Anorexia nervosa (AN) is a severe psychiatric illness usually beginning in adolescence with a lifetime prevalence among 1 to 4% of females in Europe.Reference Smink, van Hoeken and Hoek 1 , Reference Keski-Rahkonen and Mustelin 2 Intense fear of weight gain, body image disturbance and disturbed cognitive and emotional functioning are central features of the disorder. These features lead to weight loss behaviours such as dietary restriction, purging or excessive physical activity.Reference Zipfel, Giel, Bulik, Hay and Schmidt 3 Acute and chronic effects of starvation complicate treatment of people with AN, and the standardised mortality ratio is around 5.5.Reference Arcelus, Mitchell, Wales and Nielsen 4 , Reference Fichter and Quadflieg 5 In older adolescents and adults, AN commonly has a relapsing or protracted course,Reference Herzog, Deter, Fiehn and Petzold 6 and only 50% of the adults recover completely.Reference Keel and Brown 7 Psychiatric comorbidity is the rule with mood disorders (nearly 75% of people with AN) and a range of anxiety disorders (between 25 and 75%) being most common.Reference Fernandez-Aranda, Pinheiro, Tozzi, La Via, Thornton and Plotnicov 8 , Reference Raney, Thornton, Berrettini, Brandt, Crawford and Fichter 9 Mean duration of illness is nearly 7 years,Reference Herzog, Deter, Fiehn and Petzold 6 , Reference Strober, Freeman and Morrell 10 and as this disorder usually starts in adolescence, transition to adult life is fraught with difficulties finishing education, starting a job or engaging in relationships.
Patients are typically reluctant to engage in treatment, especially when it has a clear focus on weight gain, and this tendency to avoid treatment is reflected in the finding that only a minority is treated within the mental healthcare system.Reference Hoek 11 , Reference Keski-Rahkonen, Hoek, Susser, Linna, Sihvola and Raevuori 12 Where onset of the disorder is triggered by genetic, psychosocial and interpersonal factors, changes in neural networks sustain the illness. Altered reward processing to modulate emotional distress,Reference Kaye, Wierenga, Bailer, Simmons and Bischoff-Grethe 13 , Reference Steinglass and Walsh 14 increased compulsivity because of being severely underweightReference Walsh 15 and neuropsychological difficultiesReference Lopez, Tchanturia, Stahl and Treasure 16 – Reference Chan, Ahn, Bates, Busemeyer, Guillaume and Redgrave 21 might lead to the typical persistence of people with AN in their self-destructive behaviour. Final factors of importance are the altered values towards life and death in people who are currently ill with AN as opposed to recovered people with AN and the sense that the AN is part of the personal identity instead of an acquired illness.Reference Tan, Hope and Stewart 22 , Reference Treasure and Schmidt 23
These findings together with the obvious severity of the disorder lead to doubts regarding decision-making abilities or, in other words, mental capacity to consent to treatment. These are relevant doubts, as only a person with full mental capacity with regard to the medical issue at hand can refuse or consent to necessary treatment according to most international health legislations. Assessment of mental capacity generally considers four abilities:Reference Grisso and Appelbaum 24 the ability to understand information provided regarding illness and treatment; the ability to appreciate this information as relevant to one's own situation; the ability to reason with this information, weighing the consequence of decisions; and the ability to express a choice about treatment. A semi-structured interview has been developed to aid clinicians in the assessment of mental capacity to consent to treatment judging these four abilities (MacCAT-TReference Grisso, Appelbaum and Hill-Fotouhi 25 ). Although in general psychiatry a number of studies have been done (for a review see Okai et al Reference Okai, Owen, McGuire, Singh, Churchill and Hotopf 26 ), in AN studies have been scarce. Two small studies have been done in adolescents, with inconsistent results.Reference Tan, Hope and Stewart 27 , Reference Turrell, Peterson-Badali and Katzman 28 In the study by Tan et al, mental capacity of people with AN was excellent, whereas in the study by Turrell et al impairments in reasoning were shown.
It is tempting to assume that the presence of diminished mental capacity to consent to treatment is relevant to treatment outcome, but this has not yet been studied. Therefore, a longitudinal study was conducted in our treatment centre. Baseline results from this sample of 70 adult people who are severely ill with AN were reported on previously.Reference Elzakkers, Danner, Hoek and van Elburg 29 One-third of participants had diminished mental capacity at baseline (as assessed by psychiatrists). Diminished mental capacity was associated with a lower body mass index (BMI), more previous treatment for AN and a lower appreciation of disorder and treatment; duration of illness did not differ between the groups.
