Introduction
Acquired brain injury (ABI) is one of the leading causes of disability, with global prevalence rates predicted to be one in 500 people (Bryan-Hancock & Harrison, Reference Bryan-Hancock and Harrison2010; Roozenbeek, Maas & Menon, Reference Roozenbeek, Maas and Menon2013). This encompasses brain injury occurring after birth and includes traumatic injuries (TBI) as a result of external force and injuries acquired through nontraumatic processes, such as a stroke (O’Rance & Fortune, Reference O’Rance and Fortune2007). An ABI can result in temporary and long-term disturbances in mood and behaviour and deficits in cognitive, physical and psychosocial functioning (Fleminger & Ponsford, Reference Fleminger and Ponsford2005; Kumar, Kumar & Singh, Reference Kumar, Kumar and Singh2019). Consequently, treatment involves a complex, and preferably individualised, mix of acute and post-acute health and rehabilitation services and health professionals (de Koning, Spikman, Cores, Schönherr & van der Naalt, Reference de Koning, Spikman, Coers, Schönherr and van der Naalt2015; Jolliffe, Lannin, Cadilhac & Hoffmann, Reference Jolliffe, Lannin, Cadilhac and Hoffmann2018; Mellick, Gerhart & Whiteneck, Reference Mellick, Gerhart and Whiteneck2003; Prang, Ruseckaite & Collie, Reference Prang, Ruseckaite and Collie2012).
Specialist rehabilitation pathways have emerged to address the complex needs of individuals with ABI. These pathways provide a comprehensive mix of rehabilitation services to support the individual in their recovery from acute to post-acute care (Turner-Stokes, Pick, Nair, Disler & Wade, Reference Turner-Stokes, Pick, Nair, Disler and Wade2015). Whilst lacking a definitive consensus, Buntin (Reference Buntin2007) defines post-acute care as services focusing on patients’ needs after leaving acute in-hospital care. The post-acute phase can include structured programmes such as transitional living programmes, outpatient day therapy and community integration programmes, in addition to disciplinary-specific neurobehavioural services (Hall, Grohn, Nalder, Worrall & Fleming, Reference Hall, Grohn, Nalder, Worrall and Fleming2012; Simpson et al., Reference Simpson, Secheny, Lane-Brown, Strettles, Ferry and Phillips2004). Ongoing access to post-acute care services after discharge, which includes post-acute primary health care and rehabilitation services, is imperative to the maintenance and continuation of recovery (Jolliffe et al., Reference Jolliffe, Lannin, Cadilhac and Hoffmann2018; Turner-Stokes et al., Reference Turner-Stokes, Pick, Nair, Disler and Wade2015; Turner et al., Reference Turner, Fleming, Ownsworth and Cornwell2011a). However, studies have indicated that access often reduces across the transition from inpatient care back to the community (Abrahamson, Jensen, Springett & Sakel, Reference Abrahamson, Jensen, Springett and Sakel2017; O’Callaghan, McAllister & Wilson, Reference O’Callaghan, McAllister and Wilson2010). Of concern, a significant proportion of people who acquire a brain injury have insufficient access to adequate post-acute care services in the community in the first year, or miss out altogether (Collie & Prang, Reference Collie and Prang2013; Foster et al., Reference Foster, Allen and Fleming2015; Foster, Fleming, Tilse & Rosenman, Reference Foster, Fleming, Tilse and Rosenman2000; Mellick et al., Reference Mellick, Gerhart and Whiteneck2003; Ta’eed, Skilbeck & Slatyer, Reference Ta’eed, Skilbeck and Slatyer2013).
To facilitate the optimal gains in recovery, treatment and care appropriate to each individual is essential (Conneeley, Reference Conneeley2012; Hall et al., Reference Hall, Grohn, Nalder, Worrall and Fleming2012). Yet, planning and achieving appropriateness across the continuum is challenging (Copley, McAllister & Wilson, Reference Copley, McAllister and Wilson2013; Turner-Stokes et al., Reference Turner-Stokes, Pick, Nair, Disler and Wade2015). Further, the concept of appropriate access is ill defined when it comes to people who acquire a brain injury. Whilst lacking a consensus, appropriateness of access concerns the fit of the service to the user needs, centring around issues of timeliness, quality of care, adequacy and continuity of care (Levesque, Harris & Russell, Reference Levesque, Harris and Russell2013). One component of appropriateness, adequacy of services, has been defined as how well the services received meets patients’ needs. This is if there is sufficiency of services, if there are quality services, and whether what is provided is good enough (Levesque et al., Reference Levesque, Harris and Russell2013; Morrow-Howell, Proctor & Dore, Reference Morrow-Howell, Proctor and Dore1998). The necessity for appropriate access to post-acute care services is emphasised through the guidelines promoting specialist pathways and early and ongoing rehabilitation for people with ABI (Turner-Stokes et al., Reference Turner-Stokes, Pick, Nair, Disler and Wade2015). In Australia, the specialist rehabilitation pathways differ across states and territories, and with regard to the private and public funding pathways (Muenchberger, Kendall & Collings, 2001).
Although the benefits of appropriate access underpin standards in early and long-term recovery, access needs are highly personal. This aligns with the paradigm shift in how services are provided to people with lifelong disabling conditions, taking account of the aspirations and preferences of the service user, to ensure services are matched appropriately to their needs (Foster et al., Reference Foster, Henman, Tilse, Fleming, Allen and Harrington2016). This is evidenced through the implementation of major policy reforms, such as the National Disability Insurance Scheme (NDIS) in Australia. The NDIS was introduced to address equity in access to services for people with disability, through the implementation individualised funding to citizens with permanent and significant disability (Productivity Commission, 2011). However, as illustrated through ongoing disparities and unmet needs of people with ABI, these services may not always fit with service users’ perceived needs or expectations (Copley et al., Reference Copley, McAllister and Wilson2013; Foster et al., Reference Foster, Allen and Fleming2015). Therefore, there is a need to conceptualise appropriate access to post-acute care services in people with ABI. This can provide new insights about how we match services to need.
There has been an increase in research focusing on the user perspective of service access, with a growing interest in the personal experiences and recovery trajectories of those who have ABI. Research addressing personal experiences of access to rehabilitation and support services indicates what might be important to people with brain injury when defining appropriateness. A review of the literature in both giving and receiving care across the TBI trajectory, pointed to key components of appropriateness when it comes to access to services (Kivunja, River & Gullick, Reference Kivunja, River and Gullick2018). Themes related to how people with TBI received care were clustered into two main categories. The first, challenges to self-identity, included experiencing insensitivity of health professionals, wanting to overcome authoritative rule and having input into personal care. The second, feeling different, which included lacking control, being excluded from care planning, needing practical help, including longing for the right kind of help, and inadequacy of organisational resources. Further, Jackson, Hamilton, Jones and Barr (Reference Jackson, Hamilton, Jones and Barr2019) conducted a systematic review of patient reported experiences of community rehabilitation and support services of people with long-term neurological conditions. Analysis of 37 articles concluded that process quality, activities associated with person-centred care and interactions with health professionals’ impact on service engagement and are seen as important.
