The burden of mental disorders continues to grow, with significant health, social, human rights and economic effects worldwide, and many health systems have not yet adequately responded, especially in low- and middle-income countries (LMICs). As a consequence, the gap between the need for mental health treatment and its provision is wide: in LMICs, between 76 and 85% of people with mental disorders receive no treatment,Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges and Bromet1 and common mental disorders (CMDs) like depression and anxiety disorders have a particularly high prevalence in these settings. The estimated proportion of anxiety disorders in the global population is 3.6%, and depressive disorders is 4.4%; the estimated prevalence of depressive disorders has increased by 18% between 2005 and 2015.Reference Daar, Jacobs, Wall, Groenewald, Eaton and Patel2,3 These disorders have negative social, economic and physical health effects.
Prevalence of mental health disorders in primary care
Mental disorders can be identified and managed through primary care without the involvement of specialists.Reference de Jesus Mari, Tófoli and Noto4 Integrating mental health into primary care as a global policy initiative is a relatively new phenomenon, even in high-income countries.Reference Druss and Goldman5 As such, prevalence estimates for mental disorders in primary care settings vary widely, although the World Health Organization estimates that 20% of patients in primary care have at least one mental disorder.6 A 2019 Sri Lankan study found that 58.5% of primary care attendees had any mental health disorder, 46.7% had anxiety and 41.6% had depression.Reference Doherty, Hulland, Lopes-Cardozo, Kirupakaran, Surenthirakumaran and Cookson7 A 2017 study of primary care patients in Brazil, China, Mexico and Pakistan found depression in 5.1%, 7.6%, 7.1% and 10.5% of patients, respectively; and anxiety in 26.5%, 18.9%, 23.0% and 13.0% of patients, respectively.Reference Goldberg, Reed, Robles, Minhas, Razzaque and Firtes8 A 2008 study in India found a 15.4% prevalence of CMDs, with a 5% prevalence of depression and a 2.5% prevalence of anxiety.Reference Patel, Araya, Chowdhary, King, Kirkwood and Nayak9 A 2018 study in Ethiopia, India, Nepal, South Africa and Uganda found depression in 15.5%, 20.1%, 14.9%, 8.1% and 4.2% of primary care patients, respectively; and alcohol dependence in 3.6%, 0.4%, 2.6%, 1.6% and 0.1% of patients, respectively.Reference Rathod, Roberts, Medhin, Murhar, Samudre and Luitel10 A paucity of information is available regarding the prevalence of substance use and post-traumatic stress in primary care facilities in LMICs.
Mozambique mental health context
Research findings from 2010 and 2014 show that epilepsy and organic disorders make up the vast majority of out-patient mental health visits in Mozambique (78% in 2010 and 55.7% in 2014), followed by schizophrenia (9% in 2010 and 19.3% in 2014); mood disorders (depression) and neurotic disorders (anxiety) only made up of 2% and 6% of 2010 consultations, respectively.Reference Santos, Wainberg, Caldas-de-Almeida, Saraceno and Mari11 Neurotic disorders in this context refer to anxiety and anxiety-like disorders, which are categorised as such in the Mozambican healthcare system. The most common out-patient psychiatric consultations in Mozambique in the 2.5 years between January 2012 and September 2014 were for epilepsy (53%), child mental disorders (15%) and schizophrenia (14%).Reference Wagenaar, Cumbe, Raunig-Berhó, Rao, Kohrt and Stergachis12 In 2019, among all mental health consultations (including in-patient), 55.6% were for epilepsy, 12.9% were for schizophrenia and 12.1% were for mood disorders and neurotic disorders.13 This shows a continuous trend toward treatment mostly focused on severe mental illness rather than CMDs, although the percentage of consultations for CMDs is increasing. A 2015 study in Sofala ProvinceReference Wagenaar, Cumbe, Raunig-Berhó, Rao, Napua and Hughes14 found that men were more likely to present to mental health services for substance misuse (6.4% for men v. 1.9% for women), whereas women were more likely to report for neurotic disorders (12.8% for women v. 5.7% for men). These findings align with trends seen in other LMICs and low-resource settings, in which mental healthcare often disproportionately focuses on severe mental illness like psychosis and epilepsy, rather than on CMDs like anxiety and depression.Reference Kane, Ventevogel, Spiegel, Bass, Ommeren and Tol15
In Mozambique, 91% (1249 out of 1377) of health facilities are primary care facilities, and 153 facilities country-wide provide consultations for mental health services. According to the 2019 Ministry of Health (MoH) Mental Health Annual Report,13 there were 250 000 psychiatric consultations that year in Mozambique; 6% of consultations were for mood disorders (which includes most depressive disorders) and 5% of consultations were for neurotic, stress-related and somatoform disorders (which includes most anxiety disorders). Despite these statistics, the MoH allocated only 1.6% of the total health budget to mental health services in 2016,Reference Wagenaar, Cumbe, Raunig-Berhó, Rao, Kohrt and Stergachis12 citing unestablished country-level prevalence estimates of mental disorders.
