CHD is a leading cause of morbidity and mortality, especially in developed countries(Reference Wilkins, Wilson and Wickramasinghe1,Reference Benjamin, Muntner and Alonso2) . Prevention of CHD therefore remains a major public health priority. CHD arises from a mixture of genetic and lifestyle factors, and diet is an important modifiable component(Reference Hu and Willett3,Reference Dalen and Devries4) . The combined evidence from several prospective cohort studies supports an inverse association between intake of vegetables and risk of CHD(Reference Bechthold, Boeing and Schwedhelm5,Reference Aune, Giovannucci and Boffetta6) , and intake of vegetables is recommended by cardiologists and health organisations worldwide for prevention of CHD(Reference Lichtenstein, Appel and Brands7,8) . It is further recommended to eat a variety of vegetables(Reference Lichtenstein, Appel and Brands7). However, studies on the association between subgroups of vegetables and risk of CHD are limited. They have so far shown no associations or inverse associations for intake of especially green leafy vegetables (such as spinach, iceberg, romaine, kale and chard greens) and risk of CHD(Reference Aune, Giovannucci and Boffetta6).
Individuals usually maintain a relatively stable energy intake over time(Reference Hall and Guo9), and a higher intake of vegetables is likely to be associated with a lower intake of other energy-providing foods. The replaced food items could be harmful, neutral or beneficial in relation to CHD; therefore, the association between vegetable intake and CHD also depends on the replaced foods in the diet. However, most studies examining the association between vegetable intake and CHD have not specified the replaced foods. Substitution studies comparing specific vegetables with other specified foods are therefore needed to provide detailed knowledge of how different vegetables may affect the risk of CHD(Reference Lichtenstein, Appel and Brands7,10,Reference Willett11) .
Potatoes are classified as a root vegetable from a botanical perspective but are mainly eaten as a staple food like rice or pasta(Reference Schwingshackl, Schwedhelm and Hoffmann12). Compared with most other vegetables, potatoes are energy dense, nutrient poor and have a high glycaemic index(Reference Bertoia, Mukamal and Cahill13,Reference Furrer14) . Thus, replacement of potatoes with other vegetables may prevent CHD. The aim of our study was to investigate replacement of potatoes with other vegetables or subgroups of other vegetables and risk of myocardial infarction (MI). Substitutions between subgroups of other vegetables and risk of MI were also investigated.
Subjects and methods
Study population
The present study is based on data from participants in the Danish Diet, Cancer and Health cohort. From December 1993 through May 1997, 79 729 women and 80 996 men aged 50–64 years were invited by mail to participate in the cohort. In total, 57 053 participants were recruited. Eligible participants were born in Denmark and were living in the greater Copenhagen or Aarhus areas. A FFQ and a lifestyle questionnaire were filled in by each participant. All participants visited a study centre, where trained laboratory technicians conducted anthropometric measurements including height, weight and waist circumference, and the self-administered questionnaires were scanned and interviewer-checked. A thorough description of the data collection process has been published previously(Reference Tjonneland, Olsen and Boll15). The study was approved by the relevant regional ethical committees on human studies and by the Danish Data Protection Agency. All participants gave written informed consent.
Dietary assessment
The participants filled in a 192-item semi-quantitative FFQ, which was designed for the study(Reference Overvad, Tjonneland and Haraldsdottir16) and validated against two 7-d weighed diet records(Reference Tjonneland, Overvad and Haraldsdottir17). Participants reported their average intake of different food and beverage items over the previous year within 1 of 12 possible intake categories that ranged from never to ≥8 times/d. The FFQ included eight questions specifically about potatoes (boiled (eaten hot for dinner, cold for dinner as potato salad or cold for lunch in an open sandwich), baked, roasted, fried, mashed or stewed) and twenty-five questions specifically about other vegetables (e.g. raw, cooked or baked). Most of the questions covered intake of single vegetable items, like carrots, peas and beans. Few questions covered intake of dishes with vegetables as the main ingredient, like green salad and vegetable steak. In addition to these vegetable-specific questions, minor contributions to the vegetable intake came from dishes like goulash and stew. The daily intake of potatoes and other vegetables was calculated for each participant by using the software programme FoodCalc(18). Intake of potatoes was combined into one potato group, with the majority being boiled potatoes. Intake of potato chips was not included in the potato variable. The other vegetables were further grouped based on a botanical definition: fruiting vegetables (cucumber, eggplant, green pepper, red pepper, tomato, zucchini, avocado, green beans, green peas and maize), root vegetables other than potatoes (carrot, celeriac and ginger) and cabbage (white cabbage, broccoli, red cabbage, spring cabbage and Brussels sprouts). The intake of mushrooms, onions, stalk vegetables/sprouts and leafy vegetables was limited, and these vegetable groups were combined into a group named remaining vegetables. Potatoes, total vegetables other than potatoes, fruiting vegetables, root vegetables (not including potatoes) and cabbage were investigated as exposure groups.