These reviews provide insight into what valued characteristics are emerging from the literature when it comes to understanding personal experiences of receiving community rehabilitation and support. However, Kivunja et al. (Reference Kivunja, River and Gullick2018) reviewed articles pertaining to those with traumatic brain injury which constrains conclusions that can be drawn about the literature in acquired brain injury more broadly. Additionally, the review included all services including inpatient hospital service access. The literature suggests that access experiences vary across the individual’s trajectory, for example that information needs are often met during hospital stay and these emerge after discharge back into the community (Hall et al., Reference Hall, Grohn, Nalder, Worrall and Fleming2012; Rusconi & Turner-Stokes, Reference Rusconi and Turner-Stokes2003). Jackson et al. (Reference Jackson, Hamilton, Jones and Barr2019) focused on community rehabilitation access however limited the search to qualitative work. Additionally, the focus of this review included progressive neurological conditions, such as multiple sclerosis and Parkinson’s disease. Whilst some comparisons were drawn, access needs and pathways differ significantly for those with these conditions, therefore synthesis of the personal experiences of those with ABI separately would increase the generalisability of the findings.
To deepen our understanding of what appropriate access to post-acute care services is for this population, there is a need to synthesise the literature on post-acute access to services in people with an ABI. Therefore, the aim of this scoping review was to identify key characteristics of ‘appropriate’ access, as defined by the personal experiences of people with ABI, and to identify knowledge gaps in this literature. The review aimed to answer the research question: what do personal experiences of post-acute care service access indicate about characteristics of appropriateness of access for adults with an ABI?
Method
Design
A scoping review was conducted to examine the literature related to the appropriate access to post-acute care services, defined by the personal experiences of people with an ABI. While systematic reviews typically focus on a well-defined research question, seeking to assess the quality of evidence, scoping reviews are an alternative method of reviewing evidence (Grant & Booth, Reference Grant and Booth2009). Scoping reviews are commonly used to synthesise the literature on broad topics, identify key concepts and gaps in the literature (Arksey & O’Malley, Reference Arksey and O’Malley2005; Halas et al., Reference Halas, Schultz, Rothney, Goertzen, Wener and Katz2015). The present study utilises the 5-stage methodological framework developed by Arksey & O’Malley (Reference Arksey and O’Malley2005) which consists of the following stages: 1. Develop the research question; 2. Search for relevant literature; 3. Select the literature/studies; 4. Chart the data: and 5. Collate, summarise and report the results.
Identifying the research question
The present scoping review aimed to answer the following research question: What do personal experiences of post-acute care service access indicate about characteristics of appropriateness of access for adults with an ABI?
Identifying relevant studies
Electronic scientific databases were utilised for the review, see Table 1. A list of terms and filtering options for the search were developed by the research team (Author A, Author B, Author C) based on initial orientation searches, which resulted in search outcomes that were tailored to the research question. In addition, reference lists were checked to identify other relevant articles to obtain a comprehensive set of literature on this topic. The initial search produced 361 articles. After duplicate articles were removed (n = 72) there were 289 articles. The initial search strategy was developed and refined using an iterative process by the research team (Author A, Author B, Author C), with all members reviewing search results at each phase.
Table 1. Table of Search Criteria

a Personal experiences included the perspectives and narratives of the individuals who experience ABI, whether reported first-hand or by family or significant others standing as proxy.
b Studies focusing on service experiences during their stay within the hospital were excluded. Transitional rehabilitation programmes, outpatient programmes, community programmes and programmes where the patient receives ongoing accommodation through the programme were included.
Study selection
In the study selection phase, the relevance of the literature was assessed at abstract and full-text level. The first author (A) conducted the database searches and exported the results into Endnote bibliographic software. Abstracts were then reviewed for relevancy based on the inclusion and exclusion criteria. Inclusion and exclusion criteria were developed by all members of the research team (Author A, Author B, Author C). See Table 1 for detail pertaining to the inclusion and exclusion criteria of the articles. Exemplar articles based on these criteria, and articles which were difficult to determine eligibility, were reviewed and discussed as a group to obtain consensus. Full texts of the remaining publications were reviewed against the inclusion and exclusion criteria, along with articles found in references list checks, leaving articles for data extraction and charting.
Charting the data, collate, summarise and report the results
A data extraction template was developed based on a small subset of full texts and research team consultation (Author A, Author B, Author C) including the following: authors; year and country of publication; aim(s) of study; study design; study participants (number of ABI participants); time since injury/discharge; type of service if specified; access characteristics that were valued by participants; access characterises that were problematic for participants. The 52 selected articles were then reviewed and data extracted by Author A based on this template. A thematic synthesis was conducted (Thomas & Harden, Reference Thomas and Harden2008) which included three phases. Results of each included paper were reviewed and findings relating to the personal access experience post-discharge from inpatient rehab were extracted (Author A). Once text segments were extracted, results were categorised into what was valued (appreciated, satisfactory, positive) as part of their access experience and what was problematic. These were then organised into key descriptive themes using Levesque et al. (Reference Levesque, Harris and Russell2013) conceptualisation of appropriate access as benchmark for comparison against review findings; however, results were not constrained to fit. In the final stage, the results were then analysed and ‘analytical themes’ emerge. Emerging themes and findings were collated and reviewed and validated by members of the research team (Author A, Author B, Author C) through an iterative process. Once themes were finalised the articles were reviewed again, and finalised themes were then assigned to each article. Results of the review are presented below.
Results
Descriptive summary of the articles
There was a total of 52 studies that were included in the scoping review. See Fig. 1 for the flow diagram of included studies. The majority of articles were published between 2010 and 2020 (n = 39/52). The articles included thirty-six qualitative, seven quantitative, six mixed methods studies, and three reviews. The studies were conducted in Australia (n = 16), the USA (n = 13), the United Kingdom (n = 5), Canada (n = 5), Sweden (n = 3), New Zealand (n = 2), Denmark (n = 2) and one each in France, Ireland, South Africa and Botswana.
