Individual and combined effects of diet and physical activity on health
The disease burden of poor diet quality has globally increased during the last 30 years with more than 11 million deaths attributable to dietary risk factors in 2017(1). During this time, the development of nutritional epidemiology has been impressive(Reference Boeing2). A key contribution to this field has been the shift of focus from assessing isolated dietary factors to studying the effects of overall or complete dietary patterns. Dietary indices, constructed to measure adherence to specific dietary patterns as indicators of overall diet quality, have allowed epidemiologists to establish inverse associations between a healthy food pattern and multiple health outcomes(Reference Hu3). In this context, the Mediterranean dietary pattern (MedDiet) is internationally recognised as one of the best dietary strategies for the prevention of chronic diseases and premature death(Reference Schwingshackl and Hoffmann4–Reference Galbete, Schwingshackl and Schwedhelm7).
Physical inactivity is also a major and globally relevant determinant of health(Reference Guthold, Stevens and Riley8). There is abundant evidence of the effect of physical activity (PA) on health for the prevention of chronic diseases and premature mortality, whereas a lack of PA is a key risk factor for these health outcomes(Reference Loprinzi and Davis9–Reference Harridge and Lazarus12). It has been demonstrated that the replacement of PA or exercise with inactivity or sedentary behaviour will eventually adversely affect the ageing process, whatever the age of the individual. Even a simple indicator of PA, such as time spent sitting, is an independent predictor of mortality. The increase in risk of lifestyle and age-associated diseases are attributed to the decline in functional levels of many body systems and thus suboptimal maintenance of physiological functions in sedentary individuals(Reference Harridge and Lazarus12).
Moreover, diet and PA are two of the most frequently addressed modifiable lifestyle risk factors, which increase morbidity and mortality from lifestyle diseases, including CVD, obesity, type 2 diabetes and some cancers. Hand in hand, diet and PA are frequently recommended in clinical practice for general health promotion, weight loss or weight maintenance, chronic disease prevention, and increased quality of life(Reference Meulenberg13). Diet and PA are considered multidimensional variables that can influence each other(Reference Ding and Hu14). According to data from NHANES 2003–2006, US adults were 32 % more likely to eat a healthy diet if they met PA guidelines(Reference Piercy, Troiano and Ballard15). When considering the energy balance equation, diet (pertinent to energy intake) and PA (pertinent to energy expenditure) find themselves on either side of the equation, suggesting that both factors influence each other to maintain a healthy weight, possibly more so than the sources of energy themselves(Reference Ding and Hu14,Reference González-Muniesa, Mártinez-González and Hu16,Reference San-Cristobal, Navas-Carretero and Martínez-González17) .
The Mediterranean diet pyramid underlines the importance of PA and other lifestyle factors beyond diet(Reference Willett, Sacks and Trichopoulou18,Reference Berry, Lairon and Bach-Faig19) . Furthermore, existing evidence already suggests that greater adherence to both the MedDiet and PA is associated with better health biomarkers, lower risk of disease and lower mortality when compared with the MedDiet or PA alone(Reference Soltani, Jayedi and Shab-Bidar6,Reference Galbete, Schwingshackl and Schwedhelm7,Reference Loprinzi, Smit and Mahoney20–Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22) . A meta-review from nine systematic reviews and twenty-four meta-analyses concluded that the MedDiet may reduce the risk of non-communicable diseases, improve health status and reduce total lifetime healthcare costs, with a possibly even greater effect when combined with PA, as long as tobacco and excessive alcohol consumption are avoided(Reference Martinez-Lacoba, Pardo-Garcia and Amo-Saus21). Existing literature supports that a healthy MedDiet and PA may be more effective when acting in combination rather than separately, but questions remain on exactly how, to what extent, and to whom is this combined effect most beneficial to target interventions in public health. Little has been studied on the a priori analysis of the interaction between diet and PA to determine its impact on hard clinical events or mortality thus far(Reference Pronk, Anderson and Crain23,Reference Ding, Rogers and van der Ploeg24) . The existing studies have almost never quantified the synergism between diet and PA. More comprehensive, methodical, and robust evidence is needed to demonstrate that diet and PA are two sides of the same coin, as well as to identify to whom this combination may offer the greatest benefit in public health.
Interaction analysis for the potential synergism between the Mediterranean diet and physical activity
An interaction is defined as the situation in which the effect of one exposure on an outcome differs across the strata of another exposure, implying that the risk differences vary across strata of the other exposure. Thus, the presence of interaction suggests that the effect of the two exposures is different from the mere sum or multiplication of their individual effects, depending on the nature of the association between exposures and the assumed scale (additive or multiplicative) for the interaction. This interrelation of effects suggests that the reduction of either factor would also reduce the risk of the other factor in producing a given outcome(Reference Rothman, Greenland and Walker25). Different terminology is used throughout the scientific community to refer to the concept of interaction: joint effect or combined effect, synergy, interdependence, heterogeneity of effects, non-uniformity of effects, effect modification, or subgroup analysis(Reference de Mutsert, Jager and Zoccali26). For the purpose of this article, the term interaction will refer to the ‘mechanistic or biological interaction’ created when two potential causal risk factors participate in the same causal mechanism, which implies either synergism or antagonism between factors on disease risk or death(Reference Rothman, Greenland and Walker25,Reference Ahlbom and Alfredsson27) .
The current criteria within the Strengthening the Reporting of Observational Studies in Epidemiology guidelines recommend describing any methods used to examine interactions or subgroups within the statistical analysis section of the study methods(Reference von Elm, Altman and Egger28). However, many studies fall short of this recommendation(Reference de Mutsert, Jager and Zoccali26). In 2009, Knol et al. evaluated the presence of interaction in 225 epidemiological studies to examine how interaction was assessed and reported. This literature search found that not all studies that addressed effect modification or interaction provided satisfactory information on interactions between exposures (primarily treatments, medical conditions and lifestyle factors). Moreover, only one out of ten studies reported adequate information for a full assessment of additive or multiplicative interaction(Reference Knol, Egger and Scott29). This is important because an adequate reporting of methods allows for higher transparency, direct interpretation, comparison and independent recalculation of results(Reference Knol and VanderWeele30).
