Introduction
According to the WHO, the prevalence of overweight and obesity among children and adolescents aged 5–19 years was 18 % in 2016 v. 4 % in 1975(1). This situation leads to several short- and long-term undesirable health consequences(Reference Angelantonio, Bhupathiraju and Wormser2). Moreover, there are social inequalities in overweight and obesity in adolescents(Reference Chung, Backholer and Wong3). The inequalities are characterized by high levels of adiposity among less socially advantaged groups in high-income countries and low levels in developing and medium- to low-income countries(Reference Sares-Jäske, Grönqvist and Mäki4).
The literature shows that most adolescents do not achieve physical activity (PA), dietary intake (DI) and sedentary behaviour (SB) guidelines, although there is a demonstrated relation (negative for PA and positive for high energy-dense DI and SB) between these factors and weight status(Reference Ding, Fan and Yuan5,Reference Chaput, Willumsen and Bull6) . Theorical frameworks were developed to explain the link between lifestyle behaviours and social inequalities of weight status. According to the cultural-behavioural approach, the link between socio-economic status (SES) and health is a result of differences between SES in terms of health-related behaviours(Reference Bambra7). This framework exhibits how inequalities in DI, PA and SB(Reference Inchley, Currie and Jewell8) lead to a weight social gradient(Reference Akkoyun-Farinez, Omorou and Langlois9) whose reduction is the purpose of most public health interventions(Reference Hillier-Brown, Bambra and Cairns10,Reference Freudenberg11) . Nutrition public health interventions are then implemented and mainly focus on lifestyle behaviours to overcome inequalities of weight status(Reference Brown, Moore and Hooper12). However, the effect of levels of achieving lifestyle guidelines (DI and PA) on the reduction in inequalities has not been studied. The assessment of single or combined lifestyle behaviours that have a positive effect on reducing social inequalities of weight status and their required levels could be helpful for the development of effective interventions. These components could be combined in a randomised controlled trial but is difficult first because of the need for many arms of lifestyle behaviours with a large sample size, second because of additional difficulties of randomisation on SES (advantaged group and less advantaged group) and third because lifestyle behaviours change across time in adolescents (time-varying covariates)(Reference Jebeile, Kelly and O’Malley13).
Also, there is a need for statistical approaches that consider these changes. The parametric G-formula(Reference Taubman, Robins and Mittleman14) is used to estimate the effect of hypothetical interventions with repeated measurements for each individual in the context of time-varying covariates(Reference Taubman, Robins and Mittleman14). This study used the G-formula with data from the PRomotion de l’ALIMentation et de l’Activité Physique – INÉgalité de Santé (PRALIMAP-INÈS) trial to analyse the effect of achieving levels of DI and/or PA guidelines on reducing social inequalities in weight status among adolescents.
Methods
Study sample
Data were from the PRALIMAP-INÈS trial(Reference Legrand, Lecomte and Langlois15,Reference Briançon, Legrand and Muller16) that included adolescents from September 2012 to September 2015 who had excess weight: BMI greater than the International Obesity Task Force (IOTF)(Reference Cole, Bellizzi and Flegal17) cut-off and/or waist circumference greater than the McCarthy cut-off values for age and sex(Reference McCarthy, Jarrett and Crawley18). Eligible adolescents were divided into two groups according to SES measured by the Family Affluence Scale (FAS)(Reference Currie, Molcho and Boyce19). The FAS score (from 0 to 9(Reference Boyce, Torsheim and Currie20)) is based on four simple questions exploring the availability of a personal bedroom, family cars and computers and opportunities for family holidays. Advantaged adolescents (FAS score ≥5) received the standard intervention and constituted the ‘advantaged with standard care’ group. Less advantaged adolescents (FAS score < 5) were randomised to two subgroups: one-third received standard care (less advantaged with standard care) and two-thirds received standard and adapted care (less advantaged with standard and strengthened care). Randomisation was at the individual level(Reference Legrand, Lecomte and Langlois15). The interventions were implemented during one academic year, with follow-up at baseline (T0) and at the end of the intervention (T1). The PRALIMAP-INÈS trial protocol has been published elsewhere(Reference Legrand, Lecomte and Langlois15). This study was conducted according to the guidelines in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the French consultative committee for the treatment of information in health research (no. 12.299), the French National Commission for Data Protection and Liberties (no. 912372) and the French Person Protection Committee (no. 2012/15). Written informed consent was obtained from the parents of all adolescents. The trial was registered in ClinicalTrials.gov (NCT01688453) in September 2012. We included 1130 adolescents who had weight status (BMI z-score (BMIz)) data available at T0 and T1. Adolescents with missing data on BMIz at T1 were ‘non-completers’.
