Childhood obesity is a global epidemic affecting an estimated 124 million children worldwide(Reference Abarca-Gómez, Abdeen and Hamid1). Although it is well recognised that childhood obesity, as evaluated by BMI, increases the risk of developing CVD, hypertension and type 2 diabetes in adulthood; a growing body of research now indicates that abdominal obesity, particularly the accumulation of visceral adipose tissue (VAT), may be a stronger predictor of cardiovascular and metabolic disease risk than general BMI-defined obesity(Reference Kelishadi, Mirmoghtadaee and Najafi2–Reference Khoury, Manlhiot and McCrindle6). Furthermore, abdominal obesity can occur independently of BMI-defined obesity, meaning that akin to overweight and obese children; normal weight children with excess visceral adiposity are at a heighten risk of future morbidity and premature mortality(Reference Suliga4–Reference Khoury, Manlhiot and McCrindle6).
Diet is an important lifestyle factor known to influence body fat distribution. In this context, evidence indicates that Mediterranean dietary patterns may be protective against the development of abdominal adiposity(Reference Bacopoulou, Landis and Rentoumis7,Reference Romaguera, Norat and Mouw8) . However, in recent decades, there has been a distinct shift away from traditional eating habits in Mediterranean regions and increasingly, children are adopting a more Western diet characterised by an increased consumption of refined sugars, saturated fats and processed foods(Reference Grosso and Galvano9). Coinciding with this nutrition transition, children living in the Mediterranean regions of Southern Europe are now experiencing higher rates of abdominal obesity, even in the absence of an increased BMI(Reference Schröder, Ribas and Koebnick10–Reference Albuquerque, Nóbrega and Samouda12). As the accumulation of VAT begins in childhood and is an early predictor of future morbidity(Reference Staiano and Katzmarzyk13), there is a need to identify modifiable dietary habits in children that could account for the preferential distribution of fat in visceral depots.
Sugar-sweetened beverages (SSBs) are typical of the Western diet and may play a role in visceral fat partitioning, as recent studies in adults(Reference Odegaard, Choh and Czerwinski14–Reference Maersk, Belza and Stodkilde-Jorgensen17) and adolescents(Reference Shearrer, Daniels and Toledo-Corral18,Reference Mollard, Sénéchal and MacIntosh19) have reported a positive association between increased SSB consumption and VAT accumulation. To date, research regarding SSB consumption in children has typically explored associations with total adiposity; while there is now convincing evidence linking SSB consumption to weight gain and BMI-defined obesity(Reference Bleich and Vercammen20,Reference Frantsve-Hawley, Bader and Welsh21) , data on visceral adiposity remain scarce. Although a few studies in children have found SSB consumption to be positively associated with abdominal obesity(Reference Frantsve-Hawley, Bader and Welsh21–Reference Bigornia, LaValley and Noel24), these studies are limited by their use of waist circumference, which is unable to distinguish VAT from subcutaneous adipose tissue. As VAT is a stronger correlate of chronic disease risk than subcutaneous adipose tissue(Reference Staiano and Katzmarzyk13), it is important to discern whether SSB consumption is specifically associated with VAT in children.
Furthermore, while the associations between SSB consumption and general adiposity can typically be explained by an increase in energy intake, the mechanisms explaining visceral fat partitioning are lesser known. One possible mechanism may involve the stress hormone cortisol, a glucocorticoid secreted as a function of the hypothalamic–pituitary–adrenal (HPA) axis. Under basal conditions, cortisol secretion typically follows a diurnal rhythm; however, in response to psychological or physiological stressors, the HPA axis becomes hyperactive and cortisol secretion is increased(Reference Björntorp25). Dysregulation of the HPA axis and subsequent elevations in basal cortisol has been implicated in the aetiology of visceral obesity(Reference Björntorp25,Reference Anagnostis, Athyros and Tziomalos26) , and recent evidence suggests diets high in sugar may exacerbate this relationship, with work in overweight adolescents finding morning serum cortisol and high sugar intake interact to predict VAT accumulation(Reference Gyllenhammer, Weigensberg and Spruijt-Metz27). As SSBs are a major source of sugar among children(Reference Pawellek, Grote and Theurich28), it is possible that their consumption may increase VAT accumulation through mechanisms of HPA dysregulation. To date, only one study has explored the interrelationship between SSBs, cortisol and VAT. As such, the cross-sectional study by Shearrer et al. (Reference Shearrer, Daniels and Toledo-Corral18) found SSB consumption to be independently associated with cortisol and VAT in minority youth, but no interaction effects of SSB consumption and cortisol on VAT were observed. However, the study by Shearrer et al. (Reference Shearrer, Daniels and Toledo-Corral18) was limited by its small sample of overweight/obese minority youth and warrants repeating in a larger sample with a wider range of weight status. Therefore, in our study, we sought to assess the association between SSB consumption and body fat and whether sex and serum cortisol levels modified these associations in children.