There are a variety of statistical approaches for considering interactions between potential causal factors. The most frequently reported method includes conducting a likelihood ratio test to compare regression models with and without the multiplicative interaction product term. However, this most common analysis of interaction on the multiplicative scale is limited to assessing statistical interaction. The current tendency among observational studies to simply report statistical significance of the likelihood ratio test on the multiplicative scale is due to the implicit nature of epidemiological statistical modelling and software convenience(Reference Ahlbom and Alfredsson27,Reference VanderWeele, Lash and Rothman31) . When obtaining relative risks, the inclusion of a product term in multivariable regressions provides a quick analysis for investigators to report interactions with a corresponding P-value, usually implying that a P-value < 0·05 for a product term (exposureA × exposureB) implies a departure from pure multiplication of effects. This method, however, disregards the possibility of detecting additive interactions and quantifying the effect attributed to the interaction. Contrary to the common practices in standard articles of epidemiology, according to Rothman, the information provided on the additive scale, including interaction analysis, is most relevant for public health application(Reference VanderWeele, Lash and Rothman31,Reference Knol, van der Tweel and Grobbee32) . Therefore, Knol et al. suggest using more extensive methods, including analyses for the single effects of each factor, joint effects for combinations of exposures, stratification, and measures of interaction on multiplicative and additive scales(Reference Knol and VanderWeele30).
Additive interaction analysis, on the absolute risk scale, estimates the number of attributable cases due to the combined effect. In the presence of interaction, these cases will either surpass or fall short of the sum of cases due to both exposures separately, suggesting that the excess of cases depends on the extent to which risk factors A (i.e. MedDiet) and B (i.e. PA) occur together in the same individuals. Moreover, relevant to public health, this analysis provides insights towards which subgroup of a population, not necessarily the high-risk subgroup, would observe a greater absolute risk reduction from disease prevention or intervention strategies(Reference Rothman, Greenland and Walker25,Reference de Mutsert, Jager and Zoccali26,Reference de Mutsert, de Jager and Jager33) . When two independent risk factors are considered well suited to fit an additive model, the presence of biological interaction requires a departure from additivity in the scale of absolute incidence rate differences(Reference Rothman, Greenland and Walker25,Reference Ahlbom and Alfredsson27) . However, study results in epidemiology are most frequently presented on the relative risk multiplicative scale, which does not directly allow calculating an absolute risk difference. Nevertheless, alternative measures of interaction to the absolute additive model have been available for decades, including the relative excess risk due to interaction (RERI), synergy index of additivity (SI) and attributable proportion (AP) due to interaction(Reference Knol and VanderWeele30,Reference VanderWeele, Lash and Rothman31,Reference VanderWeele34) . The null value for RERI and AP is 0 and SI is 1(Reference Andersson, Alfredsson and Källberg35). Derived from the regressions on the multiplicative scale, these measures of interaction on the additive scale indicate the direction, because it can be positive (synergism, beyond the sum of effects) or negative (antagonism, below the sum of effects), as well as the magnitude of the interaction(Reference Rothman36).
Reporting interactions on the additive scale is uncommon in standard epidemiological reports. Current explanations as to why interactions may not be reported in greater detail include space constraints, word limits or editorial intervention(Reference Knol, Egger and Scott29). For instance, one study included interaction analysis on both scales, employing a cross-product term on the multiplicative scale, and AP, RERI, and SI on the additive scale; however, the authors used brief descriptive statements to report that no interactions were found and the data were not shown(Reference Loprinzi, Smit and Mahoney20). Moreover, interactions on combined lifestyle factors are rarely a primary objective nor an initially intended analysis in most studies(Reference Loprinzi, Smit and Mahoney20,Reference von Elm, Altman and Egger28,Reference Edwards and Loprinzi37) . However, the inclusion of these analyses provides essential information on the potential public health impact and causal structure of combined effects of different relevant exposures(Reference Knol, Egger and Scott29). Thus, more research is needed that report data on interactions as part of the primary hypothesis evaluated.
