Background and rationale for review
Eating disorders are relatively rare but are associated with a multitude of physiological, psychological, social and economical complications and have the highest mortality of all mental disorders.Reference Keel and Brown1–Reference Crow, Swanson, Raymond, Specker, Eckert and Mitchell3 Evidence suggests that prompt diagnosis and early intervention improves recovery prospects.Reference Zipfel, Giel, Bulik, Hay and Schmidt4 However, eating disorders are difficult to diagnose and treat.Reference Crow, Swanson, Raymond, Specker, Eckert and Mitchell3,Reference Grave5
Generally, healthcare is regarded as a partnership between patients and professionals. For eating disorders, however, this relationship can be ambivalent, with inconsistencies in healthcare.Reference Tierney, Goss and Fox6,Reference Sampson, Cooper, Barbour, Polson and Wilson7 Primary care (i.e. community-based generalist medical care) is usually the first port of call for any health-related complaint and the setting where many conditions are diagnosed and managed. Some disorders may require specialised treatment and transitions or co-management across the interface between primary and secondary (i.e. specialist) care. The coordination between different levels of care can be fraught.Reference Tierney, Goss and Fox6 For example, family physicians/general practitioners (GPs) often feel unequipped to identify and manage eating disorders and prefer to pass care to specialist services.Reference Clarke and Polimeni-Walker8 However, specialist services are often significantly under-resourced, overburdened and unable to accept high numbers of referrals. As a result, patients with eating disorders may be left untreated, facing long waiting lists, inappropriate referrals and prolonged illness, exacerbating eating disorders and decreasing the likelihood of recovery.Reference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9
In the UK, up to 1.25 million people are affected by eating disorders, yet there are relatively scarce resources available to treat them.10,11 The National Health Service (NHS) proposes to deliver better healthcare based on ‘principles and values’. English, Welsh and Scottish NHS healthcare systems all espouse principles and values for better integrated service for all patients with patient-centred, shared decision-making and better interagency working.12,13,14
Despite variation, healthcare has many similarities internationally.Reference Tierney, Goss and Fox6 Most healthcare systems face challenges of rising cost and increasing demand as quality of care improves,15 with many governments committed to improving primary–secondary transitions.Reference Mitchell, Burridge, Zhang, Donald, Scott and Dart16 Several countries successfully use similar principles and values to the UK. In New Zealand and the USA, shared partnerships and shared responsibility in treatment in distributing resources more efficiently have improved health outcomes. In the USA, more investment in primary care has successfully shifted care to out-patient clinics. In Sweden, patient-centred care is prioritised – looking at healthcare through the ‘patient's eyes’ and in the Netherlands, ‘neighbourhood care’ is optimised.15
Given the commonality of these challenges across different healthcare systems, it is important to review the current literature on eating disorder health provision at the primary–secondary care interface at an international level, to explore the facilitators and barriers existing in eating disorder healthcare, and then draw conclusions that can underpin recommendations to ensure eating disorders are diagnosed and treated in line with principles of good clinical practice.
Aims and objectives
The aim of this paper was to systematically review and thematically synthesise the current literature on the primary and secondary care healthcare interface for eating disorders. These included a range of perspectives and experiences of: individuals with eating disorders; people close to individuals with eating disorders, such as family members, loved ones and close friends; and health professionals working with eating disorders. This review was conducted to gain a better understanding and a more comprehensive account of the healthcare interface for eating disorders. To do this, data was collected from mixed methods primary studies to assess and understand a range of different experiences and perspectives and examine the facilitators to and barriers of eating disorder healthcare to provide recommendations for improvements in future research and practice.
The research questions we asked were: (a) what are the current facilitators and barriers across primary and secondary eating disorder healthcare services; and (b) what conclusions can be drawn from the international literature to improve the healthcare services for eating disorders?