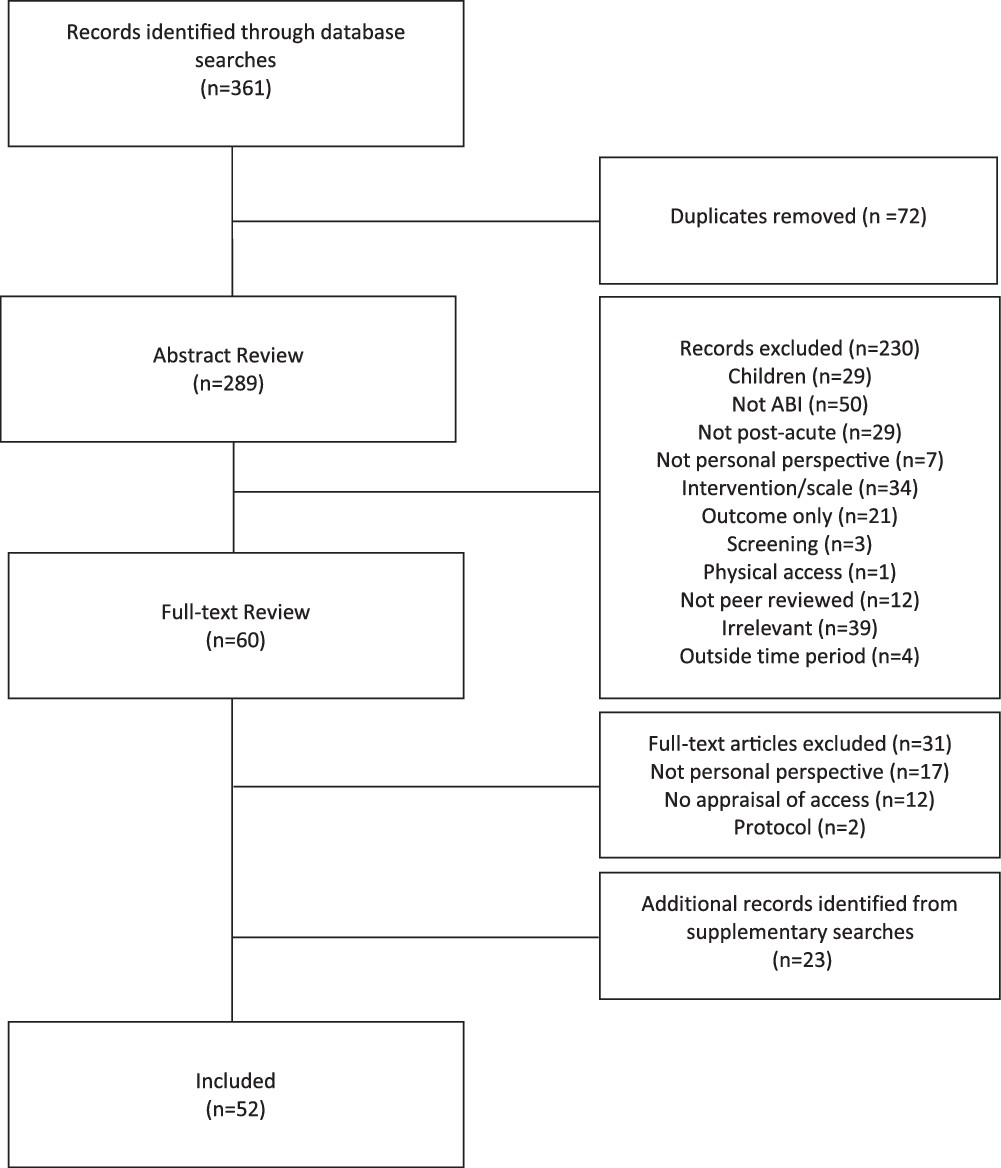
Figure 1. Flow diagram of included studies.
Twenty-six of the articles included both people with a brain injury and family members/caregivers in their samples, and participant numbers ranged from two to 1830 participants. Participants in the studies were either within a year post-discharge (n = 4), more than 1-year post-injury (n = 26), included both (n = 7) or did not report specific time since discharge or injury (n = 12). Twenty-nine of the articles were focused on TBI exclusively, twenty-one included those with ABI, one was all non-TBI brain injuries, and one was stroke specific. Few of the articles were focused on specific populations including war veterans (n = 3), women (n = 1), those in rural and remote locations (n = 3), culturally diverse or indigenous populations (n = 3), and those with alcohol-related injury (n = 1). Thirteen of the articles were regarding a specific service, including occupational therapy (n = 2), vocational or return to work (n = 4), group rehabilitation (n = 1), respite (n = 1), residential settings (n = 2) and aged care settings (n = 2), and specific funding (n = 1).
Findings
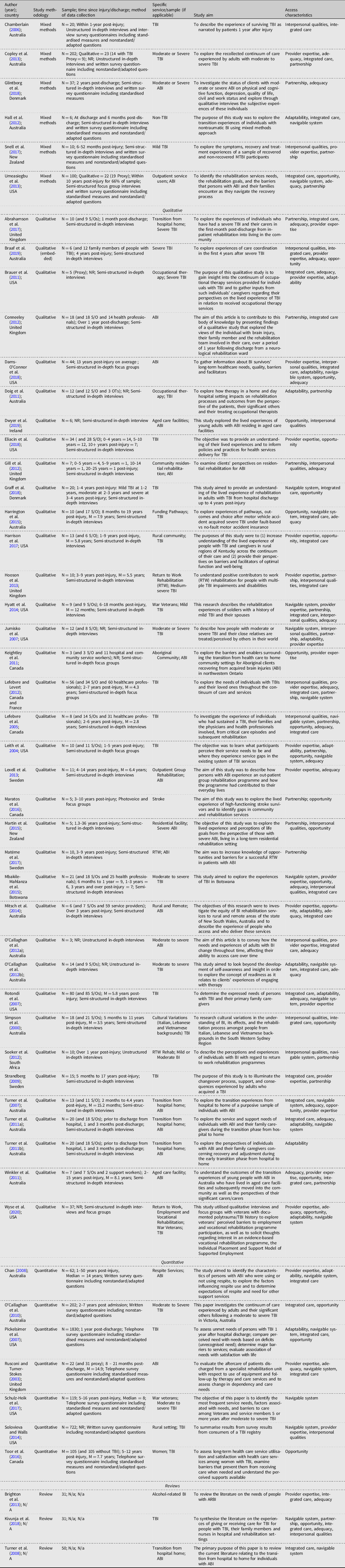
The review aimed to answer the research question: what do personal experiences of post-acute care service access indicate about characteristics of appropriateness of access for adults with an ABI? The synthesis identified eight thematic ideas which were then grouped under two broader themes. See Fig. 2. The first of these was characteristics of the provider: (i) provider expertise (n = 26); (ii) interpersonal qualities (n = 18); (iii) partnership (n = 21); (iv) adaptability (n = 14). The second was the characteristics of the service system: (v) navigable system (n = 24); (vi) integrated care (n = 33); (vii) adequacy (n = 25); and (viii) opportunity (n = 23). The access characteristics of each publication are presented in Table 2.
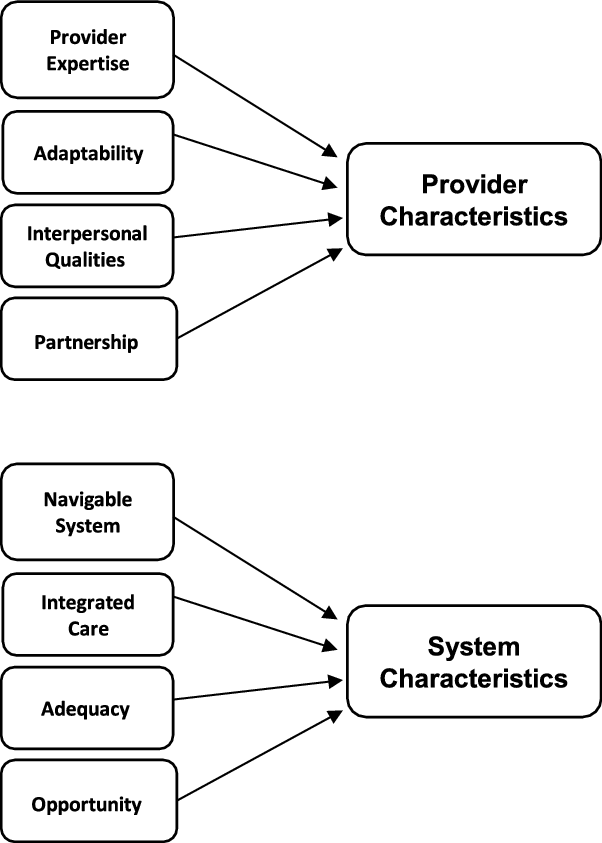
Figure 2. Diagram of themes.
