Between 2000 and 2030, the worldwide population aged >65 years is expected to increase from 6·9 to 12 % worldwide and from 15·5 to 24·3 % in Europe( 1 ). The old continent has currently the world’s highest proportion of older persons, a situation projected to continue to for at least the next 50 years( 2 ).
The current leading causes of death have shifted from infectious illness to non-communicable diseases, such as CVD and cancer, which account for 70 % of deaths in the European region( 3 ) and are positively influenced by diet and lifestyle.
With the increase in life expectancy, much effort is devoted to encourage older persons to adopt diet and lifestyle practices that minimise their risk of death from morbidity while increasing their prospects for survival( Reference Knoops, de Groot and Kromhout 4 ).
The traditional Mediterranean diet (MD) has been repeatedly associated with lower risk of major chronic diseases( Reference Sofi, Abbate and Gensini 5 ) and long considered as contributing to the reduced rates of cardiovascular and cerebrovascular events and of the longer life expectancy in adults who live near the Mediterranean Sea( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 6 ). Similarly, other food patterns, such as the traditional Japanese diet, characterised by high intake of fish and soyabean products and low intake of fat, have been shown to substantially contribute to lower death risk in the Japanese population( Reference Kurotani, Akter and Kashino 7 ).
To date, a persuasive body of evidence from observational studies has documented the association of Mediterranean-like dietary patterns with longer survival in the elderly populations, either in Mediterranean( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 6 , Reference Lasheras, Fernandez and Patterson 8 , Reference Trichopoulou, Bamia and Trichopoulos 9 ) or in non-Mediterranean countries( Reference Osler and Schroll 10 – Reference Reedy, Krebs-Smith and Miller 14 ) or in settings including cohorts of different origin( Reference Kouris-Blazos, Gnardellis and Wahlqvist 15 – Reference Bamia, Trichopoulos and Ferrari 19 ). Promising findings were also provided by the PREDIMED (Prevención con Dieta Mediterránea) trial, which tested the health effects of an MD in a group of middle-aged individuals at high CVD risk( Reference Estruch, Ros and Salas-Salvadó 20 ). However, recent data have indicated a downward trend in the adherence to this eating model especially in individuals aged >60 years who experienced the highest decrease as compared with their younger counterparts( Reference Bonaccio, Di Castelnuovo and Bonanni 21 ).
In all, three major issues still deserve attention: first, with the exception of the Greek and Spanish segments of the EPIC (European Prospective Investigation into Cancer and Nutrition) study( Reference Trichopoulou, Orfanos and Norat 17 ) and the ILSA (Italian Longitudinal Study on Aging) cohort in Italy( Reference Limongi, Noale and Gesmundo 22 ), a substantial proportion of the studies addressing the relationship between the MD and health outcomes in the elderly from the general population were conducted outside the Mediterranean basin, which is not the ideal setting for testing the benefits of an MD( Reference Martínez-González, Guillén-Grima and De Irala 23 ); second, most of the evidence is provided by cohort studies conducted in the 90s with lack of data from more recent cohorts, with the exception of the US population included in the REGARDS (REasons for Geographic and Racial Differences in Stroke) study( Reference Whalen, Judd and McCullough 24 ); third, no meta-analysis so far has specifically addressed the association of the MD and mortality within elderly cohorts.
In light of the aforementioned issues, the main purpose of the present study was to estimate the relationship between the MD and mortality in the elderly population of the Moli-sani Study, a large community-based Mediterranean population cohort established between 2005 and 2010. As a second aim, we conducted a meta-analysis of available prospective cohort studies (including Moli-sani) that evaluated the association between the MD and all-cause mortality in individuals aged ≥65 years.
Methods
Study population
We used data from the Moli-sani Study, a prospective cohort study of men and women (aged ≥35 years) randomly recruited from the general population of a Southern Italian region with the main purpose of investigating genetic and environmental risk factors in the onset of cardiovascular, cerebrovascular and tumour diseases( Reference Di Castelnuovo, Costanzo and Persichillo 25 ). From March 2005 to April 2010, 24 325 participants were enrolled. For the purpose of this study, we selected 5831 participants aged ≥65 years. After omitting those reporting implausible energy intakes (<3347 kJ/d (<800 kcal/d) in men and <2092 kJ/d (<500 kcal/d) in women or >16 736 kJ/d (>4000 kcal/d) in men and >14 644 kJ/d (>3500 kcal/d) in women), unreliable medical/dietary questionnaires, participants lost to follow-up or with incomplete personal data and individuals with missing information on the main variables of interest, the final sample consisted of 5200 participants.
The cohort was followed up until 31 December 2015 with the main outcome of interest being mortality. Overall and cause-specific mortality was assessed by the Italian mortality registry (ReNCam; Registro Nominativo delle Cause di Morte), validated by Italian death certificates (ISTAT (Istituto nazionale di statistica) form) and coded according to the International Classification of Diseases (ICD-9; online Supplementary Appendix 1).
CVD mortality included deaths from diseases of the circulatory system when the underlying cause of death included ICD9 codes 390–459. ICD-9 codes 430–438 were used to define specific cause of death for cerebrovascular disease, ICD-9 codes 410–414 and 429 for coronary artery disease (CAD); these two causes were collapsed into the CAD/cerebrovascular mortality group.
