Neurodevelopmental disorders, which include a variety of developmental problems with a common onset early in childhood, often lead to significant impairments in social, personal and academic functioning.Reference Morris-Rosendahl and Crocq1 Attention-deficit hyperactivity disorder (ADHD) is among the most common,Reference Zhou, Xia, Shen, Yang, Zhang and Xu2 with a worldwide prevalence of about 5%.Reference Polanczyk, de Lima, Horta, Biederman and Rohde3 In addition to the typical behavioural symptoms of inattention and/or hyperactivity/impulsivity,Reference Zhou, Xia, Shen, Yang, Zhang and Xu2 patients with ADHD have a high rate of comorbidity with other neurodevelopmental disorders.Reference Morris-Rosendahl and Crocq1 For instance, up to 65% of children with ADHD may also experience some behavioural symptoms of autism spectrum disorder (ASD).Reference Sokolova, Oerlemans, Rommelse, Groot, Hartman and Glennon4 On the other hand, difficulties in sustaining attention and impulse control, which are typical for patients with ADHD, are also frequently noted in patients with ASD and Tourette disorders.Reference Sokolova, Oerlemans, Rommelse, Groot, Hartman and Glennon4,Reference Oluwabusi, Parke and Ambrosini5 Despite the guideline recommendation of combining pharmacological and behavioural interventions for children diagnosed with ADHD,Reference Wolraich, Hagan, Allan, Chan, Davison and Earls6 management with comorbid disorders in ADHD could be more challenging.Reference Wolraich, Hagan, Allan, Chan, Davison and Earls6 Moreover, notwithstanding the effectiveness of pharmacological interventions for controlling the core symptoms of ADHD,Reference Rappley7 potential side-effects and stigma toward medication use frequently prevent caregivers of children with ADHD from seeking medical attention.Reference Searight, Robertson, Smith, Perkins and Searight8 This may partly explain the increasing popularity of alternative therapies for ADHD,Reference Searight, Robertson, Smith, Perkins and Searight8 which were sought by more than 60% of patients in a previous survey.Reference Stubberfield and Parry9
Probiotics for ADHD
Probiotics, which may contain different strains of microorganisms considered to offer health benefits,Reference Hill, Guarner, Reid, Gibson, Merenstein and Pot10 have been prescribed for a variety of neurodevelopmental disorders.Reference Ligezka, Sonmez, Corral-Frias, Golebiowski, Lynch and Croarkin11 The mechanism underlying the therapeutic potential of probiotics lies in the gut–brain axis, which serves as a route for bidirectional communication through neuroendocrinological pathways,Reference Cryan and Dinan12 and involves modulation of important neurotransmittersReference Asano, Hiramoto, Nishino, Aiba, Kimura and Yoshihara13,Reference Aarts, Ederveen, Naaijen, Zwiers, Boekhorst and Timmerman14 and suppression of inflammation.Reference Alipour, Homayouni-Rad, Vaghef-Mehrabany, Sharif, Vaghef-Mehrabany and Asghari-Jafarabadi15,Reference Kullisaar, Songisepp, Mikelsaar, Zilmer, Vihalemm and Zilmer16 Nevertheless, the results of previous investigations into the therapeutic benefits of probiotics in the treatment of ADHD symptoms remain inconsistent.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17–Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 Among the four randomised controlled trials (RCTs) that reported an improvement in ADHD symptoms after probiotic treatment,Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18,Reference Liu, Liong, Chung, Huang, Peng and Cheng21,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 only two showed a significantly better therapeutic effect in the probiotic group than the placebo group.Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 Variations in other factors, including differences in the number of probiotic strains used and whether probiotics were given as supplementation or an adjunct to psychostimulants, may also influence their therapeutic potency.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17–Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 However, there was no pooled evidence addressing either the therapeutic efficacy of probiotics for symptoms of ADHD or the potential factors that may influence their therapeutic efficacy.
The current study
Therefore, this meta-analysis was aimed at studying the effectiveness of probiotics for symptoms of ADHD, and identifying possible factors that may affect their therapeutic efficacy.
Method
Protocol and registration
The current meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.Reference Moher, Shamseer, Clarke, Ghersi, Liberati and Petticrew24 The protocol of this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO; identifier CRD42023409450).
Search strategy and selection criteria
Major databases, including PubMed, EMBASE, Cochrane CENTRAL, ScienceDirect, and Clinicaltrials.gov, were searched for RCTs investigating the efficacy of probiotics for ADHD treatment from inception to 6 April 2023. Detailed information regarding the keywords used for searching in individual databases is provided in Supplementary Table 1 available at https://doi.org/10.1192/bjo.2023.645. To maximise the scope of our search, we set no restrictions on language and ethnicity, and identified relevant studies from the reference lists of specific reviews or literature. We focused our study on children/adolescents instead of adults, because of variations in presentations of ADHD between the two populations that may require different scoring systems for evaluation.Reference Green, DeYoung, Wogan, Wolf, Lane and Adler25,Reference Leahy26 In addition, the suppressing effect of probiotics against central nervous system (CNS) inflammation, which is believed to play a key role in neurodevelopmental disorders,Reference Jiang, Cowan, Moonah and Petri27,Reference Davis, Aschner and Costa28 may vary in different stages of development. Our PICO (i.e. population, intervention, comparator and outcomes) criteria for study eligibility were (a) population: RCTs of patients diagnosed with neurodevelopmental disorders, aged <18 years; (b) intervention: probiotics or products including probiotics (i.e. synbiotics) used either as monotherapy or components of combination regimens; (c) comparator: placebo or interventions other than probiotics and (d) outcome: behavioural rating scales for assessing the total symptoms of ADHD and/or symptom subcategories of ADHD, including inattention, hyperactivity and impulsivity. Exclusion criteria were RCTs that did not target children or adolescents, studies using interventions unrelated to probiotics and studies without an outcome assessment for symptoms of ADHD.
