Schizophrenia is a major disabling illness which affects approximately 1% of the population worldwideReference McGrath, Saha, Chant and Welham1 and contributes 13.4 million years lived with disability to the global burden of disease.Reference Charlson, Ferrari, Santomauro, Diminic, Stockings and Scott2 Approximately one-third of patients with a schizophrenia spectrum diagnosis have treatment-resistant schizophrenia (TRS),Reference Lally and Maccabe3 i.e. they fail to respond to adequate trials of two different antipsychotics.Reference Howes, McCutcheon, Agid, de Bartolomeis, van Beveren and Birnbaum4
Tertiary services for complex TRS
Patients with TRS often have severe and enduring health needs;Reference Horsdal, Wimberley, Köhler-Forsberg, Baandrup and Gasse5 some are particularly difficult to manage in primary or secondary care and require a higher level of support.Reference Gudeman and Shore6 In the UK, tertiary care is defined as individualised and specialised multidisciplinary interventions delivered by highly trained staff in order to address problems that are complex and refractory to standard interventions.7 Tertiary services focus on high-intensity treatment of a relatively small number of the most difficult-to-treat individualsReference Ker and Anderson8 and offer specialist expertise with a high staff/patient ratio. Tertiary care programs for TRS should include individually tailored psychosocial rehabilitation, as well as personalised and evidence-based medication management, to achieve flexible and effective care.Reference Wasylenki, Goering, Cochrane, Durbin, Rogers and Prendergast9
Clozapine is the only recommended antipsychotic treatment for TRS and is the most effective agent for reducing symptoms,Reference Leucht, Cipriani, Spineli, Mavridis, Örey and Richter10 hospital use,Reference Siskind, Reddel, MacCabe and Kisely11 suicide rates,Reference Cho, Hayes, Jewell, Kadra, Shetty and MacCabe12,Reference Wimberley, MacCabe, Laursen, Sørensen, Astrup and Horsdal13 aggressive behaviour,Reference Patchan, Vyas, Hackman, Mackowick, Richardson and Love14 violent crimeReference Bhavsar, Kosidou, Orsini, Widman, Maccabe and Dalman15 and substance misuse.Reference Volavka16 However, the management of clozapine therapy for patients with severe and chronic behavioural problems requires carefully developed strategies and close monitoring of adverse effects, which can be challenging in a primary or secondary care setting. Clozapine has been found to be largely underutilised by prescribing clinicians,Reference Stroup, Lieberman, McEvoy, Davis, Swartz and Keefe17 with a considerable number of TRS patients being left on high-dose antipsychotics or polypharmacy,Reference Thompson, Clark, Legge, Kadra, Downs and Walters18 despite neither of these options having a good evidence base.Reference Dold and Leucht19,Reference Kadra, Stewart, Shetty, MacCabe, Chang and Kesserwani20
The National Psychosis Unit
The National Psychosis Unit (NPU) seeks to provide specialist evidence-based treatment for people with treatment-refractory psychosis, in order to reduce the risk of readmission and expensive long-term care costs. It is part of the National Psychosis Service (NPS), which produces out-patient and outreach assessments aimed at providing specialist input into the management of complex and refractory psychosis. The NPS is open to referrals from across the UK and beyond, and it offers an in-patient service to those patients who are deemed to need longer-term multidisciplinary and specialised input.
The NPU is an 18-bed mixed-gender in-patient facility situated within the Bethlem Royal Hospital and forms part of the South London and Maudsley (SLaM) NHS Trust. The NPU multidisciplinary team consists of psychiatrists, psychiatric nurses, pharmacists, social workers, and allied health professionals including occupational therapists and clinical psychologists. Furthermore, the NPU has an established close partnership with physical health physicians from King's Health Partners, including cardiologists and haematologists, enabling multidisciplinary medical discussions and support for the patients admitted.