Measurements
A FFQ was used to assess the number of portions of fruits and vegetables (FAV) and sugar foods and drinks (SFD) consumed by adolescents each day(21). The cut-off for DI guidelines were ‘at least five parts of FAV a day’ (yes/no) and ‘at most one a day for SFD’ (yes/no) in accordance with WHO guidelines and the French Programme National Nutrition Santé(22).
PA and SB were measured with the International Physical Activity Questionnaire (IPAQ)(Reference Craig, Marshall and Sjöström23), a valid and reliable questionnaire for adolescents in France(Reference Craig, Marshall and Sjöström23,Reference Hagströmer, Bergman and De Bourdeaudhuij24) . The IPAQ assesses the frequency (days per week) and duration (minutes) of sitting, walking, moderate and vigorous PA during the previous 7 d. According to the WHO guidelines(Reference Chaput, Willumsen and Bull6), adolescents with at least 1 h of moderate to vigorous PA per d and at least 3 d of vigorous PA per week were considered to achieve PA guidelines. Moreover, a daily screen time more than 2-h cut-off defined SB (yes/no)(Reference Chaput, Willumsen and Bull6).
Weight status was measured by trained school nurses/clinical research nurses as well as physicians by use of the BMI, the ratio of weight to height squared. Weight was expressed in kilograms and height in metres. We also calculated BMIz as the distance between the measured BMI and the mean BMI of a WHO age- and sex-specific reference population(Reference de Onis, Onyango and Borghi25). Other measurements were the waist circumference (WC) in centimetres and the prevalence of overweight or obesity according to the IOTF age- and sex-specific cut-off values for BMI(Reference Cole, Bellizzi and Flegal17).
Baseline sociodemographic characteristics included age (year), sex (boy/girl) and school type (general high school, vocational high school and middle school). Students in general and vocational high schools were in grade 10, whereas those in middle schools were in grade 9. The other sociodemographic characteristics were related to school boarding status (non-boarding, half-boarding and full-boarding), number of parents responsible (zero, one and two), social and professional class of the family (executives, farmers, craftsmen, intermediate jobs, employees, workers and other), adolescents’ perceived income level of the family (low, average and high), intervention group (less advantaged with standard care, less advantaged with standard and strengthened care, and advantaged with standard care) and SES measured by FAS score.
The main outcome of the study was the likelihood of a 1-year reduction in BMIz defined as ΔBMIzT1–T0 < 0. This cut-off was used given that a modest reduction in BMIz (i.e. > 0) after a 1-year intervention in adolescents was found associated with improvement in several cardiovascular risk factors(Reference Kolsgaard, Joner and Brunborg26). The secondary outcomes were differences in BMIz and WC from T0 to T1 (T0–T1).
Interventions were developed based on achieving DI and PA guidelines and baseline SES (advantaged and less advantaged). We considered six hypothetical interventions for 1 year (T0 and T1) as shown in Table 1. The interventions were based on a counterfactual hypothesis: What would happen if:
-
Socially advantaged adolescents maintained their lifestyle behaviours? (scenario 1). This means that adolescents were socially advantaged and maintained their baseline DI and PA.
-
Socially less advantaged adolescents maintained their lifestyle behaviours? (scenario 2). This means that adolescents were socially less advantaged and maintained their baseline DI and PA.
-
Socially less advantaged adolescents behaved like socially advantaged ones? (scenario 3). In this scenario, socially less advantaged adolescents have lifestyle behaviours (DI and PA) at T1 corresponding to those of socially advantaged ones at baseline.
-
Socially less advantaged adolescents improved their DI? (scenario 4). In this scenario, adolescents are socially less advantaged and the proportion of those achieving DI (both FAV and SFD) guidelines increases by 30 % between T0 and T1.
-
Socially less advantaged adolescents improved their PA? (scenario 5). In this scenario, adolescents are socially less advantaged and the proportion of those achieving PA guidelines increases by 30 % between T0 and T1. Given that we were in an interventional context and had less advantaged adolescents, we doubled the new target of the WHO‘s Global Action Plan on Physical Activity 2018–2030, which consists of a 15 % relative reduction in physical inactivity globally by 2030(27).
-
Socially less advantaged adolescents improved both DI and PA? (scenario 6). In this scenario, adolescents are socially less advantaged and the proportion of those achieving DI (both FAV and SFD) and PA guidelines increases by 30 % between T0 and T1.