Cancer death was recorded when the underlying cause of death included ICD9 codes 140–208. Non-cardiovascular/non-cancer causes of death were included in ‘other-cause mortality’ group. The Moli-sani Study complies with the Declaration of Helsinki and was approved by the Ethical Committee of the Catholic University in Rome, Italy. All participants provided written informed consent.
Ascertainment of risk factors at baseline
History of CVD (angina, myocardial infarction, revascularisation procedures and cerebrovascular events) was self-reported and confirmed by medical records and current therapy. History of cancer was self-reported. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg or treatment for hypertension. Hypercholesterolaemia was defined as total cholesterol ≥240 mg/dl (6·2 mmol/l) or by use of medication. Diabetes was defined as blood glucose ≥126 mg/dl (7 mmol/l) or by use of pharmacological treatment.
Leisure-time physical activity was assessed by a structured questionnaire (questions on walking, gardening and sport participation)( Reference Pereira, Fitzgerald and Gregg 26 ), and expressed as daily energy expenditure in metabolic equivalent task-h/d.
Height and weight were measured and BMI was calculated as kg/m2 and then grouped into three categories as normal (≤25 kg/m2), overweight (>25<30 kg/m2) or obese (≥30 kg/m2).
Participants were classified as never-smokers, current smokers or ex-smokers (quit at least 1 year ago). Education was based on the highest qualification attained and was categorised as up to lower secondary (approximately ≤8 years of study), upper secondary school (8–13 years of study) and post-secondary education (>13 years of study).
Household income, expressed as earned Euros per year, was a five-level variable (<10 000; 10 000–25 000; 25 000–40 000; >40 000 EUR/year) with missing values collapsed into a non-respondent category.
Dietary assessment
Food intake during the year before enrolment was assessed by the validated Italian EPIC FFQ( Reference Pisani, Faggiano and Krogh 27 ). Adherence to the traditional MD was defined according to the Mediterranean diet score (MDS) developed by Trichopoulou et al.( Reference Trichopoulou, Costacou and Bamia 28 ), which was obtained by assigning 1 point to healthy foods (fruits and nuts, vegetables, legumes, fish, cereals, monounsaturated to saturated fats ratio) whose consumption was above the sex-specific medians of intake of the Moli-sani study population; foods presumed to be detrimental (meat and dairy products) were scored positively if the consumption was below the median. All other intakes received 0 points. For ethanol, men who consumed 10–50g/d and women who consumed 5–25g/d received 1 point; otherwise, the score was 0.
The MDS ranged from 0 to 9 (the latter reflecting maximal adherence) and was used either as continuous variable (1 or 2-point increase) or categorised into three levels ranging from poor (0–3 points), average (4–6) to high (7–9) adherence.
Meta-analysis
The present meta-analysis included findings from the Moli-sani Study and previous prospective studies that reported risk estimates associated with an a priori dietary score used for assessing adherence to the MD and mortality among participants aged ≥65 years. An electronic literature search was conducted on PubMed and EMBASE databases from inception until 30 April 2018, by using a search strategy based on the search terms ‘Mediterranean diet’ OR ‘dietary patterns’ AND ‘mortality’ OR ‘death’ (online Supplementary Appendix 2).
The relevance of studies was assessed by using a hierarchical approach based on study design, population, exposure and outcome. We also screened the reference lists of searched articles to find additional relevant studies. In case the full article was not accessible, it was requested from the corresponding author along with availability in providing data regarding age-specific groups. All searches were limited to human studies in the English language. Two authors (M. B. and A. D. C.) independently assessed the eligibility of the identified records, with any disagreement resolved by consensus.
Study selection and data extraction
To be included in the meta-analysis, studies had to fulfil the following: (a) studies in humans; (b) the exposure of interest was the MD as measured by MDS or its modified versions; (c) reported risk estimates for overall mortality; (d) the study design was prospective; (e) reported risk estimates for overall mortality in elderly participants defined as aged ≥65 years selected within the general population or sub-group analysis in aged ≥65 years; (f) relative risk or hazard ratio (HR) with corresponding 95 % CI were available.
When the same population was used in multiple publications, the one with the longest follow-up or the largest number of events was included. Articles were excluded if they: (a) examined only individual nutrients or food groups; (b) did not use MDS nor its modified versions; (c) were not conducted on population-based study samples or were conducted on groups with health conditions or specific nutritional needs.
Some differences among studies exist in the range of dietary scores used, but the total adherence scores varied from a minimum of 0 points indicating low adherence to a maximum of 7–9 points indicating high adherence to the MD.
Statistical analysis of the Moli-sani cohort
Characteristics of the study population by levels of adherence to the MD were presented as numbers and percentages, or mean values and standard deviations for continuous variables. Risk estimates for all-cause and cause-specific deaths were expressed as HR with 95 % CI and calculated by using Cox regression models with time-on-study on the time scale and competing risk of dying for other causes.
Crude and multi-variable risk estimates were provided for each outcome under study.
Selection of potential confounders was made through directed acyclic graphs (DAG) by using DAGitty (http://dagitty.net/) a browser-based environment for analysing causal models through diagrams to minimise bias (online Supplementary Appendix 3).
