Introduction
Anxiety disorders are among the most common types of mental disorder worldwide. The National Comorbidity Survey Replication reported that, from 2001 to 2003, an estimated 19.1% of the adult population in the USA had anxiety disorder, and it estimated that the lifetime morbid risk of the general population was 31.1%.Reference Kessler, Chiu, Demler, Merikangas and Walters1 The prevalence of common mental disorders, including anxiety disorders, also increased from 11.5% in 1990 to 23.8% in 2010 in Taiwan.Reference Fu, Lee, Gunnell, Lee and Cheng2 The risk factors for anxiety disorder have been extensively explored and discussed, and alcohol use and/or tobacco use have been examined as risk factors for anxiety in previous studies.Reference Blanchard, Magee, Veniegas and Blanchard3,Reference Buckner and Vinci4 Although some studies have proposed several candidate mechanisms underlying how alcohol or tobacco increases anxiety, further clarification is required.Reference Schuckit and Hesselbrock5,Reference Fluharty, Taylor, Grabski and Munafò6 Another key topic is whether alcohol use and tobacco use are caused by anxiety or vice versa. Because alcohol and tobacco are regularly consumed,Reference Zhang, Guo, Saitz, Levy, Sartini and Niu7,Reference Dai, Gakidou and Lopez8 anxiety interventions that target these substances have considerable utility to public health.
In addition to alcohol and tobacco use, other factors may affect anxiety (e.g. sex, age, exercise habits, coffee or tea drinking, sleep profile and family history of mental illness). The prevalence of anxiety disorder has been reported to be higher among women (women versus men, 23.4 and 14.3%, respectively).Reference Kessler, Chiu, Demler, Merikangas and Walters1,Reference Buckner and Vinci4 Some studies have indicated that younger age is associated with a higher risk of anxiety disorders.Reference Kessler, Petukhova, Sampson, Zaslavsky and Wittchen9 Regular exercise was identified as a protective factor against anxiety disorders.Reference Carek, Laibstain and Carek10 Although caffeine consumption has long been proposed and studied as either a protective or risk factor for various psychiatric disorders, most studies have reported that caffeine intake exacerbates the symptoms of anxiety and agitation.Reference Jee, Lee, Bormate and Jung11,Reference Torabynasab, Shahinfar, Payandeh and Jazayeri12 Tea, which contains L-theanine (an amino acid that can enhance cognitive function), is widely consumed, and studies have suggested that tea consumption reduces the symptoms of anxiety.Reference Torabynasab, Shahinfar, Payandeh and Jazayeri12,Reference Williams, Everett, D’Cunha, Sergi, Georgousopoulou and Keegan13 Furthermore, adequate sleep is crucial to various aspects of human health.Reference Scott, Webb, Martyn-St James, Rowse and Weich14,Reference Kim, Kim, Jang and Park15 Studies have suggested that sleep deprivation increases the risk of mental illnesses such as anxiety.Reference Scott, Webb, Martyn-St James, Rowse and Weich14 In addition, a family history of mental illness should be considered during the evaluation of anxiety risk.Reference Milne, Caspi, Harrington, Poulton, Rutter and Moffitt16,Reference van Sprang, Maciejewski, Milaneschi, Elzinga, Beekman and Hartman17 The identification of these associations can help people modify their lifestyle habits and safeguard their mental health.
This study investigated the association of alcohol and tobacco use with anxiety. We also identified various risk and protective factors for anxiety in people from different sex and age groups who either use tobacco and alcohol or not.
Method
Taiwan Biobank
The Taiwan Biobank (TWB) was established by Taiwan’s government to collect lifestyle and genetic data on the Taiwanese population.Reference Fan, Hung and Yeh18–Reference Chen, Lu, Lai, Bair and Cheng20 Those in the TWB programme volunteer to participate, and they comprise individuals aged between 30 and 70 years without a history of cancer. After signing an informed consent form, participants in the TWB programme provide information regarding their daily lives, blood samples and physical examination results. In addition, each participant completes a questionnaire administered during a face-to-face interview with a TWB researcher. The questionnaire pertains to the participants’ personal information and lifestyles.