Identification of cases
The outcome measure was incident non-fatal and fatal MI. Participants registered with a first-time discharge diagnosis of MI (International Classification of Diseases 8th revision codes 410-410.99 and International Classification of Diseases 10th revision codes I21.0-I21.9) were identified through linkage with the Danish National Patient Register and the Danish Cause of Death Register using the unique ten-digit civil registration number provided to all Danish citizens. Furthermore, we included participants, who were registered with a diagnosis of cardiac arrest (International Classification of Diseases, 8th revision, code 427.27 or International Classification of Diseases, 10th revision, codes I46.0-I46.9) provided that the arrest was believed to be of cardiac origin after validation. From baseline through 2003, the medical records were retrieved and reviewed and the diagnoses were validated in accordance with the criteria of MI as recommended by the American Heart Association and other major health organisations for use in epidemiological studies(Reference Joensen, Jensen and Overvad19–Reference Stegger, Schmidt and Obel21). From 1 January 2004 and until the end of study on 31 December 2009, all participants with a hospital diagnosis of MI were accepted without further validation, as the diagnoses in the Danish National Patient Register have a positive predictive value above 92 %(Reference Joensen, Jensen and Overvad19). All other potential cases were validated individually by investigating all diagnoses and procedure codes of the involved participants in the National Patient Register and the Cause of Death Register.
Assessment of covariates
From the lifestyle questionnaire, we obtained information on length of education, smoking status, physical activity, menopausal status (women only) and use of postmenopausal hormones (women only) together with history of hypertension, hypercholesterolaemia and diabetes mellitus. Total length of elementary and secondary education was reported in predefined categories (≤7, 8–10 and >10 years). Smoking status was reported as never, former or current, and if current smoker, the number of cigarettes, cigars, cheroots and tobacco pipes smoked per day. Current tobacco consumption was calculated by using conversion factors of 1·0 for cigarettes, 4·5 for cigars and 3·0 for cheroots and tobacco pipes and divided into <15, 15–25 or >25 g tobacco/d. Physical activity was reported as planned physical activity and active transportation in winter and summer and divided into < or ≥3·5 h/week. History of hypertension was defined as reported hypertension and/or use of antihypertensive medications (yes, no and do not know). History of hypercholesterolaemia was defined as reported hypercholesterolaemia and/or use of cholesterol lowering medications (yes, no and do not know). History of diabetes mellitus was defined as reported diabetes mellitus and/or use of insulin (yes, no or do not know). BMI was calculated as weight in kg divided by height in meters squared (kg/m2) as measured at the visit to the study centre. Waist circumference was likewise measured by a trained laboratory technician at the study centre. Information on alcohol intake, total energy intake and intake of other food groups was obtained from the FFQ.
Exclusion criteria
Participants with a diagnosis of cancer at study enrolment that was not registered in the Danish Cancer Registry at the time of invitation (due to processing delay) were excluded. Furthermore, participants registered with a previous diagnosis of MI or cardiac arrest at baseline were excluded. Finally, participants with incomplete questionnaires or missing anthropometric measurements were also excluded.
Statistical analyses
The Cox proportional hazards model was used to calculate hazard ratios (HR) with 95 % CI for specified vegetable substitutions and risk of MI. Analyses were carried out separately for women and men. The participants’ age was used as the underlying time scale, and the observation time for each participant began at enrolment into the Diet, Cancer and Health cohort (between December 1993 and May 1997) and ended on the date of a registered diagnosis of MI, death from another cause, emigration, or 31 December 2009, whichever occurred first. All models were stratified by age and date of enrolment to allow for differences in baseline hazards by entering these variables into the strata statement of the Cox models.