Patients are referred to the NPU after treatments has failed to produce sufficient clinical improvement. Most patients are transferred from in-patient settings where they are detained under the Mental Health Act. They receive a comprehensive, multidisciplinary review of their previous psychiatric, medical and medication history, leading to an individualised care package which will typically include optimisation of pharmacological treatment and physical health, occupational therapy activities, social work input, and individual and family-based psychological interventions that have proven effective in reducing symptoms and distress and improving social functioning in TRS.Reference Perera, Broadbent, Callard, Chang, Downs and Dutta21 Optimisation of clozapine treatment, the management of its side-effects, clozapine re-challenge after suspected myocarditis, episodes of neutropenia or agranulocytosis, gastro-intestinal obstruction or other potentially life-threatening adverse effects, and issues regarding non-adherence constitute a large proportion of the work of the NPU. Another key element is the multimorbidity approach, which includes proactive physical health promotion including smoking cessation, physical exercise and weight control.
Although we have previously demonstrated short-term positive outcomes in patients admitted to the NPU,Reference Krivoy, Joyce, Tracy, Gaughran, MacCabe and Lally22,Reference Sarkar, Tracy, Fernandez, Nalesnik, Dhillon and Onwumere23 we have not described the longer-term outcomes. This study aimed to quantify the long-term effectiveness of treatment at the NPU by considering naturalistic outcome measures. Using a mirror image design, we used anonymised data from electronic health records to compare the number of psychiatric and general hospital admissions, in-patient days, acuity of placement, number of psychotropic medications and dose of antipsychotic medication prescribed before and after the treatment at the NPU.
Method
Data sources
Data were obtained from the Clinical Records Interactive Search (CRIS) system. CRIS is a large, de-identified psychiatric database sourced from SLaM electronic health records. It protects patient anonymity and maximises the data available for research. Developed in 2007, the CRIS application provides researchers with both structured and unstructured (open text) data in anonymised form from the full clinical record.Reference Perera, Broadbent, Callard, Chang, Downs and Dutta21
Age at admission to the NPU, gender, ethnicity, length of admission and date of death (when relevant) were obtained from CRIS structured fields.
Data on length of psychotic illness at admission, number of previous antipsychotic trials, acuity of residence before admission and after discharge, use of clozapine at admission and discharge, number of psychotropic medications, and antipsychotic medication dose at admission and discharge were manually collected from open text. The British National Formulary (BNF) total antipsychotic dosage was used to convert antipsychotic dosage into percentage of maximum recommended daily antipsychotic dose as per BNF guidelines.24
Data on psychiatric and general hospital admissions and Accident and Emergency (A&E) admissions during the 2 years before and the 2 years after NPU treatment were obtained by means of an anonymous linkage to the Hospital Episode Statistics (HES; https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics) system, a data warehouse containing details of all admissions at National Health Service (NHS) hospitals in England. The CRIS application is linked to the HES system; this ensures data anonymity.
Data definitions
This study used a mirror image design with the treatment at the NPU defined as the mirror. The period of 2 years prior to the date of admission to the NPU was used as the pre-mirror period, while a period of 2 years from the date of discharge was used as the post-mirror period. Data on number of admissions to psychiatric and general hospitals and to A&E during the pre- and post-mirror periods were collected, together with admission and discharge dates.
Medications at admission and discharge for which data were collected included antipsychotics, anticholinergics, benzodiazepines, mood stabilisers and antidepressants; dosages for antipsychotics were also collected. Pro re nata prescriptions were not considered.
Data on placements immediately before and after the admission to the NPU were categorised as psychiatric intensive care unit (PICU), acute ward, rehabilitation service, care home, supported accommodation and independent living (including living with family). They were ordered from the highest to the lowest intensity and were given a number from 1 to 6. The difference between pre-admission and post-discharge acuity was calculated.
Sample inclusion criteria
The cohort consisted of all patients ever admitted to the NPU after 1 January 2007 and discharged before 31 March 2015. This study period was selected because electronic records were fully implemented in SLaM in 2007, and admissions with a discharge date before 31 March 2015 allowed a 2-year follow up on the HES system, since the latest HES update available at the time of the study had data until 31 March 2017.