Although BMI was significantly different between the two mental capacity groups, still 43% of participants with a BMI below 15 kg/mReference Keski-Rahkonen and Mustelin 2 was judged to have full mental capacity, highlighting the importance of looking further than BMI alone in the assessment of mental capacity to consent to treatment in AN. The picture that emerged from these baseline data was that a significant group of participants had diminished mental capacity and that not only BMI was of importance (as yet not clear in what way) but also the ability to use one's emotions to come to adaptive decision-making. What also became clear was that almost all participants (92%) did follow the treatment advice (whether this was in-patient or out-patient treatment), suggesting that agreement with the treatment advice does not necessarily mean possessing full mental capacity.
More insight in possible differences between the two mental capacity groups in the course of the disorder is relevant to clinical practice as treatment may need to be tailored more to specific needs of the group with diminished mental capacity. The initial group of 70 participants was divided into two groups on the basis of clinical judgment, one with diminished mental capacity and one with full mental capacity to consent to treatment. In this longitudinal part of the study, we aim to answer the following questions:
-
(1) Is the course of disorder different between the two mental capacity groups on clinical variables (BMI, percentage of in-patient treatment, duration of in-patient stay, remission rate and eating disorder pathology)?
-
(2) Is the course of disorder different on psychological variables (symptoms of depression, anxiety and alexithymia)?
-
(3) Is the course of disorder different on decision-making (appreciation of illness and treatment and more general assessment of decision-making ability)?
Method
The study design has been described in detail elsewhere.Reference Elzakkers, Danner, Hoek and van Elburg 29 A longitudinal cohort study was conducted in our national specialist centre for the treatment of eating disorders and at baseline 70 consecutively referred female adults with AN were included. Males (5% of referrals) were excluded to increase homogeneity of the sample. Treatment offered in our centre follows guidelines for eating disorders and entails a range of individual and group therapies, psychomotor therapy and attention to rehabilitation on an out-patient, day patient or in-patient basis. For a description of baseline characteristics, see Table 1. The study was conducted in accordance with the ethical standards described by the Medical Research Involving Human Subjects Act (WMO) and was approved by the institutional review board. After complete description of the study to the participants, written informed consent was obtained. One and 2 years after inclusion, participants were contacted by phone and asked for their cooperation with the follow-up measurements. Some of the required data were collected from patient files (e.g. current BMI, medication, days of in-patient treatment), other were collected during assessments by psychiatrists and psychologists (e.g. interviews and the decision-making task). When patients were no longer in treatment at our centre, data on current treatment, BMI and medication were asked from them.
Table 1 Baseline characteristics of participants
| Total group (n=70) | Full MC (n=46) | Diminished MC (n=24) | P | |
|---|---|---|---|---|
| Age, years: mean (s.d.) | 27.3 (9.7) | 26.2 (9.3) | 29.4 (10.3) | 0.19 |
| Age at illness onset (years): mean (s.d.) | 17.8 (4.9) | 17.7 (4.6) | 18.1 (5.7) | 0.82 |
| Duration of illness (years): mean (s.d.) | 8.6 (8.1) | 8.5 (8.2) | 8.9 (7.9) | 0.84 |
| BMI: mean (s.d.) | 15.5 (1.9) | 16.1 (1.6) | 14.2 (1.9) | <0.001 |
| EDE: mean (s.d.) | 3.6 (1.3) | 3.7 (1.4) | 3.5 (1.2) | 0.59 |
| ANR/ANP, % | 49/51 | 47/53 | 55/45 | 0.55 |
| Previous ED treatment, % | 74 | 65 | 91 | 0.02 |
| Previous hospitalisation, % | 46 | 36 | 65 | 0.02 |
| Medication, % | 58 | 52 | 68 | 0.22 |
| Relationship, % | 37 | 43 | 24 | 0.13 |
| Welfare, % | 25 | 11 | 53 | 0.001 |
| BDI: mean (s.d.) | 29.9 (13.8) | 28.8 (13.2) | 32.1 (14.9) | 0.35 |
| STAI trait: mean (s.d.) | 59 (10.7) | 59.3 (10.7) | 58.4 (10.9) | 0.73 |
| STAI state: mean (s.d.) | 56.7 (12.8) | 56.6 (12.7) | 56.9 (13.3) | 0.94 |
| TAS: mean (s.d.) | 61.3 (9.2) | 61.4 (9.2) | 61.2 (9.4) | 0.94 |
| MacCAT-T appreciation: mean (s.d.) | 3.71 (0.62) | 3.82 (0.44) | 3.48 (0.85) | 0.03 |
| Depressive disorder, % | 48.4 | 45.6 | 55.6 | 0.47 |
| PTSD, % | 23.3 | 23.8 | 22.2 | 0.89 |
MC, mental capacity; BMI, body mass index; EDE, Eating Disorder Examination; ANR, anorexia nervosa restrictive type; ANP, anorexia nervosa purging type; ED, eating disorder; BDI, Beck Depression Inventory; STAI, Spielberger Trait State Anxiety Inventory; TAS, Toronto Alexithymia Scale; MacCAT-T, MacArthur Competence Assessment Tool-Treatment; PTSD, post-traumatic stress disorder.