The multi-variable model was eventually adjusted for sex, age (continuous), education (up to lower secondary, upper secondary, post-secondary education) household income (<10 000; 10 000–25 000; 25 000–40 000; >40 000 and non-respondent category), smoking status (non-smoker, current, former), leisure-time physical activity (continuous), BMI (categorical, <25, ≥25–30, ≥30 kg/m2), cancer (no, yes, unascertained), CVD (no, yes, unascertained), diabetes (no, pre-diabetes, diabetes, unascertained), hypercholesterolaemia (no, pre-hypercholesterolaemia, hypercholesterolaemia, unascertained), hypertension (no, pre-hypertension, hypertension, unascertained), use of anti-depressants (no/yes) and energy intake (kJ/d (kcal/d), continuous).
Appropriate terms for testing interaction were included in the multi-variable model to test for a difference of effect of the MD (MDS continuous) in relation to death risk within selected population groups.
The contribution of each single food group included in the MDS towards the risk of overall mortality was established by alternate subtraction of each food item according to a methodology previously used within the Moli-sani cohort( Reference Bonaccio, Di Castelnuovo and Costanzo 29 ).
Sensitivity analyses were run by excluding missing categories (for diabetes, CVD, cancer, hypercholesterolaemia, hypertension). Age groups were set at <80 or ≥80 years in line with the definition of very elderly individuals.
Potential dose–response relationship between the MDS (continuous) and risk of all-cause mortality was tested via a restricted cubic spline regression that was undertaken among the elderly sample of the Moli-sani cohort (n 5200). The used RCS_Reg SAS macro( Reference Desquilbet and Mariotti 30 ) created a restrictive cubic spline function of the MDS with three knots, located at the 5th, 50th, and 95th percentile, and displays the dose–response association (with its 95 % CI) between the cubic spline MDS and all-cause mortality, tested via a multi-variable Cox model.
Dummy variables for missing values were created. Two-sided P value <0·05 was considered as statistically significant.
The data analysis was generated using SAS/STAT software, version 9.1.4 of the SAS System for Windows© 2009. SAS Institute Inc. and SAS are registered trademarks of SAS Institute Inc., Cary, NC, USA.
Meta-analysis
We conducted a random-effects meta-analysis( Reference DerSimonian and Laird 31 ), and for each study we estimated the HR of total mortality for 1-point increment in the MDS. Statistical heterogeneity was evaluated with the Q and I 2 statistics( Reference Higgins and Thompson 32 ). Potential publication bias was visually assessed with a funnel plot. Meta-analyses were done by using MetaXL (version 5.3).
We also conducted a dose–response meta-analysis by including studies for which HR estimates for grouped categories of adherence to the MD, as compared to a reference level with 0 or very low adherence to the MD, were provided (Sjögren et al. (11), Tognon et al. (12) and the Moli-sani Study).
Data collected were as follows: (i) the value x of MD assigned as the midpoint of the reported ranges; (ii) frequency counts, adjusted HR and 95 % CI for each x level.
Inverse variance–weighted methods, taking into account the correlation between estimates within each study, were used( Reference Bagnardi, Zambon and Quatto 33 ). The models to be fitted were selected among fractional polynomial curves of the second order. Fractional polynomials are a family of models considering power transformations of a continuous exposure variable, restricted to a predefined set of integer and non-integer exponents. The regression models were natural log(HR)=β 1 x p +β 2 x q and the exponents p and q were selected among the following set: {−2·0, −1·0,−0·5, 0·0, 0·5, 1·0, 2·0}.
When P=0, x p is replaced by log(x), and when P=q, the model becomes log(HR)=β 1 x p +β 2 x q log(x). These choices account for a rich set of possible functions, including J-shaped relations and conventional polynomials. The best fit was defined as that with the highest likelihood. Both fixed- and random-effects models were considered.
Results
The Moli-Sani Study
In a large sample of elderly individuals, higher adherence to the MD was associated with trends towards a beneficial cardiovascular profile including lower age and more leisure-time physical activity, although reporting higher prevalence of hypercholesterolaemia (Table 1). Individuals with a closer adherence to the MD had higher socio-economic status and greater energy intake (Table 1).
Table 1 Baseline characteristics of the study population by levels of adherence to the Mediterranean diet in the elderly sample of the Moli-sani cohort study (Mean values and standard deviations and percentages)
MET, metabolic equivalent task.
* Moderate alcohol intake was defined as consumption of 10–50 g/d for men and 5–25 g/d for women.
Over a median follow-up of 8·1 years (interquartile ranges: 6·9–9·2 years; 40 887 person years), a total of 900 deaths were ascertained.
The HR for total mortality for different categories of MD and for 1-point increment in the MDS, both in the whole population and separately for men and women are reported in Tables 2 and 3, respectively.
Table 2 Risk of death in relation to adherence to the Mediterranean diet in the elderly sample (n 5200) of the Moli-sani cohort study* (Hazard ratios (HR) and 95 % confidence intervals)
Ref., reference; CAD, coronary artery disease.
* Multi-variable model adjusted for sex, age (continuous), education, household income, leisure-time physical activity, smoking status, BMI, cancer, CVD, diabetes, hypertension, hypercholesterolaemia, use of anti-depressants and energy intake.
Table 3 Risk of death in relation to adherence to the Mediterranean diet in the elderly men and women of the Moli-sani cohort study* (Hazard ratios (HR) and 95 % confidence intervals)
Ref., reference; CAD, coronary artery disease.
* Multi-variable model adjusted for age (continuous), education, household income, leisure-time physical activity, smoking status, BMI, cancer, CVD, diabetes, hypertension, hypercholesterolaemia, use of anti-depressants and energy intake.