The process of cohort identification is detailed in Fig. 1. A total of 160 patients were included in the demographical analysis. Three patients were excluded from the mirror-image study because they died within the post-mirror period, and ten patients did not have a match in the HES database or had unreliable data (e.g. outliers). A total of 147 patients admitted to the NPU were included in the mirror-image study. A sensitivity analysis was conducted to address the issue of missing data due to lack of information in the HES system about patients coming from outside England. Seven patients residing outside England were therefore excluded, and 140 patients were included in the sensitivity analysis.
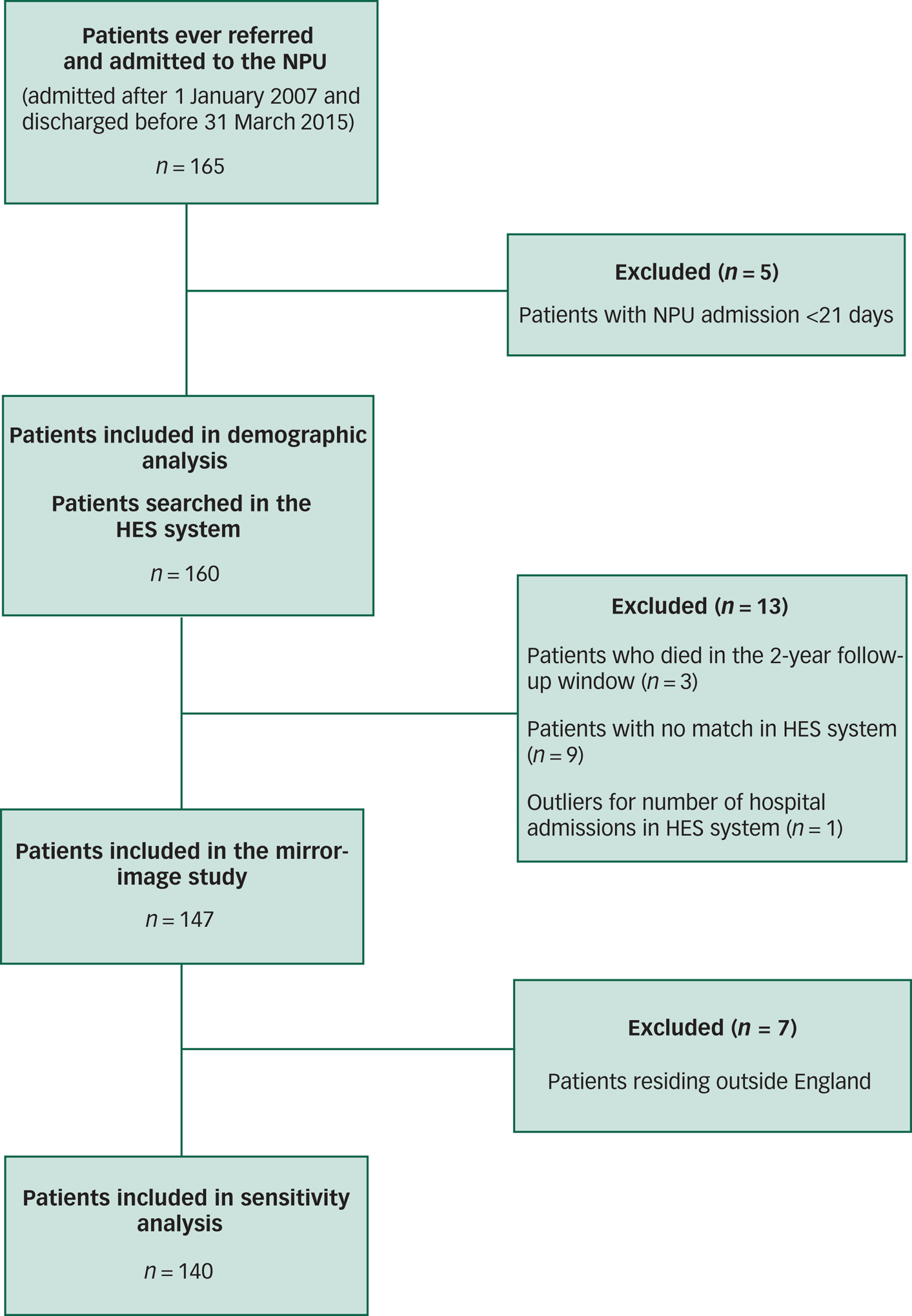
Fig. 1 Cohort selection.
