identified (EMS arrival, chest pain, dyspnea or weakness presentation, CHA2DSReference Atzema, Lam and Young2-VASc > 2) are unlikely to have an underlying condition and may be appropriate for rate or rhythm control. Patients meeting any high-risk criteria should be investigated to rule out underlying causes. The brief delay required to obtain these investigations is unlikely to adversely impact outcomes.
Acknowledgements
We thank Clare Heslop, MD, PhD, Reza Pourvali, MD, and Jan McPhee, MD, MSc, for collecting data diligently. We thank Brett Heilbron, MD, and John Ward, MD, for providing adjudication. Dr. Barrett is supported in part by a Center for Disease Control research grant through the Tennessee Department of Health. Dr. Barrett consults for Red Bull GmbH,Fuschl am See, Salzburg, Austria. F.S. conceived the idea, designed the study, and composed the first draft. E.G. provided source data. M.N., F.S., and D.B. performed statistical analysis, while G.I., B.G., J.C., and especially T.B. provided critical editorial input.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.454.
Competing interests
None declared.