Vegetable substitutions were investigated in both g/week and kcal/week by including the exposure food groups as continuous variables. All substitutions were modelled statistically and thus based on differences in dietary habits at baseline and not on actual food replacements by the study participants. For substitutions between potatoes, other vegetables, fruiting vegetables and root vegetables other than potatoes, increments of 500 g/week or 250 kcal/week (=1046 kJ/week) were used. For substitution of cabbage for potatoes or other vegetable subgroups, increments of 200 g/week or 100 kcal/week (=418·4 kJ/week) were chosen due to the limited variation in intake of cabbage. The substitutions were calculated by including each of the vegetable subgroups in the statistical models, except for the vegetable group to be replaced, in addition to a sum variable made up by the total vegetable intake (the sum of potatoes, fruiting vegetables, root vegetables other than potatoes, cabbage and remaining vegetables). For example, the replacement of potatoes with other vegetables (the sum of fruiting vegetables, root vegetables other than potatoes, cabbage and remaining vegetables) was specified in the statistical models by inclusion of the variable for other vegetables and the sum variable made up by total vegetable intake, thereby leaving out potatoes from the model. Because the total amount of vegetables was held constant by inclusion of the sum variable in the statistical models, 500 g/week increments of other vegetables implied a concomitant 500 g/week lower intake of potatoes that were excluded from the model. This method has been named the leave-one-out method and is described in more detail in the method paper on food substitution models for nutritional epidemiology by Ibsen et al. (Reference Ibsen, Laursen and Würtz22). Model 1a included age and date of enrolment as described above and total energy intake (kcal/week). By including total energy intake in the models, we compared participants with similar energy intake but with different composition of the diet. Therefore, the HR for replacement of, for example, potatoes with other vegetables may be interpreted as the estimated difference in risk for a 500 g/week or 250 kcal/week higher intake of other vegetables and a concomitantly lower intake of potatoes for the same level of total energy intake. Model 1b included variables in model 1a plus established risk factors for MI: BMI (kg/m2), waist circumference (cm), length of elementary and secondary education (≤7, 8–10 and >10 years), smoking status (never, former, current smokers of <15, 15–25 or >25 g/d), leisure-time physical activity (< or ≥3·5 h/week), alcohol abstinence (yes, no), alcohol consumption (g/d), menopausal status (premenopausal, postmenopausal, unknown) (women only) and use of postmenopausal hormones (never, former, current) (women only). Model 2 included all variables in model 1b and potential dietary confounders for the investigated associations: fruits, unprocessed red meat, processed red meat, poultry, lean fish, fatty fish, lean dairy products, fatty dairy products, refined grains, whole grains, nuts, potato chips, sweets and soft drinks (all g/week). Model 3 included variables in model 2 and possible intermediate factors: history of hypertension (yes, no and do not know), history of hypercholesterolaemia (yes, no and do not know) and history of diabetes mellitus (yes, no and do not know). Adjustment for BMI, waist circumference and alcohol consumption was expanded beyond simple linear or categorical approaches to include flexible curves via restricted cubic splines (3 knots)(Reference Greenland23). As a sensitivity analysis, we also ran our models without adjustment for total energy intake. We furthermore ran stratified analyses by quintiles of energy-adjusted intake of other vegetables. We also tested for interaction by other vegetable intake by including an interaction term between other vegetable intake and each of the two food groups of interest in each substitution analysis. We used likelihood ratio tests to compare models with and without interaction terms in substitution models that included all exposures of interest (these models are equivalent to the models used in our main analyses(Reference Ibsen, Laursen and Würtz22)). The assumption of proportional hazards in the Cox models was investigated by graphical assessment and was found to be appropriate in all models.
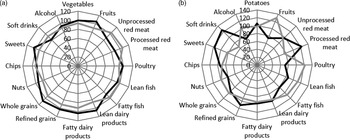
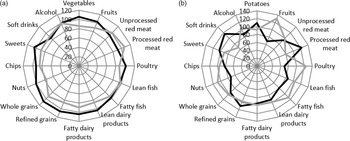
Differences in the underlying contributing dietary patterns were investigated using radar plots of energy-adjusted median intake of food and beverage groups (fruits, unprocessed red meat, processed red meat, poultry, lean fish, fatty fish, lean dairy products, fatty dairy products, refined grains, whole grains, nuts, potato chips, sweets, soft drinks and alcohol) by energy-adjusted extreme quintiles of intakes of potatoes or other vegetables. Energy-adjusted intake was calculated using the residual method(Reference Willett24). Sex-specific median intake of each food group was used as the common denominator to calculate percentage-wise deviations.
All analyses were performed with the use of Stata Statistical Software release 12 and 16 (Stata Corporation) at a two-tailed alpha of 0·05.
Results
Among the 57 053 participants recruited, 567 participants with a cancer diagnosis and 900 participants with a diagnosis of MI or cardiac arrest before baseline were excluded as well as 415 participants with incomplete questionnaires or missing anthropometric measurements. The final study population therefore included 55 171 participants (29 142 women and 26 029 men) with baseline characteristics given in Table 1. During a median follow-up time of 13·6 years for women and 13·5 years for men, 656 female and 1694 male cases with a diagnosis of MI were identified. The median energy-adjusted intakes of potatoes, other vegetables and subgroups of vegetables in g/week and kcal/week are shown in Table 2. Intake of potatoes contributed the most to the total vegetable intake, and cabbage contributed the least.