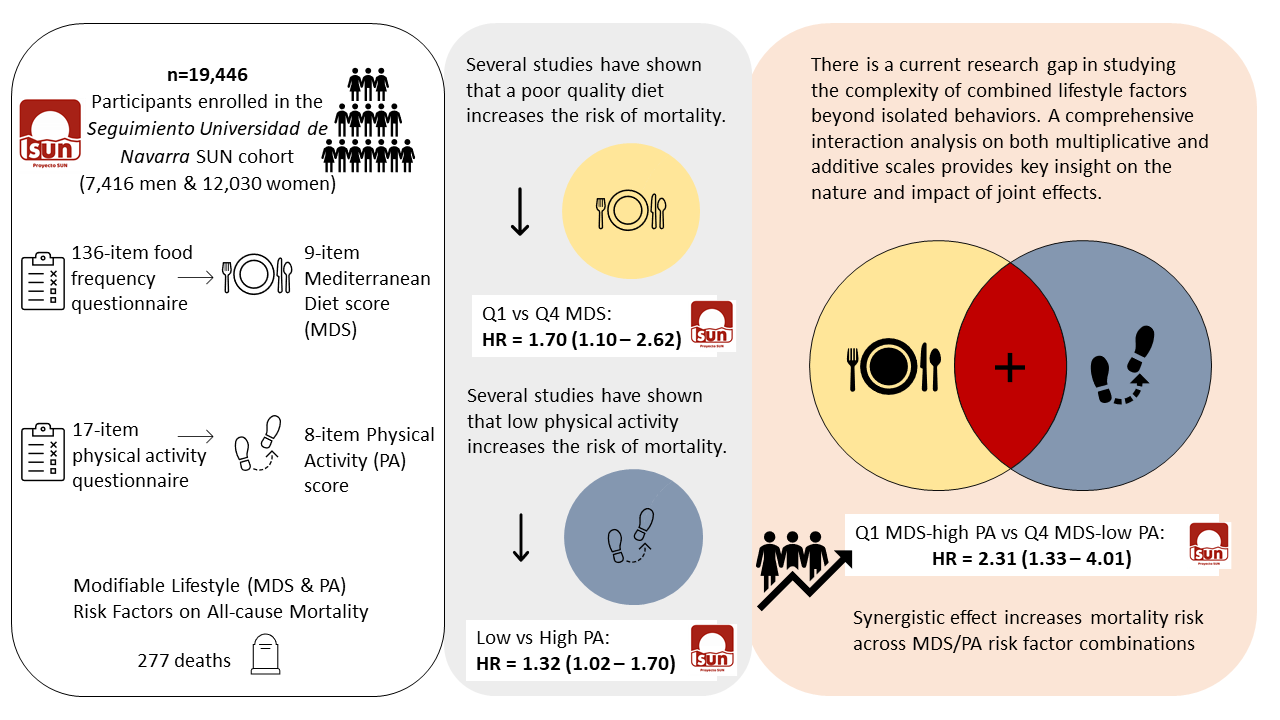
To demonstrate this research gap, we present the findings of a comprehensive review on reported interaction analyses between the MedDiet and PA on all-cause mortality, followed by an original analysis with the proposed methodology for a complete interaction analysis. The comprehensive review included original research that studied the MedDiet in combination with PA on mortality to identify the use of interaction analysis. Although we are not the first to study additive interactions between lifestyle factors, including diet and PA, to our knowledge there is no previous review that has focused on the additive interaction between the MedDiet and PA on all-cause mortality. Following this review, we provide a novel original analysis within a Spanish cohort, the Seguimiento Universidad de Navarra (SUN), to prospectively assess the joint association of the MedDiet and PA on all-cause mortality, applying both the multiplicative and additive interaction analyses for its relevance to public health.
Comprehensive review of reported interaction analyses for the Mediterranean diet and physical activity in association with mortality
We searched PubMed database for original observational research articles (in the last 10 years, English, and humans) that studied the combined effect of the MedDiet with PA on all-cause mortality, from the time when Knol and Vanderweele first published recommendations for presenting analyses of effect modification and interaction in 2012(Reference Knol and VanderWeele30). The search strategy and diagram can be found in Supplementary Table S1 and Fig. S1. We first identified the methods employed to assess the combination of diet and PA. Variations among studies included reporting relative risks for: a lifestyle score that included diet and PA items; a lifestyle score and its individual components; diet and a lifestyle score combined; diet and PA combined; or a lifestyle score, its individual components, and combinations of components. Since we were interested in accessing the presence of interaction analysis between the MedDiet and PA, we excluded all studies that did not specifically assess the relative risk for the combination of the MedDiet and PA on mortality(Reference Bonaccio, Di Castelnuovo and Costanzo38–Reference van den Brandt42). After these exclusions, only four articles met the inclusion criteria for assessment (Table 1)(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22,Reference Williamson, Polak and Simpson43–Reference Behrens, Fischer and Kohler45) .
Table 1. Summary table of the literature review conducted on the presence of interaction analysis for the combined effect between the MedDiet and PA on all-cause mortality
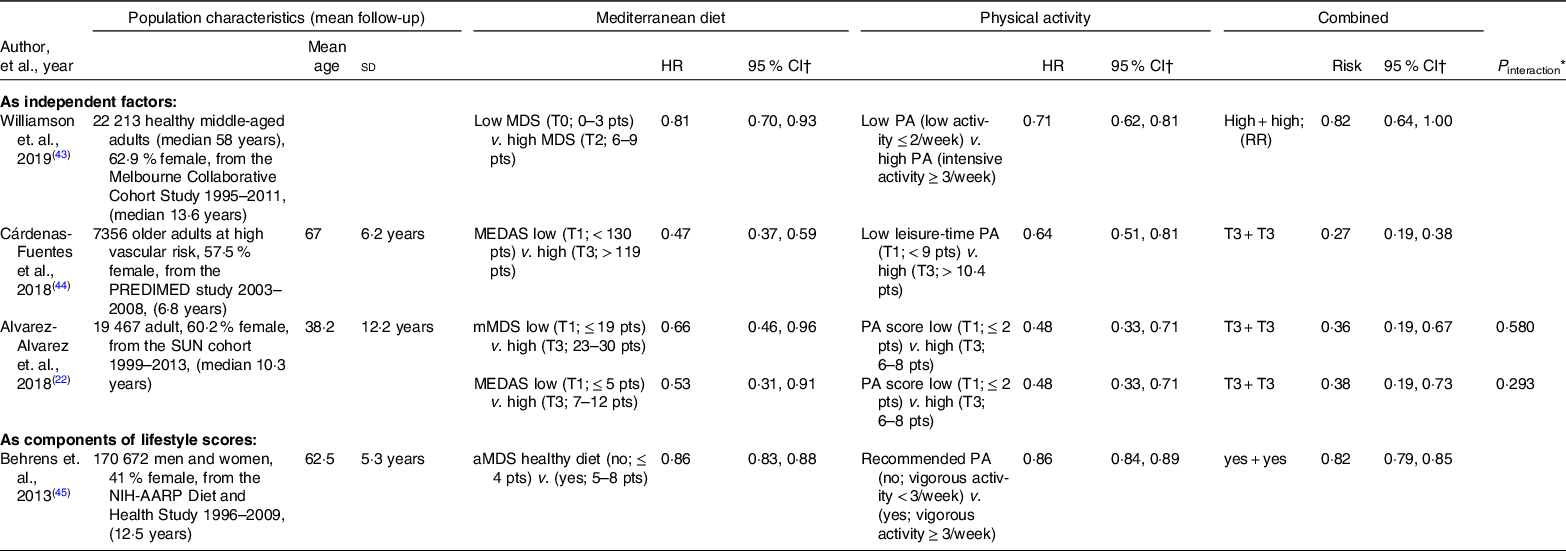
MedDiet, Mediterranean diet; PA, physical activity; HR, hazard ratio; RR, relative risk; MDS, Mediterranean diet score; pts, points; MEDAS, Mediterranean Diet Adherence Screener; mMDS, modified Mediterranean diet score; aMDS, alternate Mediterranean diet score; PREDIMED, Prevención con Dieta Mediterránea.