Data extraction and quality assessment
By using the predefined keywords and search strategy (Supplementary Table 1), the titles and abstracts of the identified studies were screened by two independent authors (S.-C.L. and C.-H.C.). The eligibility of the included studies were determined through discussion between the two authors, who were also responsible for independent extraction of information, including publication-specific detail as well as characteristics and outcome data of eligible studies. All disagreements between the two authors were resolved by discussion with a third author (C.-K.S.). Kappa coefficient was used for assessing interrater reliability.Reference McHugh29 In cases of missing data, we attempted to contact the corresponding authors by email, for original data. Cochrane's ‘risk of bias’ assessment toolReference Higgins, Thomas, Chandler, Cumpston, Li and Page30 was used to rate the quality of the included studies in accordance with seven main categories: sequence generation, allocation concealment, performance bias, detection bias, attrition bias, reporting bias and other important biases. With regard to the certainty of evidence, the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework was used to rate the level of evidence for individual outcomes of interest.Reference Guyatt, Oxman, Vist, Kunz, Falck-Ytter and Alonso-Coello31 Any disagreement on risk of bias and certainty of evidence ratings was settled through discussion with a third author.
Data synthesis and analysis
Review Manager 5 for Windows (RevMan 5.4; The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen; 2014; see https://training.cochrane.org/online-learning/core-software/revman) was used for data analysis. The primary outcome of the study was improvement in the total symptoms of ADHD rated by standardised behavioural rating scales. Our secondary outcomes included improvement in the subcategories of ADHD symptoms, including inattention and hyperactivity/impulsivity, as well as treatment acceptability evaluated by comparing the drop-out rates between treatment and comparison groups. Because different behavioural rating scales (i.e. continuous variables) may be used to assess the same outcomes of interest, a random-effects model was chosen for the analysis of our primary outcome and the subgroup analysis of the effect of different therapeutic strategies on treatment outcome. Standardised mean differences (SMDs) with 95% confidence intervals were used to give an overall estimation of the effect size for therapeutic efficacy. As for categorical data, odds ratios with 95% confidence intervals were used. The generic inverse-variance method was chosen for outcomes of continuous variables, and the Mantel–Haenszel method was used for odds ratios. Subgroup analyses focusing on the choice of treatment strategy (i.e. monotherapy versus combination therapy) and the number of probiotic strains (i.e. multiple strains versus single strain) were also performed to identify the potential sources of heterogeneity and factors that may influence the therapeutic outcomes of probiotics. The reliability and robustness of outcomes were evaluated by using leave-one-out sensitivity analysis. For assessment of heterogeneity among the eligible studies, I 2-test was used. A P-value <0.05 was used for defining statistical significance for all study outcomes. A funnel plot was inspected to detect potential publication bias, whereas an Egger's regression test was used for the quantitative assessment of publication bias for more than ten sets of data.
Results
Study selection and characteristics of included studies
Figure 1 depicts the process of study selection according to the PRISMA statement.Reference Moher, Shamseer, Clarke, Ghersi, Liberati and Petticrew24 In short, 978 articles were identified from both published and unpublished databases, and eight additional articles were retrieved from relevant reviews or studies. Following the exclusion of 954 records after screening of titles and abstracts, as well as 25 articles through review of full texts (Supplementary Table 2), seven studies with a total of 397 participants were deemed eligible for study inclusion,Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17–Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 and the data from eligible studies were extracted on 10 April 2023. The kappa coefficient was 1, indicating complete agreement among all authors on study eligibility.