Statistical analysis
Statistical analysis was carried out using Stata version 15. Number of admissions to general and psychiatric hospitals, presentation to A&E, general, psychiatric and total in-patient days, and placements before and after treatment at the NPU were compared within patients between the mirror-image periods using a Wilcoxon signed-rank test, as the data were not normally distributed. Sensitivity analysis included only patients living in England. Within-subject comparisons of number of psychotropic medications and percentages of BNF maximum antipsychotic dose at admission and discharge were conducted using paired t-tests. Clozapine medication at admission and discharge from NPU was compared using χ2-test. Comparison between acuity of placement before and after the treatment at the NPU was carried out using Wilcoxon-signed rank test.
Finally, we performed multiple linear regressions with the change in psychiatric, general and total in-patient days before and after the mirror points as the dependent variables, and the following covariates: age at admission, gender, duration of psychotic illness, length of admission and initiation of clozapine during admission.
Ethical approval
Overarching ethical approval for the use of CRIS as a research data-set was given by Oxfordshire Research Ethics Committee C (08/H0606/71), with individual projects approved by a patient-led oversight committee. This study was approved by the CRIS oversight committee (reference number 18-105). Informed consent was not required as CRIS is an anonymised case register.
Results
Study population
Table 1 summarises patient characteristics for the 160 admissions included in the demographic analysis.
Table 1 Characteristics of patients admitted to the NPU
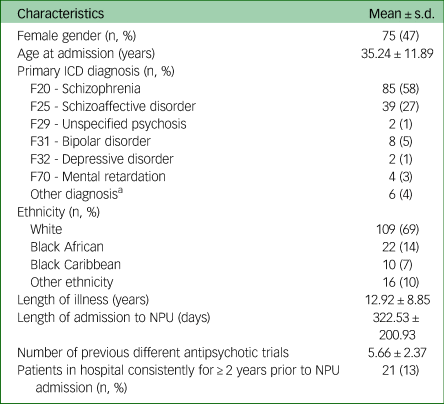
a. Other diagnoses include: autism spectrum disorder, emotionally unstable personality disorder, organic psychosis, delusional disorder, dissociative disorder, substance-induced psychosis.
Hospital admissions and length of stay
Patients had significantly fewer mental health admissions (1.65 ± 1.44 v. 0.87 ± 0.99, z = 5.594, P < 0.0001) and shorter total length of stay (335.31 ± 272.67 v. 199.42 ± 261.96, z = 5.195, P < 0.0001) in the 2 year period after treatment at the NPU, compared with the 2 years before admission. Similarly, total days of physical health admissions was significantly reduced (16.51 ± 85.77 v. 2.83 ± 17.38, z = 2.046, P = 0.0408) (Fig. 2). There was also a reduction in the number of physical health admissions (0.59 ± 2.03 v. .31 ± 1.07), although this was of borderline statistical significance (z = 1.959, P = 0.0501), while the reduction in A&E presentations (2.09 ± 7.54 v. 1.83 ± 7.00) was not statistically significant (z = −0.374, P = 0.7081). Total number of in-patient days was significantly reduced after the admission compared with before (351.82 ± 269.09 v. 202.25 ± 261.05, z = 5.621, P < 0.0001). Results for all the variables investigated were robust to the sensitivity analyses. Table 2 summarises the outcome measures considered in the study.