† HR provided are the multivariable-adjusted values.
* All interaction analyses reported were presented on the multiplicative scale.
Three articles studied diet and PA as individual factors on mortality(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22,Reference Williamson, Polak and Simpson43,Reference Cárdenas-Fuentes, Subirana and Martinez-Gonzalez44) ; meanwhile, one article included PA and diet as components of a lifestyle score and analysed the combined effect of diet and PA as a secondary analysis(Reference Behrens, Fischer and Kohler45). Three studies included the sample size and hazard ratios (HR) with 95 % CI for each combination(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22,Reference Cárdenas-Fuentes, Subirana and Martinez-Gonzalez44,Reference Behrens, Fischer and Kohler45) . The most recent article employed the parametric G-formula to estimate the relative risk associated with hypothetical interventions on the individual and combined effects of the Mediterranean-style diet and PA on all-cause mortality(Reference Williamson, Polak and Simpson43). Three articles assessed the MedDiet and PA in tertiles(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22,Reference Williamson, Polak and Simpson43,Reference Cárdenas-Fuentes, Subirana and Martinez-Gonzalez44) , whereas the other used dichotomous variables(Reference Behrens, Fischer and Kohler45). The diverse cut-off points indicated great heterogeneity for the categorisation of exposures, reinforcing categories are subject to the available data(Reference Haneuse and Rothman46). All four articles presented the combination of the MedDiet and PA as protective factors and observed relative risk reductions on all-cause mortality (Table 1). Graphical representations of the joint effects and measures of interaction varied across studies, including a contingency table, multidimensional histogram and relative risk tables for various combinations of lifestyle factors.
Only one article by Alvarez-Alvarez et al. reported P-values for the possible interaction between the MedDiet and PA on all-cause mortality(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22). The two reported measures of interaction in this article were obtained for two different scores of adherence to the MedDiet and were conducted on the multiplicative scale by incorporating an interaction term in the Cox proportional hazards model. Alvarez-Alvarez et al. observed a synergistic, but not significant, multiplicative interaction between a modified Mediterranean diet score and PA (P interaction = 0·580), as well as between a Mediterranean Diet Adherence Screener (MEDAS) and PA (P interaction = 0·293). Thus, the interpretation of the combined effect of both lifestyle factors was the existence of a synergistic interaction, beyond additivity, but not beyond multiplicativity, equivalent to the mere multiplication of relative effects(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22).
Despite the absence of an interaction analysis, Williamson et. al presented measures of association on the risk difference (additive) scale and measures of impact, in addition to the relative risk (multiplicative) scale. The combined hypothetical repeated intervention estimated an absolute reduction in all-cause mortality of 1·82 deaths per 100 people (95 % CI 0·03, 3·6). Moreover, when the authors considered an intervention only on participants with obesity, the overall risk differences and risk ratios were closer to the null, suggesting that a greater absolute effect would be obtained by intervening on the general population(Reference Williamson, Polak and Simpson43). A comprehensive interaction analysis would have further addressed the mechanism behind the observed joint effect, which suggested a potential synergism in the Melbourne Collaborative Cohort Study, with 22 213 middle-aged participants. This comprehensive review sheds light on the absence of reported interaction analyses and the research gap that exists between the frequently reported measures of association (i.e. relative risks) and less common absolute measures of association and impact for public health.
Mediterranean diet and physical activity on all-cause mortality in the Seguimiento Universidad de Navarra cohort
One of the above-mentioned studies, which assessed the combined effect of the MedDiet and PA on all-cause mortality, was nested in the SUN cohort. The SUN project is a prospective, multipurpose, cohort of Spanish university graduates, with continually open recruitment (i.e. a dynamic design), consisting of a baseline questionnaire and biennial follow-up questionnaires. Participants’ informed consent was given upon completion of the baseline questionnaire. All participants are university graduates, ensuring greater reliability, validity and retention rates associated with education status. The SUN project has been approved by the Institutional Review Board of the University of Navarra and registered at clinicaltrials.gov (NCT02669602). Further explanation of this study’s objective, design and methods has been published previously(Reference Seguí-Gómez, de la Fuente and Vázquez47,Reference Carlos, De La Fuente-Arrillaga and Bes-Rastrollo48) .