Study instruments
Anxiety measurement tool
In the TWB, Patient Health Questionnaire 4 (PHQ-4) was used to assess participants’ levels of depression and anxiety. In the present study, participants were defined as having anxiety disorder if they had a total score of ≥3 for the first two questions of PHQ-4, based on a two-item anxiety scale (Generalized Anxiety Disorder 2-item).Reference Löwe, Wahl, Rose, Spitzer, Glaesmer and Wingenfeld21
Alcohol and tobacco use
The TWB participants included in the present study were classified as alcohol users if they reported a weekly alcohol intake of >150 mL for at least 6 months and were still using alcohol when they completed PHQ-4. Those who had smoked regularly for at least 6 months and were still smoking when they completed PHQ-4 were classified as tobacco users.
Covariates
This study consulted the literature and included controls for sex, age, body mass index (BMI; weight (kg)/height (m)), exercise habits, educational attainment, sleep profile (including total sleep time on weekdays and weekends), social jet lag (SJL) between weekdays and weekends, sleep quality and family history of mental illness. Among the sleep quality data retrieved from the TWB, sleep quality was originally rated as either very good, good, average, bad or very bad. However, in our analysis, sleep quality was reclassified as either good+ (very good, good and average) or bad+ (bad and very bad). The concept of SJL refers to differences in sleep patterns between weekdays (workdays) and weekends (sleep hour difference between weekdays and weekends). SJL was revealed to be related to psychiatric disorders, including anxiety.Reference Caliandro, Streng, van Kerkhof, van der Horst and Chaves22 Furthermore, we collected data on whether menopause had occurred in women participating in the TWB.
The demographic data comprised sex, age, exercise habits, educational attainment and sleep profile; these data were obtained from participants via interviews conducted through the TWB programme. The TWB contains information on body height and weight of each participant, enabling calculation of their BMI.Reference Fu, Lee, Gunnell, Lee and Cheng2
Ethics statement
Establishment of the TWB was approved by the Institutional Review Board of Biomedical Science Research/IRB-BM, Academia Sinica, Taiwan, and by the Ethics and Governance Council of Taiwan Biobank, Taiwan. Written informed consent was obtained from all TWB participants in accordance with official regulations and the principles of the Declaration of Helsinki. The present study was also approved by the Institutional Review Board of MacKay Memorial Hospital (IRB no. 21MMHIS351e).
Statistical analysis
Participant characteristics were described using means (standard deviation, s.d.) for continuous variables and frequencies (percentages) for categorical variables; odds ratios with 95% CIs were used to describe differences between the use versus non-use of alcohol and/or tobacco. All variables were compared using one-way analysis of variance for continuous data, and χ 2 tests (or Fisher’s exact test) for categorical data. Participant characteristics with a P-value of <0.05 were included in the logistic regression model, which was used to determine the covariate-adjusted odds ratio for the risk of anxiety. All data transformations and statistical analyses were conducted using the statistical software SAS for Windows (version 9.4; SAS Institute, Cary, NC, USA). A null hypothesis was rejected at an alpha level of 0.05.
Results
Basic characteristics of TWB participants
Following the exclusion of respondents aged <40 years (n = 3201) and those with incomplete or missing information related to independent variables of interest (n = 1093), 27 916 participants were included in our analysis. All data pertaining to the included participants (i.e. PHQ-4 results, alcohol and tobacco use, sex, age, BMI, exercise habits, coffee and tea consumption, education level, residential urbanicity, family history and sleeping profile) are listed in Table 1.