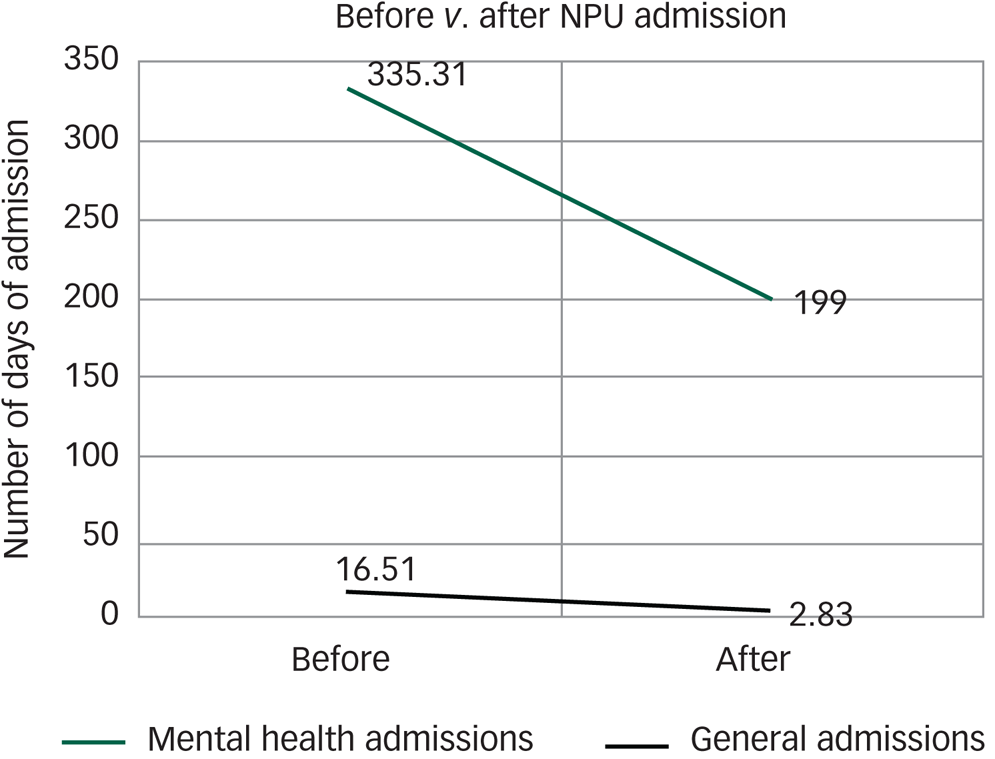
Fig. 2 Mean days of admission to mental health and general hospitals in the 2 years before versus 2 years after the NPU admission.
Table 2 Outcome measures of admissions to the NPU
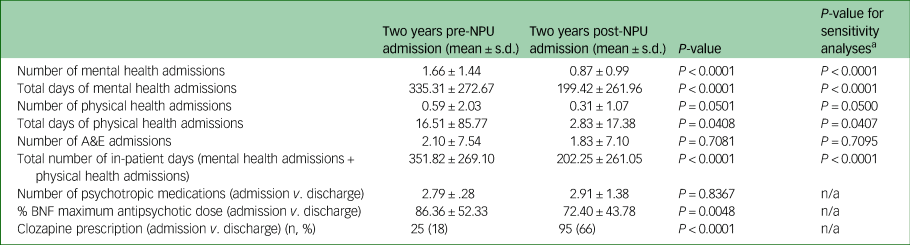
a. Sensitivity analyses conducted in patients residing in England (n = 140).
Polypharmacy and antipsychotic dosage
No statistical difference was found in the numbers of psychotropic medications prescribed at admission and discharge (2.79 ± 1.28 v. 2.91 ± 1.38, t = −0.9846, P = 0.8367). The percentage of BNF maximum antipsychotic dose was significantly higher at admission to the NPU compared with at discharge (87.25 ± 52.21 v. 73.52 ± 44.16, t = 2.6289, P = 0.0048). A higher proportion of patients were taking clozapine at discharge compared with at admission (95 v. 25, Pearson's χ2 = 12.3900, P < 0.0001).