Table 1. Baseline characteristics of the study population in the Diet, Cancer and Health cohort
(Median and interquartile range; numbers and percentages)
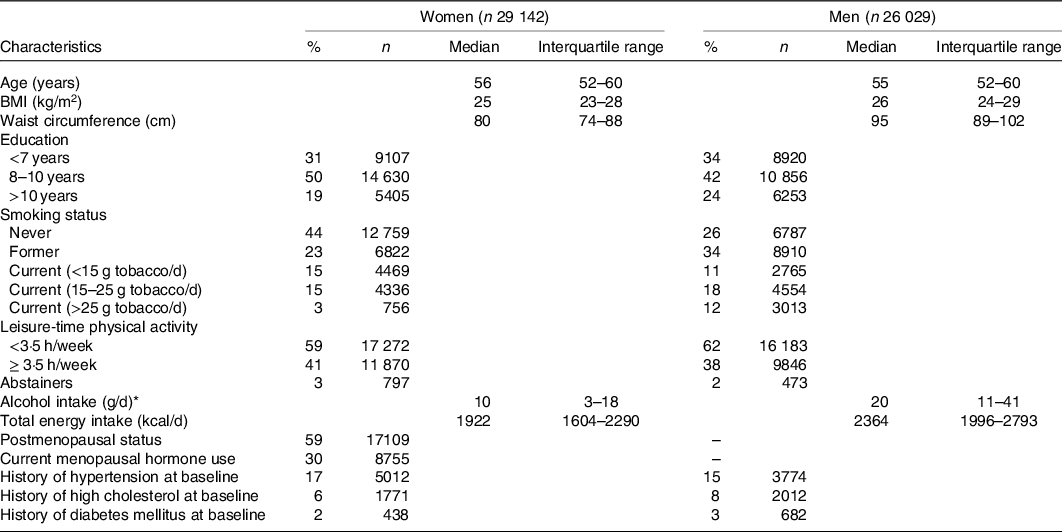
* Among users.
Table 2. Energy-adjusted intakes of potatoes and other vegetables in g/week and kcal/week among women and men in the Diet, Cancer and Health cohort
(Median and interquartile range)
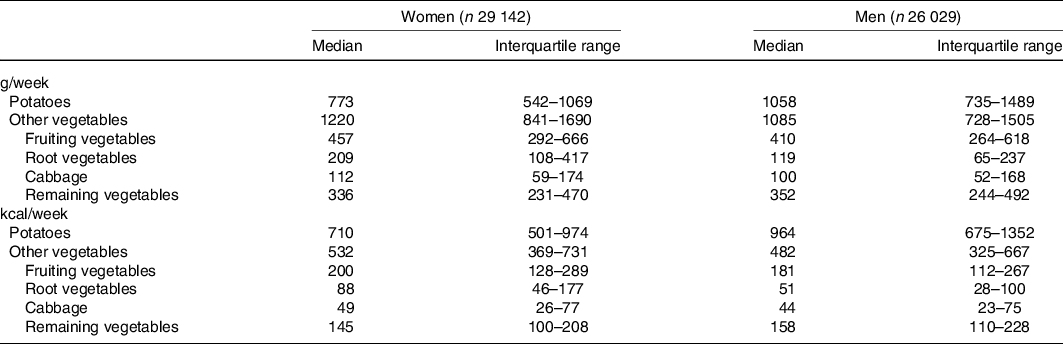
Table 3 shows HR and 95 % CI for MI associated with replacement of potatoes with other vegetables and substitutions between vegetable subgroups among women. After adjustments for established risk factors of MI, the associations were weak and not statistically significant (model 1b). The HR for MI associated with replacement of 500 g/week potatoes with other vegetables was 1·02 (95 % CI 0·93, 1·13). The HR for replacement of potatoes with fruiting vegetables was 0·93 (95 % CI 0·77, 1·13) and with other root vegetables 0·91 (95 % CI 0·77, 1·07). Direct but statistically non-significant associations were observed for a higher intake of cabbage replacing potatoes, fruiting vegetables or root vegetables. No substantial differences in the observed pattern of associations were found after additional adjustment for other foods (model 2) or after further adjustment for history of hypertension, hypercholesterolaemia or diabetes mellitus at baseline (results not shown). Weekly replacements in kcal are presented in online Supplementary Table S1, and the findings were similar to those in g/week.
Table 3. Myocardial infarction associated with substitutions between vegetable groups among women in the Diet, Cancer and Health cohort
(Hazard ratios (HR) and 95 % confidence intervals, n 29 142)
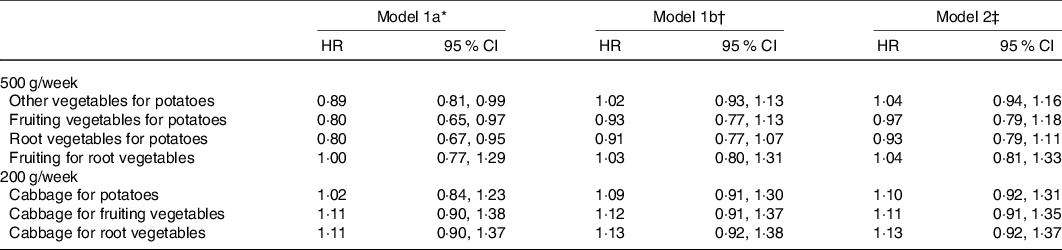
* Model 1a was stratified by age and date of enrolment and further adjusted for age and total energy intake (kcal). To explore the vegetable substitutions, we used the leave-one-out method (please see the Statistical Methods section for more details). For example, the substitution of other vegetables (fruiting vegetables, root vegetables, cabbage and remaining vegetables) for potatoes was specified in the statistical models by inclusion of other vegetables and the total sum of potatoes and other vegetables.