Methods
Participants and design
The Healthy Growth Study was a large-scale, cross-sectional epidemiological study conducted from 2007 to 2009. The Healthy Growth Study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Ethics Committee of Harokopio University of Athens. The Greek Ministry of National Education also approved the study’s protocol. The study sample comprised 2665 schoolchildren aged 9–13 years old, attending the fifth and sixth grades of primary schools located in municipalities within Attica, Aitoloakarnania, Thessaloniki and Iraklio. The sampling of schools was random, multi-stage and stratified by parents’ educational level and total population of students attending schools within these municipalities. Specifically, the municipalities in the prefectures under study were divided into three groups on the basis of average educational level of their adult population (25–65 years old) that was estimated from data provided by the National Statistical Service of Greece (2001 census). Consequently, municipalities, proportional to the size of their population of children aged 9–13 years old, were randomly selected from each socio-economic level. Finally, a number of schools were randomly selected from each municipality, proportional to the population of schoolchildren registered in the fifth and sixth grades, according to data obtained from the Greek Ministry of Education. Written informed consent was obtained from all parents before data were collected. All participating children underwent a physical examination by an experienced paediatrician and children’s health status was assessed using a standardised checklist (see online Supplementary material 1). Additionally, information regarding children’s medical history was collected from their parents via a standardised questionnaire (see online Supplementary material 2). Further details describing the sampling procedure of the Healthy Growth Study are provided elsewhere(Reference Moschonis, Tanagra and Vandorou29).
Anthropometric and visceral fat mass data
Weight was measured to the nearest 0·1 kg using a SECA model 770 digital scale (SECA) and height was measured to the nearest 0·1 cm using a stadiometer (Leicester Height Measure; Invicta Plastics Ltd). BMI was calculated using the equation weight (kg) divided by height squared (m2), and children were categorised as underweight, normal weight, overweight and obese in accordance with the International Obesity Task Force cut-off points(Reference Cole, Bellizzi and Flegal30). The WHO 2007 Growth Reference macro package was used to calculate children’s BMI-for-age z-score(Reference de Onis, Onyango and Borghi31). Bioelectrical impedance analysis was used to determine abdominal VAT (VIScan AB-140; Tanita Corporation). In this simple, non-invasive method, a weak electrical current is passed between the regions near the umbilicus and spinal cord at the umbilicus level and the voltage generated in the lateral abdomen is recorded. Because the equipotential line that passes through visceral fat appears on the lateral abdominal surface, the amount of visceral fat can be estimated by measurement of the voltage generated at this location using a regression equation determined by computed tomography(Reference Ryo, Maeda and Onda32). Although imaging techniques, such as computed tomography and magnetic resonance imaging, are considered to be the gold standard for measuring VAT, these methods are highly expensive and involve radiation exposure(Reference Shuster, Patlas and Pinthus33). The bioelectrical impedance analysis method is therefore favourable for a sample of this size and age, and VAT estimated by bioelectrical impedance analysis has previously been shown to be highly correlated with VAT determined by computed tomography(Reference Ryo, Maeda and Onda32). In the 4 h prior to measurement, children were instructed to abstain from consuming food or liquid and from any intensive exercise. Children were also instructed not to wear any metallic object during measurement. Total VAT was read straight from the instrument in a rating scale of 1–59 units, reported to the nearest 0·5 increment.