Method
Search strategy and selection criteria
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews by PRISMA 2009 Checklist.Reference Moher, Liberati, Tetzlaff and Altman17 Studies were considered for inclusion for the review if they met the predetermined study eligibility checklist shown in Appendix 1. A comprehensive search of electronic databases was conducted in May to September 2017. These databases were: Web of Science, PubMed, APA PsychNET, PsycINFO, CINAHL, SCOPUS, Science Direct and Social Sciences Citation Index. No restrictions were placed on geographic location or publication date. However, language and methodological filters were applied to ensure that studies were restricted to the English language only, and study designs were primary studies only. In addition, searches also included hand-searching, scanning of reference lists and searching internet resources. All databases and other resources were searched using a combination of search keywords and terms. These included keywords relating to population groups (for example ‘patients’, ‘sufferers’, ‘people with an eating disorder’, ‘service user’; ‘family’, ‘carer’, ‘loved one’; ‘health professionals’, ‘primary’, ‘secondary’ and so on); types of eating disorders (for example ‘anorexia nervosa’, ‘bulimia nervosa’, ‘binge-eating disorder’ and so on); and types of treatment settings (for example ‘in-patient’, ‘out-patient’, ‘primary’, ‘community’, ‘GP practice’). Each search term was adapted for individual databases or other resource types as needed, matching them against titles, abstracts and subject descriptors.
Data extraction and synthesis
The retrieved studies were screened for relevance and rated against the inclusion/exclusion criteria for further consideration by two reviewers (G.J. and J.T.) using a stepwise approach, for example screening for titles and abstracts. Eligible studies were then obtained in full-text and reviewed. Data were extracted using a data extraction form developed by the reviewers. The extracted data included: study characteristics and design, lived experiences and personal perspectives of outcomes.
To analyse the data, studies were synthesised and interpreted using a qualitative narrative synthesis methodology that integrates and compares findings, by looking for themes or constructs across individual studies.Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18 This process comprised using the extracted data from all three population groups, which were then subcategorised using a thematic approach to the data to identify emerging themes, to enable exploration of people's perceptions and experiences. An interpretivist approach was applied to this synthesis to deepen understanding of the findings across the papers and go beyond the original findings to generate new constructs and explanations.Reference Snilstveit, Oliver and Vojikova19 To do this, the data was extracted and coded, that is, data was read line-by-line, and relevant data was categorised into list-form, under specific headings and subheadings. This created descriptive themes of the data, then similar codes from each additional paper were grouped together to synthesise the data in to a more analytical format to construct themes, from which dominant themes and subthemes were then created. These themes were drawn from similarities identified in the data and matched across the three participant groups. Each identified category, heading/subheading and descriptive themes, and their analytical format were double-checked and double-coded, and any discrepancies were then discussed and resolved. This process was conducted by two of the authors (G.J. and J.T.).
Quality assessment
The studies were assessed by one author (G.J.) and a proportion (20%) of these were additionally double-coded by another (J.T.). Any discrepancies were then discussed and resolved. This was assessed using an adapted version of the Critical Appraisal Skills Programme checklist for both qualitative research and randomised controlled trials.20 The checklist consisted of four subscales (10 items) reporting: aims, methods, design, recruitment, data collection, bias, ethics, analysis/testing, findings/conclusions, and value. The highest possible score was 20. A ‘good’ rating score for each subitem was allocated a score of ‘2’, ‘fair, 1’ and ‘poor, 0’. The cut-off threshold for inclusion was set relatively low (score >10) as this is a review of perspectives and experiences, not of effectiveness or quality.
Results
An initial scope of the electronic databases and the internet (such as Google scholar and Google) generated a total of 1480 papers. Of these, 1362 papers were excluded after reading the titles and abstracts, as not meeting full criteria. The remaining 118 papers were retrieved in full, after which, a further 20 papers were excluded. A data extraction and quality assessment of the remaining 98 papers was conducted, resulting in 35 papers being excluded. In total, 63 papers met the inclusion criteria for the review.Reference Tierney21–Reference Hunt and Churchill83 Table 1 provides the quality assessment scoring of the 63 selected papers and Fig. 1 provides an overview of the selection process as a flow diagram.