Table 1. Description of hypothetical interventions (scenarios) and meanings of comparisons simulated
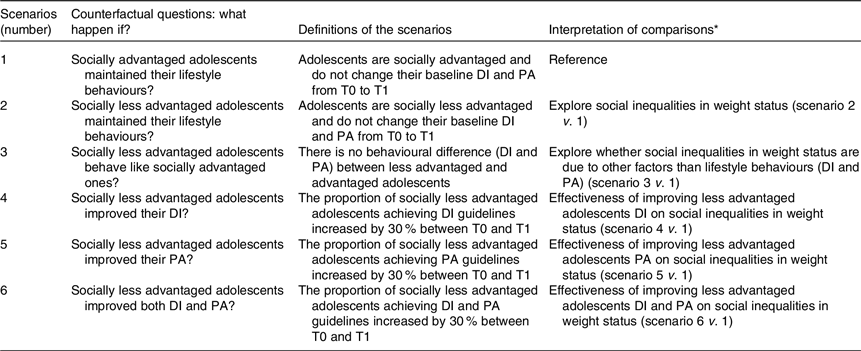
DI, dietary intake (fruit and vegetable + sugar foods/drinks); PA, physical activity; T0, baseline; T1, 1-year follow-up.
* Scenarios 2–6 were compared with scenario 1 as a reference on the likelihood of a 1-year reduction in BMIz.
By using scenario 1 as a reference for all comparisons between scenarios, their meanings are reported in Table 1.
Statistical analysis
First, Student’s t test was used for analysing continuous variables and χ 2 test for categorical variables. Then, the likelihood of a 1-year reduction in BMIz under the different hypothetical interventions was investigated with the parametric G-formula(Reference Taubman, Robins and Mittleman14). For this, we chose time-varying covariates (FAV, SFD, PA and SB guidelines achievement) and fixed baseline covariates (age, sex, school type and grade, school boarding status, number of parents responsible, social and professional class of the family, perceived income level of the family, intervention group and BMIz at baseline). SES (advantaged/less advantaged) was used as a conditional variable in the scenarios. The steps were as follows (Fig. 1):
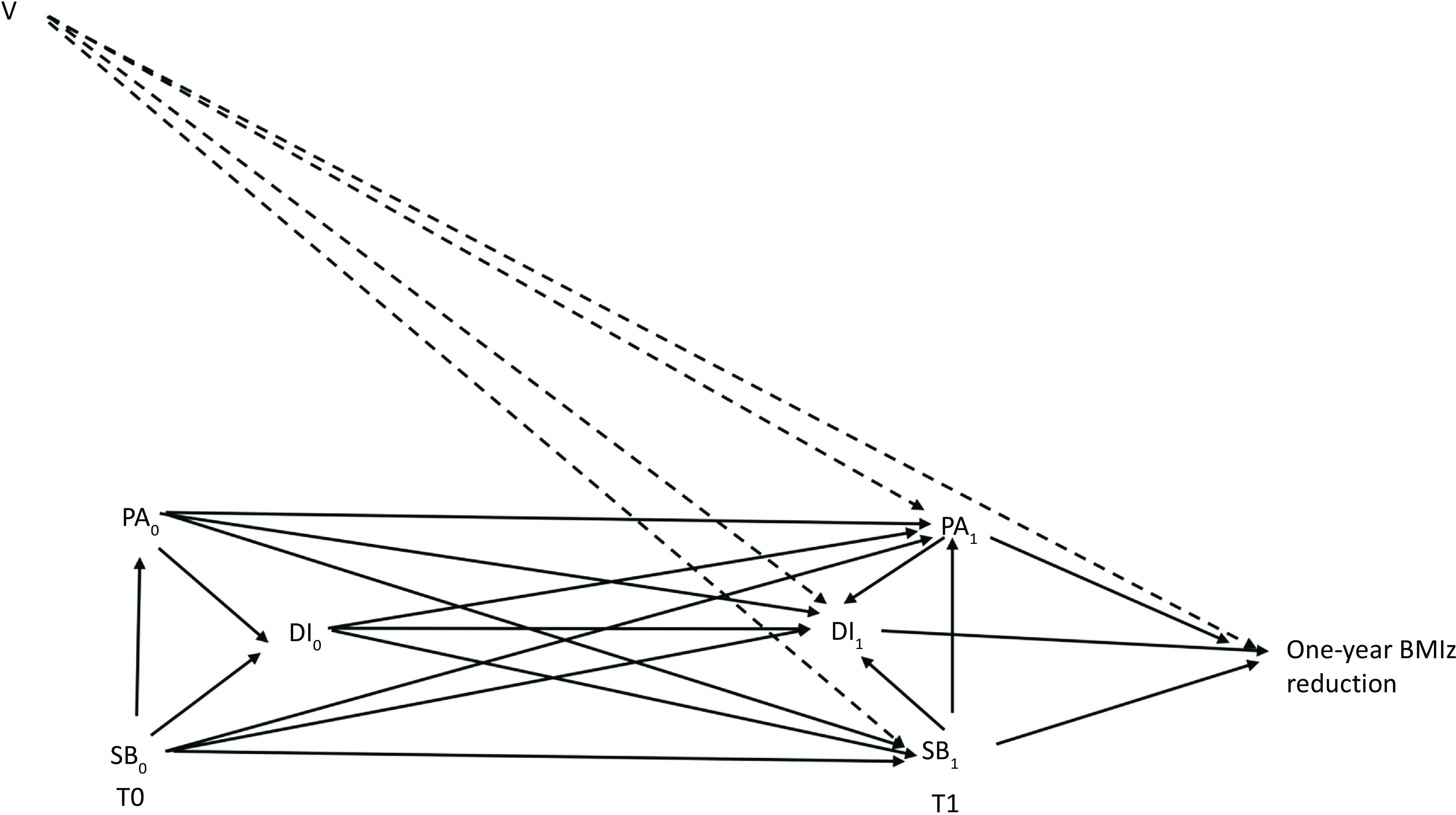
Fig. 1. Directed acyclic graph showing hypothesised causal relations among study fixed (V) and time-varying (DI, PA and SB) covariates used in scenarios at baseline (T0) and 1-year follow-up (T1). Abbreviations: V, fixed covariates (age, sex, school type and grade, school boarding status, number of parents responsible, social, and professional class of the family, perceived income level of the family and intervention group) used to adjust models. Time-varying covariates: DI, dietary intake; PA, physical activity; SB, sedentary behaviour; BMIz, BMI z-score.
Step 1: We fitted parametric regression models for the time-varying covariates at T1 as a function of T1 and T0 covariate history (baseline sociodemographic characteristics). Therefore, we developed linear regression models to estimate number of parts of FAV, SFD and duration of screen time (SB) per d and a logistic regression model for PA guidelines achievement (yes/no). SB was used as a time-varying covariate to adjust our models as baseline covariates.
Step 2: We fitted a logistic regression model for the likelihood of a 1-year reduction in BMIz as a function of hypothetical intervention and covariates history (baseline sociodemographic characteristics and time-varying covariates) among individuals under follow-up.