Limited research has examined factors associated with variations in mental health diagnostic patterns in primary care in Mozambique. A 2015 Sofala Province study found that urbanicity was associated with type of mental health diagnoses: urban clinics saw higher rates of consultations for substance use, schizophrenia and delusional disorders, and mood disorders, whereas rural clinics saw higher rates of consultations for epileptic disorders.Reference Wagenaar, Cumbe, Raunig-Berhó, Rao, Napua and Hughes14 Primary care facilities also had lower rates of schizophrenia and delusional disorders and higher rates of neurotic conditions than other levels of care. A 1997 study of mental health in primary care in Harare, Zimbabwe, found that CMD diagnosis was associated with female gender and older age, as well as food insecurity, unemployment and stressful life events.Reference Patel, Todd, Winston, Gwanzura, Simunyu and Acuda16
Study objectives
Timely and effective evidence-based interventions play a key role in addressing CMDs. Governments are in a unique position to develop and strengthen surveillance, and provide and disseminate data that can help inform necessary actions to reduce the mental health treatment gap. Good-quality data is needed to determine what is effective, but there is a lack of such evidence, especially at the regional and community level. Currently, mental health data collection in Mozambique is limited to those who present themselves to health facilities for mental health treatment, and no studies have been done regarding the prevalence of mental illness in out-patient consultations at facilities that provide primary care. Determining the prevalence of patients with CMD who seek primary care can establish a foundation for integrating mental health services into primary healthcare. This study assesses the prevalence of mental illness and examined factors associated with CMDs in patients accessing out-patient services in primary care in MoH clinics in Sofala Province, Mozambique.
Method
Structure of the mental health system in Mozambique
In Mozambique, the National Mental Health Program is managed by the Department of Mental Health at the MoH. The community-based programme sees most patients at out-patient health units, which provide primary healthcare close to communities and places of residence. Programme activities occur at the district and provincial levels, and are reported vertically to the central Ministry. The MoH has prioritised its mental health programme since 1996, and has become a leader in mental healthcare in the Southern African region. Since 1996, the programme has focused on training mid-level mental health professionals, called psychiatric technicians. These providers can diagnose and treat major mental illnesses with a focus on psychopharmacology. In 2014, the Mozambican MoH accomplished their goal of placing at least one psychiatric technician at a primary care health facility within each of the 135 districts nationally.Reference Santos, Wainberg, Caldas-de-Almeida, Saraceno and Mari11,Reference Wagenaar, Cumbe, Raunig-Berhó, Rao, Kohrt and Stergachis12 Challenges remain, however, as the majority of psychiatrists are located in the capital of Maputo, and the distribution of psychiatry technicians is also centred on urban areas, leaving many rural areas without access. Mozambique has an estimated population of 30 million,17 with 15 Mozambican psychiatrists (as of 2016)Reference Wagenaar, Cumbe, Raunig-Berhó, Rao, Kohrt and Stergachis12 and 84 beds per 100 000 population available for in-patient mental health services via two psychiatric hospitals, as well as beds in general hospitals.Reference Wagenaar, Cumbe, Raunig-Berhó, Rao, Napua and Hughes14,Reference Dos Santos, Cumbe, Gouveia, Fouchier, Teuwen and Dua18,Reference Halsted, Ásbjörnsdóttir and Wagenaar19. Existing psychosocial support services are primarily focused on patients with HIV.