Sugar-sweetened beverage consumption and dietary intake data
Data regarding dietary intake were collected for two consecutive weekdays and one weekend day via the 24 h recall method. Dietary intake recalls were analysed using the Nutritionist V diet analysis software (version 2.1, 1991; First Databank) which was extensively amended to include traditional Greek recipes and nutritional information of processed foods provided by independent research institutes, food companies and fast food chains. Mean values from the three 24 h recalls were used and daily energy intake was expressed as kJ. SSBs were defined as any beverage containing added sugar, namely sugar-sweetened soft drink and sugar-sweetened fruit juice, and consumption was measured in g/d. To align with prior research(Reference Shearrer, Daniels and Toledo-Corral18), grams were converted to fluid ounces and one serving of SSBs was defined as 8 oz (or 226·8 g). The WHO strongly recommends both children and adults limit the consumption of added sugars to less than twelve teaspoons (about 50 g) per d and suggests that a further reduction to less than six teaspoons (about 25 g) per d provides additional health benefits(34). As an 8 oz serving of SSBs typically contains approximately 25 g of added sugar, the children were classified into three SSB consumption categories, that is, low SSB consumption (<1 serving/d), medium SSB consumption (≥1 to <2 servings/d) and high SSB consumption (≥2 servings/d), the levels modelling this 25 g increase in daily added sugar intake.
Serum cortisol data
Blood samples were obtained in the morning between 08.30 and 10.30 hours following a 12-h overnight fast. Morning serum cortisol was measured by electrochemiluminescence immunoassay on the Roche Cobas e 411 analyzer (Roche Diagnostics SA). The lower and upper detection limits were 0·05 and 63·4 μg/dl, respectively.
Socio-demographic, physical activity and biological maturation data
Data on the level of parental education were collected from the parents (preferably from the mother) during face-to-face interviews. Maternal and paternal years of education were each stratified into three categories, that is, less than 9 years, which corresponds to having a junior high school degree; 9–12 years, which corresponds to having a high school degree; and more than 12 years, which corresponds to having a college, university or post-graduate education. Children’s physical activity was assessed via step count using a waist-mounted pedometer (Yamax SW-200 Digiwalker; Yamax Corporation), which they were instructed to wear for 1 week. Tanner stage, an index of biological maturation, was determined by female paediatricians, who thoroughly inspected breast development in girls and genital development in both girls and boys.
Statistical analysis
Continuous variables were expressed as mean values and standard deviations, and categorical variables were reported as frequencies and percentages. Student’s t test and χ 2 analyses were performed to evaluate differences in descriptive variables between boys and girls. Multivariate linear regression models were developed to assess the relationship between SSB consumption and VAT, BMI and BMI z-scores for the total sample. Both unadjusted models and models adjusted for sex, Tanner stage, daily energy intake, total daily steps and parental education status are presented. To explore effect modification, we first stratified all regression models by sex to understand whether the associations between SSB consumption and outcome variables are influenced by sex. We then fitted an interaction term between SSB and sex in all regression models for VAT, BMI and BMI z-scores and reported these interactions if they were statistically significant.
To adjust for the possible confounding effects of cortisol, serum cortisol level (μg/dl) was added as a continuous variable in all regression models. Serum cortisol levels were then recoded into tertiles based on its distribution within the total sample, and children were categorised as having low, medium or high cortisol levels if they were in the first, second or third tertile, respectively. We then conducted strata-specific analysis by these serum cortisol tertiles to assess the association of SSB consumption and VAT, BMI and BMI z-scores with adjustment for all possible variables. The results from the multiple linear regression models are presented as β-coefficients and 95 % CI. All statistical analyses were conducted using Stata (version 15.1, StataCorp) and the level of significance was set at P < 0·05.