Clinical measures
Severity of eating disorder symptoms was rated with the Eating Disorder Examination Questionnaire (EDEQReference Fairburn and Beglin 30 , Reference Aardoom, Dingemans, Slof Op't Landt and Van Furth 31 ) and the BMI (in kg/mReference Keski-Rahkonen and Mustelin 2 ) as measured by the Digital Tanita scale (Tanita Cooperation of America, Inc., Arlington Heights, IL). Eating disorder treatments and admissions were collected from the participants and from their files (when available), social functioning from the social history. Remission rates were assessed. Full remission was defined as having a weight in the normal range (BMI 18.5–25 kg/mReference Keski-Rahkonen and Mustelin 2 ), having resumed menses (or likely to when contraception was used and weight was in the normal range) and having no more disabling anorectic cognitions (assessed in an interview). Partial remission was defined as having two out of three of these criteria. The presence of legal measures regarding their AN was asked for. Depression and anxiety levels were measured with the Beck Depression Inventory (BDI-IIReference Beck, Steer and Brouwn 32 ) and Spielberger Stait Trait Anxiety Inventory (STAIReference Spielberger, Gorsuch, Lushene, Vagg and Jacobs 33 ), respectively. Furthermore, levels of alexithymia were assessed with the Toronto Alexithymia Scale (TASReference Bagby, Parker and Taylor 34 , Reference Bagby, Taylor and Parker 35 ).
Mental capacity
At baseline, mental capacity to consent to treatment was assessed by psychiatrists experienced in the treatment of severe eating disorders. Based on this assessment, two groups were distinguished: a group with full mental capacity to consent to treatment and a group with diminished mental capacity to do so. At baseline, the MacArthur Competence Assessment Tool-Treatment (MacCAT-TReference Grisso, Appelbaum and Hill-Fotouhi 25 ) was used. The MacCAT-T is a semi-structured interview designed to aid clinicians in determining the level of mental capacity to consent to treatment. It has good interrater reliability and construct validity and has been used in mental capacity studies in several psychiatric populations.Reference Okai, Owen, McGuire, Singh, Churchill and Hotopf 26 As previously reported,Reference Elzakkers, Danner, Hoek and van Elburg 29 appreciation of disorder and treatment was significantly lower in the group with diminished mental capacity. Therefore, we repeated this MacCAT-T measurement at follow-up. This was done in a face-to-face interview, when this was not feasible it was done by phone.
Decision-making
The Iowa Gambling Task (IGTReference Bechara, Damasio, Damasio and Anderson 36 ) was used to assess decision-making ability. The task requires participants to choose a card from four different decks and with each choice they win and sometimes also lose money. Two decks are more advantageous, whereas the other two decks are disadvantageous in the long run and participants have to find this out by relying on their ‘gut feeling’. Decision-making is determined by calculating the net score for all 100 trials as the difference in number of choices between the advantageous and disadvantageous decks.
Statistical analysis
A fully direct Bayes approach (FDB) was used to optimally account for the sample size and missing data attributable to attrition.Reference Barnes, Lindborg and Seaman 37 Each outcome of interest was fitted as a separate univariate model. There was no a priori hypothesis for the growth trajectory over time, so latent basis models were fitted, allowing the data to determine linear or non-linear growth. BMI is included as a control variable in all models to satisfy the assumption that missing values are missing at random. Prior distributions were formed using the method of McNeishReference McNeish 38 , and models were fit in Mplus 7.1 with a Bayesian MCMC (Markow chain Monte Carlo) algorithm with a Gibbs Sampler and two chains with 50 000 MCMC iterations per chain. Bayesian estimation was utilised, so frequentist P-values are unavailable. To keep reporting of results succinct and familiar to readers unfamiliar with Bayesian statistics, we report Bayesian P-values (P B). These P-values are based on the quantiles of the posterior distribution rather than area beyond a test statistic under a null distribution (as with frequentist P-values). Thus, ‘significance’ in our results refers to a value of 0 being highly unlikely in the posterior distribution rather than rejecting the null hypothesis in a frequentist setting, which are conceptually related but not identical.Reference Muthen 39
Results
Sample characteristics
After 1 year, 56 people (80%) agreed to cooperate again and after 2 years 50 people (71%) of the original 70 participants (see Fig. 1). After 1 year, 57 of the people (82%) were still in care for their eating disorder and after 2 years 48 (69%); this was not significantly different between the two groups (P=0.39 and P=0.91, respectively). Only one participant in our study was held under the Mental Health Act (MHA) at baseline, not because of his or her eating disorder, but because of comorbid alcohol dependence. No one was held under a section of the MHA during follow-up. In the first year of follow-up, one patient died of AN-related complications. We know that after the end of the study (after the second follow-up), another patient died. Both were judged to have diminished mental capacity to consent to treatment at baseline and had a BMI below 15 kg/mReference Keski-Rahkonen and Mustelin 2 .