Table 2. Characteristics of Included Studies
Characteristics of providers
Synthesis of this literature illustrates the importance of the relationship between the service provider and user when conceptualising appropriate access from the perspectives of people with brain injury. Features of these services and providers such as expert knowledge and their interpersonal qualities, adaptability and collaborative partnerships with providers have emerged as important factors when understanding appropriate access for brain injury. Synthesis of the themes are outlined below.
Provider Expertise. First, review of the studies suggests that service provider knowledge is an important feature of the access experience for people with brain injury. These studies illustrate that service providers with specialised knowledge of brain injury, such as neuropsychologists, are highly valued (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Brighton, Traynor, Moxham & Curtis, Reference Brighton, Traynor, Moxham and Curtis2013; Dams-O’Connor, Landau, Hoffman & De Lore, Reference Dams-O’Connor, Landau, Hoffman and De Lore2018; Solovieva & Walls, Reference Solovieva and Walls2014). Specialised knowledge increased the confidence that service users had in the providers’ expertise, and validation from providers about personal concerns being known consequences of brain injuries was valued (Lexell, Alkhed & Olsson, Reference Lexell, Alkhed and Olsson2013; Snell, Martin, Surgenor, Siegert & Hay-Smith, Reference Snell, Martin, Surgenor, Siegert and Hay-Smith2017). Service users were also likely to have their needs met, and therefore have a good fit of services, when their providers had the brain injury-specific expertise.
Braaf et al. (Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019) found that specialised knowledge of severe TBI was highly valued and resulted in more perceived productive interactions by patients with their health and rehabilitation providers. Not only was this expertise valued, people with TBI also emphasised that a lack of brain injury-specific knowledge was problematic. In circumstances where providers lacked expert knowledge, service users were likely to perceive that their issues were not acknowledged or addressed (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019). This emphasis on specific expertise also emerged in populations within brain injury, such as those with alcohol-related brain injury who valued knowledge specific to their concerns (Brighton et al., Reference Brighton, Traynor, Moxham and Curtis2013).
Results of the reviewed studies further support this finding that a lack of specialised brain injury-specific expertise is problematic for people with ABI (Eliacin, Fortney, Rattray & Kean, Reference Eliacin, Fortney, Rattray and Kean2018; Harrison et al., Reference Harrison, Hunter, Thomas, Bordy, Stokes and Kitzman2017; Brauer, Hay & Francisco, Reference Brauer, Hay and Francisco2011). When considering appropriate access for people with ABI, results suggested that lack of access to specialised, age appropriate health services in the community was a significant issue (Eliacin et al., Reference Eliacin, Fortney, Rattray and Kean2018). The unwillingness of general and specialty care providers to learn more about ABI was also perceived as highly problematic (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018). This work suggests that providers with specialised or injury-specific knowledge are a valued aspect of appropriate access. Specifically, specialised knowledge was important when it came to people with ABI feeling that their needs were being acknowledged or addressed.
Interpersonal Qualities. Interpersonal qualities of providers were an important aspect of appropriate access from service users’ perspectives. This specifically included qualities such as empathy, sensitivity, honesty, and respect (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Dwyer, Heary, Ward & MacNeela, Reference Dwyer, Heary, Ward and MacNeela2019; Hooson, Coetzer, Stew & Moore, Reference Hooson, Coetzer, Stew and Moore2013; Kivunja et al., Reference Kivunja, River and Gullick2018; Lefebvre & Levert, Reference Lefebvre and Levert2012). Gill, Wall and Simpson (Reference Gill, Wall and Simpson2012) found that participants valued the trustworthiness and reliability of staff, which impacted on a positive relationship between the service user and provider. The empathetic nature of the provider was important to service users (Hooson et al., Reference Hooson, Coetzer, Stew and Moore2013; Kivunja et al., Reference Kivunja, River and Gullick2018; Lefebvre & Levert, Reference Lefebvre and Levert2012). When providers demonstrated care and understanding of the service users concerns, the service users felt that they were able direct the sessions based on their needs (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019). Findings of another study outlined that that good communication was the most valued skill of providers to those with ABI, particularly good communication involving listening and explaining medical terms (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018).
In contrast, a lack of interpersonal skills was found to be problematic. Chamberlain (Reference Chamberlain2006) reported that concerns about professionals treating them with distrust, and a lack of empathy when concerning ‘invisible symptoms’, such as headaches. Another study found that distrust exhibited by providers regarding symptoms resulted in service users feeling their integrity and self-esteem was impacted (Snell et al., Reference Snell, Martin, Surgenor, Siegert and Hay-Smith2017). While the ability of a provider to ensure the service user feels acknowledged in itself is important, the focus placed on trust, and acknowledging invisible symptoms that emerges in the literature seems to intersect with provider expertise. Knowledge and the validation and acknowledgement of brain injury-specific symptoms appears critical.
Sensitivity emerged as a valued quality, particularly when delivering bad news (Dwyer et al., Reference Dwyer, Heary, Ward and MacNeela2019). Review of the studies indicate that this lack of sensitivity on part of the health professionals often resulted in the diminishing of individuals hope (Chamberlain, Reference Chamberlain2006). The importance of qualities which foster a good relationship between the service user and provider points to the importance of an ongoing relationship with the provider (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Brauer et al., Reference Brauer, Hay and Francisco2011; Rusconi & Turner-Stokes, Reference Rusconi and Turner-Stokes2003; Simpson, Mohr & Redman, Reference Simpson, Mohr and Redman2000; Winkler, Farnworth, Sloan & Brown, Reference Winkler, Farnworth, Sloan and Brown2011). The results of the reviewed studies indicate that service users valued ongoing treatment with a single provider that they had developed a relationship with, and therefore understood their history and progress. Likewise, lack of an ongoing relationship with a provider emerged as challenging. Findings of one study outlined that high levels of changeover in staff resulted in the inability to implement recommended rehabilitation advice, prescribed to reduce pain in an individual with severe ABI (Winkler et al., Reference Winkler, Farnworth, Sloan and Brown2011). The importance of provider interpersonal skills are highlighted by resultant impacts to the service user. A lack of trust and knowledge of their previous history may result in recommendations not being adhered to, or service users not feeling enabled to ask questions which can best facilitate their recovery.