Results
The sample was composed of 2665 children (50·5 % boys) attending the fifth and sixth grades of primary school. Ages ranged from 9−13 years, with a mean age of 11·2 (sd 0·7) years (Table 1). Of the total sample, 3·1 % of children were underweight, 55·1 % were normal weight, 30·3 % were overweight and 11·5 % were obese. Significant sex differences were found in regard to adiposity, with boys having a higher BMI, BMI z-score and visceral fat rating than girls. In addition, girls were found to have significantly lower cortisol levels and were more likely to be in Tanner stages 3–5 compared with boys. Regarding energy intake and expenditure, boys consumed more energy per d and were more physically active than girls. No significant sex differences were found in regard to socio-economic characteristics (maternal and paternal education).
Table 1. Descriptive characteristics of children by sex
(Mean values and standard deviations; numbers and percentages)
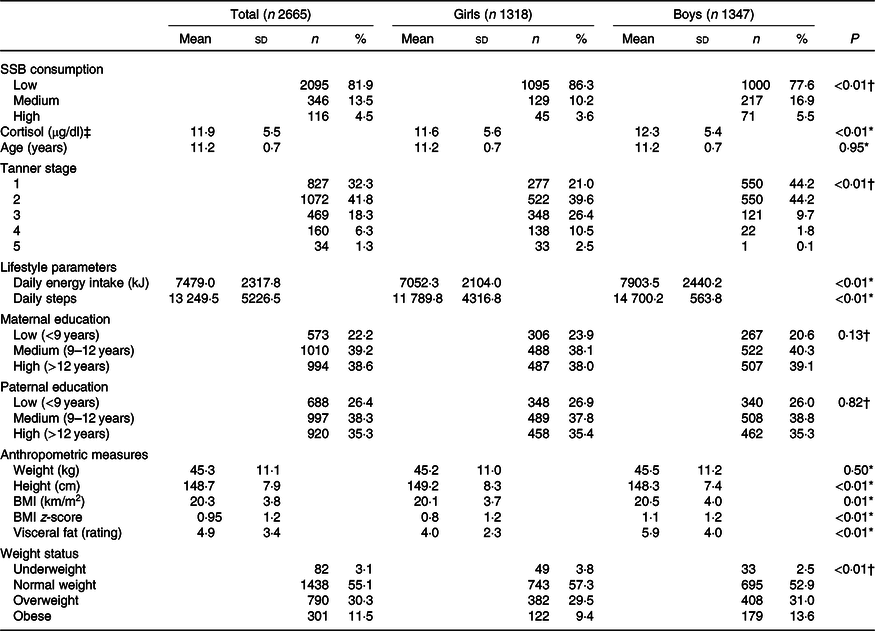
SSB, sugar-sweetened beverage.
* Derived from Student’s t test.
† Derived from χ 2 test.
‡ Cortisol values are presented in conventional units (μg/dl). To convert values to SI units (nmol/l), multiply by 27·6.
The majority of children (81·9 %) were categorised as having low SSB consumption, although boys were more likely than girls to be medium (62·7 v. 37·3 %) and high (61·2 v. 38·8 %) consumers of SSBs (P < 0·01; Table 1).
High SSB consumption was significantly associated with VAT but not with BMI or BMI z-scores (Table 2). High SSB consumers had a visceral fat rating 1·3 units higher than low consumers (95 % CI 0·3, 2·3, P = 0·01) and adjusting for covariates strengthened this relationship (β = 1·4, 95 % CI 0·4, 2·3, P = 0·01). In this model, sex, daily energy intake and physical activity were significantly associated with VAT (P < 0·01) as well as Tanner stages 2 and 3, and maternal education >12 years (P < 0·05). Sex was significantly associated with measures of adiposity in each model, with girls having significantly lower VAT, BMI and BMI z-scores compared with boys (P < 0·01, results not shown). Therefore, to assess for potential effect modification, models were stratified by sex (Table 2). While no significant associations were found between SSB consumption and measures of adiposity in girls, high SSB consumption in boys was significantly associated with VAT, but not BMI or BMI z-scores, in the adjusted model (β = 1·8, 95 % CI 0·3, 3·4, P = 0·02). In this model, the following covariates were significant: daily energy intake (P < 0·01), physical activity (P < 0·01), maternal education >12 years and paternal education 9–12 years (P < 0·05).