In the multi-variable model, high adherence to the MD was associated with 25 % lower risk of death as compared with the lowest category (95 % CI 3, 42 %; Table 2, multi-variable model); the magnitude of the association was similar for men (HR=0·75; 95 % CI 0·56, 1·01; Table 3, model 2) and women (HR=0·71; 95 % CI 0·42, 1·17; multi-variable model), although statistical significance was not retained. A 1-point increase in MDS was inversely associated with risk of all-cause death, in the whole population (HR=0·94; 95 % CI 0·90, 0·98) and in men (HR=0·94; 95 % CI 0·89, 0·99), whilst for women, a downward trend was observed (HR=0·95; 95 % CI 0·88, 1·02); sex was not an effect modifier of the association of MDS with mortality (Table 3).
Online Supplementary Fig. S1 reports the adjusted dose–response association between MDS and risk of all-cause death showing an inverse linear dose–response relationship (P value for overall association=0·0026; P value for non-linear association=0·99).
Risks of death from CAD/cerebrovascular causes and mortality from other causes were found to be reduced by 9 (95 % CI 1, 17) % and 11 (95 % CI 4, 19) % for each 1-point increase in the MDS, respectively (Table 2; multi-variable models). Analyses by sex revealed a protection limited to CAD/cerebrovascular in men (HR=0·88; 95 % CI 0·78–0·99) and to non-vascular/non cancer death risk (Table 3; multi-variable model), whilst among women the magnitude of the associations between MDS and mortality outcomes was similar to those documented for men, although statistical significance was not hold likely due to a relatively low number of events. No associations were found for CVD or cancer mortality, neither for the whole study sample nor for men and women separately (Tables 2 and3; multi-variable models).
Sensitivity analyses for the association of 1-point increment in the MDS and all-cause mortality are reported in Table 4. An inverse association was confirmed in all sub-groups except within CVD or cancer patients, individuals aged ≥80 years or without prevalent diabetes or hypercholesterolaemia.
Table 4 Sensitivity analyses for the association of 1-point increment in Mediterranean diet score and all-cause mortality in the Moli-sani cohort study* (Hazard ratios (HR) and 95 % confidence intervals)
* Multi-variable model adjusted for age (continuous), education, household income, leisure-time physical activity, smoking status, BMI, cancer, CVD, diabetes, hypertension, hypercholesterolaemia, use of anti-depressants and energy intake.
However, no difference of effect was found (all P values for interaction >0·05), with the exception of diabetes at baseline (P for interaction=0·035).
The relative contribution of each food group included in the MDS in relation to risk of all-cause mortality is shown in Table 5.
Table 5 Risk of death associated with 2-point increase in Mediterranean diet score (MDS) and after alternate subtraction of each of its dietary components in the Moli-sani cohort study and by sex or age groups* (Hazard ratios (HR) and 95 % confidence intervals)

* Multi-variable models adjusted for sex, age (continuous), education, household income, leisure-time physical activity, smoking status, BMI, cancer, CVD, diabetes, hypertension, hypercholesterolaemia, use of anti-depressants and energy intake.
† Change (%) in total effect was obtained by (HRfor 2-point increase in MDS−HRfor 2-point increase in MDS minus each dietary component)/(HRfor 2-point increase in MDS).
Among the whole study sample, the greatest contribution derived from higher MUFA to SFA ratio (−24 % reduction of the effect, after elimination of this component from the score), high intake of fish (−20·7 %) and moderate consumption of alcoholic beverages (−15·9 %). We found similar results for men and individuals aged ≤80 years, for whom MUFA:SFA ratio and fish intake mostly drove the global effect of MDS towards mortality risk, while for women and elderly aged >80 years a consistent role was played also by high intake of cereals (Table 5).
Meta-analysis of prospective cohort studies
We conducted a meta-analysis by combining the results of the Moli-sani cohort with the findings of other prospective studies.
A flow chart of study selection is reported in Fig. 1. Our literature search resulted in the identification of 3533 articles, and after exclusion of duplicate records (n 1111) a total of 535 studies were screened by title and abstracts out of which twenty reported the results of prospective studies on the MD and risk of death in elderly populations( Reference Knoops, de Groot and Kromhout 4 , Reference Trichopoulou, Kouris-Blazos and Wahlqvist 6 , Reference Lasheras, Fernandez and Patterson 8 – Reference Bamia, Trichopoulos and Ferrari 19 , Reference Limongi, Noale and Gesmundo 22 , Reference Whalen, Judd and McCullough 24 , Reference Bagnardi, Zambon and Quatto 33 , Reference Hodge, Bassett and Dugué 34 ). Of them, three publications( Reference Knoops, de Groot and Kromhout 4 , Reference Osler and Schroll 10 , Reference Haveman-Nies, de Groot and Burema 16 ) were excluded because their findings were included in a subsequent study( Reference Knoops, Groot de and Fidanza 18 ) including larger events; two other studies( Reference Limongi, Noale and Gesmundo 22 , Reference Whalen, Judd and McCullough 24 ) because they did not assess dietary exposure by using the MDS nor its modified versions; six other records were omitted because data were generated within institutionalised population( Reference Lasheras, Fernandez and Patterson 8 ), obtained in patients with previous disease( Reference Trichopoulou, Bamia and Trichopoulos 9 ), risk estimates were not available for sub-group aged ≥65 years( Reference Hodge, Bassett and Dugué 34 – Reference van den Brandt 36 ), and another one was a review article( Reference de Groot, Verheijden and de Henauw 37 ). Other records were excluded because of age cut-offs set at age >60 years without providing sub-groups analyses on age( Reference Reedy, Krebs-Smith and Miller 14 , Reference Trichopoulou, Orfanos and Norat 17 , Reference Bamia, Trichopoulos and Ferrari 19 ). Additional data for the association of the MD with risk of overall death in individuals aged ≥65 years were provided by three authors( Reference Sjögren, Becker and Warensjö 11 , Reference Limongi, Noale and Gesmundo 22 , Reference Whalen, Judd and McCullough 24 ).