Synthesis of the literature suggests that the impact of provider interpersonal qualities on service user experience can be exacerbated in people from different cultures, service users already at more risk of experiencing social isolation and stigma (Mbakile-Mahlanza, Manderson & Ponsford, Reference Mbakile-Mahlanza, Manderson and Ponsford2015; Simpson et al., Reference Simpson, Mohr and Redman2000). Simpson et al. (Reference Simpson, Mohr and Redman2000) conducted a study in Australia interviewing people with TBI and their families from Italian, Lebanese and Vietnamese backgrounds. Participants reported a lack of sensitivity on behalf of the providers, and some valued interpersonal qualities such as friendliness or attentiveness more so than providers experience or expertise. This points to the importance of cultural competency of providers when defining appropriateness.
Partnership. The third prevalent theme relating to characteristics of providers was the partnership between the service user and provider. Importantly, the partnership was integral to the experience of choice and control within the interaction and whether there was a sense of appropriateness. This included the ability of the provider to foster a relationship that emphasised collaborative care with the service user being actively involved in decisions and goals of their care. Partnership emerged as a key factor in facilitating return to work. The reviewed studies emphasised that communication and transparency between the provider, the service user and the employer created a partnership which was crucial for successful return to work (Matérne, Lundqvist & Strandberg, Reference Matérne, Lundqvist and Strandberg2017; Soeker, Van Rensberg & Travill, Reference Soeker, Van Rensburg and Travill2012). This suggests that good partnerships can assist in the management of challenges across the continuum.
Gill et al. (Reference Gill, Wall and Simpson2012) found that service users with ABI valued when providers offered suggestions based on the service users interests and gave the service user the choice of whether to engage with this recommendation. The service users felt their autonomy was valued by staff who utilised these tactics and reported a positive, collaborative relationship with them as a result. This is corroborated by other reviewed literature suggesting that the ability of the staff to facilitate autonomy in service users with ABI was viewed as a positive quality (Lefebvre, Pelchat, Swaine, Gelinas & Levert, Reference Lefebvre, Pelchat, Swaine, Gelinas and Levert2005; Martin, Levack & Sinnott, Reference Martin, Levack and Sinnott2015; Soeker et al., Reference Soeker, Van Rensburg and Travill2012).
In contrast, providers who take an authoritative approach can contribute to a poor access experience. Abrahamson et al. (Reference Abrahamson, Jensen, Springett and Sakel2017) reported that service users felt frustrated as they were unsupported in their attempts to take control of their rehabilitation. This was reflected in the mismatch between the goal focus of professionals in contrast to service users. For example, professionals often focusing on short term goals, whilst service users desired to focus on the long-term goals. This issue with lack of control is evidenced by mismatched expectations between service users and providers specifically the acceptable distances to travel for therapies and reasonable lengths of time (Copley et al., Reference Copley, McAllister and Wilson2013). Conneeley (Reference Conneeley2012) reported that people with ABI feel that gains in their cognitive awareness over time were not reflected in greater responsibility or autonomy over rehabilitation decisions. This result is supported by Maratos et al. (Reference Maratos, Huynh, Tan, Lui and Jarus2016) findings that people with brain injury feel they can be constrained by the clinicians’ expectations as opposed to their abilities. Research has indicated that some people with ABI experienced providers being ‘overprotective’ and ‘clingy’ and treating them as ‘disabled’, which would result in the service user feeling disempowered (Glintborg, Thomsen & Hansen, Reference Glintborg, Thomsen and Hansen2018; Strandberg, Reference Strandberg2009). Jumisko, Lexell and Soderberg (Reference Jumisko, Lexell and Soderberg2007) found that service users reported that providers would be deliberately evasive when asked for additional information about their treatment, prognosis or asked for more rehabilitation. This resulted in a perceived poor relationship between the service user and provider.
This literature supports the need for patient directed care, when it comes to what is appropriate. Those with an ABI are often thrust into a role where decisions are being made for them not by them early on, due to injury and health professionals attitudes (Lefebvre et al., Reference Lefebvre, Pelchat, Swaine, Gelinas and Levert2005). The literature suggests that service users are more likely to engage actively with their care and rehabilitation when they are involved in the decisions and understand its purpose. Service users value being included and empowered, and the onus is on the providers to continue to attempt to do this across their recovery.
Adaptability. The fourth valued characteristic of providers is the extent to which providers are willing to accommodate varying service user needs and preferences in how they provide services, namely, the adaptability of the providers. This characteristic often coincided with provider expertise, suggesting that providers who have brain injury-specific knowledge are aware of the ongoing needs and more likely to make accommodations (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Brauer et al., Reference Brauer, Hay and Francisco2011; Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018). Dams-O’Connor et al. (Reference Dams-O’Connor, Landau, Hoffman and De Lore2018) found that patients with ABI valued providers adapting service provision to their specific needs, which included cognitive or memory limitations. The experiences reported in the research suggested the importance of providers who were willing to adapt the environment such as providing dimmed lighting or ensuring additional reminders of upcoming appointments (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018). Participants suggested that when providers made these accommodations it facilitated their ability to keep appointments and follow through with provider recommendations. Other physical accommodations are also valued, including adapting service timing (Jumisko et al., Reference Jumisko, Lexell and Soderberg2007) or the willingness to conduct sessions from the service user’s home, which was outlined in some Australian studies (Chan, Reference Chan2008; Doig, Fleming, Cornwell & Kuipers, Reference Doig, Fleming, Cornwell and Kuipers2011; Hall et al., Reference Hall, Grohn, Nalder, Worrall and Fleming2012). Doig et al. (Reference Doig, Fleming, Cornwell and Kuipers2011), interviewed people with TBI, their caregivers and occupational therapists soon after discharge from inpatient rehabilitation, and found that service users preferred to receive treatment at home as it gave them a sense of ownership of their therapy. Service users reported that this accomodation allowed caregivers to be involved and also avoided the trauma that could be triggered by being in a hospital setting (Doig et al., Reference Doig, Fleming, Cornwell and Kuipers2011). The theme of adaptable provision also emerged in regards to the timing of services, with emphasis on the importance of participant readiness for services, and therefore the need for services to be adaptable to the service user (Copley et al., Reference Copley, McAllister and Wilson2013; O’Callaghan, McAllister & Wilson, Reference O’Callaghan, McAllister and Wilson2012b). The emphasis on adapting the model of provision was evident in the reviewed literature. The more adaptable services seem to result in increased opportunity to fit services to need and subsequently, more likelihood of maintaining engagement of the service user.
Characteristics of the service system
Characteristics of the service systems have an impact on the experiences and perceptions of access, both in terms of what is realised and whether it is matched to service users’ needs. Synthesis of the themes are outlined below.