Table 1 Quality assessment score
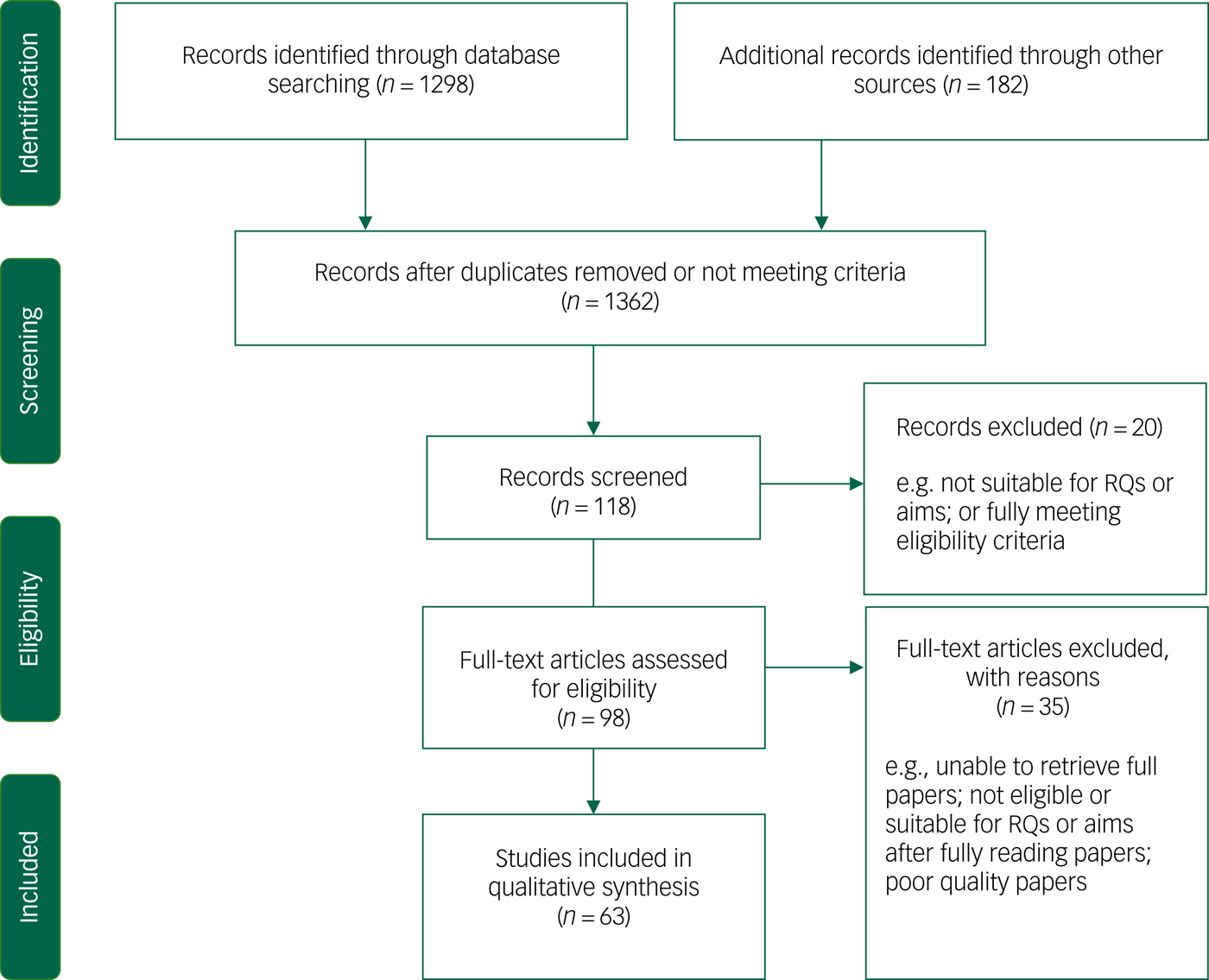
Fig. 1 Flow diagram of selection of papers.