In the previous study by Alvarez-Alvarez et. al., a descriptive evaluation of the relation between the MedDiet and PA showed that physically active participants had lower BMI and adhered better to the MedDiet by consuming more vegetables, fruits, legumes, cereals, fish and nuts, but less red and white meat. The authors calculated an eight-item active lifestyle score as a proxy of PA that considered the volume, intensity and frequency of leisure-time physical activities and sedentary behaviour (i.e. exercise, walking, climbing stairs, watching television and sitting). They found that participants who engaged in a more physically active lifestyle (6–8 points) and also presented higher adherence to the modified Mediterranean diet score (23–30 points) showed a 64 % relative reduction (HR = 0·36; 95 % CI 0·19, 0·67) on all-cause mortality compared with participants in the lowest category of PA and MedDiet. In addition, high adherence (7–9 points) to MEDAS in combination with high PA (6–8 points) was associated with a 61 % decreased relative risk of all-cause mortality (HR = 0·39; 95 % CI 0·21, 0·72) compared with the lowest adherence to PA and MedDiet category(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22,Reference Trichopoulou, Costacou and Bamia49) . These observations and joint effects suggested the interrelationship between these two lifestyle factors and the potential interaction that may drive a greater risk reduction on all-cause mortality than the individual effects of diet or PA alone.
Alvarez-Alvarez et al. tested the potential synergism between the MedDiet and PA using a likelihood ratio test, comparing Cox proportional hazards models with and without the interaction product term created by the MedDiet and PA. P–values for multiplicative interaction were not statistically significant for neither the modified Mediterranean diet score (P = 0·580) nor MEDAS (P = 0·293). Therefore, their combined effect was inferred to only have synergistic effects on mortality risk reduction, but not beyond multiplicativity(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22). This interpretation, nonetheless, should be further assessed with appropriate statistical methods. Hence, this initial joint effect analysis provided the foundation for the following comprehensive assessment of interactions in search of a clearer understanding of the nature between these two lifestyle factors which are so frequently combined.
Comprehensive interaction analysis in the Seguimiento Universidad de Navarra cohort
From December 1999 to August 2020, a total of 22 893 participants had been recruited for the SUN cohort. After exclusions, a total of 19 446 participants, consisting of 7416 men and 12 030 women (61 %), were included in the present analysis (online Supplementary Fig. S2). Dietary data in the SUN cohort were collected using a validated 136-item semiquantitative FFQ at baseline(Reference Martin-Moreno, Boyle and Gorgojo50,Reference de la Fuente-Arrillaga, Vázquez Ruiz and Bes-Rastrollo51) . For our analysis, Trichopoulou’s operational definition of the MedDiet, a nine-item Mediterranean diet score (MDS) in which each item scored 0 or 1 point, assessed adherence to the MedDiet(Reference Trichopoulou, Costacou and Bamia49). Additionally, a seventeen-item PA questionnaire collected at baseline inquired about the frequency and time dedicated to leisure-time physical activities, sports and sedentary behaviour(Reference Martínez-González, López-Fontana and Varo52). PA was measured with an eight-item a priori defined index with final scores ranging between 0 and 8 points(Reference Alvarez-Alvarez, Zazpe and Pérez de Rojas22). PA items included exercise (yes and no), intensity (moderate and vigorous), Metabolic equivalent of task-h/week (< 16·1 and ≥ 16·1), walking speed (low/normal and brisk/fast), walking time (< 0·5 h/d and ≥ 0·5 h/d), climbing upstairs (< 3 floors/d and ≥ 3 floors/d), television viewing time (≥ 1·5 h/d and < 1·5 h/d) and sitting time (≥ 5 h/d and < 5 h/d). These exposures, traditionally presented as protective factors, were transformed and presented as risk factors by recommendation of Knol et al. when conducting interaction analyses on the additive scale(Reference Knol, Vanderweele and Groenwold53). Thus, MDS scores were presented as quartiles (Q4: high adherence to Q1: low adherence) and PA scores were dichotomised into categories of high (4–8 points) and low (0–3 points) activity levels. This categorisation of each exposure identified the most appropriate distribution of individuals with differentiated MedDiet adherence and PA level. Combinations of both exposures were created with a contingency table for quartiles of MDS and dichotomous PA.
After a median follow-up of 12 years (±4·5 sd), a total of 277 deaths (including 9 (3·25 %) deaths with unconfirmed cause) were observed. Deaths were confirmed by death certificates and medical records sent by next of kin or computerised record linkage to the Spanish National Statistics Institute (INE, www.ine.es). The date and cause of death were recorded and encoded using the International Classification of Diseases (ICD-10). Follow-up for each participant was calculated from the date the baseline questionnaire was returned to the date the last questionnaire was received or the reported date of death.
A multivariable statistical analysis was conducted using a Cox regression model for the assessment of individual and combined effects between adherence to the MedDiet and PA on all-cause mortality. Age was the underlying time variable, and all Cox regression models were stratified by age in decades (seven categories) and the year in which participants entered the study (six categories). Multivariable-adjusted HR were adjusted for sex, BMI (five categories), education level (bachelor’s degree/masters or doctorate), smoking status (never, active and former smoker), cigarettes smoked (packs/d-year), alcohol consumption (continuous), total energy intake (continuous), family history of CVD, prevalent hypertension, hypercholesterolemia and history of depression at baseline (ever/never). Individual exposures were additionally adjusted for the remaining lifestyle factor. Linear trend tests were performed by assigning medians to each category and treating it as a continuous variable.
Interactions were analysed according to the methodology proposed by Knol and Vanderweele by studying the single and joint effects of the exposures followed by an interaction analysis on both the multiplicative and additive scales(Reference Knol and VanderWeele30,Reference Vanderweele and Knol54) . Knol et al. made particular emphasis that protective factors should be recoded as risk factors, selecting the reference group as those not exposed to either risk factor, representing the lowest risk on the given outcome, for the correct calculation of RERI(Reference Knol, Vanderweele and Groenwold53). On the multiplicative scale, a likelihood ratio test compared Cox regression models with and without a product term for the lowest MDS and low PA level. On the additive scale, the lowest MDS quartile and low PA category were employed for calculating the RERI, as well as the AP due to interaction (online Supplementary Table S4).
All P-values < 0·05 were considered statistically significant. All statistical analyses were conducted using STATA version 14 (StataCorp).