Acuity of placement
Patients’ placements before admission to and after discharge from the NPU were compared. A value from 1 to 6 was assigned to each placement, from the highest (PICU) to the lowest (independent living) intensity. The reduction in level of support before and after treatment at the NPU was statistically significant (z = −8.099, P < 0.0001). Figure 3 shows a mosaic plot of patients’ placements pre- and post-NPU treatment, demonstrating that the majority of patients were admitted from acute in-patient units and most were discharged to rehabilitation units or independent living.
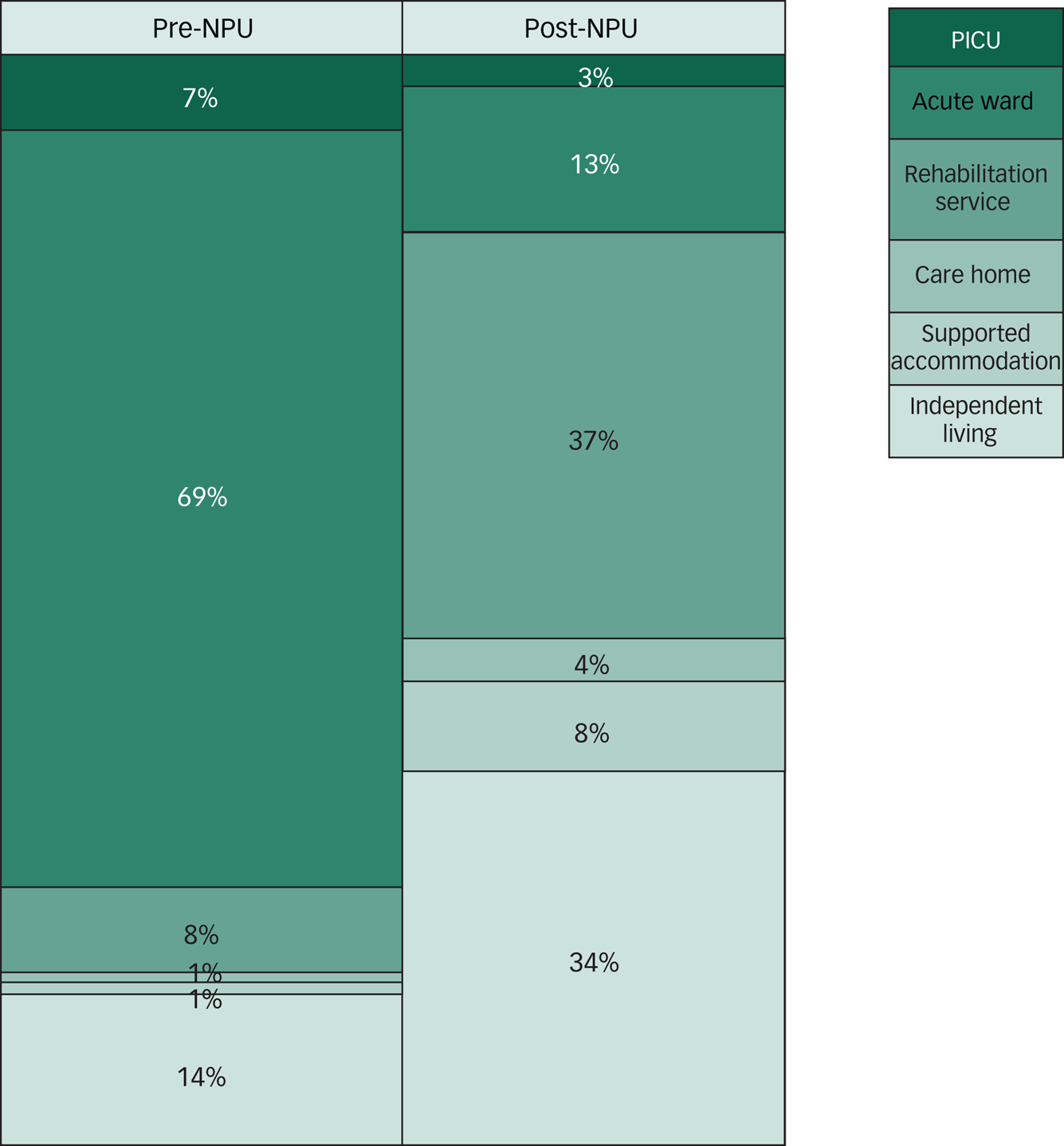
Fig. 3 Mosaic plot of treatments pre- and post-NPU placement.