Table 2. Associations of sugar-sweetened beverage (SSB) consumption and measures of adiposity
(β-Coefficients and 95 % confidence intervals)
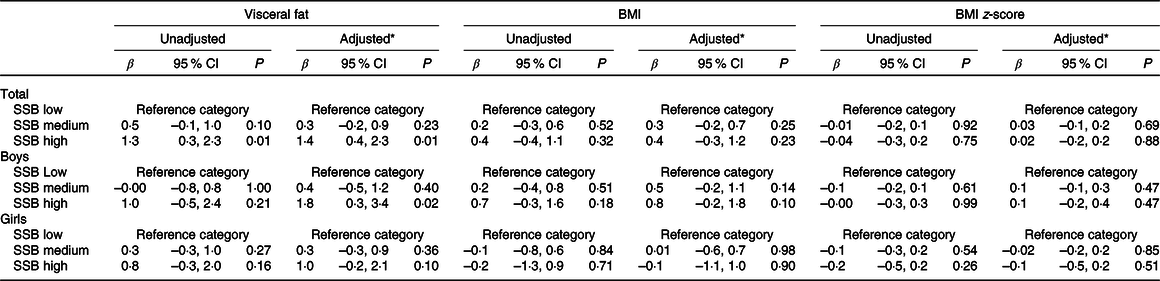
* Adjusted for sex (total sample only), Tanner stage, total daily energy intake, parental education and total steps per d.
After inclusion of cortisol in the models (Table 3), high SSB consumption remained significantly associated with VAT in the adjusted model (β = 1·3, 95 % CI 0·3, 2·3, P = 0·01), as did sex (P < 0·01), Tanner stage 3 (P < 0·01), daily energy intake (P < 0·01), physical activity (P < 0·01) and maternal education >12 years (P < 0·05). Although cortisol was not significantly associated with measures of general adiposity (BMI and BMI z-scores), an inverse association was found between cortisol and visceral adiposity, with every 1 μg/dl increase in cortisol predicting a –0·04 reduction in VAT (95 % CI –0·1, –0·0, P = 0·01). Converted to SI units, every 1 nmol/l increase in cortisol is associated a –0·001 reduction in VAT (95 % CI –0·003, –0·0003, P = 0·01; SI units are not presented in Table 3). The effects for the sex stratification remained the same after inclusion of cortisol as a covariate in the adjusted models (Table 3).
Table 3. Association between sugar-sweetened beverage (SSB) consumption, cortisol and measures of adiposity
(β-Coefficients and 95 % confidence intervals)
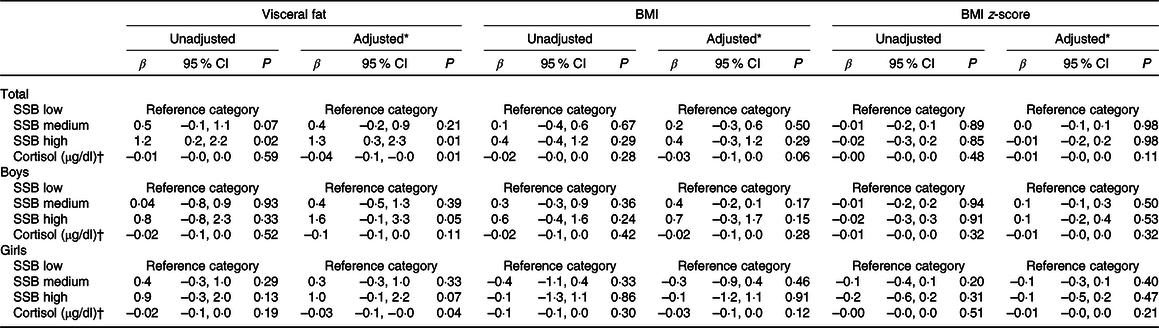
* Adjusted for sex (total sample only), Tanner stage, total daily energy intake, paternal education and total steps per d.
† Cortisol values are presented in conventional units (μg/dl). SI units (nmol/l) are not presented.