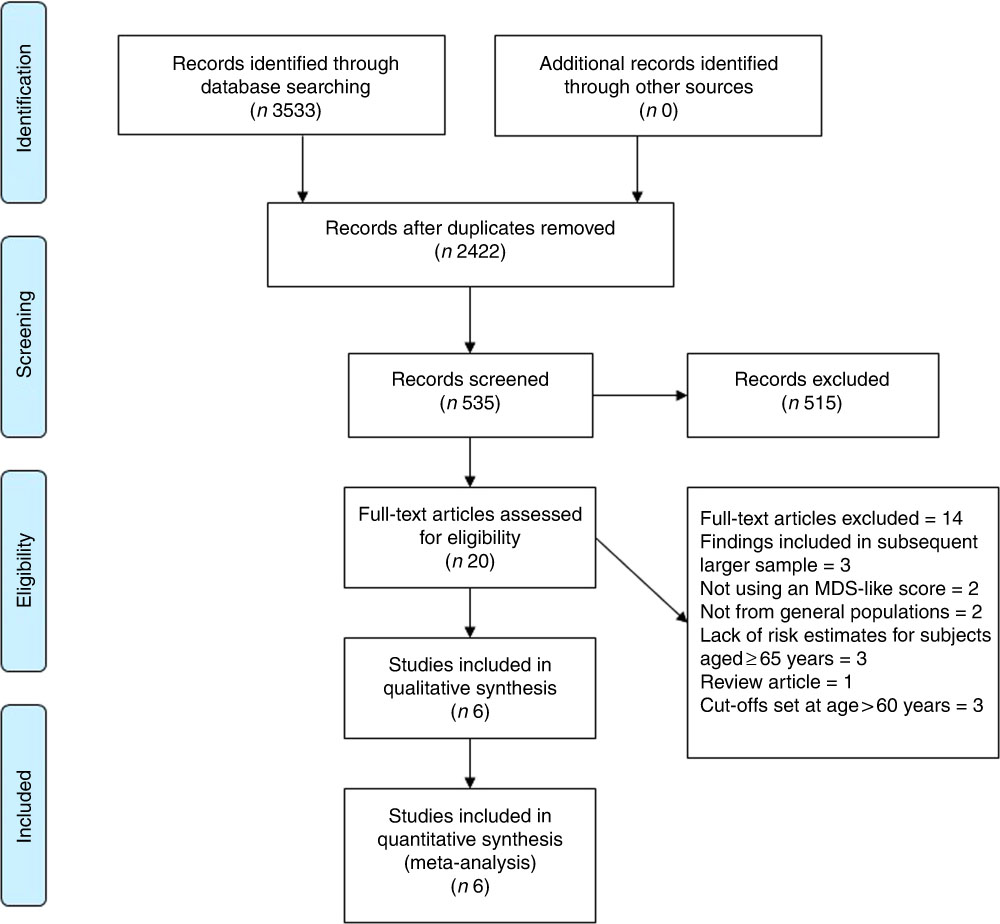
Fig. 1 Selection of prospective cohort studies for inclusion in this meta-analysis. MDS, Mediterranean diet score; MD, Mediterranean diet.
Finally, six prospective studies were selected for the meta-analysis which included the results of the Moli-sani cohort for a total of seven records analysed, 11 738 participants and 3874 deaths (Table 6).
Table 6 Main characteristics of prospective cohort studies evaluating adherence to the Mediterranean diet and risk of all-cause mortality in the elderly*
MDS, Mediterranean diet score; HALE, Healthy Ageing: a Longitudinal study in Europe.
* All dietary scores were obtained by calculation of sex-specific medians for each food group.
Overall, only two out of seven were conducted among Mediterranean populations (one in Greece( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 6 ) and the present study), and four were from non-Mediterranean countries (two in Sweden( Reference Sjögren, Becker and Warensjö 11 , Reference Tognon, Rothenberg and Eiben 12 ), and one each in UK( Reference McNaughton, Bates and Mishra 13 ) and Australia( Reference Kouris-Blazos, Gnardellis and Wahlqvist 15 )), and one investigation was from a collaborative initiative including a number of cohorts from all over Europe( Reference Knoops, Groot de and Fidanza 18 ).
All studies documented a protective effect of an MD against mortality ranging from 4 to 19 % for 1-point increase in MDS.
Overall, we found an inverse association between 1-point increment in MDS and total mortality (overall HR=0·95; 95 % CI 0·93, 0·96) with a low heterogeneity among studies (I 2=0·0 %; Fig. 2).