Predictors of good outcome
In the multiple linear regression, age at admission, gender, ethnicity, duration of psychotic illness, length of admission and introduction of clozapine were not associated with any statistically significant reduction in total in-patient days in psychiatric hospitals (F(5131) = 1.28, P = 0.28, R 2 = 0.05), general hospitals (F(5131) = 1.02, P = 0.41, R 2 = 0.04) or psychiatric and general hospitals combined (F(5131) = 1.52, P = 0.19, R 2 = 0.05).
Discussion
This study aimed to investigate long-term outcomes of treatment at a specialised in-patient facility for adults with a treatment-resistant psychotic disorder. Numbers of psychiatric admissions and psychiatric, general and overall in-patient days were lower in the 2 years following the intervention than in the 2 years prior.
These results are in line with those of previous studies of mental health tertiary services, which have evaluated specialised facilities dedicated to affective disorders.Reference Shepard, Insole, McAllister-Williams and Nicole25–Reference Brodaty, Harris, Wilhelm, Hickie, Boyce and Mitchell27 In fact, disease-specific integrated care models are becoming more common, especially for long-term conditions such as epilepsy; by specialising in a particular clinical area, centres of excellence can develop targeted expertise and have complex diagnostic and therapeutic capabilities which improve the chances of achieving a positive outcome. However, no specific guidelines exist on referring a patient with a treatment-refractory psychotic illness to a tertiary facility, as opposed to other complex chronic conditions such as epilepsy.28 Emerging data from a range of specialised NHS services have demonstrated improvement in patients’ outcomes compared with non-specialist services.Reference Kingsmore, Hole and Gillis29–Reference Bird, Farquhar-Smith, Wigmore, Potter and Gruber31 Such data re-emphasise the need for increased investment in specialist services in the NHS to continue to improve the population's health status and quality of care.Reference Majeed, Allwood, Foley and Bindman32
A significant overall reduction in the acuity of the care setting following discharge was demonstrated. Most of the patients referred to the NPU came from either PICUs or acute wards (76%), whereas only 16% of the patients were discharged to such environments, with 37% moving on to rehabilitation services and 34% to independent accommodation in the community. Not only does this reflect a substantial improvement in patients’ disability, it also corresponds to a significant cost reduction for health and social care systems, which is likely to be sustained well beyond the 2 years of follow-up demonstrated in this study, as 13% of people admitted to NPU had been in-patients consistently for at least 2 years before admission. Of note, the discharge of some of the patients to local acute wards might have been due to failure to find a placement best suited to their needs rather than the necessity of such a high level of support.
It is notable that these improvements in function were achieved despite a statistically significant reduction in total antipsychotic dose. Clozapine was introduced in most patients admitted to the NPU, as it is the gold standard treatment for TRS. This reflects the fact that many patients are referred to the NPU specifically for clozapine treatment, when this has been difficult to achieve in the acute setting, or when clozapine has been discontinued owing to significant concerns about physical health and a safe re-challenge of clozapine is sought. Our previous short-term outcome studies also reported a rationalisation of antipsychotic medication and increase in the use of clozapine from admission to discharge.Reference Perera, Broadbent, Callard, Chang, Downs and Dutta21,Reference Krivoy, Joyce, Tracy, Gaughran, MacCabe and Lally22,Reference Tracy, Joyce, Sarkar, Fernandez and Shergill33 Evidence suggests a response rate of up to 75% to clozapine in those who have failed to respond to previous antipsychotic trials.Reference Agid, Arenovich, Sajeev, Zipursky, Kapur and Foussias34 Furthermore, many patients with a diagnosis of a treatment-resistant psychotic disorder might decline oral medications owing to their delusional beliefs and lack of insight into their illness.Reference Daod, Krivoy, Shoval, Zubedat, Lally and Vadas35 The present study suggests that the level of support and expertise a tertiary service can provide allows patients to access clozapine where this had not proved possible in the local setting.