† Model 1b: as model 1a plus BMI, waist circumference, length of education, smoking status, physical activity, alcohol abstinence, alcohol intake, menopausal status and use of postmenopausal hormones.
‡ Model 2: as model 1b plus fruits, unprocessed red meat, processed red meat, poultry, lean fish, fatty fish, lean dairy products, fatty dairy products, refined grains, whole grains, nuts, potato chips, sweets and soft drinks.
Table 4 shows HR and 95 % CI for MI associated with replacement of potatoes with other vegetables and substitutions between vegetable subgroups among men in g/week. The associations were weak and not statistically significant after adjustment for established risk factors of MI (model 1b). Overall, the pattern of associations was found to be similar to that for women. Weekly replacements in kcal are presented in online Supplementary Table S2, and the findings were similar to those in g/week.
Table 4. Myocardial infarction associated with substitutions between vegetable groups among men in the Diet, Cancer and Health cohort
(Hazard ratios (HR) and 95 % confidence intervals, n 26 029)
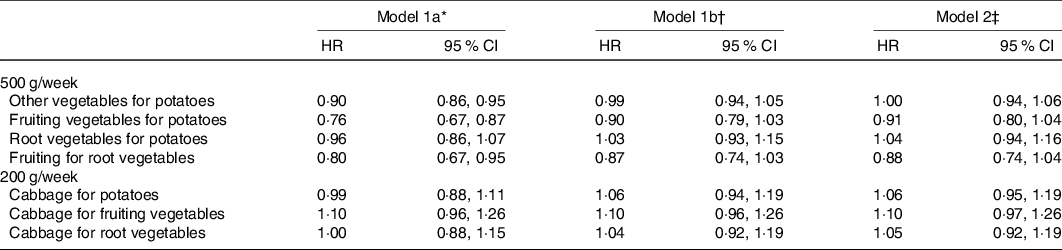
* Model 1a was stratified by age and date of enrolment and further adjusted for age and total energy intake (kcal). To explore the vegetable substitutions, we used the leave-one-out method (please see the Statistical Methods section for more details). For example, the substitution of other vegetables (fruiting vegetables, root vegetables, cabbage and remaining vegetables) for potatoes was specified in the statistical models by inclusion of other vegetables and the total sum of potatoes and other vegetables.
† Model 1b: as model 1a plus BMI, waist circumference, length of education, smoking status, physical activity, alcohol abstinence and alcohol intake.
‡ Model 2: as model 1b plus fruits, unprocessed red meat, processed red meat, poultry, lean fish, fatty fish, lean dairy products, fatty dairy products, refined grains, whole grains, nuts, potato chips, sweets and soft drinks.
The findings from substitution models in g/week without adjustment for total energy intake were similar to the models with adjustment for total energy intake (results not shown). We did not find indication of effect modification by other vegetable intake (see online Supplementary Tables S3 and S4).
Sex-specific radar plots of median intake of foods and beverages among participants within extreme quintiles of potato intake or extreme quintiles of other vegetable intake are presented in Figs. 1 and 2. In general, the eating patterns among women and men were similar. Participants in the highest quintile of potato intake consumed more unprocessed and processed red meat and less fruits, nuts, and lean dairy products compared with participants in the lowest quintile of potato intake. In contrast, participants in the highest quintile of other vegetable intake consumed more fruits, poultry, fish and nuts and less processed red meat, sweets and soft drinks compared with participants in the lowest quintile of other vegetable intake.