Table 1 Baseline characteristics of all follow-up participants stratified by alcohol drinking and smoking behaviors (N = 30 836)
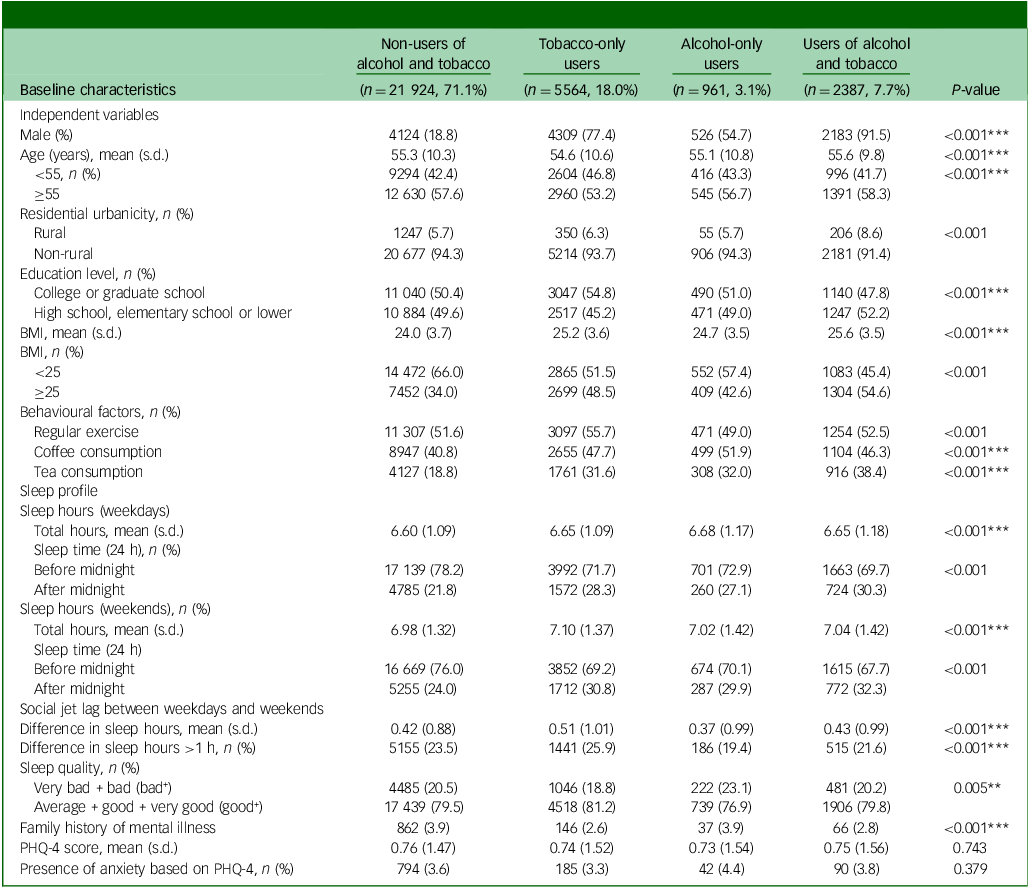
s.d., standard deviation.
*P < 0.05, **P < 0.01, ***P < 0.001 (P-value, χ 2 test or one-way analysis of variance test).
The included participants were classified into four groups based on smoking and drinking status: non-users of both alcohol and tobacco (n = 19 889, 71.2%), tobacco-only users (n = 4947, 17.7%), alcohol-only users (n = 858, 3.1%) and users of both alcohol and tobacco (n = 2222, 8.0%). Mean (s.d.) PHQ-4 scores for the four groups were as follows: non-users of both alcohol and tobacco, 0.76 (1.47); tobacco-only users, 0.74 (1.52); alcohol-only users, 0.73 (1.54); and users of both alcohol and tobacco, 0.75 (1.56). Because PHQ-4 scores in the TWB were low in our survey, we added binary measures of anxiety. In accordance with the previous study,Reference Löwe, Wahl, Rose, Spitzer, Glaesmer and Wingenfeld21 a participant was defined as having anxiety disorder if they had a total score of ≥3 for the first two questions in PHQ-4. The prevalence of anxiety according to PHQ-4 scores of the four groups was as follows: non-users of both alcohol and tobacco, 794 (3.6%); tobacco-only users, 185 (3.3%); alcohol-only users, 42 (4.4%); and users of both alcohol and tobacco, 90 (3.8%). That is, anxiety based on PHQ-4 scores did not differ significantly between alcohol and tobacco users in the univariate analysis. Therefore, we used logistic regression for a multivariate test, as recommended in previous studies.Reference Morissette, Tull, Gulliver, Kamholz and Zimering23,Reference Anker and Kushner24
Significant covariates with P < 0.05 (i.e. sex, age, BMI, exercise habits, coffee and tea consumption, education level, residential urbanicity, family history and sleeping profiles (including SJL and sleep quality)) were controlled for in a subsequent multivariate analysis. Definitions of covariates are listed in Supplementary Table 1.