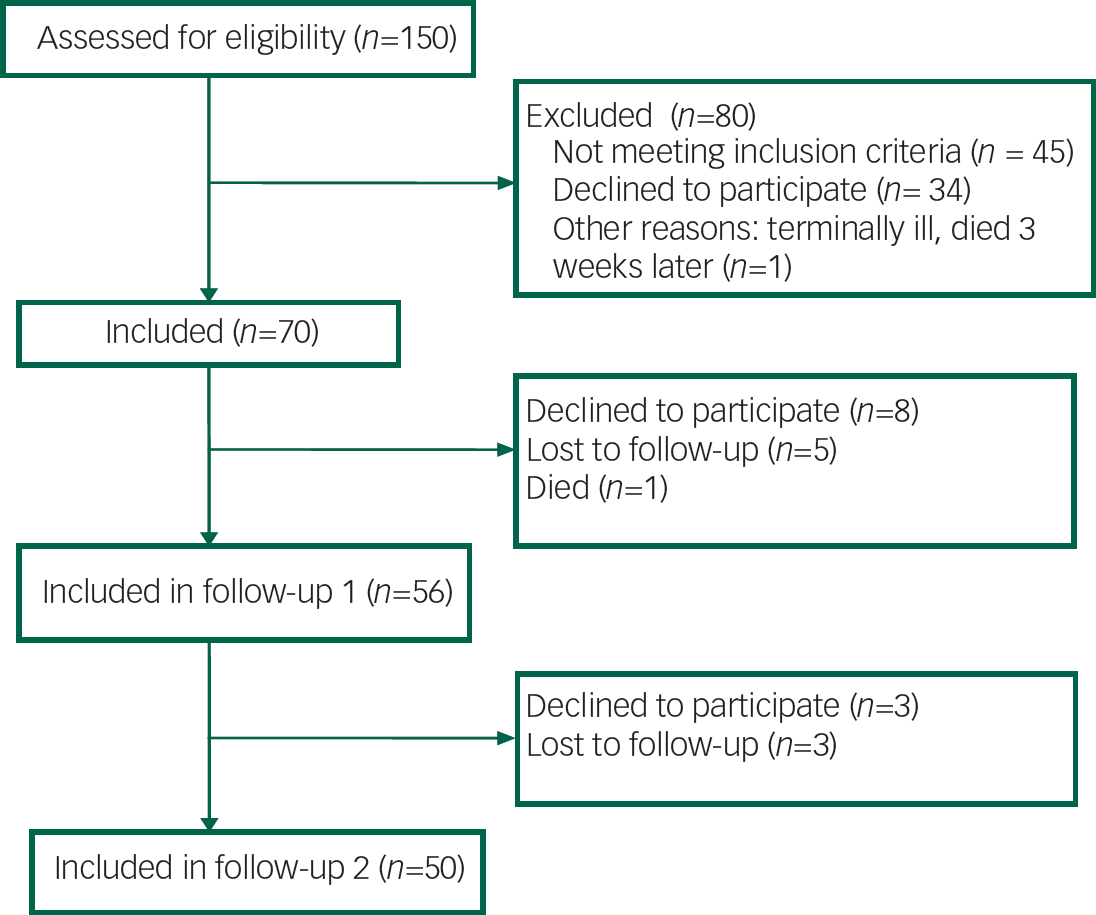
Fig. 1 Flow diagram of inclusion and follow-up process.
Is the course of disorder different with respect to clinical variables?
Body mass index
Figure 2 shows results from an unconditional growth model for BMI. Both groups show a significant increase in BMI from baseline to the Year 1 (P B<0.001) but a non-significant change from Year 1 to Year 2 (P B=0.38). The growth over time was not significantly different between the groups (P B=0.70). The diminished mental capacity group had a significantly lower BMI at baseline than the full mental capacity group (14.2 kg/mReference Keski-Rahkonen and Mustelin 2 , P B<0.001), and this significant difference persisted over time. In DSM-5 terminology, this represents on average a change in category from moderate to mild for the group with full mental capacity and from extreme to moderate for the group with diminished mental capacity. The fit of the model was quite good with a posterior predicted P (PPP) value of 0.542 (PPP ranges from 0 to 1 and 0.50 is ideal).