When the association between SSB consumption and measures of adiposity was stratified by cortisol levels (Table 4), it was found that high compared with low SSB consumption was associated with a greater VAT in children with low cortisol levels (β = 2·8, 95 % CI 1·0, 4·6, P < 0·01). For children with medium or high cortisol levels, no associations were found between SSB consumption and measures of adiposity.
Table 4. Association between sugar-sweetened beverage (SSB) consumption and measures of adiposity, stratified by serum cortisol levels
(β-Coefficients and 95 % confidence intervals)
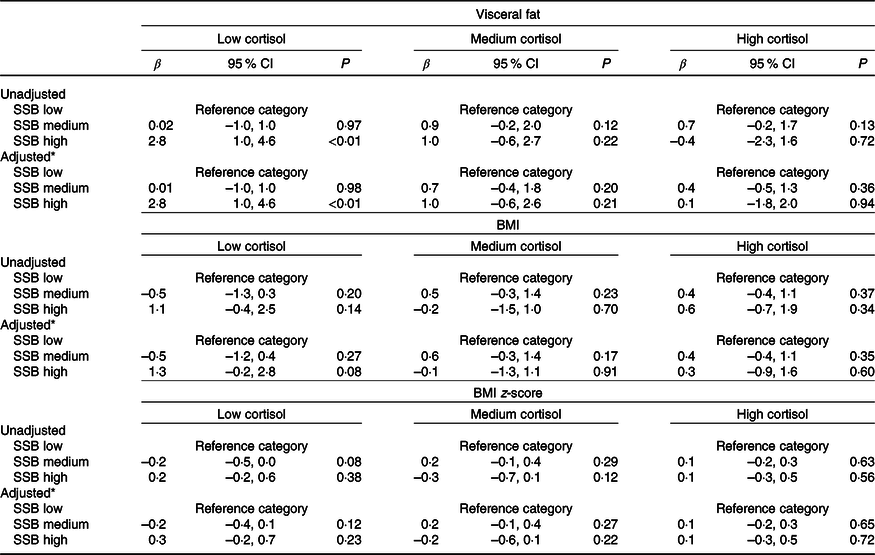
* Adjusted for sex, Tanner stage, total daily energy intake, parental education and total steps per d.
Discussion
Our findings suggest an association between high SSB consumption and visceral, but not general, adiposity, and this association was found to be stronger in boys. Furthermore, we aimed to investigate HPA dysregulation as a potential mechanism accounting for the association between SSBs and fat partitioning in visceral adipose depots. The results from our stratified analysis found high SSB consumption was only associated with VAT in children with low morning cortisol levels.
To date, much of the focus has been on the association between SSBs and general adiposity in children(Reference Bleich and Vercammen20,Reference Frantsve-Hawley, Bader and Welsh21) , but we found no association between SSBs and BMI or BMI z-scores. Although the majority of the literature supports a positive association, much of this research was conducted in US children with reportedly high SSB intakes(Reference Bleich and Vercammen20,Reference Frantsve-Hawley, Bader and Welsh21) . One other study in Greek schoolchildren also found a positive association between SSB consumption and BMI(Reference Papandreou, Andreou and Heraclides35); however, SSB consumption in their sample was similar to that reported in US children and was much higher than what was observed in the present study. It is therefore possible that consumption patterns are not high enough in our sample to have observable effects on general adiposity. Additionally, fewer than 20 % of children in our sample consumed more than one serving of SSBs per d, and so our analysis may have lacked sufficient power to detect a significant association in medium or high SSB consumers. Moreover, it has been argued that studies should not adjust for energy intake in their analyses, as energy is likely to mediate the association between SSBs and adiposity(Reference Hu36). However, even without adjustment for energy intake, we found no association between SSBs and general adiposity.