Study setting and participants
This study was carried out in Sofala Province (Fig. 1), located in central Mozambique with a population of approximately 2.3 million according to the most recent census conducted in 2017. The official language is Portuguese, with Cisena and Cindau languages commonly spoken in rural areas. This province has a literacy rate of 56%, an infant mortality rate of 83 per 1000 live births, a life expectancy of 54 years (51 for men and 57 for women) and an HIV prevalence of 14%.20,Reference Cumbe, Muanido and Manaca21 According to statistical data from the Provincial Health Directorate, there are 166 health facilities in Sofala Province, of which 25 (15 percent) have trained mental health personnel. This team includes three psychiatrists, 29 clinical psychologists, 28 psychiatric technicians and one social worker.22 Beira City is the capital of Sofala Province and the second-largest city in Mozambique, with a population of approximately 500 000. Beira City has 13 primary care health facilities, one quaternary-level central hospital and several private health facilities. Dondo is the closest city to Beira (30 km away), and has 16 primary care health facilities serving a population of 180 000.Reference Instituto Nacional de Estatistica23 In both Dondo and Biera City, general consultations, prenatal consultations and postpartum consultations make up the majority of visits to primary care facilities. This study was conducted in three health facilities: two in Beira City (Macurungo and Chingussura) and one in Dondo (Dondo health facility). We selected these facilities because: they had at least one psychiatric technician and one clinical psychologist; they were health units with a high flow of patients receiving general primary healthcare; they provided comprehensive maternal and child healthcare and they were representative of other urban and peri-urban primary health facilities in Mozambique.

Fig. 1 Political map of Mozambique, including provincial capital cities. Focal area of Beira City and surrounding Dondo highlighted by the box.
Adaptation of the Mini International Neuropsychiatric Interview to the Mozambican context for use as a gold standard
The Mini International Neuropsychiatric Interview version 5.0 (MINI 5.0) is a short diagnostic interview developed for the ICD-10 (psychiatric disorders). Mozambique currently uses the ICD-10 classification system for the diagnosis and treatment of mental disorders. It can be administered in approximately 30–45 min by qualified technicians in the area of mental health.Reference Amorim24 The MINI 5.0 includes a structured psychiatric interview for all CMDs, severe mental disorders, alcohol/drug misuse and suicidal ideation. Our team used the Brazilian Portuguese version of the MINI 5.0 as a starting point for adaptation to the Mozambican context. A group of local Mozambican mental health professionals (two clinical psychologists and three psychiatric technicians) was first recruited to collaboratively adapt the Brazilian MINI 5.0 to the Mozambican linguistic and cultural context, resulting in the MINI 5.0 MZ. The instrument was then coded in REDCap (version 6 for Windows; Vanderbilt University, Nashville, Tennessee, USA; https://www.project-redcap.org) for use on tablets by a local Mozambican study staff member. Following coding, the same group of mental health staff re-reviewed the MINI 5.0 MZ and focused on understanding, ease of use and logical sequence of questions. All mental health professionals in each health facility participating in the study attended a 2-day training on the correct use of the MINI 5.0 MZ, in which participants practiced administering and being screened with the MINI 5.0 MZ, and notes and revisions were made to improve the instrument. Trainings were led by study staff as well as Mozambican mental health professionals who were experts in administration of the instrument. Participants had one-on-one supervision by experts to ensure proper administration of the tool. Next, the MINI 5.0 MZ pilot was carried out, in which the instrument was tested for 4 days among primary care patients attending out-patient consultations at the Macurungo health centre in the city of Beira, under the supervision of study staff and trained experts. Patients who were administered the MINI 5.0 MZ in piloting were asked what they thought was the underlying meaning of each question, whether the question was obscure or inappropriate or difficult to understand and, if so, how they suggested improving each issue. Following cognitive interviews and the pilot implementation, the mental health professionals reviewed the cognitive interview data and engaged in a collaborative process of improving the MINI 5.0 MZ based on this feedback.