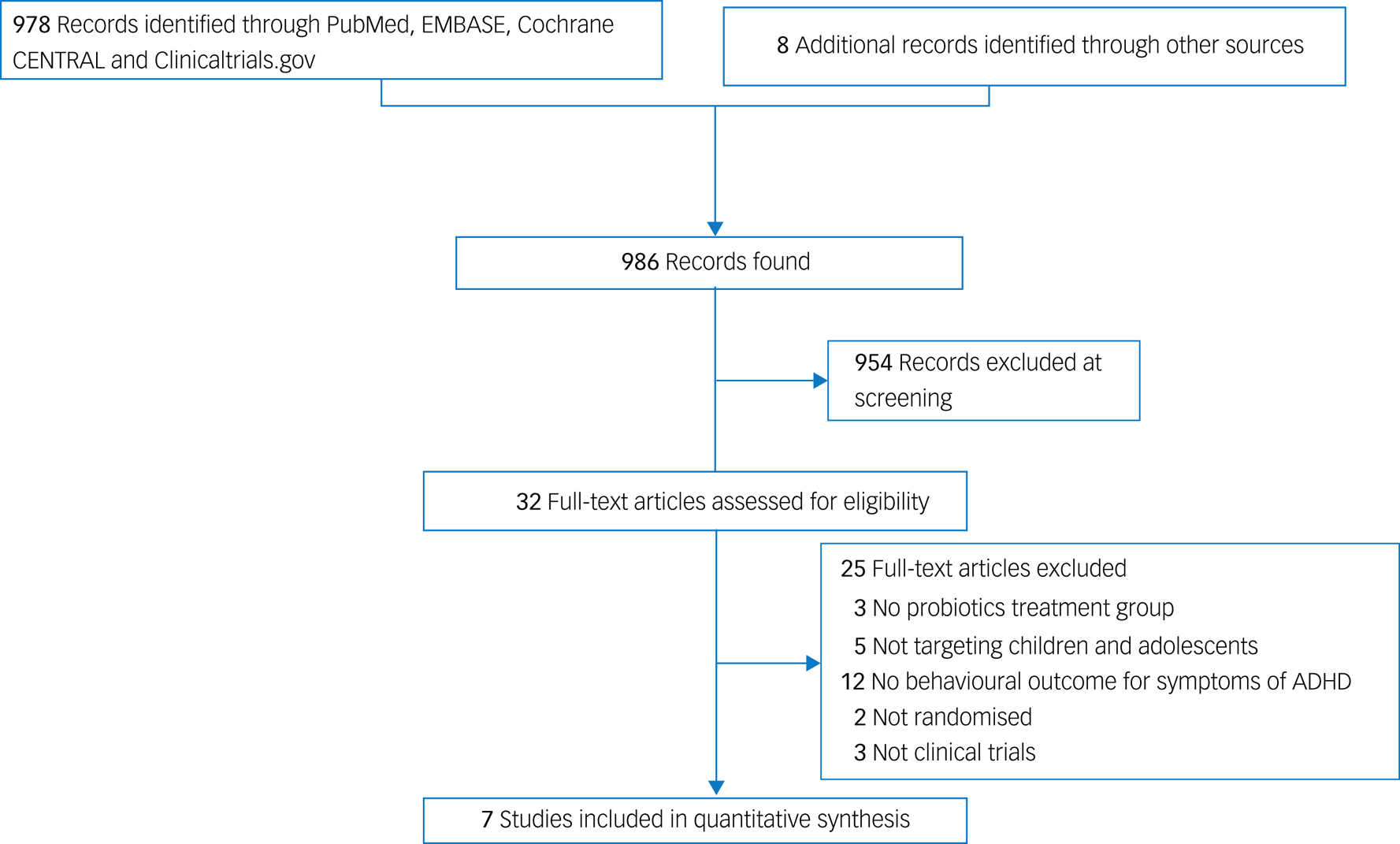
Fig. 1 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram of identifying eligible studies. ADHD, attention-deficit hyperactivity disorder.
Table 1 provides a summary of the characteristics of the included studies. The mean age of the participants was 10.37 years (range: 4–18 years), with a predominance of male participants (female participants: 0–31.6%). Five out of the seven studies recruited patients with a primary diagnosis of ADHD,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18–Reference Skott, Yang, Stiernborg, Söderström, Rȕegg and Schalling20,Reference Bazinet22,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 one enrolled participants diagnosed with ASDReference Liu, Liong, Chung, Huang, Peng and Cheng21 and the other recruited those with Tourette syndrome.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17 Three types of rating scales – the Swanson, Nolan, and Pelham (SNAP) scale; the Conners’ Parent Rating Scales – Revised (CPRS-r) and the Disruptive Behavior Disorder (DBD) rating scale – were used for outcome measurement. We compared the ratings from the same type of observers (e.g. parents) for each outcome, to reduce the risk of informant biases between different types of observers. Because only one study used ratings from teachers’ observations,Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17 we were unable to conduct statistical analysis for outcomes from the teacher's perspective. The median duration of treatment was 8 weeks (range: 4–12 weeks). Four out of the seven studies used multiple strains of probiotics, and three used a single strain (Table 1). All studies used the Lactobacillus family in their probiotics regimen, with Lactobacillus plantarum being most commonly used (i.e. two single-strain probiotic studies and two multiple-strain probiotic studies) (Table 1). Most studies allowed the use of psychotropics except for one,Reference Kumperscak, Gricar, Ülen and Micetic-Turk19 and two studies recruited participants receiving methylphenidate;Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 information regarding the use of psychotropics was not provided in two studies.Reference Liu, Liong, Chung, Huang, Peng and Cheng21,Reference Bazinet22 The geographic locations of the included trials were diverse, including two in the Middle East,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 two in Taiwan,Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Liu, Liong, Chung, Huang, Peng and Cheng21 two in EuropeReference Kumperscak, Gricar, Ülen and Micetic-Turk19,Reference Skott, Yang, Stiernborg, Söderström, Rȕegg and Schalling20 and one in North America.Reference Bazinet22
Table 1 Summary of characteristics of studies in the current meta-analysis

ADHD, attention-deficit hyperactivity disorder; RCT, randomised controlled trial; CPRS-r, Conners’ Parent Rating Scales – Revised; SNAP, Swanson, Nolan, and Pelham scale; ASD, autism spectrum disorder; DBD, Disruptive Behavior Disorder scale.