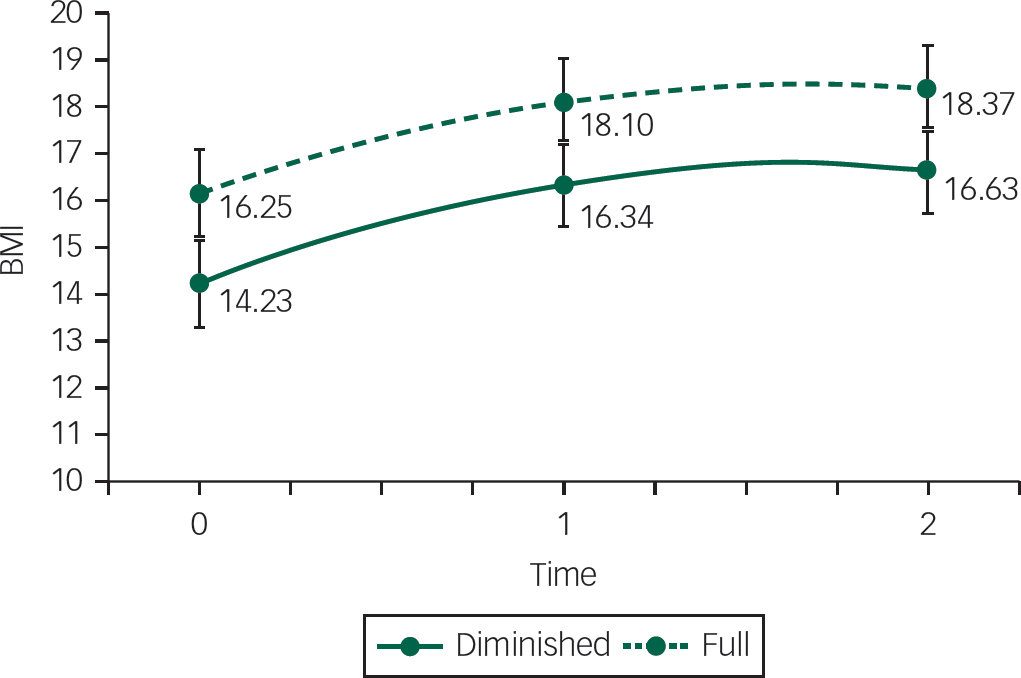
Fig. 2 BMI change (in kg/m2) between baseline, first follow-up (after 1 year) and second follow-up (after 2 years) between the group with full mental capacity (full) and the group with diminished mental capacity (diminished).
In-patient treatment
Difficulties with sample size and missing data were too great to fit a growth model with this outcome, so we fit models separately at each time point. At both follow-up time points, the group with diminished mental capacity had a borderline significant increase in the probability of having received in-patient treatment after controlling for BMI at baseline (after 1 year 63% v. 47%, P B=0.053; after 2 years, 37% v. 23% P B=0.057). However, after controlling for previous admissions, this difference was no longer significant at 1 year follow-up (P B=0.096), but the difference became more significant after 2 years follow-up (P B=0.034). Patients with previous admissions were more likely to have been admitted in the course of 1 year (P B=0.029) and between the first and second year of follow-up (P B=0.022), regardless of group. After 1 year follow-up, previous admission is largely responsible for the differences between the groups. Between the first and second year follow-up, the difference between the groups was not fully explained by BMI and previous admissions.
Remission rate
Unlike all other models, the remission outcome includes BMI as part of the criteria. We considered the conceptual appropriateness of including BMI as a covariate and whether the partial redundancy would hinder interpretation or estimation of the model. We ran the model two different ways, one with BMI as a covariate and one without. The results were quite similar, and inferential conclusion did not differ between the models. We therefore report only the model with BMI as a covariate in Table 2. Similar to the model for in-patient treatment, estimation difficulties required that we fit a separate model to each time point rather than a single longitudinal model. Remission rate is also a binary variable, so we used logistic models to determine predicted probabilities of remission. As shown in Table 2, after 2 years the group with diminished mental capacity was more likely to show no remission (53.9% compared with 26.6% in the full mental capacity group, P B=0.026). Full remission rates were still low (35.8 and 38.9%, respectively) in both groups at 2 year follow-up.
Table 2 Percentage of each mental capacity group in each remission category

| No remission | Partial remission | Full remission | ||
|---|---|---|---|---|
| After 1 year | Diminished MC | 69.8 | 16.3 | 14.0 |
| Full MC | 44.8 | 40.7 | 13.7 | |
| P B | 0.03 | 0.05 | 0.49 | |
| BMI P B | 0.42 | 0.16 | 0.16 | |
| After 2 years | Diminished MC | 53.9 | 10.8 | 35.8 |
| Full MC | 26.6 | 33.7 | 38.9 | |
| P B | 0.03 | 0.05 | 0.48 | |
| BMI P B | 0.45 | 0.32 | 0.27 |
MC, mental capacity; BMI, body mass index.
The P-value is the comparison between the diminished and full groups in each column. For example, the first P B-value of 0.03 shows that the difference between 69.6 and 45.0% is significant.