Influence of tobacco and alcohol use on anxiety
Those participants who were non-users of both tobacco and alcohol formed the reference group, which was compared with those who were tobacco-only users, alcohol-only users or users of both tobacco and alcohol. All variables with significant results (P < 0.05) in our univariate analysis were selected as covariates for our logistic regression analysis. Tobacco-only users, alcohol-only users and users of both tobacco and alcohol were compared with the reference group (non-users of both tobacco and alcohol), and were revealed as being more prone to developing anxiety (adjusted odds ratio (aOR) with 95% CI: tobacco-only users, 1.30 [1.08–1.56]; aOR with 95% CI: alcohol-only users, 1.51 [1.09–2.10]; aOR with 95% CI: users of both tobacco and alcohol, 1.77 [1.36–2.29]). Several covariates (i.e. age, sex, exercise habits, tea consumption and sleep quality) were significantly correlated with a reduced risk of anxiety (aOR [95% CI]: age ≥55 years, 0.60 [0.52–0.69]; tea consumption, 0.84 [0.72–0.98]; regular exercise, 0.69 [0.60–0.79]; and good+ sleep quality, 0.28 [0.25–0.32]) By contrast, female sex was significantly correlated with an increased risk of anxiety (aOR [95% CI]: 1.91 [1.60–2.27]). These results are listed in Table 2.
Table 2 Effect of alcohol drinking and smoking behaviours on risk of anxiety
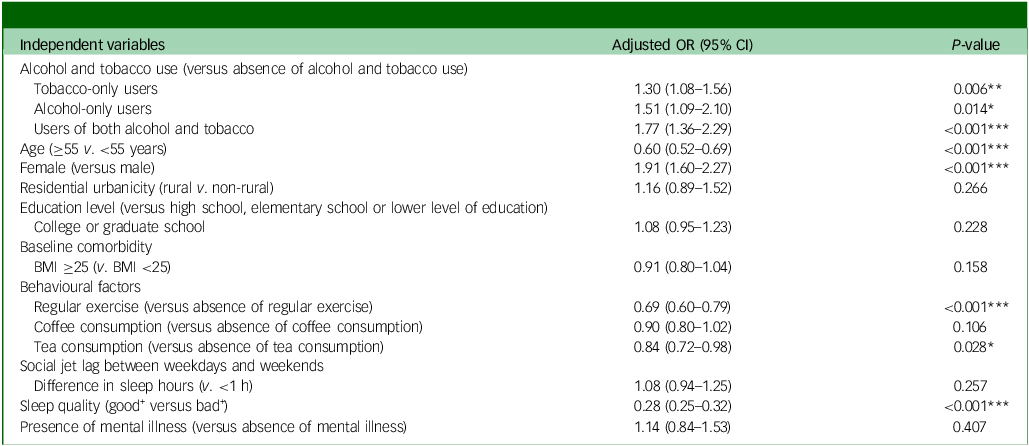
BMI, body mass index; CI, confidence interval; OR, odds ratio.
*P < 0.05, **P < 0.01, ***P < 0.001.