a Bacillus subtilis PXN 21, Bifidobacterium bifidum PXN 23, Bifidobacterium breve PXN 25, Bifidobacterium infantis PXN 27, Bifidobacterium longum PXN 30, Lactobacillus acidophilus PXN 35, Lactobacillus delbrueckii ssp. bulgaricus PXN 39, Lactobacillus casei PXN 37, Lactobacillus plantarum PXN 47, Lactobacillus rhamnosus PXN 54, Lactobacillus helveticus PXN 45, Lactobacillus salivarius PXN 57, Lactococcus lactis ssp. lactis PXN 63 and Streptococcus thermophiles PXN 66.
b Lactobacillus reuteri, Lactobacillus acidophilus, Lactobacillus fermentum and Bifidobacterium bifidum.
c Synbiotic 2000 comprises Lactobacillus plantarum, Pediococcus pentosaceus and Lactobacillus casei ssp. paracasei.
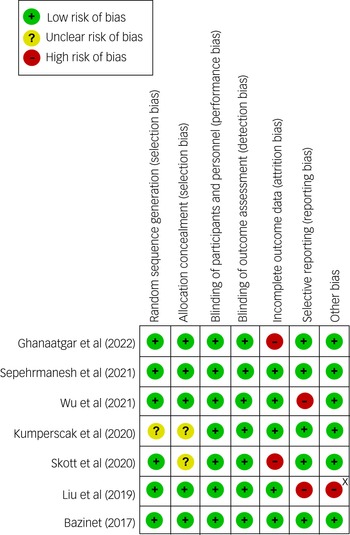
Risk-of-bias assessment
According to the Cochrane Collaboration's tool for risk-of-bias assessment in randomised trials, most studies had a low risk in detection and performance biases because of their double-blind, placebo-controlled trial design (Fig. 2). However, some studies did not have detailed descriptions about their randomisation process (Fig. 2). Taking into account that two studies had a high risk of reporting bias because they did not primarily focus on ADHD symptoms,Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Liu, Liong, Chung, Huang, Peng and Cheng21 the overall quality of evidence could be a concern.
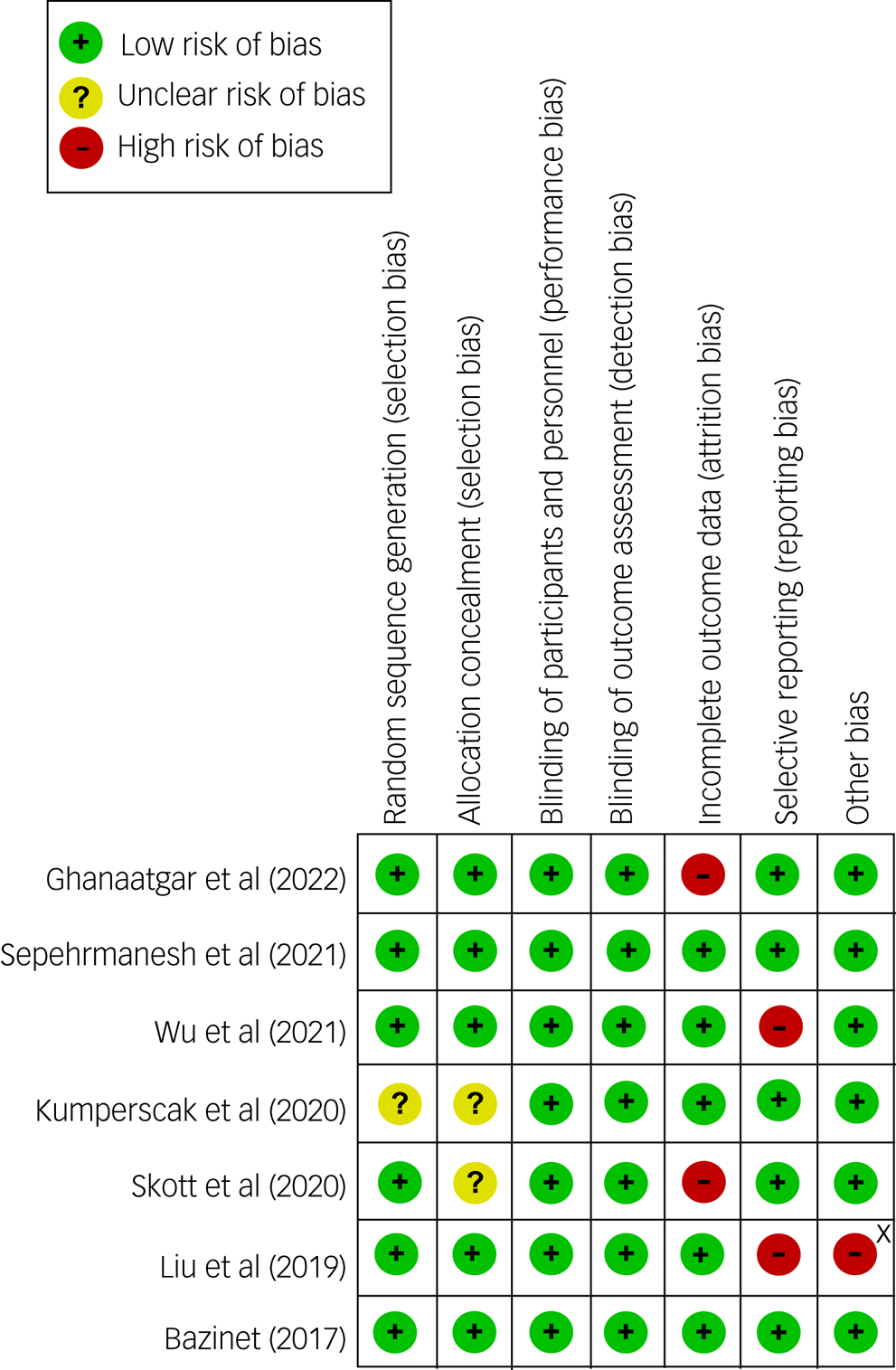
Fig. 2 Risk of bias for eligible studies. X, sponsored by a pharmaceutical company.