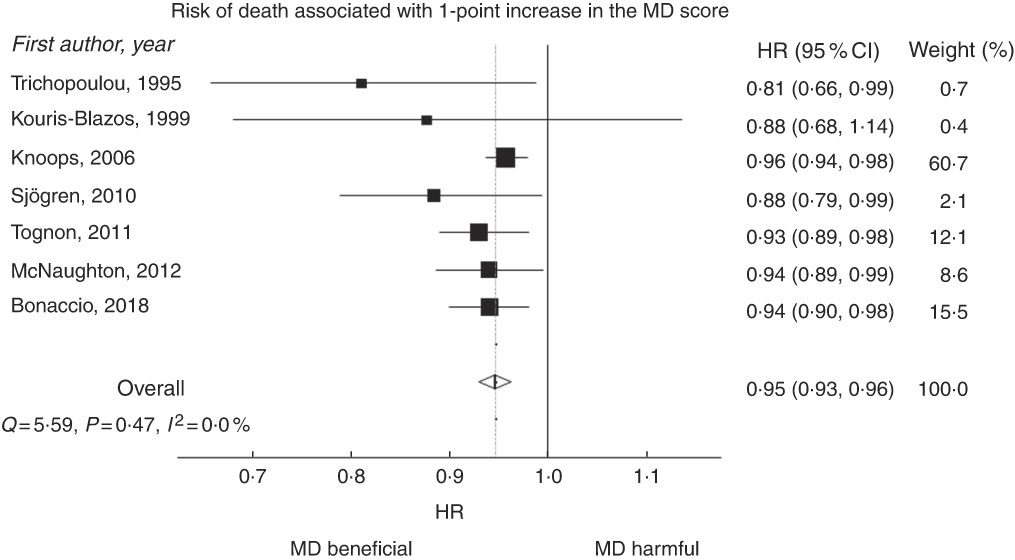
Fig. 2 Hazard ratios (HR) for all-cause mortality for 1-point increment in Mediterranean diet (MD) score. HR were combined using a random-effects model. Squares indicate study-specific HR estimates (size of the square reflects the study-specific statistical weight); horizontal lines represent 95 % CI; diamonds represent the combined HR with their 95 % CI. Tests for heterogeneity: Q=5·59; P=0·47; I 2=0·0 %.
We also conducted a dose–response meta-analysis including three studies (Sjögren et al.( Reference Sjögren, Becker and Warensjö 11 ), Tognon et al.( Reference Tognon, Rothenberg and Eiben 12 ) and the Moli-sani Study) for a total of 7161 individuals and 1745 deaths. The reference category for the study by Sjögren et al.( Reference Sjögren, Becker and Warensjö 11 ) was MDS=0–2 and had three dose-level comparisons; the study by Tognon et al.( Reference Tognon, Rothenberg and Eiben 12 ) and the Moli-sani used the same reference category (MDS=0–1) and had eight dose-level comparisons each (online Supplementary Table S2). The dose–response meta-analysis resulted from a total of eight dose-level comparisons.
The best fitting model was obtained at P=1 and q=0·5, corresponding to the model natural log(HR)=β 1 x+β 2√x. The fitted parameters were β 1=−0·087 (se 0·045) (P value=0·026) and β 2=0·074 (se 0·114) (P value=0·26) for fixed model analysis, and β 1=−0·093 (se 0·049) (P value=0·030) and β 2=0·088 (se 0·124) (P value=0·24) for random model. As displayed in Fig. 3, an inverse linear relationship was found between MDS and total mortality risk with significant inverse associations being documented at MDS >3.
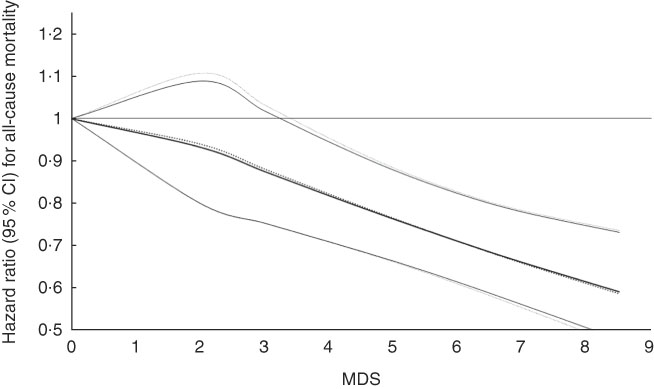
Fig. 3 Hazard ratio (HR) for all-cause mortality (95 % CI) and Mediterranean diet score (MDS) extracted from three studies using fixed- and random-effects models. ![]() Fixed model: Ln(HR)=−0.087x +0.074√x(P value β1:0.026; β2:0.24).
Fixed model: Ln(HR)=−0.087x +0.074√x(P value β1:0.026; β2:0.24). ![]() Random model: Ln(HR)=−0.093x +0.088√x(P value β1:0.030; β2:0.24).
Random model: Ln(HR)=−0.093x +0.088√x(P value β1:0.030; β2:0.24).
Discussion
The present findings show that closer adherence to the MD was associated with 25 % lower risk of all-cause death in a large sample of elderly individuals from a Mediterranean general population.
Our results are in line with those from previous observational studies reporting a favourable effect of an MD or other vegetable-based dietary patterns in reducing mortality risk in the elderly( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 6 – Reference Lasheras, Fernandez and Patterson 8 ). More recently, the landmark PREDIMED trial on middle-aged/older individuals at high cardiovascular risk reported that an MD supplemented with olive oil or nuts is capable to reduce the risk of death from CVD by 30 %( Reference Estruch, Ros and Salas-Salvadó 20 ). Past evidence from the Lyon diet heart study had shown prolonged survival associated with the MD in middle-aged patients with previous CVD( Reference de Lorgeril, Salen and Martin 38 ). We found a weaker association of the MD with total CVD mortality, which is possibly due to the inclusion of CVD-related outcomes, for some of which data on the effectiveness of the MD are scarce or contrasting.