Step 3: We used a Monte Carlo simulation to generate a 10 000-individual population based on original data from PRALIMAP-INÈS and under each of the hypothetical interventions to minimise simulation error(Reference Thoemmes, MacKinnon and Reiser28). For everyone, the values of baseline covariates (T0) were randomly sampled with replacement from the individual’s PRALIMAP-INÈS trial data. Then, time-varying covariates were generated at T1 by using the equation of the parametric regression models of step 1. After the values were generated at T1, values of covariates that were to undergo hypothetical interventions (scenarios 1–6) were then changed according to the specified scenario rule. The likelihood of a 1-year reduction in BMIz was finally estimated for each of the 10 000 histories under each hypothetical intervention based on the logistic regression models in step 2.
Step 4: We computed the likelihood of a 1-year reduction in BMIz in the population under each hypothetical intervention (population risk), the population risk differences (PRD) (differences between less advantaged and advantaged adolescents in the likelihood of a 1-year reduction in BMIz) and the population risk ratio (ratio of likelihood of a 1-year reduction in BMIz) between hypothetical interventions by using scenario 1 as the reference for each comparison. A significant PRD reflected inequalities in the likelihood of a 1-year reduction in BMIz (positive values in favour of less advantaged adolescents and negative values in favour of advantaged ones), whereas a non-significant PRD means that inequalities were not shown.
Step 5: We repeated the previous steps in 100 bootstraps to obtain 95 % CI of the different estimators. The algorithm also calculated the likelihood of a reduction in BMIz under a natural course (no change in any of the time-varying covariates estimated in step 3 at T1). The goodness of fit of the model was appreciated by the observed likelihood of the reduction in BMIz (likelihood of a 1-year reduction in BMIz based on PRALIMAP-INÈS data and without any simulation), which must be included in the CI of the same reduction under the natural course for a good model fit. The natural course represents a simulation of 10 000 adolescents based on the PRALIMAP-INÈS trial without any change in levels of achieving DI and PA guidelines.
Sensitivity analysis
The same analyses were performed for secondary outcomes (BMIz and WC difference from T0 to T1). The model estimated the means of differences and standard errors under each hypothetical intervention. Finally, ratios of means, differences of means and their corresponding 95 % CI were calculated by using scenario 1 as a reference.
Data were analysed with SAS 9.4 (SAS Institute) with an implementation of the macro G-formula 3(Reference Taubman, Robins and Mittleman14). The macro is available at http://www.hsph.harvard.edu/causal/software. P < 0·05 was considered statistically significant.