Understanding how diet and physical activity interact on mortality in the Seguimiento Universidad de Navarra cohort
Descriptive baseline characteristics for our final study population are described by means and standard deviation or percentage in Supplementary Table S2. As expected, our final study population from the SUN cohort further demonstrated the interrelatedness between dietary and PA habits. Those with higher levels of PA exhibited slightly higher MDS, greater total daily energy intake with a greater percentage from carbohydrates, higher intakes of fibre, vegetables, fruits, cereals, fish, dairy products and nuts, as well as lower percentage of total energy intake from fat and lower meat consumption compared with participants with a low PA level. On the other hand, those with higher adherence to the MDS showed slightly higher PA scores, more frequent exercise, higher weekly energy expenditure, faster walking pace, more minutes walking per d, climbed more stairs and spent fewer hours sitting per d as compared with participants with lower MDS adherence. Supplementary Table S3 shows the frequency of points awarded to each item of the MDS and PA scores. Statistically significant differences were observed across categories of the opposite lifestyle factor, with the exception of dairy product consumption and monounsaturated to saturated fat ratio between PA levels (P > 0·05). These differences suggest that a greater adherence to the MDS is associated with a greater PA level and vice versa.
The main causes of death included cancer (53·8 %) and CVD (18·4 %) with a mean age at death of 61 years. As shown in Table 2, each protective factor as a continuous variable was associated with a statistically significant decreased risk on all-cause mortality. Additionally, poorer adherence across quartiles of the MDS and a low level of PA showed statistically significant increased risks of mortality compared with the highest MDS adherence quartile and the high PA category, (Q1 HR = 1·70; 95 % CI 1·10, 2·62) (HR = 1·32; 95 % CI 1·02, 1·70), respectively. The joint effect of the lowest MDS adherence with low PA showed an even greater increased risk (HR = 2·31; 95 % CI 1·33, 4·01) compared with the highest MDS and high PA combination (Table 2). As represented in Fig. 1, this joint association showed a linear increasing trend as MDS and PA combinations worsened (P for trend < 0·001).
Table 2. Prevalence, individual and joint effects (HR), and measures of interaction on multiplicative and additive scales between adherence to the MedDiet and PA on all-cause mortality
(Numbers and percentages; hazard ratios and 95 % confidence intervals)

HR, hazard ratio; MedDiet, Mediterranean diet; PA, physical activity; n, sample population size; MDS, Mediterranean diet score; pts: points.
* Adjusted for sex, BMI, education level, smoking status, cigarettes smoked, alcohol, total energy intake, family history of CVD, prevalent hypertension, hypercholesterolemia, depression, and stratified by year entering the cohort and age in decades. Individual exposures were additionally adjusted for the remaining lifestyle factor.
† Variables are presented as risk factors.

Fig. 1. HR (95 %CI) for the combinations of adherence to the MedDiet and PA levels on all-cause mortality. MedDiet, Mediterranean diet; PA, physical activity; HR, hazard ratios.
The joint effect analysis suggested a potential synergism between the two independent variables. This finding was supported by the comprehensive interaction analysis for the doubly exposed category, which observed a RERI coefficient greater than 0 for the point estimate, although it had wide CI and it was not statistically significant (RERI = 0·46; 95 % CI −0·83, 1·75). An additional analysis to increase statistical power was conducted with continuous risk factors, yet no statistical significance was observed (RERI = 0·21; 95 % CI −0·03, 0·07). Table 2 shows that 36 % of the joint effect was attributed to the interaction, whereas low MDS and low PA accounted for 47 % and 16 %, respectively. Lastly, no multiplicative interaction was detected in this analysis since the comparison of regression models with and without a multiplicative interaction term did not observe statistical significance (P = 0·73). Our results indicated the joint association between the lowest adherence to the MDS (Q1) and low level of PA (0–3 pts) on all–cause mortality most likely involves an interaction beyond additivity, but below multiplicativity.
The potential synergism between the MedDiet and PA, as risk factors for premature mortality, may be explained in part by the complex dynamic balance between energetic intake and energy expenditure, in addition to a wide array of other biological mechanisms(Reference Navas-Carretero, San-Cristobal and Alvarez-Alvarez55). Energy intake exceeding energy needs has been associated with an increased mortality risk(Reference Lassale, Hernáez and Toledo56). Both a healthy diet and adequate PA maintain body weight and composition through interconnected pathways regulated by the neural and endocrine systems(Reference González-Muniesa, Mártinez-González and Hu16). Moreover, a high-quality diet, represented by higher adherence to the MedDiet, has been associated with benefits regarding lipid oxidation(Reference Fitó, Guxens and Corella57), HDL function(Reference Hernáez, Castañer and Elosua58), insulin sensitivity(Reference Mirabelli, Chiefari and Arcidiacono59), endothelial function(Reference Storniolo, Casillas and Bulló60), inflammation(Reference Aleksandrova, Koelman and Rodrigues61,Reference Razquin and Martinez-Gonzalez62) and telomere length(Reference Canudas, Becerra-Tomás and Hernández-Alonso63), suggesting potential biological mechanisms for a lower risk of mortality(Reference Sotos-Prieto, Bhupathiraju and Mattei5). Similarly, regular exercise alleviates the negative effects caused by free radicals, reducing the risk of sarcopenia, insulin resistance, chronic disease, and consequently, premature death(Reference Simioni, Zauli and Martelli64). Thus, the detrimental effects of inadequate nutrition and lack of PA, which increase morbidity and mortality from lifestyle diseases, are most likely due to an energy imbalance, the modification or disruption of regulatory processes, and harmful effects caused by inflammation and oxidative stress on health.