Sex-stratified difference in influence of tobacco and alcohol use on anxiety
According to a sex-stratified analysis among women, the use of tobacco only (aOR [95% CI], 1.33 [1.04–1.70]) and the use of both tobacco and alcohol (2.12 [1.31–3.43]) were associated with higher anxiety risk relative to their non-use. Among men, only the use of both tobacco and alcohol (1.67 [1.19–2.33]) was associated with a higher anxiety risk relative to their non-use. For both male and female participants, several covariates (e.g. age ≥55 years, regular exercise and sleep quality) were significantly correlated with a reduced risk of anxiety (aOR [95% CI]: male participants aged ≥55 years, 0.50 [0.38–0.6]; female participants aged ≥55 years, 0.61 [0.49–0.76]; male participants who exercised regularly, 0.69 [0.53–0.91]; female participants who exercised regularly, 0.69 [0.59–0.81]; male participants with good+ sleep quality, 0.29 [0.23–0.37]; and female participants with good+ sleep quality, 0.28 [0.24–0.32]). Those male participants who drank tea had a significantly lower risk of anxiety (aOR [95% CI]: 0.74 [0.56–0.97]), whereas those with a family history of mental illness had a significantly higher risk of anxiety (aOR [95% CI]: 2.05 [1.12–3.75]). These results are listed in Table 3.
Table 3 Sex-stratified effects of alcohol drinking and smoking behaviours on risk of anxiety
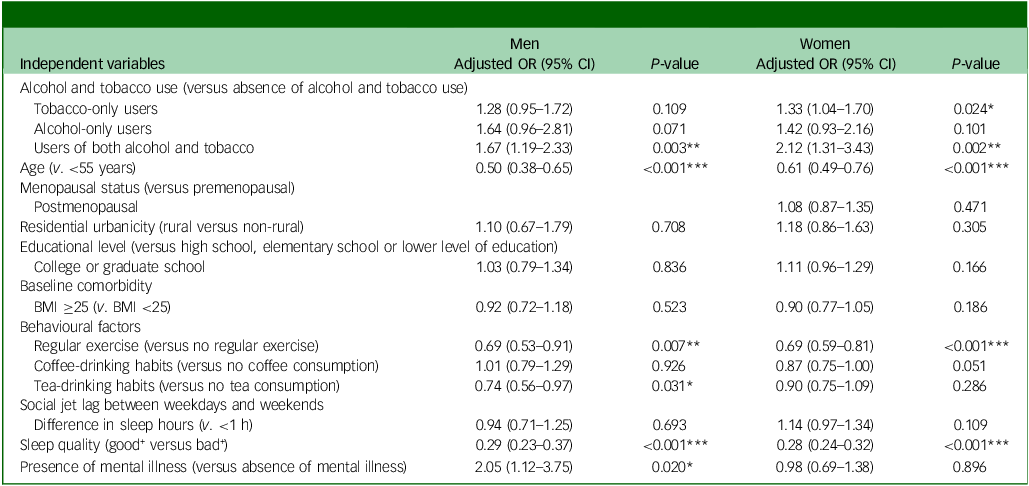
BMI, body mass index; CI, confidence interval; OR, odds ratio.
*P < 0.05, **P < 0.01, ***P < 0.001.