Data collection procedures
Data collection took place from October 2018 to February 2019 at three MoH facilities in Sofala Province. Patients were excluded in cases where they had an acute health condition or disability that impeded their ability to complete the survey. Eligible patients were referred to a trained mental health professional (psychologist or psychiatry and mental health technician), who administered the MINI 5.0 MZ, and sociodemographic data were collected by trained data collectors. The MINI 5.0 MZ assessed the presence of MDD symptoms in the previous 2 weeks, GAD symptoms in the previous 2 weeks, PTSD symptoms in the previous month and alcohol and substance use in the previous 12 months. Administrators of the MINI 5.0 MZ were blinded to the responses of the patient on the sociodemographic information. Tablet-based REDCap softwareReference Harris, Taylor, Thielke, Payne, Gonzalez and Conde25,Reference Harris, Taylor, Minor, Elliott, Fernandez and O'Neal26 was used for data collection.
Data analysis procedures
Demographic and clinical characteristics were assessed, including age, gender, marital status, education, the reason for visiting the health facility, monthly income and HIV status. We calculated the prevalence of common mental health disorders by using the sociodemographic information administered by data collectors, with the MINI 5.0 MZ administered by psychiatric technicians and psychologists as the gold standard. Summary statistics for mental disorders were analysed by individual disorders, as well as by using the binary variable of ‘any common mental illness’ versus ‘no common mental illness’. CMDs analysed in the present study included major depressive disorder (MDD), generalised anxiety disorder (GAD), post-traumatic stress disorder (PTSD) and any substance misuse or dependence (including alcohol and/or drug use).
Regression analyses examined unadjusted and adjusted odds ratios for each CMD diagnostic category. Generalised linear mixed models with a binomial distribution were utilised, including a random intercept by health facility to account for clustering. Adjusted analyses were fully adjusted for patient gender, the reason for health facility visit, marital status, education, HIV status and monthly income simultaneously in the statistical model. Stata software (version 16 for Windows) and an alpha value of 0.05 were used for all statistical analyses.
Ethics
All participants provided informed consent for research procedures. The informed consent process included the following procedure. Individuals interested in participation were directed by a research assistant to a private consultation room to administer the consent form. The form was read to the participant by the research assistant and a copy of the form was provided to the participant. Participants were given the opportunity to ask questions and efforts were made to ensure participants fully understood the research procedures. Participants were given the option to sign their name or provide a fingerprint if they could not sign.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human patients were approved by the Mozambican National Committee for Bioethics in Health (CNBS), whose code is IRB00002657, with the approval number 290/CNBS/18. Study procedures were also simultaneously approved by the University of Washington ethics review board.
Results
Sociodemographic and clinical characteristics
Of the 502 patients interviewed, 74.1% were female (n = 372) and the average age was 27.8 years (s.d. = 7.4). Of these, 44.6% were seeking care for a general out-patient consultation (n = 224), 27.5% were seeking care for a prenatal consultation (n = 138) and 27.9% were seeking care for a postpartum consultation (n = 140). Of all participants, 5.8% were officially married (n = 29), 70.7% were in a civil union (n = 355), 20.0% were single (n = 100), 0.8% were divorced (n = 4) and 1.4% were either separated or widowed (n = 7). Of all participants, 0.4% never went to school or formally studied (n = 2), 14.7% had finished some primary school (n = 74), 11.2% finished primary school (n = 56), 31.3% had some high school (n = 157), 27.5% finished high school (n = 138) and 13.0% had education beyond high school (n = 65). The reported family average income was USD 118.5 (s.d. = 147.9), and 58.1% had a monthly income <USD 100 (n = 259). Also, 27.9% reported being HIV positive (n = 140). Table 1 displays all sociodemographic and clinical characteristics.
Table 1 Demographic and clinical characteristics by common mental disorders of 502 patients

CMD, common mental disorder (to include MDD, GAD, PTSD and substance misuse/dependence); MDD+, positive for current (past 2 weeks) major depressive disorder; GAD+, positive for current (past 2 weeks) generalised anxiety disorder; PTSD+, positive for current (past month) post-traumatic stress disorder; any substance misuse/dependence, positive for any alcohol or drug misuse or dependence in past 12 months.
a. Converted to USD with the exchange rate of 60 MZN to 1 USD.
CMD prevalence in primary care
Of all participants, 23.9% (n = 120) screened positive for at least one or more CMDs. Specifically, 8.6% screened positive for MDD (positive for current (past 2 weeks) MDD; n = 43), 13.3% screened positive for GAD (positive for current (past 2 weeks) GAD; n = 67), 4.8% screened positive for PTSD (positive for current (past month) PTSD; n = 24) and 4.0% screened positive for any substance misuse or dependence (positive for substance misuse or dependence (past 12 months); n = 20). A full breakdown of CMD prevalence by demographic and clinical characteristics can be found in Table 1.