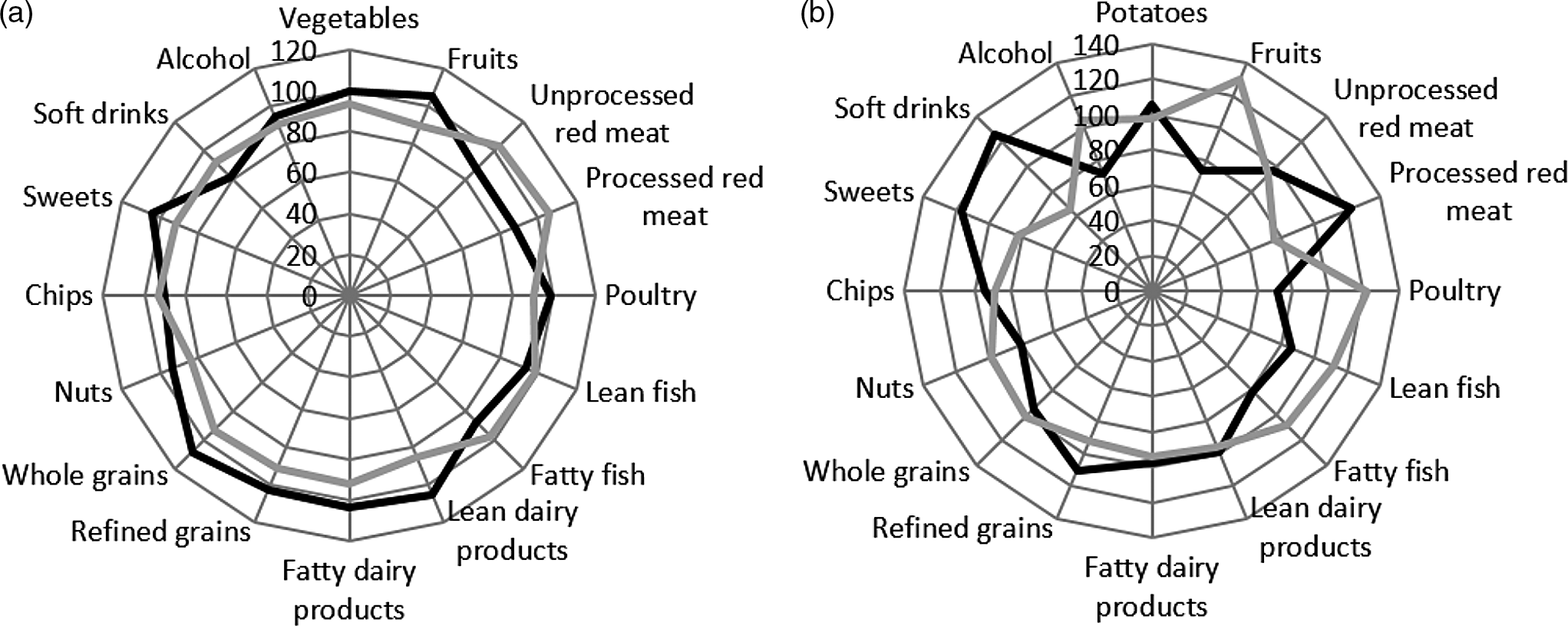
Fig. 1. Radar plots illustrating percentage-wise differences in intake of fifteen food and beverage groups by extreme quintiles of potato (panel a) or other vegetable (panel b) intake among women in the Diet, Cancer and Health cohort. Median intake of each food group was used as the common denominator to calculate deviations. If the relative intake of a food is above 100 %, it indicates a higher intake of that food compared with the median intake and vice versa when the relative intake is below 100 %. Intake of foods was adjusted for total energy intake. The black line indicates the first quintile of potato or other vegetable intake. The grey line indicates the fifth quintile of potato or other vegetable intake.
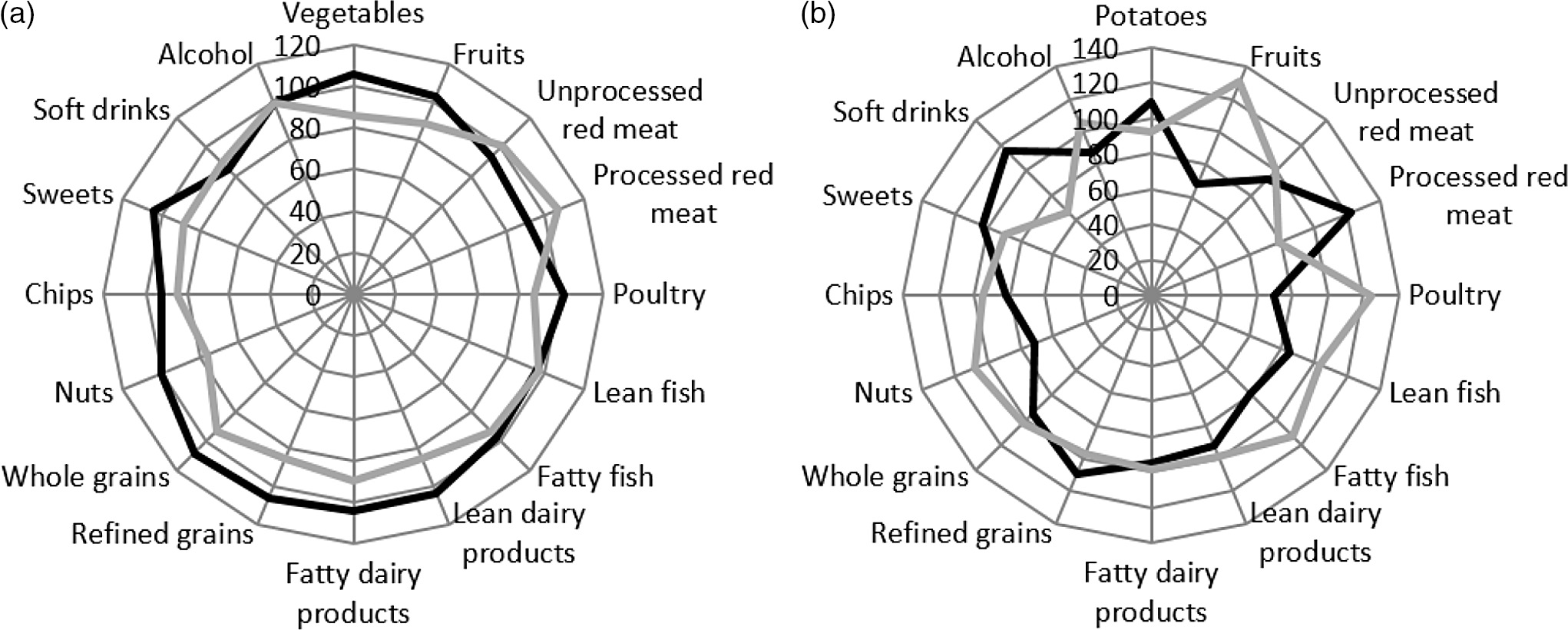
Fig. 2. Radar plots illustrating percentage-wise differences in intake of fifteen food and beverage groups by extreme quintiles of potato (panel a) or other vegetable (panel b) intake among men in the Diet, Cancer and Health cohort. Median intake of each food group was used as the common denominator to calculate deviations. If the relative intake of a food is above 100 %, it indicates a higher intake of that food compared with the median intake and vice versa when the relative intake is below 100 %. Intake of foods was adjusted for total energy intake. The black line indicates the first quintile of potato or other vegetable intake. The grey line indicates the fifth quintile of potato or other vegetable intake.
Discussion
In this cohort study including 2350 cases with a diagnosis of MI, we investigated whether a lower intake of potatoes replaced with a higher intake of other vegetables or replacements between subgroups of other vegetables was associated with the risk of MI. We observed that the associations between substitution of potatoes with other vegetables or vegetable subgroups and risk of MI were weak and statistically non-significant. Likewise, the associations of substitution between subgroups of other vegetables and risk of MI were weak and not statistically significant.
Main strengths of this population-based cohort study are the nearly complete follow-up (99·6 %), the large number of validated cases, the validated assessment of dietary intake and the detailed information about a wide range of potential confounders. The study population consisted of middle-aged subjects and was slightly overrepresented by participants of higher socio-economic status. We do, however, expect the direction of the investigated associations to be independent of socio-economic status. Information bias is unlikely to have affected the results as events of MI were identified by record linkage to the Danish National Patient Register and the Cause of Death Register, and diagnoses were established independently of the dietary information provided by the participants. Due to a low positive predictive value of the diagnosis unstable angina(Reference Joensen, Jensen and Overvad19), unstable angina was not included in the outcome definition. We used FFQ to assess the dietary intake, and this instrument may reflect the habitual diet(Reference Tjonneland, Olsen and Boll15,Reference Overvad, Tjonneland and