In this respect, our findings appear to be in line with previous evidence highlighting a stronger association of an MD with CHD or stroke risk rather than with total CVD risk( Reference Hoevenaar-Blom, Nooyens and Kromhout 39 , Reference Rosato, Temple and La Vecchia 40 ). The positive association between the MD and risk of death was confirmed in the present meta-analysis of seven prospective cohort studies, comprising the findings of the Moli-sani cohort.
A 5 % risk reduction in mortality associated with 1 point-increment in the MDS found in our meta-analysis (equivalent to 9·8 % for 2-point increment) is comparable to the findings reported in the meta-analysis by Sofi et al.( Reference Sofi, Abbate and Gensini 5 ) who documented an 8 % lower risk of death associated with 2-point increase in the MDS, a finding recently confirmed (9 % risk reduction) in an umbrella review of meta-analyses( Reference Dinu, Pagliai and Casini 41 ). Moreover, an inverse dose–response relationship emerged from the meta-analysis of three prospective studies showing lower death risk at MDS >3.
As it emerges from the selected studies, despite being the traditional dietary pattern of the countries bordering the Mediterranean Sea, the potential health benefits of the MD have been mainly examined to date in non-Mediterranean populations.
Indeed, four out of seven studies here considered were from non-Mediterranean countries (Northern Europe( Reference Sjögren, Becker and Warensjö 11 – Reference McNaughton, Bates and Mishra 13 ), Australia( Reference Kouris-Blazos, Gnardellis and Wahlqvist 15 ) and one from the European HALE (The Healthy Ageing: a Longitudinal study in Europe) project( Reference Knoops, Groot de and Fidanza 18 ) in which a sizable proportion of participants did not come from Mediterranean areas), and only two studies used data from populations recruited in Mediterranean settings (Trichopoulou et al.( Reference Trichopoulou, Kouris-Blazos and Wahlqvist 6 ) and the present study).
The appropriateness of studying the MD within Mediterranean countries has been subsequently discussed( Reference Martínez-González, Guillén-Grima and De Irala 23 , Reference Martínez-González, Hershey and Zazpe 42 ), arguing that in non-Mediterranean areas, actual conformity with the Mediterranean dietary pattern is likely to be uncommon. Indeed, there are several food items whose consumption substantially differs between Mediterranean and non-Mediterranean countries, such as olive consumption which tends to be very low in non-Mediterranean areas. In the latter, the main source of MUFA is red meat, the main source of ethanol intake is beer and liquors instead of wine, and the main dietary sources of some micronutrients are vitamin supplements rather than natural fresh fruits and vegetables( Reference Martínez-González, Guillén-Grima and De Irala 23 ).
In addition to different food sources, a number of potential gaps still persist, as those related to patterns of consumption: for instance, a traditional MD includes moderate alcohol (preferably wine) consumption, almost exclusively during meals, spread out over the week, with occasional or no liquor consumption. As yet, binge drinking and preference for beer instead of wine are not part of the traditional MD( Reference Martínez-González, Hershey and Zazpe 42 ). Other differences between countries may relate to consumption of avocado, which is likely to be healthy, but is not a traditional MD food, nor soya nor the use of unsaturated fat cooking oils other than olive oil (i.e. peanut, maize, sunflower oils) which do not pertain to the traditional MD( Reference Martínez-González, Guillén-Grima and De Irala 23 , Reference Martínez-González, Hershey and Zazpe 42 ).
Another issue addressed in the present study relates to the comparison between earlier and more recent studies which may be useful to estimate the potential beneficial effects of the MD over time. Indeed, it is well-known that rates of adherence to the MD have decreased over time( Reference Bonaccio, Di Castelnuovo and Bonanni 21 ), and in light of this, it is crucial to study the association of the MD with health outcomes within population settings in which the exposure (MD) is likely to be different (decreased) as compared to the past. In addition to this, it is worth acknowledging several problematic nutritional aspects closely linked to analysis on the MD, and diet in general. Over time, the composition of the MD has consistently changed, and the quality and quantity of food people eat nowadays may have little to do with the traditional MD( Reference Tosti, Bertozzi and Fontana 43 ). Some examples include the high grain product intake almost exclusively from white flour but not from whole grain flour, higher total energy intake and higher salt intake( Reference Stamler 44 ). Thus, it is likely that changes in the composition of foods included in the MD pyramid may affect long-term health effects associated with the MD.
The exact mechanism by which the traditional MD exerts its favourable effects on health is not fully known. Possible mechanisms have been identified in the anti-inflammatory properties of the bundle of foods typical of this dietary patterns, such as fruits, vegetables, and legumes( Reference Bonaccio, Pounis and Cerletti 45 ). As yet, more recent evidence has demonstrated a number of health benefits possibly associated with intake of monounsaturated fats which are abundant in either extra-virgin olive oil or in nuts( Reference Estruch, Ros and Salas-Salvadó 20 , Reference Guasch-Ferré, Hu and Martínez-González 46 ) and a role of fish for heart health has been highlighted in several studies( Reference Zheng, Huang and Yu 47 , Reference Bonaccio, Ruggiero and Di Castelnuovo 48 ).