Furthermore, the absolute measures presented, RERI and the AP due to interaction, provide informative estimates regarding the impact of the joint effect. The effect of the interaction varies according to the prevalence of the two exposures and the outcome within a given subgroup. Hence, the public health implications of the MedDiet and PA depend on the proportion of the population in which these factors occur jointly(Reference Rothman, Greenland and Walker25). The greater the number of subgroups, the fewer cases of mortality correspond to each combination, the smaller the effect observed from the interaction. According to our data, which observed increased relative risks as lifestyle factor combinations worsened, surpassing the risks of the individual factors, we quantified the effect due to the interaction was 36 % of the total joint effect. Hence, the subgroup with low MedDiet adherence and low PA would benefit from an intervention targeting both habits simultaneously to reduce the risk posed by this synergism. This subgroup received three or less points for both the MDS and PA scores, indicative of individuals with ample room for improvement in many possible aspects of diet and PA compared with the rest of the study population. Similarly, from a more applicable perspective to public health, increasing risk reductions were observed across combinations of MDS and PA on protective scales (online Supplementary Table S5 and Fig. S3). Although quantifying the interaction requires transforming healthy lifestyle factors into their corresponding risk factors, the observed joint effect of adhering to the MedDiet and PA, greater than the sum of the effect of each individual lifestyle habit, offers a more translatable message to the public.
Strengths of this analysis include the large population size, long follow-up, adjustment for numerous potential confounders and greater validity of self-reported data from an educationally homogenous population of university graduates. Nevertheless, considering a multivariable analysis requires a large sample size, an interaction analysis requires an even greater sample size and, therefore, the AP due to interaction may add strength to the RERI estimate. Although the remaining cases of mortality were few after exclusions were applied, a recent meta-analysis showed that the association between a healthy lifestyle and all-cause mortality was stronger in studies with longer follow-up or among younger participants, indicating larger benefits could be obtained if people adopt healthy lifestyles at an early age and follow for a long time(Reference Zhang, Pan and Chen65). Although we may not have had the sufficient statistical power for a more robust interaction analysis, the power to detect interactions tends to be greater on the additive scale than the multiplicative scale when the main effects are positive(Reference VanderWeele66,Reference VanderWeele67) . In addition, the primary limitations posed by measuring long-term habitual patterns of dietary intake and PA from self-reported measurements include residual confounding due to variations in habits over time and recall bias(Reference Willett68). Furthermore, our analysis employed baseline data, whereas an analysis with repeated measures may detect associations and interactions between decreased adherence to the MedDiet and PA over time. Lastly, our results should be interpreted with caution due to the use of recoded variables as risk factors (i.e. non-adherence to the MedDiet rather than high adherence and physical inactivity rather than PA), which may not infer the same results for exposures in their preventive form(Reference Knol, Vanderweele and Groenwold53). The categorisation of exposures may be debatable given the irregular distribution of participants; however, the biological relevance and case distribution were considered to present the most appropriate analysis(Reference Haneuse and Rothman46).
As previously mentioned, measures of interaction are commonly non-significant and considered unnecessary to authors and therefore are often not presented(Reference Knol, Egger and Scott29). One of the main methodological reasons for the absence of statistically significant interaction terms previously acknowledged and the reason for underreporting interaction analyses is the lack of statistical power to detect RERI and reduce type II error(Reference VanderWeele66,Reference VanderWeele67,Reference Li and Chambless69) . Both follow-up duration and sample size should be considered when conducting additive interaction analysis, provided that the detection of causal interactions may depend on the progression of time and more precise estimates may require very large study populations(Reference VanderWeele70). This frequent concern may be solved in part by calculating the AP due to interaction, which does not solely rely on statistical significance, making it a valuable measure of interaction(Reference VanderWeele34). Furthermore, statistical significance for interactions is frequently established at P < 0·10, rather than P < 0·05, due to the limitations of statistical power(Reference Greenland71).
Significance of studying interactions between lifestyle factors
Just as the MedDiet and PA have been studied as the combined effect created by their individual components, such as a priori defined dietary patterns rather than single food groups or foods, lifestyle can be assessed by studying specific combinations of behaviours(Reference Hu3,Reference Loprinzi and Davis9,Reference Martínez-González and Gea72,Reference McAloney, Graham and Law73) . This methodology was anticipated by Rothman, who stated ‘as more causal factors are associated with health outcomes, greater interest will be given to the joint effects created by combinations of exposures’(Reference Rothman74). More and more lifestyle scores, including simple scores, Life’s Simple 7 (LS7) and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) score, encompass a healthy dietary pattern complemented by PA, other lifestyle habits and cardiometabolic parameters to define a larger concept of lifestyle(Reference Prinelli, Yannakoulia and Anastasiou41,Reference Zhang, Pan and Chen65,Reference van Dam, Li and Spiegelman75–Reference Ruiz-Estigarribia, Martínez-González and Díaz-Gutiérrez77) . A recent meta-analysis observed the risk reductions for all-cause and CVD mortality related to LS7 were similar or even weaker compared with the simple score, indicating that more emphasis should be given to lifestyle factors, in addition to cardiometabolic markers, for the prevention of premature deaths(Reference Zhang, Pan and Chen65). In addition to studying the global effect of a lifestyle score, studying combinations of lifestyle factors is relevant for understanding the impact these multifaceted and interrelated habits have on individual and population health. These studies provide key insight for implementing successful multicomponent lifestyle interventions(Reference Hamer, Bates and Mishra78–Reference Gong, Zhang and Wang82). Consequently, studying the conjoint effect of diet and PA is especially relevant given the current research gap between the effects of individual factors and the complexity of an overall lifestyle.