Haraldsdottir16) . However, a potential source of random measurement error arises from dietary self-reporting. Also, the use of standard recipes to partly estimate intake of vegetables may be a potential source of random measurement error. The FFQs were completed between 1993 and 1997, and even though we do not expect most people between 50 and 64 years to change their diet substantially, the food market has changed during follow-up. The dietary habits of the study participants might also have changed, for example, due to awareness of the presence of cardiometabolic risk factors, and measurement error due to change in diet during follow-up cannot be excluded. For instance, study participants in high risk of developing MI might have shifted to a higher vegetable intake during follow-up.
Detailed control for established risk factors for MI attenuated the measures of association, and residual confounding cannot be excluded. Confounding from other MI risk factors not taken into account may also contribute to explaining the observed associations. Total energy intake was included as a covariate in all models. This implies that participants with similar total energy intake are compared. We also ran our models without adjustment for total energy intake and found comparable results. A high vegetable intake may be an indicator of a healthier eating pattern and a healthier lifestyle in general(Reference Thompson, Margetts and Speller25–Reference Imamura, Lichtenstein and Dallal27). The healthy eating pattern was confirmed in radar plots of selected foods and food groups among participants in the present study. Participants with the highest intake of vegetables other than potatoes also had the highest intake of fruits, poultry, fish and nuts and the lowest intake of processed red meat, sweets and soft drinks compared with participants with the lowest intake of other vegetables. In contrast, we did not observe a similar healthy eating pattern when comparing participants with the highest potato intake with participants with the lowest potato intake. In the substitution models, we therefore adjusted for the underlying eating pattern in additional multivariable models. Although results from models with and without additional adjustment for other foods must be interpreted differently, the pattern of associations were similar. In substitution models not adjusted for other dietary factors (model 1b), the underlying dietary pattern associated with different choices of potatoes or other vegetables is allowed to vary according to potato and other vegetable intake, whereas models adjusted for other dietary factors (model 2) restrict differences in other aspects of the diet composition. In relation to dietary guidelines in a public health perspective, we consider the results from model 1b most relevant as these take into account that a given food choice is naturally accompanied by intake of other foods. Among others, hypertension, hypercholesterolaemia and diabetes mellitus may be considered both as risk factors for MI and as intermediate factors in the causal pathway between vegetable intake and development of MI. However, a similar pattern of associations was observed after adjustment for these factors.