Primary outcome
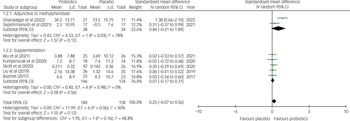
The current meta-analysis showed no significant difference in the improvement of the total symptoms of ADHD between the probiotic and placebo groups (SMD = 0.25, 95% CI −0.07 to 0.56; P = 0.12; seven studies with 342 participants) (Fig. 3). Despite no notable asymmetry on funnel pot inspection (Supplementary Fig. 1), there was a trend of heterogeneity on this outcome (I 2 = 50% and P = 0.06). Moreover, although robustness assessment with leave-one-out sensitivity test did not reveal any significant change in primary outcome, the heterogeneity of results was substantially reduced (I 2 = 0% and P = 0.98) after excluding the trial by Ghanaatgar et al, which was the only study demonstrating a significant improvement in ADHD total symptoms related to treatments with probiotics and methylphenidate compared with methylphenidate treatment alone,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18 indicating that study was an important source of heterogeneity. Our other subgroup analyses regarding treatment strategies (i.e. supplementation versus adjunct to methylphenidate) and number of probiotic strains (i.e. single versus multiple) did not reveal any significant difference between different subgroups (Fig. 4, Supplementary Figs 2 and 3). Nevertheless, a marked but non-significant difference in effect size was observed between the subgroup of studies using probiotics as an adjunct to methylphenidate and those using probiotics as a supplementation (SMD = 0.84 v. 0.07; P = 0.16) (Fig. 4). There was also a moderate but non-significant difference in effect size (SMD = 0.45 v. 0.03; P = 19) regarding the therapeutic effects of probiotics for the treatment of ADHD symptoms between those treated with multiple strains of probiotics and those treated with a single strain (Supplementary Fig. 3).
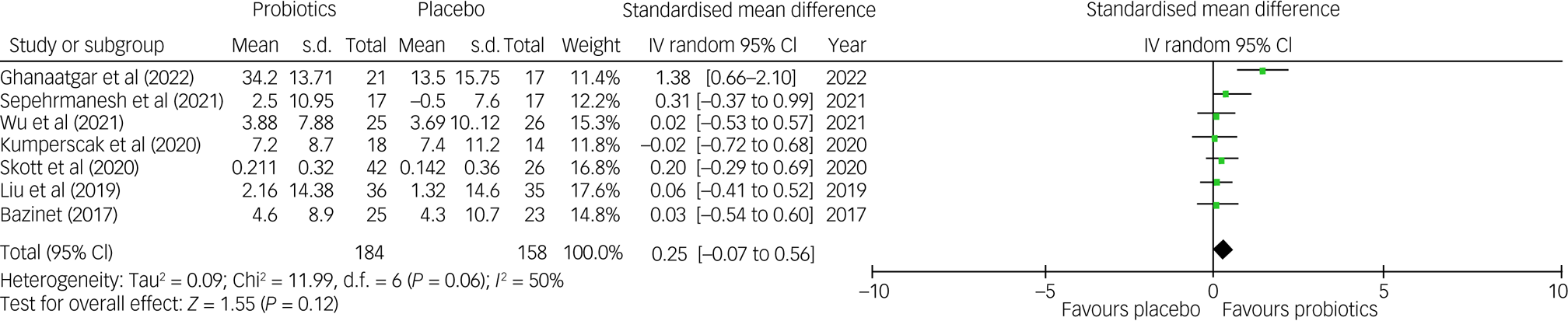
Fig. 3 Forest plot of effect size for comparing the difference in the improvement of total symptoms of ADHD between probiotics and placebo groups. ADHD, attention-deficit hyperactivity disorder; IV, inverse variance.

Fig. 4 Subgroup analysis showing a forest plot of effect sizes in a subgroup of studies using probiotics as supplementation versus an adjunctive to methylphenidate; IV, inverse variance.
Secondary outcomes
The results of secondary outcomes also failed to show significant improvement in the symptoms of inattention (SMD = 0.14, 95% CI −0.12 to 0.38; P = 0.3; four studies with 238 participants) (Supplementary Fig. 3) or hyperactivity/impulsivity (SMD = 0.08, 95% CI −0.18 to 0.34; P = 0.54; four studies with 238 participants) (Supplementary Fig. 4), compared with the controls. There was no significant heterogeneity, inconsistency on leave-one-out sensitivity analysis or notable asymmetry on funnel plot inspection for both outcomes (Supplementary Figs 5 and 6). There was also no significant difference in the drop-out rate between probiotics and comparison groups (odds ratio 0.99, 95% CI 0.54–1.83; P = 0.98; six studies with 361 participants) (Supplementary Figs 7 and 8).