Factors associated with any CMD in primary care
In fully adjusted analyses, patients attending postpartum consultations had 58% decreased odds of any CMD compared with those attending out-patient primary care (adjusted odds ratio (aOR) 0.42, 95% CI 0.18–0.98). Those having never tested for HIV also had lower odds of any CMD compared with those who tested HIV negative (aOR = 0.46, 95% CI 0.34–0.63). In unadjusted analyses, females were 52% less likely to have any mental disorder compared with males (odds ratio 0.48, 95% CI 0.23–0.99); however, once adjustment was made this association was no longer significant (aOR = 0.65, 95% CI 0.33–1.3). Additionally, unadjusted regression results showed that those patients who were single (odds ratio 1.38, 95% CI 1.24–1.54) or divorced, separated or widowed (odds ratio 4.67, 95% CI 1.5–14.2) had an elevated risk of any CMD, compared with those in a civil union. However, these associations were not statistically significant in fully adjusted models. Full regression results for factors associated with any CMD are in Table 2.
Table 2 Regression analyses of adjusted and fully adjusted models for any common mental disorder in primary care in Sofala, Mozambique (N = 502)

CMD, common mental disorder (to include major depressive disorder, generalised anxiety disorder; post-traumatic stress disorder and any substance misuse/dependence).
a. Converted to USD with the exchange rate of 60 MZN to 1 USD.
* P < 0.05; **P < 0.01.
Factors associated with MDD in primary care
In fully adjusted analyses, each 10-year increase in patient age was associated with 44% decreased odds of MDD (aOR = 0.56, 95% CI 0.54–0.59) among all primary care patients. Patients seeking care for postpartum consultations (aOR = 0.26, 95% CI 0.09–0.77) and prenatal consultations (aOR = 0.35, 95% CI 0.22–0.55) also had significantly lower odds of MDD compared with those attending out-patient primary care visits. Individuals who were married (aOR = 2.48, 95% CI 1.30–4.74) or divorced, separated or widowed (aOR = 2.97, 95% CI 1.01–8.75) had significantly higher odds of MDD compared with those in a civil union. In unadjusted analyses, those with no school or some primary school had elevated odds of MDD (odds ratio 1.85, 95% CI 1.12–3.0) compared with those with some high school, although this was not significant in fully adjusted analyses. Full regression results for factors associated with MDD are shown in Table 3.
Table 3 Regression analyses of adjusted and fully adjusted models for major depressive disorder in primary care in Sofala, Mozambique (N = 502)

MDD+, positive for current (past 2 weeks) major depressive disorder.
a. Converted to USD with the exchange rate of 60 MZN to 1 USD.
* P < 0.05; **P < 0.01.
Factors associated with GAD in primary care
In unadjusted analysis, the odds of a diagnosis of GAD was associated with being single (aOR = 1.66, 95% CI 1.46–1.90, P < 0.01) compared with those in a civil union; and finishing primary school was associated with decreased odds of a GAD diagnosis (aOR = 0.58, 95% CI 0.47–0.72, P < 0.01) compared with those with some high school education. After adjusting for covariates, these associations remained significant, and never having been tested for HIV became significant (aOR = 0.20, 95% CI 0.08–0.53, P < 0.01). Full regression results for factors associated with GAD are shown in Table 4.
Table 4 Regression analyses of adjusted and fully adjusted models for generalised anxiety disorder in primary care in Sofala, Mozambique (N = 502)

GAD+, positive for current (past 2 weeks) generalised anxiety disorder.
a. Converted to USD with the exchange rate of 60 MZN to 1 USD.
* P < 0.05; **P < 0.01.
Factors associated with PTSD in primary care
In unadjusted analysis, a diagnosis of PTSD was associated with the marital status of single (odds ratio 2.7, 95% CI 1.48–5.0, P < 0.01) and divorced/separated/widowed (odds ratio 12.0, 95% CI 2.8–51.7, P < 0.01) compared with those in a civil union, as well as having a postgraduate education (odds ratio 1.08, 95% CI 1.00–1.16, P < 0.05) compared with those with some high school education, and being female was associated a decreased association with PTSD (odds ratio 0.46, 95% CI 0.30–0.71, P < 0.01) compared with being male. None of these variables remained significant after adjusting for covariates. Full regression results for factors associated with PTSD are shown in Table 5.