Methodological quality and study characteristics
The quality of the included papers was considered to be good to fair. All these papers were rated highly for design, methodology, recruitment, analysis and overall value. Therefore, all 63 papers were considered of an appropriate quality for inclusion in this review.
The included papers consisted of qualitative methodologies (n = 44), including semi-structured/in-depth interviews or focus groups and quantitative methodologies (n = 24) using questionnaires or online essays (63 papers in total, but some had mixed-method approaches – n = 68 methodologies). Of the included papers, the sample size varied substantially, ranging between 5 to 1522 participants. The samples were a mix of ages and genders. The included papers were published between the years 1995 and 2016. The studies were conducted across a range of geographic locations, including the UK and Ireland (n = 20), USA and Canada (n = 18), Australia and New Zealand (n = 13), Sweden and Norway (n = 11), and Netherlands and Belgium (n = 2). The population groups of these studies included individuals with eating disorders across a range of eating disorder types and severities (n = 37), family/friends (n = 10) and health professionals (n = 21).
The settings of the included papers of individuals with eating disorders and family/friends were ‘in-patient’ (child, adolescent, adult, eating disorders and mental health) (n = 17), drop-in specialist eating disorder centres (n = 2), university centres (n = 1), out-patient (n = 8), community recruitment/in home settings (n = 8), general medical wards/hospital (n = 4), private practice (n = 1) or online resources (n = 1).
For health professionals, the reported occupations/settings included: specialist eating disorder clinicians, medical doctors and nurses (GP practice, general ward, paediatric, mental health), psychiatrists, psychologists, dieticians, obstetricians, gynaecologists, counsellors, therapists (psychiatric, occupational), social workers, health visitors, midwives, dentists and student/fellow/resident health professionals. The characteristics for each paper are outlined in supplementary Table 1 (available at https://doi.org/10.1192/bjo.2019.48).
Summary of thematic analysis
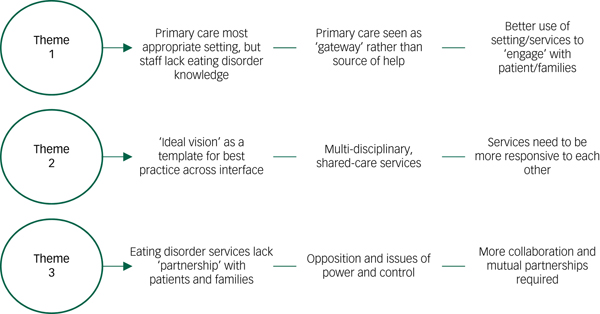
By gathering the data and comparing the types of perspectives and experiences, three dominant themes emerged from the synthesis of the studies to allow for similarities and disparities to emerge and provide a comprehensive insight into the functions and barriers of the healthcare interface for eating disorders. The dominant themes and the subthemes are outlined in detail below. Appendices 2–4 provide a summary of each theme.
Theme 1: the help-seeking process
The first dominant theme that emerged from the literature is the help-seeking process and the primary care setting. This entails two subthemes and describes the process of individuals with eating disorders and family/friends of those with eating disorders seeking professional help in primary care settings, and the professional role of the primary health professionals in this process.