Certainty of evidence
Supplementary Table 3 provides the details regarding the certainty of evidence for individual outcomes of interest. Given the limited number of eligible trials, problems with heterogeneity and the fact that two studies were not primarily designed for ADHD,Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Liu, Liong, Chung, Huang, Peng and Cheng21 the certainty of evidence was rated as very low for the primary outcome. The certainty of evidence was rated as low for secondary outcomes because there were only four studies with data availability, two of which did not focus primarily on the symptoms of ADHD.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Liu, Liong, Chung, Huang, Peng and Cheng21
Discussion
Despite the proposal of probiotics as a compromising therapeutic regimen for individuals with ADHD,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 its efficacy remains controversial.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18,Reference Liu, Liong, Chung, Huang, Peng and Cheng21,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 Also, the effects of other factors, such as the use of probiotics as a supplementation or adjunct to psychostimulants, as well as the number of bacterial strains being used, have not been adequately addressed. To the best of our knowledge, our meta-analysis is the first to investigate the efficacy of probiotics for the symptoms of ADHD in children and adolescents. Although our results failed to show superior efficacy of probiotics for the treatment of total or subdomain symptoms of ADHD compared with placebo groups, the limited number of eligible trials cannot rule out the potential therapeutic benefits in this population. In particular, one of the included studies that compared the therapeutic efficacy between participants receiving a combination of methylphenidate with multiple strains of probiotics and those receiving methylphenidate alone, demonstrated a therapeutic benefit of the combined regimen,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18 suggesting the potential merit of multiple-strain probiotics or the use of probiotics as an adjunct to methylphenidate. Moreover, despite a lack of statistical significance in our findings on subgroup comparisons, larger effect sizes in the subgroups of studies using multiple strains of probiotics or those combining probiotics with methylphenidate may provide a therapeutic insight into the potential adjunctive use of probiotics for ADHD.
The most important hypothesis underlying the relationship between intestinal microbiome and the CNS is the gut–brain axis, through which the gut microbiome and CNS may have bidirectional communication via a variety of neural, endocrine and inflammatory pathways.Reference Cryan and Dinan12 There is increasing evidence suggesting the involvement of intestinal microbiota in homeostasis of the entire body, including the CNS.Reference Cryan and Dinan12,Reference Mayer32 Regarding the possible mechanisms, an animal study demonstrated a possible role of the vagus nerve in the communication between the central gamma-aminobutyric acid (GABA) system and gut microbiome.Reference Bravo, Forsythe, Chew, Escaravage, Savignac and Dinan33 Further, the modulation of several important neurotransmitters, including norepinephrine and dopamine,Reference Dinan and Cryan34 by certain intestinal microbiota has been reported in both animal and human studies.Reference Asano, Hiramoto, Nishino, Aiba, Kimura and Yoshihara13,Reference Aarts, Ederveen, Naaijen, Zwiers, Boekhorst and Timmerman14 Also, the anti-inflammatory effects of some probioticsReference Alipour, Homayouni-Rad, Vaghef-Mehrabany, Sharif, Vaghef-Mehrabany and Asghari-Jafarabadi15,Reference Kullisaar, Songisepp, Mikelsaar, Zilmer, Vihalemm and Zilmer16 may be beneficial in the treatment of various neurodevelopmental disorders in which systemic and CNS inflammation may play a key role during the developmental period.Reference Jiang, Cowan, Moonah and Petri27,Reference Davis, Aschner and Costa28 Previous evidence has shown an association of a perturbation of the microbiome and gut–brain axis with a variety of neurodevelopmental disorders.Reference Ligezka, Sonmez, Corral-Frias, Golebiowski, Lynch and Croarkin11 Indeed, probiotics have been used as a therapeutic alternative for ADHD in several studies.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17–Reference Bazinet22 Nevertheless, despite the finding of a significant improvement in the symptoms of ADHD after treatment with probiotics in previous studies,Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Liu, Liong, Chung, Huang, Peng and Cheng21 most failed to demonstrate a significant difference between placebo effects and the therapeutic benefits of probiotics.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Kumperscak, Gricar, Ülen and Micetic-Turk19–Reference Bazinet22 In fact, only one out of the seven studies reported a significant therapeutic efficacy of probiotics compared with placebos.Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18 Another study also showed no difference in therapeutic effects between participants receiving probiotics adjunctive to methylphenidate and those treated with methylphenidate alone,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 despite emergence of statistical significance after adjusting for baseline values of age, body mass index and several biochemical variables (e.g. level of high-sensitivity C-reactive protein). Consistent with those findings, our meta-analytic results failed to support a superior therapeutic efficacy of probiotics compared with placebos in the treatment of symptoms of ADHD. On the other hand, taking into account the efficacy of multiple-strain probiotics (up to 14 strains) in one of the included studies,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18 as well as the significant therapeutic benefit of combining probiotics with methylphenidate compared with methylphenidate alone,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 it appeared that the efficacy of probiotics for the treatment of ADHD symptoms may be enhanced through a modification of the regimen.