Table 5 Regression analyses of adjusted and fully adjusted models for post-traumatic stress disorder in primary care in Sofala, Mozambique (N = 502)
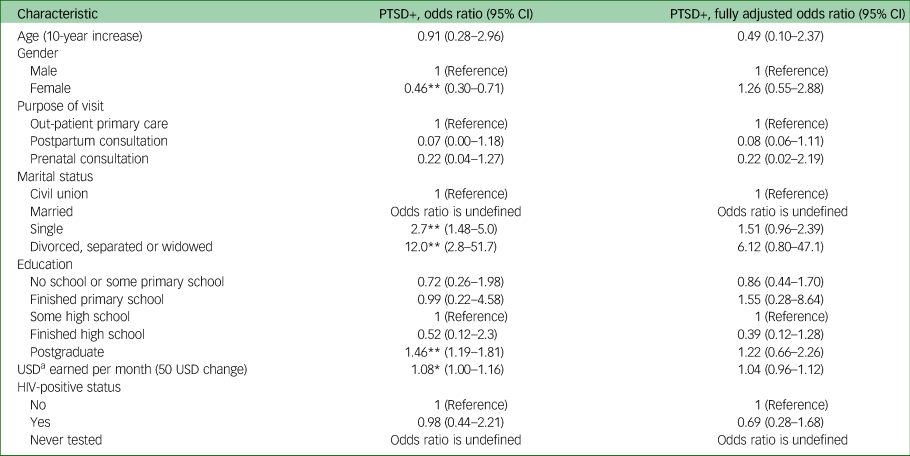
PTSD+, positive for current (past month) post-traumatic stress disorder.
a. Converted to USD with the exchange rate of 60 MZN to 1 USD.
* P < 0.05; **P < 0.01.
Factors associated with any substance misuse or dependence in primary care
Unadjusted analysis found increased odds of substance misuse/dependence associated with being divorced/separated/widowed (odds ratio 6.25, 95% CI 2.8–13.9, P < 0.01) compared with those in a civil union, female gender (odds ratio 0.05, 95% CI 0.03–0.09, P < 0.01) compared with male, and never having been tested for HIV (odds ratio 4.7, 95% CI 1.7–12.9, P < 0.01) compared with those who reported HIV negative serostatus. Adjusted analysis found increased odds of substance misuse/dependence diagnosis were associated with every 10-year increase in age (aOR = 1.44, 95% CI 1.20–1.73, P < 0.01), and decreased odds were associated with female gender (aOR = 0.16, 95% CI 0.06–0.43, P < 0.01) compared with male, being single (aOR = 0.79, 95% CI 0.69–0.90, P < 0.01) compared with in a civil union, and reporting HIV positive serostatus (aOR = 0.17, 95% CI 0.36–0.50, P < 0.01) compared with negative. Female gender was the only factor showing significant association in both unadjusted and adjusted analysis. Full regression results for factors associated with any substance use or alcohol dependence are shown in Table 6.
Table 6 Regression analyses of adjusted and fully adjusted models for alcohol or drug misuse or dependence in primary care in Sofala, Mozambique (N = 502)

Any substance misuse/dependence, positive for any alcohol or drug misuse or dependence in the past 12 months.
a. Converted to USD with the exchange rate of 60 MZN to 1 USD.
* P < 0.05; **P < 0.01.
Discussion
In this study, we examined the prevalence and associated factors of CMDs in primary healthcare (out-patient, postpartum and prenatal care) at three large MoH facilities in Sofala Province, Mozambique. We found an overall prevalence of 24% for any CMD among 502 patients interviewed. The most commonly diagnosed disorder was generalised anxiety (13.3%), followed by major depression (8.6%), post-traumatic stress (4.8%) and any substance misuse and/or dependence (4.0%).