Eating disorder pathology
At the two follow-up measurements, the EDE-Q was measured. In the analysis BMI was controlled for. The group with full mental capacity went from an EDEQ global score of 3.08 at follow-up 1 to 2.76 at follow-up 2, which is a non-significant change (P B=0.15). The group with diminished mental capacity went from 2.59 to 2.27, which is also non-significant (P B=0.27). Eating disorder pathology as measured by the EDE-Q did not differ between the groups after 1 year or after 2 years (P B=0.21).
Is the course of disorder different with respect to psychological variables?
Separate latent growth models were fit to each outcome all controlling for BMI. Both the full and the diminished mental capacity group improved significantly after 2 years in depression score (BDI improved from both 30 to both 20, P B<0.001) and anxiety score (STAI state improved from 57–54 to 44–42, respectively, P B<0.001), there are no significant differences between groups at any time-point (BDI: P B=0.44, STAI: P B=0.42). As shown in Fig. 3, the full mental capacity groups showed a significant improvement in alexithymia score (60.8– 48.8, P B<0.001), which was below the clinical cut-off of 52 for possible alexithymia.Reference Bagby, Parker and Taylor 34 , Reference Bagby, Taylor and Parker 35 The diminished mental capacity group did not improve (P B=0.10) and stayed around the clinical cut-off of 61 for alexithymia. The difference over time between groups was significant (P B=0.006). The PPP values of the alexithymia, depression and anxiety score models were 0.41, 0.48 and 0.59, respectively, all indicating acceptable fit.
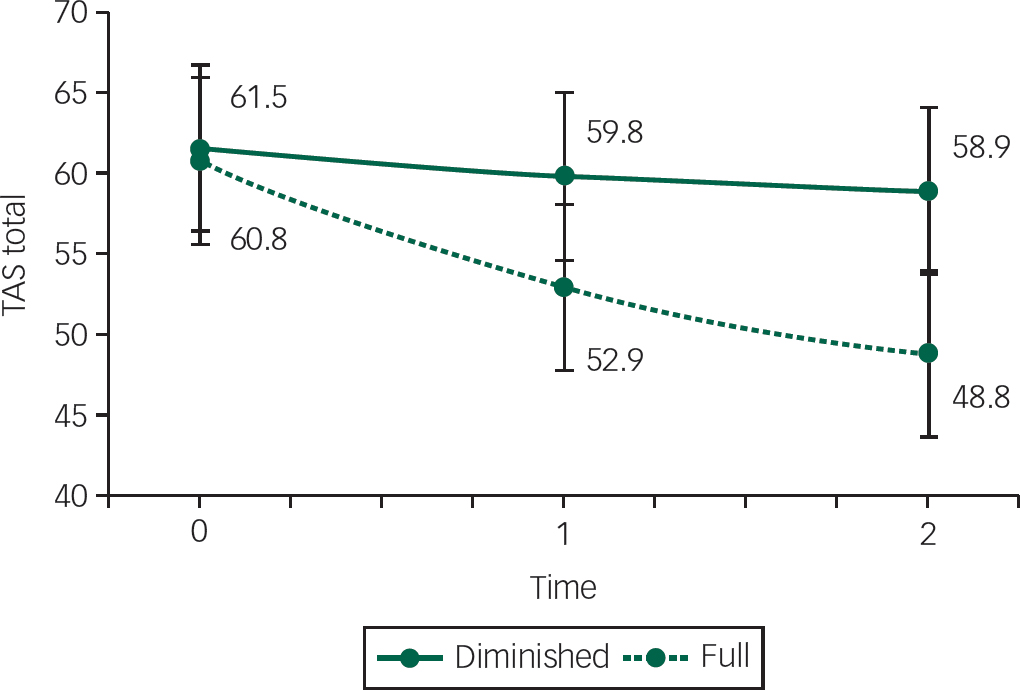
Fig. 3 Alexithymia scores between baseline, first follow-up (after 1 year) and second follow-up (after 2 years) between the group with full mental capacity (full) and the group with diminished mental capacity (diminished), controlled for BMI (in kg/m2).