Influence of tobacco and alcohol use on anxiety in men across age groups
We compared the results of male participants aged <55 and ≥55 years. In both age groups, participants who were users of both tobacco and alcohol were more prone to having anxiety than were those who were users of neither product (aOR [95% CI]: male participants aged <55 years with tobacco and alcohol use, 1.64 [1.08–2.49]; and male participants aged ≥55 years with tobacco and alcohol use, 1.84 [1.03–3.27]). Among male participants aged ≥55 years, those who were tobacco-only users were more prone to having anxiety (aOR [95% CI]: 1.84 [1.12–3.04]); this significant difference was not identified in male participants aged <55 years. In both age groups, male participants with good+ sleep quality were less prone to having anxiety than were those without (aOR [95% CI]: male participants aged <55 years with good+ sleep quality, 0.24 [0.17–0.33]; and male participants aged ≥55 years with good+ sleep quality, 0.40 [0.26–0.60]). Notably, male participants aged <55 years were more prone to having anxiety if they lived in a rural area. By contrast, male participants aged ≥55 years were less prone to having anxiety if they lived in a rural area (aOR [95% CI]: male participants aged <55 years who lived in a rural area, 2.76 [1.12–6.81]; and male participants aged ≥55 years who lived in a rural area, 0.49 [0.27–0.90]). Those male participants aged <55 years and who had a family history of mental illness were significantly more prone to having anxiety than were those without such a history (aOR [95% CI]: male participants aged <55 years with a family history of mental illness, 2.19 [1.02–4.67]). This significant difference was not identified in male participants aged ≥55 years. Those male participants aged ≥55 years who exercised regularly or consumed tea were significantly less prone to having anxiety than were those who did not engage in these activities (aOR [95% CI]: male participants aged ≥55 years who exercised regularly, 0.67 [0.45–1.00]; and male participants aged ≥55 years who consumed tea, 0.51 [0.32–0.82]). These significant differences were not identified in male participants aged <55 years. These results are listed in Table 4.
Table 4 Age-stratified effects of alcohol drinking and smoking behaviours on risk of anxiety in men (<55 v. ≥55 years)
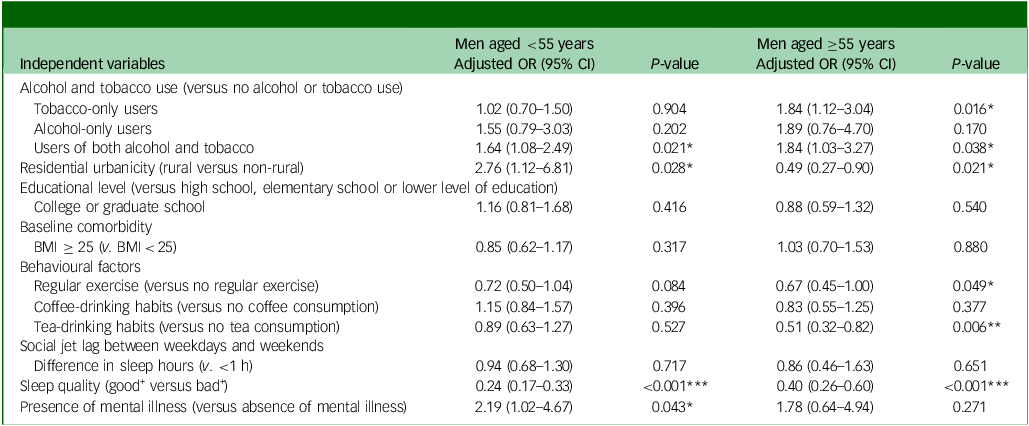
BMI, body mass index; CI, confidence interval; OR, odds ratio.
*P<0.05, **P<0.01, ***P<0.001.
Influence of tobacco and alcohol use on anxiety in women across age groups
Among female participants aged <55 years, anxiety risk was not significantly associated with the use of tobacco or alcohol or both. Among female participants aged <55 years, only the use of both tobacco and alcohol was associated with higher anxiety risk (aOR [95% CI]: 2.18 [1.24–3.85]). In both age groups, those female participants with regular exercise or good+ sleep quality were less prone to having anxiety relative to those without regular exercise or without good+ sleep quality (aOR [95% CI]: female participants aged <55 years with regular exercise, 0.77 [0.61–0.96]; female participants aged ≥55 years with regular exercise, 0.63 [0.50–0.78]; aOR [95% CI]: female participants aged <55 years with good+ sleep quality, 0.29 [0.24–0.34]; and female participants aged ≥55 years with good+ sleep quality, 0.27 [0.22–0.34]). These results are listed in Table 5.