Nevertheless, SSB consumption patterns in our sample were sufficient to detect an association between SSB consumption and visceral adiposity, with our results showing that those consuming ≥2 servings of SSBs per d had a significantly greater visceral fat rating than those consuming <1 serving per d, even after adjustment for energy intake. Previous work investigating the relationship between SSBs and visceral adiposity has shown that increased SSB consumption is positively associated with VAT accumulation in adults(Reference Odegaard, Choh and Czerwinski14–Reference Maersk, Belza and Stodkilde-Jorgensen17) and adolescents(Reference Shearrer, Daniels and Toledo-Corral18,Reference Mollard, Sénéchal and MacIntosh19) ; however, the present study is the first to extend these findings to children. Moreover, our results are consistent with several studies demonstrating a positive association between SSB consumption and waist circumference in school-aged children(Reference Frantsve-Hawley, Bader and Welsh21–Reference Bigornia, LaValley and Noel24), and further support WHO recommendations to reduce added sugar intake to below 50 g/d(34).
Sex-stratified analyses revealed that the association between SSB consumption and VAT was stronger in boys. However, when an interaction term was included in the regression models, the results were not statistically significant and so additional studies are needed to replicate our findings. Nevertheless, one other study has examined sex differences in the relationship between SSBs and abdominal obesity in children(Reference Collison, Zaidi and Subhani22). In line with our findings, Collison et al. (Reference Collison, Zaidi and Subhani22) reported SSB consumption was associated with a higher waist circumference in Saudi school boys but not in girls. There are several possible interpretations to explain these sex differences. Firstly, it is well established that men accumulate more visceral fat than females, who typically store more fat in subcutaneous depots, particularly in their hips and thighs(Reference Wells37). Moreover, in a review of evidence in children, Staiano & Katzmarzyk(Reference Staiano and Katzmarzyk13) confirmed that sexual dimorphism in fat patterning may also be evident in children, as was demonstrated in our study, whereby boys had an average visceral fat rating 1·9 units higher than girls. Although the mechanisms responsible for these sex differences in body fat distribution are not well understood in children(Reference Staiano and Katzmarzyk13), the aforementioned differences may explain why the association between SSB consumption and VAT was more pronounced in boys. Secondly, in both our sample and the sample of Saudi schoolchildren, boys were greater consumers of SSBs than girls. While this is to be expected, as males typically consume greater intakes of SSBs than females globally(Reference Singh, Micha and Khatibzadeh38), it is possible that consumption patterns in girls were not high enough to detect a significant association and/or stratified analyses may have lacked sufficient power. Furthermore, it is important to note that the majority of girls in our sample were at later stages of pubertal maturation than were boys and this could also play a part in the sex differences observed.
The positive association between SSB consumption and VAT remained robust, even after adjustment for morning serum cortisol levels. Moreover, we found a weak negative association between morning serum cortisol and VAT accumulation. Literature on the relationship between morning cortisol and abdominal adiposity in youth is limited. Although some studies have shown morning serum cortisol to be positively associated with visceral adiposity(Reference Gyllenhammer, Weigensberg and Spruijt-Metz27,Reference Weigensberg, Toledo-Corral and Goran39,Reference Barat, Gayard-Cros and Andrew40) , these studies have only included overweight and obese subjects. Two studies inclusive of normal weight children assessed morning salivary cortisol(Reference Hill, Eisenmann and Gentile41,Reference Hill, Eisenmann and Holmes42) , a strong correlate of serum cortisol(Reference Dorn, Lucke and Loucks43). Both studies were conducted in samples of Western children and neither found an association between cortisol and abdominal adiposity(Reference Hill, Eisenmann and Gentile41,Reference Hill, Eisenmann and Holmes42) . Disparities between our results and those previous may be explained by differences in the characteristics of study participants as well as differences in cortisol sampling procedures, as some studies used salivary cortisol and the time at which samples were collected varied. Furthermore, in the present study, associations between cortisol and VAT were adjusted for lifestyle factors such as energy intake and physical activity, while similar adjustments were only made in one of the previous studies(Reference Gyllenhammer, Weigensberg and Spruijt-Metz27). Although our findings are novel in children, low morning serum cortisol levels have been observed in adults with abdominal obesity and are thought to be a consequence of increased peripheral cortisol clearance, facilitated by increased VAT(Reference Björntorp44). However, whether this explains the negative association we observed in children is yet to be tested.