Results
Baseline sociodemographic, anthropometric characteristics and achievement of lifestyle guidelines for the study sample and the non-completers (BMIz data not available at T1) are in Table 2. As compared with non-completers, the study sample was younger (mean age 15·2 ± 0·7 v. 15·5 ± 0·7 years, P < 0·001) and had more boys (45·7 % v. 37·4 %). Completers were also more enrolled in middle school and less in high school. Adolescents with at least one parent responsible and high prevalence of SB were more able to attend the follow-up. Additionally, non-completers and the study sample significantly differed in the social and professional class of their family (P = 0·02). Moreover, the study sample and non-completers did not differ in the most relevant baseline variables such as SES (family affluent scale score, perceived income level of the family), anthropometric characteristics and lifestyle guidelines except screen time.
Table 2. Comparison of baseline sociodemographic, anthropometric characteristics and lifestyle guidelines achievement between the study sample and non-completers

FAS, Family Affluence Scale; PRALIMAP-INÈS, PRomotion de l’ALIMentation et de l’Activité Physique – INÉgalité de Santé; BMIz, BMI z-score; MVPA, middle to vigorous physical activity; VPA, vigorous physical activity.
All percentages were calculated with the denominator as the total number (n in the column head) minus the number of missing data. Bold values are used for statistical significance (P < 0·05).
* SD.
† P-value for χ 2 test for categorical variables, Student’s t test for quantitative variables.
‡ Close to overweight (International Obesity Task Force 25 percentile minus 1 kg/m2) associated with waist circumference greater than the McCarthy cut-off values for age and sex or eating disorders.
Adolescents in the PRALIMAP-INÈS trial had low levels of achieving lifestyle guidelines at baseline regardless of their SES (22·1 % and 25·6 % achieved FAV and PA guidelines, respectively) (Table 3). We found social inequalities in achieving FAV (16·7 % v. 26·3 %; P < 0·001) and PA (20·9 % v. 29·1 %; P = 0·003) guidelines in favour of advantaged adolescents at baseline. Overall, 56 % of adolescents reduced their BMIz at 1 year, with no difference by SES. There was also no difference in WC reduction by SES.
Table 3. Comparison of baseline lifestyle guidelines achievement and weight status change between T0 and T1 according to socio-economic status
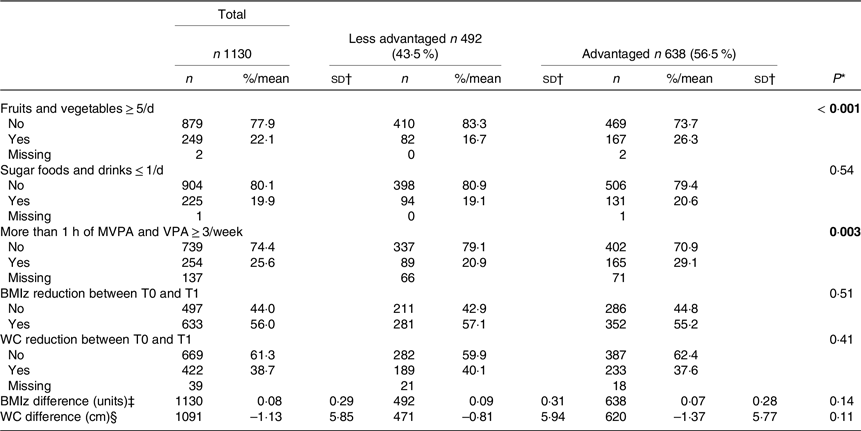
MVPA, middle to vigorous physical activity; VPA, vigorous physical activity; BMIz, BMI z-score; T0, baseline; T1, 1-year follow-up; WC, waist circumference.
All percentages were calculated with the denominator as the total number (n in the column head) minus the number of missing data. Bold values are used for statistical significance (P < all percentages were calculated with the denominator as the total number (n in the column head) minus the number of missing data. Bold values are used for statistical significance (P < 0·05).
* P-value for χ 2 test for categorical variables.
† SD.
‡ BMIz difference = BMIz at T0 minus BMIz at T1.
§ WC difference = WC at T0 minus WC at T1.