Subtheme 1: the help-seeking process at its current state
Individuals with eating disorders’ perspective of barriers to care and unhelpful experiences
In the literature, individuals with eating disorders considered primary healthcare the most appropriate and opportunistic setting to diagnose eating disorders and intervene in the first instance.Reference Keel and Brown1,10,12,Reference Linville, Brown, Strum and McDougal24 Identified primary healthcare professionals included a GP/family physician or primary practice nurse,Reference Keel and Brown1,Reference Hay and Mond2,10,12,Reference Linville, Brown, Strum and McDougal24,Reference Gulliksen, Nordbo, Espeset, Skarderud and Holte32,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 social worker,Reference Keel and Brown1,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 dietician,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 counsellor or psychologist.Reference Keel and Brown1,10,12,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 However, the health professionals in primary care settings were reported as presenting challenges and difficulties at the early stages of help-seeking. Individuals with eating disorders reported lack of eating disorder experience, understanding and knowledge among primary care professionals, particularly among GPs, practice nurses and social workers.Reference Keel and Brown1,Reference Hay and Mond2,Reference Grave5,10,12,Reference Snilstveit, Oliver and Vojikova19,Reference Tierney21,Reference Robinson, Mountford and Sperlinger25 Furthermore, frequent failure to detect eating disorder symptoms and provide a timely diagnosis was described.Reference Keel and Brown1,Reference Snilstveit, Oliver and Vojikova19 For individuals with eating disorders, primary care professionals not only lacked time and resourcesReference Grave5,Reference Rosenvinge and Klusmeier30 to diagnose and treat eating disorders, but were also ‘uninterested’ in eating disorders, believing it is simply a matter of ‘just eating’,Reference Robinson, Mountford and Sperlinger25 or focused on physical symptoms of an eating disorders.Reference Snilstveit, Oliver and Vojikova19,Reference Robinson, Mountford and Sperlinger25 In consequence, diagnosis of an eating disorders often only occurred when physical symptoms became severe and pronounced.Reference Keel and Brown1,Reference Snilstveit, Oliver and Vojikova19,Reference Robinson, Mountford and Sperlinger25 However, even in severe cases, long waiting lists and a lack of resources with no guarantee of admission and treatment by more specialised services for eating disorders were major barriers.Reference Keel and Brown1,Reference Hay and Mond2,Reference Grave5,Reference Snilstveit, Oliver and Vojikova19,Reference Tierney21,Reference Robinson, Mountford and Sperlinger25,Reference Rosenvinge and Klusmeier30 For individuals with eating disorders, the primary care service was described as an ‘obstacle’ or ‘barrier’Reference Keel and Brown1,Reference Snilstveit, Oliver and Vojikova19,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 to care, rather than the first port of call or effective ‘gate-keepers’ to specialist services.Reference Snilstveit, Oliver and Vojikova19
Family/friends’ perspective of barriers to care and unhelpful experiences
Likewise, for family/friends of individuals with eating disorders, help-seeking was initially sought in primary care or community settings such as GP practices and schools,Reference Federici and Kaplan36,Reference Fox and Diab37,Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38,Reference Pettersen and Rosenvinge42 but self-help books, internet resources, support-based organisations or private treatment were where most of the ‘useful help’ was located.Reference Federici and Kaplan36,Reference Fox and Diab37 For some family/friends, primary health professionals were helpfulReference Fox and Diab37,Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38,Reference Escobar-Koch, Banker, Crow, Ringwood, Smith and Furth39,Reference Swain-Campbell, Surgenor and Snell40 in terms of providing ‘active support’, without blame or judgement.Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38 Some described ‘thorough and competent’ primary care professionals.Reference Escobar-Koch, Banker, Crow, Ringwood, Smith and Furth39 However, others found primary care a negative experience,Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38 feeling ‘fobbed off’.Reference Swain-Campbell, Surgenor and Snell40 They reported that primary care professionals lacked eating disorder knowledgeReference Fox and Diab37,Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38,Reference Escobar-Koch, Banker, Crow, Ringwood, Smith and Furth39 and the training required to diagnose and respond to eating disorders.Reference Pettersen and Rosenvinge42 They did not provide clear adviceReference Escobar-Koch, Banker, Crow, Ringwood, Smith and Furth39 or provide essential management of eating disorders.Reference Fox and Diab37,Reference Pettersen and Rosenvinge42 Knowledge of available treatment optionsReference Fox and Diab37,Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38 and the ability to negotiate with other healthcare systems to get access to referrals was poor.Reference Federici and Kaplan36,Reference Fox and Diab37,Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38,Reference Pettersen and Rosenvinge42 This caused ‘frustration and anger’Reference Smith, Chouliara, Morris, Collin, Power and Yellowlees38 and ‘resentment’ towards the professionals.Reference Federici and Kaplan36 The process of help-seeking was described as a ‘long arduous journey’ by family/friends,Reference Federici and Kaplan36 and some described how their own resourcefulness and inexhaustible search for help ultimately helped the person with an eating disorder obtain the treatment they need – which is about being ‘not prepared to give up’ and do ‘whatever is necessary to aid recovery’.Reference Federici and Kaplan36
Healthcare professionals’ perspective of barriers to care and unhelpful experiences
Professionals in primary care settings (for example GP practices, general wards, student/resident placements) described their professional role regarding eating disorders as a ‘double-bind’.Reference Reid, Williams and Burr63 They faced challenges and difficulties with individuals with eating disorders, their families and the eating disorder healthcare interface itself. Primary care professionals argued that individuals with eating disorders are difficult and challengingReference Reid, Williams and Burr63 and create tension between all parties.Reference Reid, Williams and Burr63 They felt that people with eating disorders often lack motivation and adherence with treatment, with much of the drive for help-seeking and recovery coming from the families.Reference Grange and Gelman43,Reference Paulson-Karlsson and Nevonen46,Reference Colton and Pistrang47,Reference Zaitsoff, Pullmer, Menna and Geller48,Reference Offord, Turner and Cooper49,Reference Reid, Williams and Burr63 Therefore, some primary care professionals were reluctant to work with eating disorders,Reference Clinton, Bjork, Sohlberg and Norring51 with expressions of ‘frustration’,Reference Paulson-Karlsson and Nevonen46,Reference Zaitsoff, Pullmer, Menna and Geller48 ‘resentment’Reference Walker and Lloyd45 and ‘irritability and disgust’ in the physical comorbidities,Reference Walker and Lloyd45,Reference Colton and Pistrang47 considering eating disorders as being ‘low prestige’ compared with other illnesses,Reference Walker and Lloyd45 with some stating they ‘don't like’ or ‘don't want to work with them’.Reference Paulson-Karlsson and Nevonen46,Reference McMaster, Beale, Hillege and Nagy56 Other primary care professionals indicated that they just ‘don't’, or ‘don't want’ to screen for eating disorders,Reference Paulson-Karlsson and Nevonen46,Reference Offord, Turner and Cooper49,Reference Roots, Rowlands and Gowers55,Reference Winn, Perkins, Murray, Murphy and Schmidt57 as they find them time consuming or too complex,Reference Grange and Gelman43,Reference Paulson-Karlsson and Nevonen46,Reference Colton and Pistrang47,Reference Offord, Turner and Cooper49,Reference Rance, Moller and Clarke50,Reference Clinton, Bjork, Sohlberg and Norring51 or just preferred to diagnose eating disorders rather than manage their care and treatment.Reference Colton and Pistrang47,Reference Evans, Hat, Mond, Paxton, Quirk and Rodgers53,Reference Tierney60 Yet others were frustrated they ‘can't work’ with eating disorders,Reference Grange and Gelman43,Reference Walker and Lloyd45 expressing a wish to be trained in eating disorders, because their role in detecting eating disorders symptoms was important.Reference Roots, Rowlands and Gowers55,Reference Winn, Perkins, Murray, Murphy and Schmidt57