The estimated prevalence of CMDs in primary care varies widely. A 1995 study conducted across 15 World Health Organization sites found that approximately 21% of all patients seen by primary healthcare professionals have one or more of either generalised anxiety, depression or alcohol dependence, and that these estimates are similar in LMICs and high-income countries.6 Although data did not assess PTSD or other substance use, they are similar to the findings in our study, in which 24% of those visiting health facilities for primary care had at least one CMD. Conversely, our estimate is somewhat higher than the 15.4% estimated prevalence of CMDs in primary care in India.Reference Patel, Araya, Chowdhary, King, Kirkwood and Nayak9 Our estimated 8.6% prevalence for depression is higher than estimates in Brazil, China, Mexico, Uganda and South Africa (5.1%, 7.6%, 7.1%, 4.2% and 8.1%, respectively), but lower than estimates in Pakistan, Ethiopia, India and Nepal (10.5%, 11.5%, 20.1% and 14.9%, respectively).Reference Goldberg, Reed, Robles, Minhas, Razzaque and Firtes8,Reference Rathod, Roberts, Medhin, Murhar, Samudre and Luitel10 Conversely, our 13.3% prevalence estimate for anxiety is lower than Brazil, China and Mexico (26.5%, 18.9% and 23.0%, respectively), and the same as Pakistan (13.0%).Reference Goldberg, Reed, Robles, Minhas, Razzaque and Firtes8 Although the methods of measuring and classifying these prevalence estimates are slightly different in the various studies (ICD-10 codes versus CMD screening tools), they remain important for policy prioritisation and funding allocation.
We found that patients visiting primary care for general consultations and those who reported being HIV negative had two-fold increased odds of any mental disorder compared with postpartum consultations (aOR = 0.42) and those who had never been tested for HIV (aOR = 0.46). Our study did not find any association change in age, which differs from previous research in primary care settings in LMICs that found CMD diagnosis to be associated with older age,Reference Patel, Todd, Winston, Gwanzura, Simunyu and Acuda16,Reference Stordal, Mykletun and Dahl27,28 although these associations have been poorly studied in primary care settings in LMICs.
Our results showed that a 10-year increase in age was associated with two-fold decreased odds of MDD diagnosis (aOR = 0.56), and that general out-patient clinic consultations were associated with three- and four-fold increased odds of MDD compared with prenatal (aOR = 0.35) and postpartum (aOR = 0.26) consultations, respectively, which suggests the advantage of a particular focus on screening in general out-patient consultations. We also found that a marital status of civil union was associated with an almost three-fold decreased odds of MDD compared with divorced/separated/widowed (aOR = 2.97), and was associated with an almost 2.5-fold decrease in odds of MDD compared with married status (aOR = 2.48). This is consistent with research in LMIC primary care settings that found associations between marital status of divorced/widowed/separated and the presence of depression.Reference Kaur, Tee, Ariaratnam, Krishnapillai and China29 Studies suggest that the prevalence of depression is higher in primary care settings than in the community, as patients with depression tend to be more frequent users of medical services,Reference Katon and Schulberg30 so implementing depression screening into primary care (and especially in general out-patient consultations) represents one method of expanding the reach of mental healthcare and reducing the treatment gap.
Having a marital status of civil union was associated with a >1.5-fold decreased odds of GAD compared with being single (aOR = 1.66), and having finished some high school education was associated with a >1.5-fold increased odds of GAD compared with having finished primary school (aOR = 0.58). We also found that those reporting HIV negative serostatus had five-fold increased odds of GAD compared with those who had never been tested (aOR = 0.20). Although less research has examined the factors associated with GAD in LMIC primary care settings, its frequent co-occurrence with depression and association with high utilisation of primary care medical servicesReference Ford, Trestman, Steinberg, Tennen and Allen31 further suggest that implementing screening in primary care settings is an opportunity to expand coverage and provide patients with comprehensive treatment.
We found that men had a more than six-fold increased odds of substance use and dependence compared with women (aOR = 0.16), which is corroborated by previous research that found that men present a burden of disorders related to the consumption of alcohol and drugs almost six times greater than women.Reference Pires, Belo, Anube, Santos, Arroz and Pereira32–34 We also found that HIV-positive serostatus was associated with an almost six-fold increased odds of substance misuse and dependence compared with those who reported being HIV negative (aOR = 0.17). HIV-positive status has a well-established association with substance use and dependence, both insideReference Mimiaga, Reisner, Grasso, Crane, Safren and Kitahata35 and outsideReference Chander, Himelhoch and Moore36 of primary care settings, and integrated primary care models have sought to address this frequent co-occurrence.Reference Soto, Bell and Pillen37 Decisions about resource allotment in Mozambique could take into account these associations.