Table 4 shows the likelihood of a 1-year reduction in BMIz under different hypothetical interventions. Under the natural course (simulation of 10 000 adolescents based on the PRALIMAP-INÈS trial without any change in levels of achieving DI and PA guidelines), the likelihood of a 1-year reduction in BMIz was 51·2 % (95 % CI = (45·2, 56·6)), which included the observed likelihood (likelihood of a 1-year reduction in BMIz based on PRALIMAP-INÈS data and without any simulation: 56·0 %), and suggests a good model fit. Under scenario 1 (i.e. advantaged adolescents maintaining their baseline achievement of DI (FAV: 26·3 %; SFD: 20·6 %) and PA (29·1 %) guidelines), the likelihood of adolescents reducing the 1-year BMIz was 54·9 % (95 % CI 48·5 %, 60·5 %). Additionally, when less advantaged adolescents maintained their baseline achievement of lifestyle guidelines (scenario 2: FAV (16·7 %); SFD (19·1 %) and PA (20·9 %)), 53·3 % (46·6 %, 58·6 %) were able to reduce their BMIz. As compared with scenario 1 (reference), the PRD was −1·6 % (–3·0 %, −0·5 %) and confirms the social inequalities of weight status among adolescents. Moreover, the number needed to treat was 62, so for 62 less advantaged adolescents under this hypothetical intervention, one adolescent increased or maintained the BMIz after 1 year as compared with advantaged adolescents (scenario 1). These inequalities were not observed when less advantaged adolescents behaved like advantaged ones (scenario 3: FAV (16·7 % to 26·3 %); SFD (19·1 % to 20·6 %) and PA (20·9 % to 29·1 %)) with a PRD of −0·2 % (–1·6 %, 0·5 %). Similar results were observed when less advantaged adolescents increased the proportion of those achieving DI guidelines by 30 % (scenario 4: FAV (16·7 % to 46·7 %) and SFD (19·1 % to 49·1 %)) with a PRD of 2·2 % (–0·5 %, 5·0 %). Unlike when less advantaged adolescents increased the proportion of only those achieving PA guidelines by 30 % (scenario 5: PA (20·9 % to 50·9 %)), inequalities persisted with a PRD of −3·9 % (–6·8 %, −1·3 %). Finally, we found no inequalities of weight status when less advantaged adolescents increased the proportion of those achieving DI and PA guidelines by 30 % (scenario 6: FAV (16·7 % to 46·7 %); SFD (19·1 % to 49·1 %) and PA (20·9 % to 50·9 %)) with a PRD of 2·2 % (–0·5 %, 4·0 %). Results in Table 5 confirm our findings when BMIz reduction was used as a continuous variable. Online Supplementary Table S1 shows that social inequalities were not observed for the likelihood of a 1-year reduction in WC when scenarios involved DI or PA or both. However, with WC used as a continuous variable, we did not find social inequalities in the evolution of WC from T0 to T1 (online Supplementary Table S2).
Table 4. Probabilities of a 1-year reduction in BMIz under various achievements of DI and PA guidelines
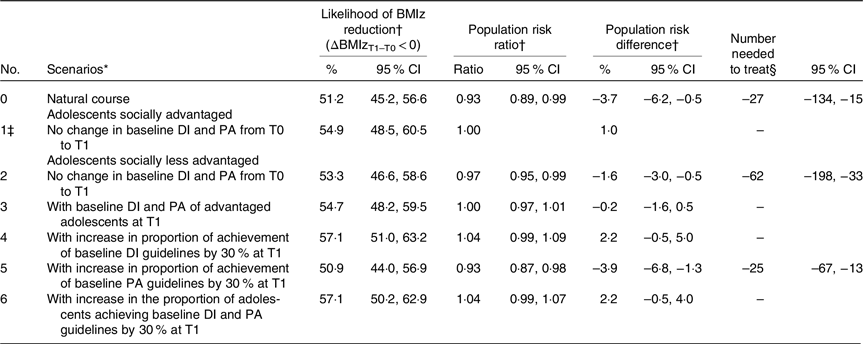
BMIz, BMI z-score; DI, dietary intake (fruit and vegetable + sugar foods/drinks); PA, physical activity; T0, baseline; T1, 1-year follow-up.
Observed likelihood of a 1-year reduction in BMIz was 56·0 %.
Population risk differences: differences between less advantaged and advantaged adolescents (reference) in likelihood of a 1-year reduction in BMIz.
Population risk ratio: ratio of likelihood of a 1-year reduction in BMIz between hypothetical interventions by using scenario 1 as a reference category for each comparison.
* Simulated scenarios under parametric G-formula modelling based on observed data.
† All models included lagged values of time-varying covariates (fruits and vegetables, sugar foods and drinks, PA and sedentary behaviour guidelines achievement) and baseline fixed covariates (age, sex, school type and grade, school boarding status, number of parents responsible, social and professional class of the family, perceived income level of the family, intervention group, socio-economic status and BMIz at baseline).
‡ Reference category.
§ Number needed to treat is given only when the population risk difference reaches statistical significance.
Table 5. Means of a 1-year difference in BMIz under various levels of achievement of DI and PA guidelines

BMIz, BMI z-score; DI, dietary intake (fruit and vegetable + sugar foods/drinks); PA, physical activity; T0, baseline; T1, 1-year follow-up.