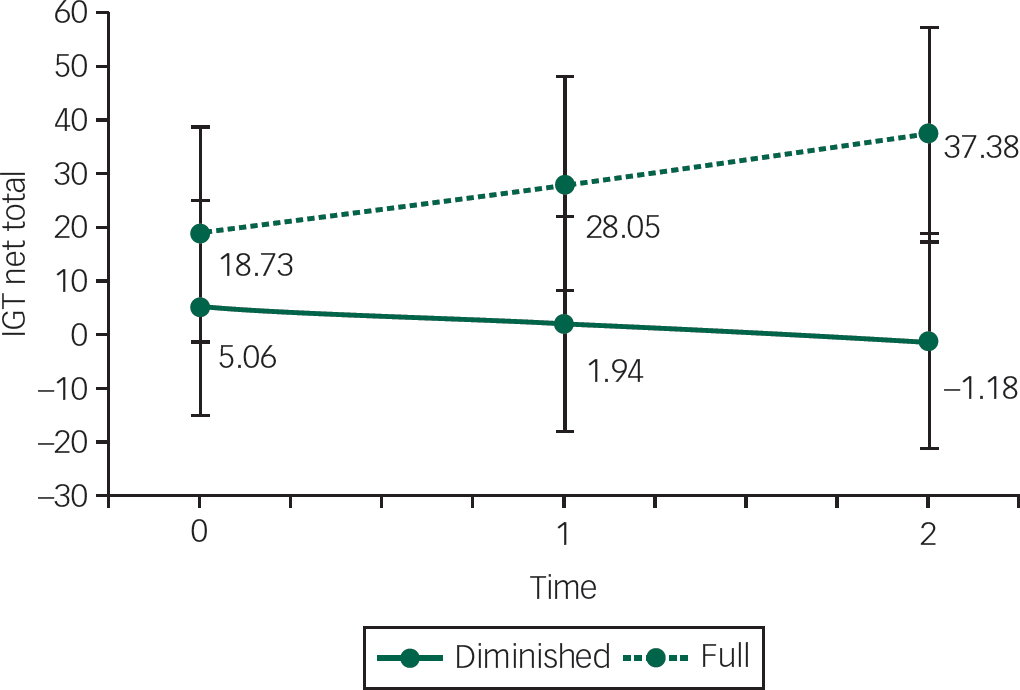
Fig. 4 Iowa Gambling Task (IGT) scores between baseline, first follow-up (after 1 year) and second follow-up (after 2 years) between the group with full mental capacity (full) and the group with diminished mental capacity (diminished), controlled for BMI (in kg/m2), depression and alexithymia scores.
Is the course of disorder different with respect to decision-making?
Decision-making task
Changes in decision-making were modelled with a latent growth model. Because symptoms of depression and alexithymia may theoretically have an influence on decision-making ability,Reference Danner, Sternheim, Bijsterbosch, Dingemans and van Elburg 40 , 41 a model was tested including BDI and TAS next to BMI as control variables. The group difference at baseline was not significant in this model (19.0 v. 5.9; P B=0.11). BMI (P B=0.43), TAS (P B=0.32) and BDI (P B=0.30) were not significant predictors of the IGT score at baseline nor were they significant predictors of the change over time (BMI P B=0.16, TAS P B=0.41 and BDI P B=0.38). The two groups differed in their change over time, with the full mental capacity group doing better than the diminished mental capacity group (P B=0.040; see Fig. 4). The PPP value for this model was 0.514.
Appreciation
The appreciation scores of the MacCAT-T were difficult to analyse over time as the distribution was highly negatively skewed (most participants scored 3 or higher). Therefore, we conducted a mean comparison test in the Bayesian framework which allows the normality assumption to be relaxed. The descriptive mean scores, Bayesian P-values and standardised effect differences are reported for each time point in Table 3. The group with full mental capacity did well at baseline and kept appreciating well. The group with diminished mental capacity differed noticeably at baseline and after 2 years.
Table 3 Appreciation scores over time between groups
| Full mental capacity mean (s.d.) | Diminished mental capacity mean (s.d.) | Group difference P B | Standardised effect | |
|---|---|---|---|---|
| Baseline | 3.8 (0.4) | 3.5 (0.8) | 0.02 | 0.25 |
| One year follow-up | 3.8 (0.5) | 3.6 (0.5) | 0.12 | 0.16 |
| Two year follow-up | 3.8 (0.5) | 2.9 (1.4) | <0.01 | 0.40 |
Discussion
This is the first large study into mental capacity to consent to treatment in people who are severely ill with AN using a longitudinal design. The results of this follow-up study have two important implications. First, prognosis seems more unfavourable for the group with diminished mental capacity to consent to treatment. Participants with full mental capacity had a mild AN at follow-up, whereas those with diminished mental capacity still fell within the moderately ill category (DSM-5 41 ). And as the rise in BMI mainly occurred in the first year after starting treatment and the percentage of no and partial remission is significantly higher in the group with diminished mental capacity, one would not expect the diminished mental capacity group to reach full remission in the near future. In the long run, diminished mental capacity to consent to treatment means a higher likelihood of in-patient treatment. These findings suggest a longer duration of care for this particular group. Although the diminished mental capacity group had a lower BMI at baseline, other parameters of prognostic relevance such as duration of illness, percentage of participants with the purging subtype of AN or comorbidity were equal between the groups. Diminished mental capacity therefore seems a factor of relevance to prognosis, next to the more obvious factor of BMI. Both groups improved on BMI at 1 year follow-up and maintained this improvement 1 year later at 2 year follow-up, which is reassuring. Also, anxiety and depression levels lower equally in the course of treatment, and remission rates after 2 years were similar.