As mentioned above, patients are referred to the NPU from all over the UK. Consistently, our sample provides a good representation of patients with TRS in the UK, as demonstrated by the proportion of patients of Black African and Caribbean ethnicity, who represent approximately 3% of the UK population36 and have a 5.8-fold increase in risk of schizophrenia compared with the White population.Reference Fearon, Kirkbride and Morgan37 This reflects the nature of a national service which is open to referrals for anyone in the country who needs specialised care. Nonetheless, it does not reflect the reported disparity of involuntary psychiatric care in Black ethnic groups compared with White British patients.Reference Barnett, Mackay, Matthews, Gate, Greenwood and Ariyo38,39 This might be owing to less inequality in tertiary referrals compared with compulsory in-patient psychiatric care, or it might reflect potential biases in the referral processes such that members of Black ethnic groups are less likely to be referred to specialised care than their White peers.
Limitations
A benefit of this study is the fact that informed consent was not required as the data were retrieved from pseudonymised databases. This eliminated the selection bias in favour of higher-functioning patients that often taints research on treatment-resistant psychosis. That said, this study was not without its limitations.
One potential limitation was that we had limited clinical information about the patients before admission and after discharge from the NPU, as their care was usually given by different healthcare providers. Instead, we considered hospital admission as a marker of the overall mental health of the patients. It may be argued that the change in services during the timeframe covered by our study could have influenced our results. Although this should be highlighted as a limitation, there were no major changes to TRS-focused service provision in SLaM in the timeframe considered.
The mirror-image design allowed for a within-patient analysis, minimising the selection bias that may complicate comparisons between groups in naturalistic research. Nonetheless, the lack of a comparator group is a potential disadvantage, and our results may reflect background variations occurring irrespective of the treatment received.
To obtain information about admissions, we used the HES database, which contains data on admissions within the NHS, including private patients treated in NHS hospitals, and care delivered by treatment centres (including those in the independent sector) funded by the NHS in England. Owing to administrative differences, admissions in Scotland, Wales, Northern Ireland and other areas of the British Isles are not recorded. Reassuringly, when sensitivity analyses were conducted including only patients residing in England (n = 140), no difference in significance was found for any of the variables considered.
Owing to the nature of this study, we could not focus on the patients’ perspective or whether there was a specific component or components that yielded the positive outcome. However, there are some preliminary data which illustrate the aspects that families have found helpful during NPU admission.Reference Onwumere, Jansen and Kuipers40
Conclusions
Our study demonstrates the long-term effectiveness of a tertiary service specialising in treatment-resistant psychotic disorders. This supports the existing literature on the need for and importance of specialist care for complex cases of severe mental illnesses.
Acknowledgement
The publication of this paper is supported by a grant from The Royal College of Psychiatrists Academic Freedom Fund established by Kenneth R. Kaufman, MD FRCPsych. For further details about the fund please visit: https://www.cambridge.org/core/journals/bjpsych-open/information/instructions-contributors.
Author contributions
C.C. and J.H.M. contributed to the conception and design of the study. C.C., E.O. and M.P. collected and analysed the data. F.G., E.W., S.S.S. and J.O. took part in the interpretation of the data; and all authors contributed to the drafting and revision of the manuscript.
Funding
This paper describes independent research funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at SLaM and King's College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjo.2020.51.









eLetters
No eLetters have been published for this article.