BMIz difference = BMIz at T0 minus BMIz at T1.
Observed mean of a 1-year difference in BMIz was 0·8 units.
Ratio of means: ratio of means of BMIz difference between hypothetical interventions by using scenario 1 as the reference category for each comparison.
Population risk differences: differences between less advantaged and advantaged adolescents (reference) in means of BMIz differences.
* Simulated scenarios under parametric G-formula modelling based on observed data.
† All models included lagged values of time-varying covariates (fruits and vegetables, sugar foods and drinks, PA and sedentary behaviour guidelines achievement) and baseline fixed covariates (age, sex, school type and grade, school boarding status, number of parents responsible, social and professional class of the family, perceived income level of the family, intervention group, socio-economic status and BMIz at baseline).
‡ Reference category.
Discussion
The results of this study confirm low levels of achieving lifestyle guidelines in adolescents regardless of SES with social inequalities in weight status (likelihood of a 1-year reduction in BMIz under each scenario). Differences by SES in obesity-related behaviours with a high prevalence of unhealthy lifestyle behaviours in adolescents with low SES result in a social gradient of lifestyle behaviours(Reference Inchley, Currie and Jewell8) and weight status(Reference Manneville, Omorou and Legrand29).
In this work, we developed scenarios targeting mainly less advantaged adolescents. If adolescents achieved the same levels of lifestyle guidelines as advantaged ones, there would be no social inequalities of weight status. This result suggests that social inequalities of weight status are mostly mediated by differences in lifestyle behaviours due to differences in SES, as supported by the cultural-behavioural theory of health inequalities(Reference Bambra7). An unequal distribution of resources and environments prevents excess weight gain for height (healthy food, opportunities for PA, primary and preventive healthcare, and protection from stressors) that results in inequalities of weight status(Reference Freudenberg11). Future interventions should actively target a balanced distribution of lifestyle behaviours across different levels of the social hierarchy. In a systematic review, Beauchamp et al. showed that unlike studies targeting individual-level behaviour, those that primarily included community-based strategies or policies and aiming at structural changes to the environment were effective for low-SES participants(Reference Beauchamp, Backholer and Magliano30). Such strategies include restrictions in marketing unhealthy food and drink and pricing measures. However, their implementation is politically difficult(Reference Peeters and Backholer31).
When less advantaged adolescents achieved both FAV and SFD (DI guidelines) rather than PA guidelines by 30 %, social inequalities of weight status were not observed. Moreover, we showed that interventions targeting PA in order to reduce social inequalities of weight status must be combined with improvements in diet to be effective (scenario 6 v. 1). The contribution of diet quality to social inequalities of weight status was reported in an adult population-based study in Switzerland(Reference de Mestral, Chatelan and Marques-Vidal32): the proportion of the association between educational level and obesity that was mediated by diet quality was 22·1 % when using BMI. The authors suggested that focusing efforts on improving the diet quality of less advantaged groups could help reduce social inequalities in obesity.
When the proportion of less advantaged adolescents who achieved PA guidelines increased by 30 %, inequalities persisted. Studies examining PA by SES showed mixed results(Reference Andrade, Lachat and Ochoa-Aviles33,Reference Hollis, Sutherland and Campbell34) , potentially due to differences in how PA was measured. Previous interventions aiming to increase the proportion of less advantaged adolescents that achieved PA guidelines had no effect on mean BMIz or prevalence of overweight and obesity(Reference Andrade, Lachat and Ochoa-Aviles33,Reference Pfeiffer, Robbins and Ling35) . In a randomised controlled trial that assessed the impact of a school-based PA intervention on adiposity of less advantaged adolescents, the authors found no effect on BMIz after 1 year, but a significant reduction after 2 years of the intervention(Reference Hollis, Sutherland and Campbell34). The short duration of interventions (1 year in our scenarios) could underestimate the impact of PA on inequalities of weight status. However, using retrospective cohort data for children in the UK, Pearse et al. (Reference Pearce, Hope and Griffiths36) simulated various interventions on the achievement of the WHO PA guidelines. The authors showed that universal achievement of the WHO’s PA guidelines, if attainable, would reduce the prevalence of childhood overweight and obesity but not inequalities. The same result was reported when the authors targeted less advantaged groups. As shown in our study, these authors suggested that reducing inequalities in overweight/obesity should involve examining policy scenarios that also focus on the upstream influences on diets. Nevertheless, given that inadequate health literacy is strongly associated with low SES(Reference Svendsen, Bak and Sørensen37), the difference in the effectiveness of DI and PA interventions on social inequalities of weight status raises the question of bias related to how the messages were transmitted and the ability of adolescents to understand.