Navigable system. When considering the appropriateness of their access experience, being enabled to locate and navigate access according to needs was highlighted in several studies on experiences of people with ABI. A central feature of this was being informed. Research indicated that information about services was not provided consistently throughout the recovery trajectory and that often the information was insufficient (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018; Graff, Christensen, Poulsen & Egerod, Reference Graff, Christensen, Poulsen and Egerod2018; Schulz-Heik et al., Reference Schulz-Heik, Poole, Dahdah, Sullivan, Adamson and Date2017). The literature reflected that service users felt they were often provided with extensive information during inpatient rehabilitation; however, this stopped after discharge (Hall et al., Reference Hall, Grohn, Nalder, Worrall and Fleming2012; Rusconi & Turner-Stokes, Reference Rusconi and Turner-Stokes2003). This poses a significant problem given the memory deficits common in early stages of recovery of ABI. One study’s findings relayed suggestions from service users that additional written resources that might ensure the information was assessable later in recovery trajectories (Hall et al., Reference Hall, Grohn, Nalder, Worrall and Fleming2012).
The literature emphasised that service users perceived a general lack of information about where to go for rehabilitation, or further information about the rehabilitation (Graff et al., Reference Graff, Christensen, Poulsen and Egerod2018; Harrington, Foster & Fleming, Reference Harrington, Foster and Fleming2015; Pickelsimer et al., Reference Pickelsimer, Selassie, Sample, Heinemann, Gu, J. and Veldheer2007). Graff et al. (Reference Graff, Christensen, Poulsen and Egerod2018) suggested that people with TBI felt a lack of transparency at an organisation level, such that there was no information on where to find appropriate rehabilitation, whom to contact about duration of symptoms or when to return to work. The study findings indicated participants felt that often those with severe TBI were supported to access care after discharge from hospital, for example they were allocated a case worker. However, those with moderate or mild TBI felt they were left to attempt to manoeuvre the system alone. Another study further supported the emphasis on the utility of the case management role to facilitate service users’ access, however, found that only five participants were receiving this support at three months post-discharge (Turner, Fleming, Ownsworth & Cornwell, Reference Turner, Fleming, Ownsworth and Cornwell2011a). This research emphasises the need for provider and service-driven follow-up and continuity, with service users not feeling equipped to seek and utilise the information that is required and reporting they have to ‘chase the care’ to receive the services and support they need (Hyatt, Davis & Barroso, Reference Hyatt, Davis and Barroso2014).
Integrated care. Integrated care was a further feature of appropriate personal experiences of access. Ongoing provision of service throughout the recovery trajectory was a valued element of access (Hooson et al., Reference Hooson, Coetzer, Stew and Moore2013; Lefebvre & Levert, Reference Lefebvre and Levert2012; Strandberg, Reference Strandberg2009). This research suggested that people with ABI often felt their care was disjointed. In particular, studies exploring experiences in the first year after discharge in Australia revealed that service users often experienced a lack of continuity from the hospital to the community (Chamberlain, Reference Chamberlain2006; Hall et al., Reference Hall, Grohn, Nalder, Worrall and Fleming2012; Turner et al., Reference Turner, Fleming, Cornwell, Worrall, Ownsworth and Haines2007; Turner, Fleming, Ownsworth & Cornwell, Reference Turner, Fleming, Ownsworth and Cornwell2008, Reference Turner, Fleming, Ownsworth and Cornwell2011a, Reference Turner, Fleming, Ownsworth and Cornwell2011b). The period of time moving back into the community from in-patient rehabilitation has been shown to be a critical time, in which appropriate available services can facilitate transitions (Turner et al., Reference Turner, Fleming, Cornwell, Worrall, Ownsworth and Haines2007; Turner et al., Reference Turner, Fleming, Ownsworth and Cornwell2008). Results of a study by Turner et al. (Reference Turner, Fleming, Ownsworth and Cornwell2011a) suggested that the organisation of ongoing post-acute care services was often not completed as part of the discharge preparation process, and therefore families were often required to do this themselves, resulting in delays. These delays in service provision in those with ABI can result in the exacerbation of existing problems (Copley et al., Reference Copley, McAllister and Wilson2013; Leith, Phillips & Sample, Reference Leith, Phillips and Sample2004; O’Callaghan et al., Reference O'Callaghan, McAllister and Wilson2012a, Reference O’Callaghan, McAllister and Wilson2012b). The reviewed literature emphasised that service users’ needs are often time-dependent, one study found that support with guidance and planning was often vital right after discharge (Rotondi, Sinkule, Balzer, Harris & Moldovan, Reference Rotondi, Sinkule, Balzer, Harris and Moldovan2007).
Additionally, the reviewed research suggests that integration of care between providers is a issue for the appropriate access of people with ABI (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018; Lefebvre & Levert, Reference Lefebvre and Levert2012; Strandberg, Reference Strandberg2009). In one study participants indicated that they were able to effectively solve problems that emerged during their healthcare through medical providers collaborating on a care plan, discussing medication needs, or being referred to specialists who maintained regular contact with the referring provider (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018).
Results of the reviewed literature indicated a need for a care coordinator. The literature suggested that service users would value a key contact, coordinator or case manager to assist with communicating with all the services, ensuring collaboration between providers (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Copley et al., Reference Copley, McAllister and Wilson2013; Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018; Graff et al., Reference Graff, Christensen, Poulsen and Egerod2018; Hyatt et al., Reference Hyatt, Davis and Barroso2014; Umeasiegbu, Waletich, Whitten & Bishop, Reference Umeasiegbu, Waletich, Whitten and Bishop2013). However, this literature indicates that people with ABI are rarely able to have access to someone who would take on this role. Frequently it emerged that those who had caregivers, to advocate on their behalf, felt they were able to access the care they needed and supplement this lack of a key contact (Copley et al., Reference Copley, McAllister and Wilson2013; Graff et al., Reference Graff, Christensen, Poulsen and Egerod2018; Harrington et al., Reference Harrington, Foster and Fleming2015; Harrison et al., Reference Harrison, Hunter, Thomas, Bordy, Stokes and Kitzman2017).
Adequacy. Adequacy of services received emerged as a theme in the literature. Inconsistency in the quality and sufficiency of provision from service providers was evident as a key issue when considering appropriate access for those with an ABI. The reviewed literature suggests that service users perceived varied quality in services they received and that providers were inconsistent in the level of effort they demand from service users, often resulting in poor improvement (Brauer et al., Reference Brauer, Hay and Francisco2011; Rotondi et al., Reference Rotondi, Sinkule, Balzer, Harris and Moldovan2007). One study found that people with moderate and severe ABI described a mismatch between service users’ needs and clinician focus, in that often clinicians would focus on the physical and practical issues, resulting in service users with a lack of psychological support (Glintborg et al., Reference Glintborg, Thomsen and Hansen2018). Aligning with this, a study in war veterans reported that service users felt that providers were often treating symptoms as opposed to addressing the cause of the issues, which resulted in service users feeling the treatment was ineffective (Hyatt et al., Reference Hyatt, Davis and Barroso2014).