Primary care professionals saw the lack of training and resources in eating disorders as a barrierReference Grange and Gelman43 and felt that frustration caused negative attitudes that then impeded therapeutic relationships.Reference Grange and Gelman43 It was widely recommended that a well-validated universal screening protocol for eating disorders would build confidence in primary care settings.Reference Offord, Turner and Cooper49,Reference Rance, Moller and Clarke50,Reference Evans, Hat, Mond, Paxton, Quirk and Rodgers53,Reference Roots, Rowlands and Gowers55
Primary care professionals insisted that the challenges of working with eating disorders and professional negative attitudes were associated with ‘clinical’ problemsReference Lindstedt, Neander and Gustafsson44 such as feeling unequipped to diagnose and intervene with eating disordersReference Rance, Moller and Clarke50,Reference Winn, Perkins, Murray, Murphy and Schmidt57 because of a lack of eating disorder experience,Reference Grange and Gelman43,Reference Bannatyne and Stapleton65,Reference McMaster, Beale, Hillege and Nagy56,Reference McCormack and McCann58,Reference Reid, Williams and Burr63 knowledge/understanding,Reference Grange and Gelman43,Reference Lindstedt, Neander and Gustafsson44,Reference Offord, Turner and Cooper49,Reference McMaster, Beale, Hillege and Nagy56 and adequate training and skills.Reference Grange and Gelman43,Reference Walker and Lloyd45,Reference Colton and Pistrang47,Reference Offord, Turner and Cooper49,Reference Rance, Moller and Clarke50,Reference Clinton, Bjork, Sohlberg and Norring51,Reference Tierney60 They identified larger-scale ‘organisational’ problemsReference Clinton, Bjork, Sohlberg and Norring51 that eating disorders are considered specialist disorders and requiring specialised care.Reference Grange and Gelman43 However, they recognised that specialist care referrals are often unavailable or unobtainable;Reference Grange and Gelman43,Reference Colton and Pistrang47,Reference Offord, Turner and Cooper49 thus, primary care professionals were faced with challenges of trying to make referrals to inaccessible specialist treatment.Reference Offord, Turner and Cooper49,Reference Roots, Rowlands and Gowers55,Reference Reid, Williams and Burr63
Subtheme 2: utilising the primary care setting
In the literature, individuals with eating disorders suggested that the early stages of contact with a primary care professional needs to be a ‘positive experience’12 and this is greatly influenced by two factors. First, they expected sufficient knowledge of eating disorders and good interpersonal skills among primary care professionals.12 Second, they expected sensitivity regarding eating disorder ‘control’.Reference Keel and Brown1,12,14,Reference Gulliksen, Nordbo, Espeset, Skarderud and Holte32 For individuals with eating disorders, anxiety, ambivalence and resistance to treatment and/or help-seeking are often grounded in a fear of ‘losing personal control’.12,Reference Gulliksen, Nordbo, Espeset, Skarderud and Holte32 Because individuals with eating disorders often approached help-seeking with mixed feelings and motives, they felt that the professionals should emphasise ‘facilitating positive reactions’, encouraging individuals with eating disorders to speak openly rather than attempting to change behaviours and fix the eating disorder.12,Reference Gulliksen, Nordbo, Espeset, Skarderud and Holte32,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 This would allow individuals with eating disorders to feel they are in good hands, yet ‘feel safe and listened to’12 and able to sustain some personal control and the ability to take responsibility for their own actions.12,14,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 For individuals with eating disorders, this was a crucial point early in the help-seeking, which was necessary to enable them to be ready to change and seek recovery – a ‘testing the waters’Reference Gulliksen, Nordbo, Espeset, Skarderud and Holte32 or a tentative ‘action stage’ in eating disorder treatment.12,14,Reference Mitchell, Burridge, Zhang, Donald, Scott and Dart16,Reference Rie, Noordenbos, Donker and Furth22,Reference Linville, Brown, Strum and McDougal24 Being an active agent throughout treatment and into recovery was described in the literature as ‘turning points’ and success stories were described as ‘internal motivation’ or ‘want(ing)’ help,Reference Keel and Brown1,Reference Zipfel, Giel, Bulik, Hay and