Social inequalities in WC among adolescents have been reported(Reference Setiono, Guerra and Leung38) with controversial results of interventions(Reference Leme, Lubans and Guerra39,Reference Moore, Borawski and Love40) . The discrepancy in the results when the difference in WC was used as binary v. continuous variable could be explained by the limitations of this weight status indicator with variability due to the measurement site(Reference Lee, Kim and Han41).
In this study, we only reported short-term results, but the sustainability of healthy behaviours is required. According to authors who advocate incremental changes, only modest change is politically feasible(Reference Freudenberg11). They argue that reducing DI by 50–100 energy content a day or increasing daily PA by 10 min is sufficient, if sustained to bring about measurable declines in obesity.
Limitations and strengths
The first limitation is that scenarios were simulated by using data from an intervention that was effective in reducing social inequalities(Reference Briançon, Legrand and Muller16) in weight status among adolescents with overweight and obesity (no difference in the proportion of a 1-year reduction in BMIz between advantaged and less advantaged adolescents). This leads to a natural course, which was the context of PRALIMAP-INÈS trial and could limit the generalisation of our findings. However, this context was taken into account by considering another hypothetical intervention (scenario 1) as a reference category, and all simulations were adjusted on intervention groups of the PRALIMAP-INÈS trial as a fixed baseline covariate. Second, the measurement of PA, DI and SB involved self-reporting questionnaires (FFQ and IPAQ). However, these questionnaires are valid and reliable(21,Reference Craig, Marshall and Sjöström23,Reference Hagströmer, Bergman and De Bourdeaudhuij24) . Third, SB was not included in the scenarios given that a recent paper on PRALIMAP-INÈS baseline data demonstrated that PA rather than SB was socially determined in French adolescents with overweight and obesity(Reference Omorou, Manneville and Langlois42). Nevertheless, it was used as a time-varying covariate to adjust our models. Fourth, the result about the effectiveness of interventions aiming to improve PA on social inequalities of weight status (BMIz) should be taken with caution because absence of evidence is not evidence of absence(Reference Wasserstein and Lazar43).
Despite these limitations, this study has several strengths. First, this is the only study that investigated the effect of different levels of lifestyle guidelines achievement on social inequalities of weight status with a longitudinal design and a large sample size (1130 participants). Second, the target of 30 % improvement in the proportion of adolescents achieving lifestyle guidelines in the scenarios is reasonable. For example, the WHO’s target is an increase of 15 % in PA globally by 2030(27). We doubled this target, given that less advantaged adolescents with lower levels of achievement of recommendations were interested in our strategies. This is the principle of targeted interventions in order to narrow the health gap(Reference Graham and Kelly44). Third, the absence of significant differences in relevant variables between the study sample and non-completers suggests a limitation of the risk of selection bias and could increase the generalisation of our results. Finally, this study shows the real effect of several interventions targeting less advantaged groups on the reduction in social inequalities of weight status by considering the natural course in the advantaged group as a reference. It offers more robust conclusions on social inequalities of weight status than most interventions considering the natural course of less advantaged adolescents as a reference and did not allow for conclusions on reducing inequalities but only on changes in weight status indicators(Reference Pfeiffer, Robbins and Ling35,Reference Prado, Fernandez and St. George45) .
Conclusion
This study confirms social inequalities of a 1-year reduction in BMIz. By increasing the proportion of adolescents achieving DI guidelines by 30 %, these inequalities were no longer observed. Policies that address inequalities of weight status among adolescents could focus on and improve levels of achievement of DI guidelines. Additionally, interventions aiming at improving PA could be associated with DI to be more effective on inequalities of weight status. Most efforts are required to allow less advantaged adolescents to access healthy foods in order to achieve DI guidelines.
Acknowledgements
In the name of the PRALIMAP-INÈS trial group, the authors thank all those who, through their various roles, led to the implementation of this project. The PRALIMAP-INÈS Trial Group: Philip Böhme, Serge Briançon, Rozenn De Lavenne, Cécile Gailliard, Johanne Langlois, Edith Lecomte, Karine Legrand, Laurent Muller, Abdou Y. Omorou, Céline Pourcher, Marie-Hélène Quinet, Laura Saez, Elisabeth Spitz and Brigitte Toussaint.
This research did not receive any specific funding from agencies/institutions in the public, commercial or not-for-profit sectors.
M. D. contributed to designing the study, carrying out the study, analysing the data, interpreting the findings and writing the article. F. M., A. O. and F. G. contributed to formulating the research question, designing the study, interpreting the findings and writing the article. J. L., K. L., E. L., P. B., E. S. and S. B. contributed to interpreting the findings and proofreading the article.
The authors declare no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524001090