In addition to quality, sufficiency in the quantity emerged as important. Service users felt they accessed less than what they perceived they needed for maximal recovery, which ultimately resulted in these services failing to meet their needs (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Gill et al., Reference Gill, Wall and Simpson2012; Lexell et al., Reference Lexell, Alkhed and Olsson2013; Turner et al., Reference Turner, Fleming, Ownsworth and Cornwell2011a; Umeasiegbu et al., Reference Umeasiegbu, Waletich, Whitten and Bishop2013). This aligns with concerns around receiving the right service at the right time. One component of receiving the right service at the right time is the fit of the service to the need of the service user. The ability to provide service users with this service when needed is reliant on the current system waiting and response times. The literature suggests that service users experience significant waiting times to access the services they need (Glintborg et al., Reference Glintborg, Thomsen and Hansen2018), and unexplained delays in service commencement after services have been approved (Abrahamson et al., Reference Abrahamson, Jensen, Springett and Sakel2017; Leith et al., Reference Leith, Phillips and Sample2004; Turner et al., Reference Turner, Fleming, Ownsworth and Cornwell2011a). The notion of the right service at the right time, including the perceived intensity and frequency of services, echoes the emphasis on how the ideal of service user choice and control can be difficult to achieve in practice. The ability to provide service users with the right service at the right time is enabled by both system and individual-level factors. Research in this area suggests that not only is optimal care facilitated by access to the right service, but access to this service based on the individual’s recovery timeline and at their own pace at the right dose.
Opportunity. Opportunity to access appropriate services was reflected in experiences of those who were unable to access resources in particular areas, particularly regional and rural areas due to lack of availability (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018; Keightley et al., Reference Keightley, Kendall, Jang, Parker, Agnihotri and Colantonio2011; Mitsch, Curtin & Badge, Reference Mitsch, Curtin and Badge2014). This lack of opportunity of access also emerged with regards to funding (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; Harrington et al., Reference Harrington, Foster and Fleming2015; Leith et al., Reference Leith, Phillips and Sample2004; O’Callaghan et al., Reference O’Callaghan, McAllister and Wilson2010). Those receiving different funding were given the opportunity to access different services and different dosage of services, as opposed to accessing the services depending on their needs (Braaf et al., Reference Braaf, Ameratunga, Christie, Teague, Ponsford, Cameron and Gabbe2019; O’Callaghan et al., Reference O’Callaghan, McAllister and Wilson2010). Research emphasises that often service users were restricted from accessing speciality providers due to funding restrictions, cost and transportation (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and De Lore2018; Maratos et al., Reference Maratos, Huynh, Tan, Lui and Jarus2016; Toor et al., Reference Toor, Harris, Escobar, Yoshida, Velikonja and Rizoli2016; Umeasiegbu et al., Reference Umeasiegbu, Waletich, Whitten and Bishop2013). Research conducted in the USA has consistently reported that people with a TBI, are often denied access due to rigid service criteria, and policies (Leith et al., Reference Leith, Phillips and Sample2004; Pickelsimer et al., Reference Pickelsimer, Selassie, Sample, Heinemann, Gu, J. and Veldheer2007; Wyse, Pogoda, Mastarone, Gilbert & Carlson, Reference Wyse, Pogoda, Mastarone, Gilbert and Carlson2020). In addition to being denied the opportunity to access to needed services, the research indicated that there is often a lack of opportunity to access appropriate resources altogether. Several studies revealed that often young people with an ABI were forced to receive care from nursing homes, as these were the only available facilities that could accommodate their needs (Eliacin et al., Reference Eliacin, Fortney, Rattray and Kean2018; Graff et al., Reference Graff, Christensen, Poulsen and Egerod2018; Winkler et al., Reference Winkler, Farnworth, Sloan and Brown2011). In an Australian study, interviews were undertaken with those who had transitioned from an aged care facility to community-based accommodation (Winkler et al., Reference Winkler, Farnworth, Sloan and Brown2011). Results suggested that when enabled to access more appropriate services, service users were able to make significant improvements in functional life skills, for example being able to regain continence, and engage in feeding themselves, as opposed to using feeding tubes and adult continence pads.
The need for opportunity to access appropriate resources emerged in several studies, which found that often the providers and resources available were not available in specific languages for people with brain injury, and there was no availability of translating services (Keightley et al., Reference Keightley, Kendall, Jang, Parker, Agnihotri and Colantonio2011; Mbakile-Mahlanza et al., Reference Mbakile-Mahlanza, Manderson and Ponsford2015; Mitsch et al., Reference Mitsch, Curtin and Badge2014). Likewise, there was a lack of culturally sensitive access for people with brain injury, which may contribute to the often-compounded disadvantage experienced by these groups. This suggests that despite shifts in policies and services aligning with choice and control for service users, and provision of service based on need, people are still limited in their opportunity to access services appropriate to their needs.
Discussion
The current study used a scoping review to identify key characteristics of ‘appropriate’ access, as defined by the personal experiences of adults with ABI to post-acute care services. The present study revealed that while some service users reported positive experiences in receiving services post-discharge, many were not receiving the right fit for their needs. Features of these services and providers such as expert knowledge and their interpersonal qualities, adaptability and collaborative partnerships with providers have emerged as important factors when understanding appropriate access for people with a brain injury. Results highlighted the issues at the system-level pertaining to a lack of communication and cooperation between providers, leaving service users to manage their care on their own. Results revealed a lack of research in the first few months after discharge with a majority of the studies sampling participants with an average of over 1-year post-injury, with some studies sampling participants ranging over 10 years in difference in time post-injury. Additionally, a majority of the review literature was a qualitative design. This highlights that although there is emerging evidence about what is appropriate access to post-acute care services, to verify and elaborate on these findings there is a need for research focused on access in the period after discharge, utilising mixed designs, and addressing both system-level and provider-level factors.
The features of services and providers that emerged as key centred around interpersonal qualities, being collaborative and brain injury-specific knowledge. This supports previous findings that, despite the emphasis on person-centred healthcare, traditional didactic approaches are still used and are problematic for service users (Jackson et al., Reference Jackson, Hamilton, Jones and Barr2019). Furthermore, a quality relationship appears to underpin subsequent care experiences, resulting in the service user feeling safe and empowered to ask questions and engage in their care which enables them to adhere to recommendations. The sometimes ‘invisible’ nature of brain injury (Chamberlain, Reference Chamberlain2006), but equally complex presentation, further underscores the importance of quality provider relationships and the importance of specialist knowledge. Memory impairment, fatigue, ‘inappropriate’ or impulsive behaviours, inability to modulate their speech, and lack of self-awareness often manifest following brain injury (Fleminger & Ponsford, Reference Fleminger and Ponsford2005; Kumar et al., Reference Kumar, Kumar and Singh2019). Previous literature has emphasised the stigma experienced by those with ABI by community and health professionals alike for ‘malingering’ or deviant ‘mad’ behaviour (Simpson et al., Reference Simpson, Mohr and Redman2000; Simpson, Simons & McFadyen, Reference Simpson, Simons and McFadyen2002). The emphasis on expertise reported presently may align with the stigma and inner distress of not having validation for their concerns and needs. This provides key targets of intervention that could improve access experiences for those with ABI. Interpersonal skills, patient-centred care and specialised brain injury knowledge competencies and training might facilitate and improve experiences and outcomes.