Moreover, it is worthwhile to mention the reduced risk of all-cause mortality and cardiovascular endpoints, associated with moderate alcohol intake, one of the component of the MDS( Reference Costanzo, Di Castelnuovo and Donati 49 ). Indeed, in our study moderate drinking was a major contributor to the overall death protection associated with the MD.
Finally, it has been proposed that the MD, which is rich in fibre content, may act favourably also for glycaemic control, a major health risk factor( Reference Esposito, Maiorino and Di Palo 50 ).
Late studies have documented a positive relationship between the MD and telomere length, a biomarker of ageing highly susceptible to oxidation and inflammation-related mechanisms( Reference Boccardi, Esposito and Rizzo 51 ). A diet rich in antioxidants or with marked anti-inflammatory properties, as the MD, might reduce the rate of telomere shortening, that in turn might delay the ageing process thus explaining (at least in part) the longer survival rates of the Mediterranean populations.
Moreover, the ageing process in humans is associated with chronic low-grade inflammation, a condition recently referred to as ‘inflammaging’( Reference Santoro, Brigidi and Gonos 52 ). Several studies have shown that adherence to an MD or other vegetable-based dietary patterns is associated with lower sub-clinical inflammation( Reference Bonaccio, Di Castelnuovo and Pounis 53 , Reference Barbaresko, Koch and Schulze 54 ), which in turn, when elevated, is predictive of poor health outcomes also in the elderly( Reference Bonaccio, Di Castelnuovo and Pounis 55 ).
Additional modifications induced by the MD include a lipid-lowering effect, protection against oxidative stress, modification of hormones and growth factors involved in the pathogenesis of cancer, inhibition of nutrient sensing pathways by specific amino acid restriction, and gut microbiota-mediated production of metabolites influencing metabolic health( Reference Tosti, Bertozzi and Fontana 43 ).
Strengths and limitations of the present study
The strengths of our longitudinal study within the Moli-sani cohort include the selection of elderly individuals, its large sample size, its prospective population-based design and the inclusion of detailed information on diet and other lifestyle factors to accommodate possible confounding by these variables.
Potential limitations consist in the observational nature of the study which cannot fully rule out residual confounding. In addition, dietary data were based on self-reported information and therefore may be susceptible to error and bias. Finally, participants’ information was collected at baseline only, thus life-course changes possibly occurring during the follow-up may influence the strength of the findings.
The major strength of our meta-analysis is due to the fact that, to the best of our knowledge, this is the first meta-analysis specifically addressing and documenting the association between the MD and mortality in an elderly population. One major limitation is in contrast the subjective nature of the dietary scores used in the original manuscripts; moreover, most studies used a dietary score based on population-specific median intakes, thus absolute intakes of food groups scored could vary substantially among different cohorts. Finally, our meta-analysis only comprised observational studies, thus sharing all the limitations pertaining to this study type.
Conclusions
To summarise, we found that adherence to the MD is associated with increased survival in a large sample of the elderly. Findings from the Moli-sani cohort and the subsequent meta-analysis of prospective cohort studies strongly support the appropriateness for older persons to preserve/adopt a Mediterranean-type diet in order to increase their prospects for longevity. This is of crucial importance especially in the light of the rapid shifting from the MD documented in recent years, which has been mainly experienced by the elderly( Reference Bonaccio, Di Castelnuovo and Bonanni 21 ), and also because the burden of healthcare costs associated with increased life expectancy strictly depends on whether additional life years are spent in good or poor health( Reference Wouterse, Huisman and Meijboom 56 ).
Finally, a better understanding of lifestyle behaviours influencing longevity is of extreme interest for health administrators and governments for better tailoring their prevention strategies and policies.
Acknowledgements
The Moli-sani Research Investigators thank the Associazione Cuore Sano Onlus (Campobasso, Italy) for its cultural and financial support. The authors thank Doctor Per Sjögren from Uppsala University (Sweden), and Doctor Gianluca Tognon (Sweden) for providing us with data from their cohorts.
The enrolment phase of the Moli-sani Study was supported by research grants from Pfizer Foundation (Rome, Italy), the Italian Ministry of University and Research (MIUR, Rome, Italy)–Programma Triennale di Ricerca, Decreto no. 1588 and Instrumentation Laboratory, Milan, Italy. Funders had no role in study design, collection, analysis, and interpretation of data; in the writing of the manuscript and in the decision to submit this article for publication. M. B. was supported by a Fondazione Umberto Veronesi Fellowship. S. C. was the recipient of a Fondazione Umberto Veronesi Travel Grant. All authors were and are independent from funders. The present analyses were partially supported by the Italian Ministry of Health 2013 (young investigator grant to M. B., no. GR-2013-02356060) and by the Italian Association for Cancer Research (AIRC) with grant AIRC ‘5×1000’ to L. I., Ref. no. 12237.
L. I., M. B. and A. D. C. contributed to the conception and design of the study reported here and to interpretation of data; S. C. and M. P. managed data collection of the Moli-sani Study; M. B., A. D. C., A. G. and S. C. analysed the data; M. B. wrote the first draft of paper; L. I., M. B. D., G. d. G., C. C. and A. D. C. originally inspired the Moli-sani Study and critically reviewed the manuscript.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114518002179