Several nutrients and bioactive components in vegetables such as dietary fibre, vitamins, minerals and phytochemicals have been suggested to have a beneficial effect on risk factors of MI, such as hypertension and inflammation(Reference Alissa and Ferns28,Reference Boeing, Bechthold and Bub29) . Potatoes are a source of vitamin C, K, Mg, fibre and polyphenols, but compared with most other vegetables, potatoes are also energy dense and have a high glycaemic index, although this may vary with preparation method(Reference Furrer14). Hence, a higher intake of other vegetables and a concomitant lower intake of potatoes may act through multiple mechanisms to reduce the risk of MI. However, we did not observe a lower risk of MI associated with substitution of other vegetables for potatoes.
Several cohort studies have examined the association between vegetable intake and risk of CHD while adjusting for total energy intake without specifying the replacement food. For total vegetables, the combined evidence from prospective studies shows an inverse association with CHD, although findings from the individual studies are heterogeneous(Reference Bechthold, Boeing and Schwedhelm5,Reference Aune, Giovannucci and Boffetta6) . For subgroups of vegetables, two recent meta-analyses have summarised the evidence for potatoes and found no association between potato consumption and CHD(Reference Aune, Giovannucci and Boffetta6,Reference Schwingshackl, Schwedhelm and Hoffmann12) . For other vegetable subgroups, no associations or inverse associations, especially for green leafy vegetables, were reported(Reference Aune, Giovannucci and Boffetta6). The heterogeneity between studies may be due to differences in the methodological approaches. As individuals usually change the dietary composition to maintain energy balance, a higher vegetable intake might replace other energy-providing foods in the diet which may have beneficial, neutral or detrimental effects with consequences for the interpretation of the study results. In the present study, substitutions between vegetable subgroups were not associated with risk of MI. However, the effects of substitution of vegetables may vary depending on the categorisation of the vegetables. We used a botanical categorisation but other classifications may be relevant to CHD risk such as the fibre content and glycaemic index of the vegetables. Substitutions were investigated in g/week and kcal/week. An advantage of investigating substitutions in g/week is the straightforward translation into food-based dietary guidelines, while investigation of substitutions in kcal/week is not easily translated. Substitution in kcal/week, however, has an isoenergetic interpretation, whereas substitutions in g/week may introduce an unspecified substitution of energy from other foods. The energy content of 200 g of, for example, cooked broccoli is 296 kJ, and the energy content of 200 g of, for example, boiled potato is 720 kJ(30). Thus, substituting the same absolute amount of cooked broccoli for potatoes is also followed by a higher intake of other foods. In the present study, however, the pattern of associations for g/week was similar to that for kcal/week.
In conclusion, this study found no benefits of replacing potatoes with other vegetables and no benefits of replacements between vegetable subgroups for prevention of MI. Thus, the study supports food-based dietary guidelines recommending to consume a variety of vegetables from all subgroups.
Acknowledgements
We thank the staff from the Danish Cancer Society who kindly provided the data necessary for our analysis. The Danish Diet, Cancer and Health cohort was approved by the regional ethical committees of human studies in Copenhagen and Aarhus and by the Danish Data Protection Agency.
This work is part of the project ‘Diet and prevention of ischemic heart disease: a translational approach’ (DIPI, www.dipi.dk), which was supported by the Danish Council for Strategic Research (today, Innovation Fund Denmark) (Contract 0603-00488B). This work was furthermore supported by the Graduate School of Health at Aarhus University and the Danish Cancer Society. The funding agencies had no role in the design, analysis or writing of this article.
The contributions of the authors were as follows: A. M. L. W., M. D. H., K. O. and M. U. J. designed the study; A. T. and K. O. collected the data; A. M. L. W. and M. D. H. were the principal investigators and performed the data analyses. A. M. L. W. and M. D. H. wrote the manuscript. A. T., E. B. S., E. B. R., K. O. and M. U. J. contributed to the data analysis and to the writing of the manuscript. All authors have read and approved the final manuscript.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521000349