Table 5 Age-stratified effects of alcohol drinking and smoking behaviours on risk of anxiety in women (<55 v. ≥55 years)
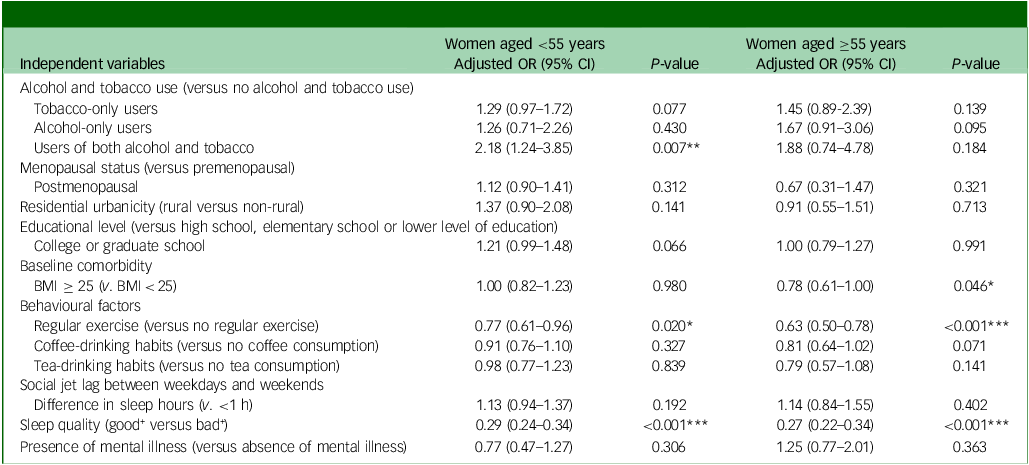
BMI, body mass index; CI, confidence interval; OR, odds ratio.
*P < 0.05, **P < 0.01, ***P < 0.001.
Discussion
We investigated the influence of tobacco and alcohol use on anxiety by analysing data retrieved from the TWB, thereby addressing several literature gaps. First, we discovered that those participants who were tobacco-only users, alcohol-only users or users of both tobacco and alcohol were more prone to having anxiety than was the reference group (those participants who were non-users of both tobacco and alcohol). Several studies have also discussed this topic. One of the most convincing hypotheses is based on the stress-coping model, which posits that individuals who experience more stress are more prone to using tobacco, alcohol or other substances as emotional regulators.Reference Weiss, Kiefer, Goncharenko, Raudales, Forkus and Schick25
Second, our sex-stratified results indicated that women were significantly more prone to having anxiety (Table 2) and that those men who were tobacco-only users, alcohol-only users or users of both tobacco and alcohol were significantly more prone to having anxiety than men who were not users. By contrast, among female participants, only those who were users of tobacco and alcohol were significantly more prone to having anxiety relative to the reference group (Table 3). Although female participants were significantly more prone to having anxiety relative to male participants, the effects of tobacco and alcohol use on anxiety were less frequently observed in the former.Reference Flensborg-Madsen, Tolstrup, Sørensen and Mortensen26 This finding may also have been due to the greater susceptibility of women to anxiety (Table 2). By contrast, male participants were more prone than female participants to using tobacco and alcohol when they experienced anxiety (Table 3). These topics are highly relevant and warrant further investigation, because the prevalence of tobacco and alcohol use among women has been increasing in Taiwan in recent years.Reference Wen, Levy, Cheng, Hsu and Tsai27,Reference Huang, Wu, Hsiao, Chen, Ting and Chen28
Third, we compared participants on the basis of age (<55 v. ≥55 years). The results indicate that older age is a protective factor against anxiety (Tables 2 and 3): that is, older participants were less prone to having anxiety. This finding is consistent with those of another study that investigated a sample of adults in the USA, and reported that the prevalence of anxiety disorders was 34.2% among individuals aged 45–59 years but significantly lower (at 17.8%) among individuals aged >60 years.Reference Mojtabai, Stuart, Hwang, Eaton, Sampson and Kessler29 Although the age grouping of that study differs from that of ours, the differences with respect to age and the tendency to develop anxiety disorders are similar.