Only one other study has previously assessed the interaction between cortisol and SSB consumption on visceral adiposity. In a small sample of overweight and obese adolescents, Shearrer et al. (Reference Shearrer, Daniels and Toledo-Corral18) found no interactive effect between morning salivary cortisol and SSBs on VAT. Although our findings are similar for children with medium and high morning cortisol levels, where no associations were observed when stratified for these cortisol levels, we did find an association between high SSB consumption and visceral fat in children with low levels of morning cortisol. The reason for this effect is unclear; however, low morning cortisol in children may be a marker of allostatic load resulting from repeated or chronic exposure to stress(Reference Badanes, Watamura and Hankin45). Under conditions of chronic stress, individuals are more likely to consume foods high in sugar(Reference Torres and Nowson46) and evidence suggests they may also be more vulnerable to diet-related abdominal obesity(Reference Aschbacher, Kornfeld and Picard47). Taken together, it is possible that chronic stress may be accounting for the association between high SSB consumption and VAT in children with low morning cortisol levels. However, as we do not have data pertaining to children’s perceived stress, this interpretation is speculative and the possibility that morning serum cortisol is a stronger determinant of VAT than high SSB intake should also be considered as an explanation for the lack of association between SSBs and VAT in children with cortisol levels in the two highest tertiles. Further research is warranted to explain how low morning cortisol levels, as opposed to high, may moderate the association between SSBs and visceral adiposity.
A major strength of the present study was the large representative sample of primary school-aged children. Furthermore, the sample included children covering a wide range of BMI and was sufficiently sized to allow for strata-specific analyses. However, several limitations should be considered when interpreting our findings. Firstly, given the cross-sectional nature of the present study, we are unable to determine causality. Secondly, children’s diets were assessed using a subjective method and self-reports of dietary intake are often susceptible to error, particularly underreporting of energy intake from fats and sugars(Reference Foster and Bradley48). In addition, dietary intake was only assessed for three consecutive days, which may not accurately reflect children’s long-term habitual intake. Nevertheless, dietary recalls remain widely used in epidemiological studies and are a validated tool for measuring dietary intake in children of this age(Reference Foster and Bradley48). Lastly, morning serum cortisol was only assessed once for each child. Given that cortisol secretion follows a diurnal pattern, a single measure may be imperfect as a marker of HPA axis activity, and by nature of the design, we are unable to ascertain abnormalities in individual secretory patterns. Although the use of a single cortisol measure is most practical for a sample of this size, multiple measures throughout the day would have provided a more accurate assessment of HPA dysregulation.
In summary, in this cross-sectional study, high SSB consumption was associated with visceral adiposity in young children and boys were at an elevated risk. Morning serum cortisol may moderate the association between SSB consumption and VAT; however, additional studies are needed to replicate our findings and more precise measures of HPA dysregulation should be explored. As visceral adiposity is a strong predictor of future disease risk, it is important that SSB consumption is reduced during childhood and public health policy needs to continue to prioritise the reduction of sugar intake across all populations.
Acknowledgements
The authors thank the ‘Healthy Growth Study’ group for the valuable contribution to the completion of the study, as well as all children and parents who participated in thestudy.
The present research has been co-financed by the European Union (European Social Fund-ESF) and Greek national funds through the Operational Programme ‘Education and Lifelong Learning’ of the National Strategic Reference Framework (NSRF) – Research Funding Programme: Heracleitus II. Investing in knowledge society through the European Social Fund. The funders had no role in the design, analysis or writing of this article.
G. M. and Y. M. designed the Healthy Growth Study and were responsible for coordinating the data collection and curation, which was carried out by S. G., E. K. and C. M. The research question was formulated by B. E. and C. G. Statistical analyses were performed by K. A. L. and C. G. The manuscript was drafted and prepared by C. G. under the supervision of B. E., K. A. L. and G. M. All authors contributed in reviewing and revising the manuscript and all authors approved the final version of the manuscript.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary materials referred to in this article, please visit https://doi.org/10.1017/S0007114520003256