Results highlighted the issues around continuity of care evident in the health systems with service users concerns about having a navigable system and integrated care emerging as connected. Service users, who were often unable to find the information or resources to navigate the system on their own, wished for integrated collaborative systems of care to address the gaps and uncertainties across the recovery trajectory. This suggests that the system is unable to provide the road map to services and recovery between providers across the recovery timeline, likely due to health professionals lacking time, incentives and a medium to collaborate on patients care. This seems to be resultant from the structure and process of the ‘inpatient’ versus ‘community care’ rehabilitation model. Whilst changes in policies evidenced by the introduction of schemes such as NDIS and NIIS in Australia have been implemented to increase the choice and control of the service users, the resource-limited nature of services have not been adapted to support this model. The siloed nature of health services often results in a lack of communication and cooperation between providers, leaving service users to manage their care on their own (Rusconi & Turner-Stokes, Reference Rusconi and Turner-Stokes2003; Turner et al., Reference Turner, Fleming, Cornwell, Worrall, Ownsworth and Haines2007). As a result, service users are unequipped to navigate the system and are left unable to design and implement the healthcare that is the best fit for their needs. This is highlighted by the focus in the literature on the value of a key advocate managing the overall care and communication between providers. The role of a key coordinator emerged as important to bridge the existing gap between providers through assisting in care navigation. This suggests the need for a deeper understanding of the mix of services, the roles and relationships between health professionals and the importance of characteristics that people with ABI value in their access experiences.
This review also suggests that opportunity to access services is also integral to a personalised understanding of appropriateness of access. From the review findings, however, there was an evident disparity in the opportunity for access. Some studies reported on the impact of variations in opportunity for age appropriate and culturally sensitive services (Keightley et al., Reference Keightley, Kendall, Jang, Parker, Agnihotri and Colantonio2011; Simpson et al., Reference Simpson, Mohr and Redman2000; Winkler et al., Reference Winkler, Farnworth, Sloan and Brown2011). The literature also emphasised the disparity in opportunity according to location, particularly less specialised, available, timely services in rural and regional communities (Copley et al., Reference Copley, McAllister and Wilson2013; Eliacin et al., Reference Eliacin, Fortney, Rattray and Kean2018). This disparity relates to the rural health workforce and lack of specialised knowledge of brain injury, due to the difficulty in recruiting and retaining health care professionals in remote geographic locations or due to a rotating system or FIFO (Mitsch et al., Reference Mitsch, Curtin and Badge2014). Notably, to enable choice and control, policy can influence the distribution of resources across geographical locations and therefore, the access experiences of people with ABI.
Implications and Recommendations
A significant majority of the work that has been conducted focusing on appropriateness of post-acute care services is qualitative. Whilst providing rich data on personal experiences, there is a need for quantitative data to analyse trends and patterns in larger cohorts (McCusker & Gunaydin, Reference McCusker and Gunaydin2015). Quantitative measurement of an individual’s experiences of services and their injury is challenging. Much of the quantitative work uses measures of met and unmet needs, and facilitators and barriers to services to capture information about post-acute service access (Pickelsimer et al., Reference Pickelsimer, Selassie, Sample, Heinemann, Gu, J. and Veldheer2007; Schulz-Heik et al., Reference Schulz-Heik, Poole, Dahdah, Sullivan, Adamson and Date2017; Solovieva & Walls, Reference Solovieva and Walls2014; Toor et al., Reference Toor, Harris, Escobar, Yoshida, Velikonja and Rizoli2016). However, research concentrating on needs assessments in this population has primarily focused on the emotional, cognitive and social needs rather than the provision of services that may occur in response to those needs (Andelic, Soberg, Bernsten, Sigurdardottir & Roe, Reference Andelic, Soberg, Berntsen, Sigurdardottir and Roe2014). This work provides some insight into the unmet needs of this population, however, it still fails to capture the complexity around the fit for need of the mix of services for the service user and their experience of adequacy of services received. A more in-depth conceptualisation of met and unmet needs is needed to begin to understand the complexity of access in this population.
This review illustrated that despite the knowledge base emphasising the first six months after discharge as critical targets for ongoing recovery, and typically challenging times for those with ABI, there is a dearth of research exploring the access experiences of people with a ABI in the months after discharge (Nalder et al., Reference Nalder, Fleming, Foster, Cornwell, Shields and Khan2012; Turner, Fleming, Cornwell, Haines & Ownsworth, Reference Turner, Fleming, Cornwell, Haines and Ownsworth2009). A majority of the studies sampled participants with an average of over 1-year post-injury, with some studies sampling participants ranging over 10 years in difference in time post-injury (Eliacin et al., Reference Eliacin, Fortney, Rattray and Kean2018). Given the themes relating to the changes in information and support needs over time, longitudinal research focusing on the early stages after discharge seems to be needed.
Results of this review highlight the need to address characteristics at the structural and policy level, through further targeted research and service user input at the design level. Since the implementation of the NDIS in Australia, there is increasing interest in the evaluation of such schemes and the subsequent impact on those with disability. Further research is needed to explore the utility of funding schemes in terms of personalised appropriateness of access for those with ABI. Analysis in relation to country and policies was beyond the scope of the present work. This is a limitation and further research into the implications of country and policies are needed to fully understand the systemic impact.
Limitations
The limitations of utilising a scoping review mean that it is possible that some articles were missed. Studies in Australia had the highest proportion of those included in this scoping review, this could potentially be resultant of missed articles due to international terms. Due to the complex nature of the concept of access, there is a vast range of terms for services and experiences. This can result in difficulties developing an expansive list of search terms. To address this a rigorous method and a range of search terms and criteria were utilised to ensure the review was able to capture the related articles. The present article targeted articles focusing on acquired brain injury and therefore did not use specific terms such as ‘stroke’. Therefore articles only referring to the sample as people with stroke may have been missed. Additionally, only English articles were included. Given that access issues around culturally appropriate services emerged, it is possible that there is work in other languages that may be relevant. Consistent with the chosen methodology, articles were not formally appraised for quality, so there are limitations to the strength of conclusions drawn from the body of work.
Conclusions
Findings from this scoping review highlight a multitude of factors that characterise appropriate access based on the service access experiences and opportunities of adults with ABI after leaving inpatient rehabilitation. Whilst a critical appraisal was beyond the scope of this study, there were a range of aims and designs which were identified, and high variability in the sample sizes, the time since injury and discharge. This demonstrates that although there is emerging evidence about what is appropriate access to post-acute care services, to draw conclusions there is a need for rigorous, research, particularly focused on access in the period after discharge, utilising mixed designs, longitudinal follow-up, and addressing both system-level and provider-level factors.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Kirstyn Laurie is supported by a Australian Government Research Training Program (RTP) Stipend Scholarship.
Conflicts of interest
Kirstyn Laurie has no conflicts of interest to disclose. Michele Foster has not conflicts of interest to disclose. Louise Gustafsson has no conflicts of interest to disclose.