With regard to the association between the composition of gut microbiota and the symptoms of ADHD, previous studies focused primarily on two aspects: (a) comparing differences in microbiome between patients with ADHD and healthy controls, and (b) investigating the diversity of intestinal microflora in ADHD and healthy populations.Reference Kalenik, Kardaś, Rahnama, Sirojć and Wolańczyk35 However, the results of those studies remain inconsistent, possibly as a result of a variety of methodological issues, including small sample sizes, differences in methods used for microbiome profiling and a lack of control for potential confounding factors such as diet, age and the presence of gastrointestinal diseases.Reference Kalenik, Kardaś, Rahnama, Sirojć and Wolańczyk35 For instance, the prevalence of Bifidobacterium was found to be lower in one report,Reference Kalenik, Kardaś, Rahnama, Sirojć and Wolańczyk35 but higher in another,Reference Aarts, Ederveen, Naaijen, Zwiers, Boekhorst and Timmerman14 among individuals diagnosed with ADHD than in controls. In contrast, the prevalence of the Lactobacillus family, which was the most commonly used strain of probiotics in our included studies, has been shown to be consistently lower in those with ADHD than in their healthy counterparts.Reference Pärtty, Kalliomäki, Wacklin, Salminen and Isolauri36,Reference Wang, Yang, Chou, Lee, Chou and Kuo37 Previous animal studies also reported an association of certain members of the Lactobacillus family with an increase in neurotransmitter release in the CNS,Reference Liu, Chuang, Huang, Wu, Chou and Wang38 as well as improved memory task performance in mice fed with Lactobacillus supplementation.Reference Ohland, Kish, Bell, Thiesen, Hotte and Pankiv39 Variations in the choice of probiotic strain and the diversity of microbiomes in the included studies may be two major reasons for the observed heterogeneity in our findings. Although the choice of probiotic strain may not be the major contributor (because all of our included studies used probiotic strains from the Lactobacillus family), the correlation between the diversity of microflora and ADHD symptoms remains unclear.Reference Kalenik, Kardaś, Rahnama, Sirojć and Wolańczyk35 Despite the report of a lower diversity of intestinal microflora in individuals diagnosed with ADHD than in their healthy counterparts in one study,Reference Prehn-Kristensen, Zimmermann, Tittmann, Lieb, Schreiber and Baving40 other studies did not find significant differences between the two groups.Reference Wang, Yang, Chou, Lee, Chou and Kuo37,Reference Szopinska-Tokov, Dam, Naaijen, Konstanti, Rommelse and Belzer41 In addition, the use of single versus multiple strains may contribute to a difference in efficacy. An in vitro study demonstrated that, compared with a single-strain regimen, a combination of multiple strains in probiotic supplementation may enhance its therapeutic benefits through an inhibition of other competing intestinal organisms.Reference Collado, Meriluoto and Salminen42 Concordantly, the only study that showed a superior therapeutic effect for the treatment of ADHD symptoms compared with the placebo group in our meta-analysis adopted a multiple-strain probiotic regimen.Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18 In agreement with this finding, a larger effect size reflecting a higher therapeutic efficacy was noted in studies that used multiple strains of probioticsReference Skott, Yang, Stiernborg, Söderström, Rȕegg and Schalling20,Reference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 than in those adopting single-strain regimens, despite a lack of statistical significance. Therefore, although current evidence is still not strong enough to support the superior therapeutic effects of the multiple strains of probiotics, the possibility of a more favourable therapeutic outcome associated with the use of multiple-strain probiotic regimens remains, and this requires further elucidation.
Focusing on the impact of therapeutic strategies on the efficacy of probiotics in this clinical setting, a subgroup comparison between the use of probiotics as an adjunct to methylphenidate and its use as supplementation revealed a much larger effect size for use as an adjunct to methylphenidate, despite a lack of statistical significance (SMD = 0.84 v. 0.07; P = 0.16). Interestingly, the only study that excluded the use of medication for ADHDReference Kumperscak, Gricar, Ülen and Micetic-Turk19 also showed the lowest effect size of efficacy for the treatment of ADHD symptoms. The pharmacological effects of methylphenidate for the treatment of ADHD symptoms are primarily derived from a modulation of the dopamine system,Reference Faraone43 and probiotics may improve neurocognitive functions through their anti-inflammatory effects.Reference Cryan and Dinan12 Nevertheless, given the limited number of included studies with non-significant findings, the possibility that probiotics may provide additional benefits through different pathways warrants further investigation.
An analysis of our secondary outcomes not only failed to show better therapeutic effects for probiotics than placebos for the treatment of symptoms of inattention and hyperactivity/impulsivity, but also demonstrated very low effect sizes (i.e. therapeutic efficacies) of probiotics for the two symptom entities (i.e. effect sizes of 0.14 and 0.08, respectively). Nevertheless, none of the studies that provided data for secondary outcome analysis used probiotics as an adjunctive treatment to methylphenidate, and most of them used only one or two strains of microflora in their probiotic regimens.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Kumperscak, Gricar, Ülen and Micetic-Turk19–Reference Bazinet22 Therefore, our findings could not exclude possible therapeutic effects of probiotics for the treatment of symptoms of inattention and hyperactivity/impulsivity when being used as an adjunct to medication or as multiple-strain regimens. Regarding acceptability, the lack of difference in drop-out rate between the treatment and placebo groups indicated satisfactory tolerance of probiotics among individuals with ADHD.