A second important finding in this study supports the decision-making difficulties clinicians so clearly observe in everyday practice on a more fundamental level. Using the IGT, it has become clear that decision-making is more maladaptive in people with diminished mental capacity, independent of BMI. The IGT is based upon the theoretical model by Damasio (somatic marker hypothesisReference Damasio 42 , Reference Bechara, Damasio, Tranel and Damasio 43 ), which states that adaptive decision-making is not a merely rational process but relies heavily on emotional factors and ‘gut feeling’. Emotional dysregulation has been found to be an important maintaining factor in AN.Reference Treasure and Schmidt 23 , 41 , Reference Fairburn, Cooper, Doll, O'Connor, Bohn and Hawker 44 – Reference Wildes, Marcus, Cheng, McCabe and Gaskill 46 In this study, participants also displayed high levels of emotional problems, such as severe depressive symptoms, a high level of anxiety and moderate to high levels of alexithymia. Although depression scores decreased significantly during treatment, levels indicative of moderate depression still existed after 2 years. In addition, in the diminished mental capacity group, alexithymia levels remained at a clinical level even after weight improvement. However, even after controlling for BMI, depression and alexithymia, the diminished mental capacity group still performed significantly worse on decision-making over time. This suggests that the difference between groups cannot be fully explained by the difference in emotional problems as measured in this study (BDI, TAS). Appreciation of the diminished mental capacity group over time remained less than that of the full mental capacity group, linking the concept of more fundamental decision-making (and ‘gut feeling’) to the concept of appreciation in AN. Future research should therefore be focused on the interplay between emotional dysregulation (as measured with more direct markers) so often found in AN and the diminished appreciation of illness and treatment.
The high level of emotional problems in our participants support the emphasis laid on emotion recognition and processing in recently developed cognitive–affective treatments for AN, such as the Maudsley Anorexia Nervosa Treatment for Adults (MANTRAReference Schmidt, Wade and Treasure 47 ) and enhanced form of cognitive–behavioural therapy (CBT-EReference Fairburn 48 ). In recent years, several randomised clinical trials have been done that have shown that both MANTRA, CBT-E and Focal Psychodynamic Therapy (FPT) have a positive effect on outcome in AN.Reference Schmidt, Oldershaw, Jichi, Sternheim, Startup and McIntosh 49 – Reference Schmidt, Magill, Renwick, Keyes, Kenyon and Dejong 51 It is as yet not clear what works for whom. Perhaps, MANTRA is of more value to people with AN with a higher level of affective dysregulation, but this is speculative. Also motivational stage of change might be an important factor, although a recent study could only show a relation between the stage of contemplation and the strength of the therapeutic alliance, but not outcome.Reference Mander, Keifenheim, Zipfel and Giel 52 , Reference Mander, Jacob, Götz, Sammet, Zipfel and Teufel 53
Strengths and limitations
Major strengths in this study are the longitudinal design, the high participation after 1 and 2 year follow-up (80 and 70%, respectively) and the generalisability of the results, as this was a naturalistic study. Also the assessment of decision-making on a clinical as well as on a more fundamental level provided the opportunity to bring together more basic science and bedside, a strategy very fruitful to move forward in the body of knowledge regarding an issue so complex as decision-making.
This study being a naturalistic study with hardly any exclusion criteria, there were missing data in the course of follow-up. For a clinical study with people with AN, who are usually highly avoidant of treatment,Reference Hoek 11 , Reference Keski-Rahkonen, Hoek, Susser, Linna, Sihvola and Raevuori 12 we consider the loss to follow-up of 20 and 29% after 1 and 2 years as acceptable. Also, in the statistical analyses missing data were accounted for. Nevertheless, outcome might have been influenced by these missing data.
Although clinicians doing the clinical judgment were masked to the outcome of the MacCAT-T, for obvious reasons, they could not be masked to their own assessment of mental capacity. We do not think this resulted in treatment bias on the part of the clinicians as this assessment is part of routine clinical practice, especially in complex cases and therefore has not had a major influence on treatment advised.
In our previously reported study,Reference Elzakkers, Danner, Hoek and van Elburg 29 a substantial group was found to have diminished capacity to consent to treatment. Contrary to what might be expected, follow-up results show that this particular group improves on both weight, eating disorder and more general psychopathology, which is encouraging. On the down side, after 2 years BMI is still in the moderately severe range and longer duration of care is expected. Decision-making on a more fundamental level is maladaptive proposed to be caused by an interaction between emotional dysregulation and lack of appreciation of illness and treatment. Therefore, a key component in treatment should be to improve precisely this hampered emotional functioning, a feature central to more recently developed AN treatments like MANTRA and CBT-E. Whether or not the heightened focus on these emotional difficulties will improve adaptive decision-making is an issue that should be assessed in future research.
Funding
This research was supported by a grant from the Nuts Ohra Foundation.











eLetters
No eLetters have been published for this article.