Not only the MedDiet and PA but other lifestyle factors as well should be studied in combination with each other to understand the interaction between multifactorial causes of disease and mortality and create effective guidelines for general, at risk, and diseased populations. Translating the findings of an interaction analysis into a public health message, however, is difficult. Future strategies will require educating health professionals on the synergism between lifestyle factors to communicate the synergistic health benefits to patients. There are considerable limitations when asking a dietitian to speak on PA or a PA expert to speak on diet, let alone other lifestyle factors. Thus, clinicians should be specifically trained to discuss lifestyle factors as proposed by Frates et al.(Reference Frates, Bonnet and Joseph83) This issue is similar at the public health level, we need to better combine the dietary guidelines with PA guidelines in a more integrative manner, such as the Dietary Guidelines for Americans(84) and the Physical Activity Guidelines for Americans(85). These recommendations must be supported by long-term policies, communication and implementation strategies across sectors(Reference Ding, Mutrie, Bauman and Pratt86).
Provided that chronic disease affects all aspects of health and the combination of poor diet and PA may play a greater role in the burden from chronic disease, more so than overall mortality, future research should study cause-specific mortality, premature mortality and death free of chronic disease, including CVD, diabetes, cancer and the metabolic syndrome(87,Reference Lee, Walker and Bourdillon88) . Research in this line has already been devised and conducted with network analysis (analysis of regularities or patterns of interaction within the network) to understand the multiple connections between associations of healthy ageing. In a similar manner to studying biological interactions, this methodology has been used to focus on the meaning of the interactions between aspects of health and vitality along the path that leads to frailty and its adverse consequences, and how they change over time(Reference Aliberti and de Oliveira89). Complementary to the presently suggested interaction analysis, network analysis may also contribute to the research gap regarding the pathways involved in interactions with the MedDiet in the field of public health(Reference Luke and Harris90).
In conclusion, this article addresses the current research gap regarding interaction analyses reported for the combination of the MedDiet and PA, beyond individual and joint measures of association, and presents an original analysis within the SUN cohort. Our analysis focused on quantifying the interaction between the MedDiet and PA; however, more studies are needed to study other dietary patterns for greater generalisability and a meta-analysis of the effect attributed to the interaction would provide further evidence. Similar to studying an overall dietary pattern as a cumulative effect of several individual components, lifestyle indices are used to study the cumulative effect of individual behaviours. Nevertheless, the mechanism by which these individual components interact is complex, suggesting the use of interaction analysis as an essential statistical method to complement frequently reported joint effects. Our analysis in the SUN cohort suggested a synergism between low adherence to the MDS and low level of PA on all-cause mortality. While quantifying the synergism between the MedDiet and PA focuses on one interaction among many possible lifestyle interactions, this methodology and network analysis may be advantageous towards understanding the potential synergism between multiple lifestyle factors. More studies on interactions are needed to fill this gap in nutritional epidemiology and provide high-quality evidence as interest grows in studying overall lifestyle patterns on health.
Acknowledgements
The authors other members of the SUN Group: Aguilera-Buenosvinos I, Alonso A, Álvarez-Álvarez I, Balaguer A, Barbería-Latasa M, Barrio-López MT, Basterra-Gortari FJ, Battezzati A, Bazal P, Benito S, Bertoli S, Bes-Rastrollo M, Beunza JJ, Buil-Cosiales P, Carlos S, de Irala J, de la Fuente-Arrillaga C, de la O V, de la Rosa PA, Delgado-Rodríguez M, Díaz-Gutiérrez J, Díez Espino J, Domínguez L, Donat-Vargas C, Donazar M, Eguaras S, Fernández-Lázaro CI, Fernández-Montero A, Fresán U, Galbete C, García-Arellano A, Gardeazábal I, Gea A, Gutiérrez-Bedmar M, Gomes-Domingos AL, Gómez-Donoso C, Gómez-Gracia E, Goñi E, Goñi L, Guillén F, Hernández-Hernández A, Hershey MS, Hidalgo-Santamaría M, Hu E, Lahortiga F, Leone A, Llavero M, Llorca J, López del Burgo C, Marí A, Martí A, Martín-Calvo N, Martín-Moreno JM, Martínez JA, Martínez-González MA, Mendonça R, Menéndez C, Molendijk M, Molero P, Muñoz M, Navarro AM, Pano O, Pérez de Ciriza P, Pérez-Cornago A, Pérez de Rojas J, Pimenta AM, Ramallal R, Razquin C, Rico-Campà A, Romanos-Nanclares A, Ruiz L, Ruiz-Canela M, San Julián B, Sánchez D, Sánchez-Bayona R, Sánchez-Tainta A, Sánchez-Villegas A, Santiago S, Sayón-Orea C, Toledo E, Vázquez Z and Zazpe I. We especially thank all participants in the SUN cohort for their long-standing and enthusiastic collaboration and our advisors from Harvard TH Chan School of Public Health Walter Willett, Alberto Ascherio, Frank B. Hu and Meir J. Stampfer who helped us design the SUN project, the Prevención con Dieta Mediterránea (PREDIMED) study and the PREDIMED-PLUS ongoing trial.
The SUN project has received funding from the Spanish Government-Instituto de Salud Carlos III, and the European Regional Development Fund (FEDER) (RD 06/0045, CIBER-OBN, Grants PI10/02658, PI10/02293, PI13/00615, PI14/01668, PI14/01798, PI14/01764, PI17/01795, PI20/00564 and G03/140), the Navarra Regional Government (27/2011, 45/2011, 122/2014), and the University of Navarra. MSH receives financial support from the Programa de Ayudas de la Asociación de Amigos de la Universidad de Navarra.
M. R. C. and J. A. M. formulated the research question, M. A. M. and M. R. C. designed the study, M. S. H., I. A. A., and M. R. C. carried out the study, M. S. H., I. A. A., and M. R. C. analysed the data, M. S. H., M. R. C., and M. A. M. interpreted the findings, M. S. H., M. A. M., and M. R. C. wrote the article, and all authors reviewed and contributed to the final version of the manuscript.
There are no conflicts of interest
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114521002877