Although we were able to identify seven studies investigating the effects of probiotics for the treatment of ADHD symptoms, a high level of heterogeneity in our primary result underscored the importance of identifying possible confounding factors that may influence the observed therapeutic outcomes. The source of heterogeneity included patient-related factors (i.e. age, gender, dietary patterns, ethnicity),Reference Kalenik, Kardaś, Rahnama, Sirojć and Wolańczyk35 as well as those related to treatment strategies (i.e. duration of treatment, supplementation or adjunctive use of probiotics, choice of probiotics, number of probiotic strains in the product). Interestingly, although our leave-one-out sensitivity analysis demonstrated a substantial reduction in the level of heterogeneity (I 2 = 0% and P = 0.98) after excluding the trial by Ghanaatgar et al,Reference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18 the exclusion of another study conducted in the same country (Iran) that also used probiotics as an adjunctive to methylphenidateReference Sepehrmanesh, Shahzeidi, Mansournia, Ghaderi and Ahmadvand23 had no significant impact on heterogeneity. Therefore, the source of heterogeneity from the study by Ghanaatgar et alReference Ghanaatgar, Taherzadeh, Ariyanfar, Jahromi, Martami and Gharaei18 may be attributed to its distinctive feature of including up to 14 strains of probiotics in their treatment regimen, taking into account the reported synergistic effects of multiple strains of probiotics through inhibition of other competing intestinal organisms.Reference Collado, Meriluoto and Salminen42,Reference Ouwehand, Invernici, Furlaneto and Messora44 Such a finding may shed light on a possible direction for future studies focusing on enhancing the therapeutic effectiveness of probiotics for the treatment of ADHD symptoms.
There were several limitations in the present meta-analysis. First, our conclusion, derived from only seven RCTs with a total of 397 participants, was not robust enough to provide solid evidence for clinical practice. In particular, a near-significant heterogeneity in our results may suggest possible sources of heterogeneity. Our subgroup analyses further demonstrated a large difference in effect size between the subgroup of studies using probiotics as an adjunct to methylphenidate and those prescribing probiotics as supplementation, as well as a moderate difference in effect size between the subgroup of studies using multiple-strain probiotics and those adopting single-strain regimens. Further studies are required to elucidate the therapeutic benefits of probiotics, using different therapeutic approaches (e.g. single versus multiple strains). Second, potentially important confounders, such as the use of other nutritional supplements, were not controlled for in most of the included studies. Moreover, because of a lack of relevant information and the limited number of eligible studies, we could not conduct meta-regression to further investigate the effects of other important factors (e.g. age, duration of treatment and country of study) on the therapeutic efficacy of probiotics. Third, a median follow-up duration of merely 8 weeks in our included studies, with none of them having a follow-up period of over 12 weeks, precluded our exploration of the long-term benefits of probiotics in the treatment of ADHD. Fourth, the mean age of 10 years (range: 4–18 years) among the participants limited the extrapolation of our findings to younger children in an active stage of neurological development, whose response to probiotics may be different from that in their older counterparts. In fact, two previous studies reported beneficial effects of an early use of probiotics during the gestational period and early infancy on attentional and cognitive functions.Reference Pärtty, Kalliomäki, Wacklin, Salminen and Isolauri36,Reference Slykerman, Kang, Van Zyl, Barthow, Wickens and Stanley45 Fifth, despite no obvious asymmetry on the funnel plots, publication bias could not be reliably assessed because of the limited number of eligible trials (fewer than ten), which precluded the conduction of Egger's regression for statistical analysis. Moreover, taking into account previous evidence showing a significant decrease in the effect size of meta-analyses focusing on complementary and alternative medicine after excluding reports in languages other than English,Reference Moher, Pham, Lawson and Klassen46 our results may underestimate the effects of probiotics because of the possibility of language bias. Finally, two out of the seven included studies did not focus primarily on patients with ADHD, which contributed to an increased risk of reporting bias.Reference Wu, Wong, Hsu, Yang, Tsai and Cheng17,Reference Liu, Liong, Chung, Huang, Peng and Cheng21 Overall, given the potential risks of bias and other possible sources of heterogeneity in the present study, further large-scale investigations focusing on patients with ADHD are needed to provide more robust evidence regarding the therapeutic efficacy of probiotics for the treatment of ADHD symptoms.
In conclusion, our study showed no significant difference in therapeutic efficacy between probiotics and placebos for the treatment of ADHD symptoms. However, given the potential sources of heterogeneity and a high risk of attrition bias in some of the included studies, further clinical investigations are warranted to verify our findings. In addition, trends of better therapeutic efficacies observed in certain studies using multiple-strain probiotics or combining probiotics with methylphenidate may provide an avenue for further research to enhance the therapeutic efficacies of probiotics for ADHD.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2023.645
Data availability
The data-sets used and/or analysed during the current study are available from the corresponding author, K.-C.H., on reasonable request.
Author contributions
S.-C.L., C.-K.S. and C.-H.C. conceived and designed the study. Y.-S.C., R.-F.T., M.Y.W. and Y.-C.C. contributed to data extraction. Y.-S.C. and H.-J.C. analysed the data. S.-C.L., C.-K.S., C.-H.C. and K.-C.H. were major contributors to writing the manuscript. All authors contributed sufficiently to this work. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.







eLetters
No eLetters have been published for this article.