In addition to tobacco and alcohol use, other covariates were used to adjust our statistical analysis. Covariates such as exercise habits and sleep quality were examined as potential protective factors, and our results are consistent with those of other studies. Specifically, our results suggest that regular physical exercise is a protective factor against anxiety and is associated with a lower prevalence of anxiety.Reference Ströhle30 They also suggest that regular physical exercise reduces or even treats symptoms of anxiety.Reference Ströhle30,Reference Stonerock, Hoffman, Smith and Blumenthal31 The mechanism underlying the relationship between anxiety and physical activity remains unclear. The positive and significant effect of exercise on anxiety in older adults was also reported in other studies.Reference Philippot, Dubois, Lambrechts, Grogna, Robert and Jonckheer32,Reference Wu, Zhang, Yang and Jiang33 Several studies have reported that poor sleep quality increased the odds ratio of having anxiety and various other mental disorders.Reference Kim, Kim, Jang and Park15,Reference Yu, Rawtaer, Fam, Jiang, Feng and Kua34,Reference Blake, Trinder and Allen35 In addition to alcohol and tobacco use, various studies have also identified other risk and protective factors that can modify or influence the development of depression and anxiety in adolescents.Reference Cairns, Yap, Pilkington and Jorm36,Reference Yap, Pilkington, Ryan and Jorm37 However, the evidence supporting the existence of modifiable risk factors for anxiety in adults is limited. The results of our covariate analysis suggest that interventions focused on regular exercise and sleep habits should be developed and implemented for people with anxiety.
In the present study, the risk of anxiety was considerably higher among users of tobacco or alcohol than among non-users. Although women exhibited a higher risk of anxiety than did men, the influence of alcohol and tobacco use on anxiety was greater in men than in women. Our analysis indicates that considerably fewer women use tobacco and alcohol than do men (Table 1). However, the associations of anxiety with tobacco and alcohol use in women may change because the prevalence of women using tobacco and alcohol in Taiwan has increased markedly.
Limitations
The present study adopted a cross-sectional observational design. Because physical illness records, including those related to medication use, were not documented in the database, their influence on anxiety could not be measured in our study. We analysed responses to the first two questions in PHQ-4 from the included participants to determine whether they had anxiety. Because the first two questions comprise a series of questionnaires and a scoring system designed to measure the risk of anxiety, enquiring into the presence of anxiety symptoms only, results from clinical diagnoses were not examined in the present study. Because the first two questions in PHQ-4 comprise a questionnaire and scoring system designed to assess the risk of anxiety, evaluating the presence of anxiety symptoms only, clinical diagnosis results were not examined in this study. To confirm the associations of anxiety disorders with tobacco and alcohol use, the definition of anxiety should be reconsidered. Additionally, those individuals enrolled in the TWB completed baseline questionnaires that recorded alcohol drinking and tobacco smoking only as categorical outcomes. Because we recruited individuals with baseline conditions in our study, we could not assess any potential dose–response effect or determine the effect of the number of years of alcohol or tobacco consumption.
Supplementary material
The supplementary material is available online at https://doi.org/10.1192/bjo.2025.24
Data availability
The data supporting the findings of this study are available upon reasonable request from the Taiwan Biobank (TWB). The TWB restricts public access to its data.
Acknowledgements
The purchase of data from the TWB research database was supported by a grant from Taitung MacKay Memorial Hospital, Taitung, Taiwan (grant no. TTMMH-107-07). This manuscript was edited by Wallace Academic Editing.
Author contributions
S.-J.C. proposed the concept of this study. S.-J.C. and J.C.-Y.L. were responsible for developing the methodology, collected data and provided supervision. J.C.-Y.L. analysed data. Y.-T.W. and K.-P.L. wrote the original draft of the manuscript. S.-J.C. reviewed and edited the manuscript. All authors have read and approved the final manuscript.
Funding
Funding was provided by Taitung MacKay Memorial Hospital, Taitung, Taiwan.
Declaration of interest
None.









eLetters
No eLetters have been published for this article.