Mental health research in Mozambique is still emerging from a nascent mental healthcare system. The mental health treatment gap is exacerbated by the scarcity of resources (professionals, medicines, infrastructure), as well as stigma regarding mental illness.Reference Zhang, Augusto, Ásbjörnsdóttir, Akullian, Cumbe and Rao38–Reference Patel, Simbine, Soares, Weiss and Wheeler40 Many Mozambicans attribute mental disorders to supernatural causes, and in about three-quarters of all cases, consult a traditional healer.34 Nearly half of the people with these disorders in rural areas were reported as being in poor health.Reference Patel, Simbine, Soares, Weiss and Wheeler40 Although the formalised mental health system in Mozambique is still growing and is not equitably available across the country, primary healthcare facilities provide an opportunity to substantially expand the reach of mental healthcare with integrated services. Along with the MINI 5.0 MZ, other work has been done to adapt and validate mental health screening toolsReference Cumbe, Muanido and Manaca21 that could be used in primary care settings.
Our study provides important prevalence estimates of mental disorders among patients who access primary care health facilities for general out-patient services. The lack of research in mental health limits the planning and quality of assistance in the National Health System in Mozambique. This improved context can inform the government and other stakeholders in designing effective strategies for mental health service implementation and resource allocation.
Limitations
Our study had several limitations. First, our sample only included patients at three high-volume urban health facilities, so there may be limited generalisability to other areas of Mozambique and other facility types. Similarly, because we measured the prevalence in patients in out-patient consultations, our data do not capture the burden of CMDs among people who do not visit a health facility, and therefore is not generalisable as community prevalence. Second, the MINI 5.0 tool used as a gold-standard diagnostic interview in this study has not been validated for use specifically in Mozambique. Although we employed a systematic and rigorous adaptation process, the lack of validation means there may yet be undiscovered issues that would interfere with its effectiveness as a gold standard. Third, our sampling procedure was to interview willing participants in waiting rooms, and was therefore a convenience sample rather than a full random sample, which could have introduced bias.
Strengths
Our study had several strengths. First, our sample size of 502 patients was relatively large for a study looking to assess prevalence of CMDs in primary care. Second, as the majority of primary care facilities in Mozambique are run by the MOH, the study facilities from which we derived our sample are largely representative of other clinics in Mozambique. Third, we utilised trained mental health clinical staff for our diagnostic interviews rather than, for instance, research assistants with no experience in mental health clinical settings. Fourth, we evaluated prevalence across multiple primary care service settings (out-patient primary care generally, prenatal care, postpartum care). Fifth, we employed a rigorous process of professional collaboration to culturally adapt the MINI 5.0 for use as our diagnostic instrument.
In conclusion, the prevalence of CMDs in primary care in Mozambique is high (over 20%), and appears to be particularly high in general out-patient care compared with prenatal and postpartum consultations. The current standard of care in out-patient care settings in Mozambique does not include screening for CMDs. There is an urgent need to implement the integration of CMD screening and treatment into primary care. A specific focus on patients attending general out-patient visits, young people for depression, and people living with HIV and men for substance misuse/dependence would provide a targeted response to high-risk demographics.
Data availability
The data-sets used and/or analysed during the current study are available from Comité para Saúde de Moçambique (formerly Health Alliance International, Mozambique) under reasonable request addressed to the corresponding author, A.M.
Author contributions
B.H.W. and V.C. conceived the idea and led the organisation of the study and data collection. A.M. supervised data collection in health facilities, with input from N.M., B.H.W., V.C. and L.H. All authors contributed to writing the paper and provided critique and scientific input. A.M. led the analyses, with input from B.H.W. and K.E.F. A.M. wrote the first version of the paper, with support from K.E.F., B.H.W. and all other authors. All authors have read and approved the final version of this manuscript.
Funding
This work was supported by grant number K01MH110599 from the National Institute of Mental Health. The content of this paper is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Declaration of interest
None.











eLetters
No eLetters have been published for this article.