Schmidt4,Reference Mitchell, Burridge, Zhang, Donald, Scott and Dart16,Reference Rie, Noordenbos, Donker and Furth22,Reference Clinton, Almlof, Lindstrom, Manneberg and Vestin23,Reference Sheridan and McArdle27,Reference Halvorsen and Heyerdahl54 which depended greatly on ‘timing’ and being in the right place at the right time.12,Reference Rie, Noordenbos, Donker and Furth22,Reference Linville, Brown, Strum and McDougal24 Therefore, a therapeutic approach was crucial at earlier stages of help-seeking in primary care, because if ‘positive perceptions at help-seeking are formed as a result of this initial attempt, then future treatments were more effective in altering disordered eating behaviours’.Reference Gulliksen, Nordbo, Espeset, Skarderud and Holte32
Despite difficulties, studies suggested efforts were needed to better utilise the primary care setting as an opportunity to encourage the ‘action’ stage from individuals with eating disorders by providing supportive and therapeutic relationships14,Reference Mitchell, Burridge, Zhang, Donald, Scott and Dart16,Reference Rie, Noordenbos, Donker and Furth22 and offering a sense of safety, commitment and validation11 while maintaining a mutual relationship among all parties as mutual ‘agents of change’.Reference Federici and Kaplan36,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 Primary care professionals could potentially help turn the first highly ambivalent consultation into a positive experience or successful turning point.12 A successful first encounter at primary care was described as a potential ‘powerful catalyst’ enable further treatment of and recovery from eating disorders.14 Appendix 2 outlines the key points from theme 1.
Theme 2: expectations of care and appropriate referrals
The second dominant theme is the ‘expectations of care and appropriate referrals’. This theme entails two subthemes. This looks at the ‘ideal’, and the functions and barriers surrounding the assumed ‘best’ eating disorder service.
Ideal characteristics of care and treatment
Individuals with eating disorders and their family/friends said ‘one professional’ could make a real difference in eating disorder care and treatment.Reference Halvorsen and Heyerdahl54 This ‘good’ professional, regardless of whether they belonged to primary or secondary care services, was characterised as someone they can trust,Reference Sheridan and McArdle27,Reference Rosenvinge and Klusmeier30 and build a strong therapeutic relationship with,Reference Sampson, Cooper, Barbour, Polson and Wilson7,15,Reference Rie, Noordenbos, Donker and Furth22,Reference Linville, Brown, Strum and McDougal24,Reference Robinson, Mountford and Sperlinger25,Reference Boughtwood and Halse28,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 who is respectful and empathic.Reference Keel and Brown1,Reference Hay and Mond2,Reference Grave5,Reference Sampson, Cooper, Barbour, Polson and Wilson7,11,13,15,Reference Moher, Liberati, Tetzlaff and Altman17,Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Snilstveit, Oliver and Vojikova19,Reference Rie, Noordenbos, Donker and Furth22,Reference Robinson, Mountford and Sperlinger25,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 This ‘good professional’ needed to be available and consistentReference Sampson, Cooper, Barbour, Polson and Wilson7,13,15,Reference Rie, Noordenbos, Donker and Furth22 and have a sufficient understanding,Reference Grave5,11,12,13,Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Snilstveit, Oliver and Vojikova19,Reference Tierney21,Reference Clinton, Almlof, Lindstrom, Manneberg and Vestin23,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 knowledge and experience of eating disorders.Reference Keel and Brown1,Reference Clarke and Polimeni-Walker8,Reference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9,12,13,Reference Rie, Noordenbos, Donker and Furth22,Reference Robinson, Mountford and Sperlinger25,Reference Bravender, Elkus and Lange26 The ideal setting for this treatment to take place was in a safe and supportive environment – somewhere that feels ‘like home’,Reference Sampson, Cooper, Barbour, Polson and Wilson7,11,13,15,Reference Tierney21,Reference Rie, Noordenbos, Donker and Furth22,Reference Clinton, Almlof, Lindstrom, Manneberg and Vestin23,Reference Sheridan and McArdle27,Reference Boughtwood and Halse28,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29 considers the individual with eating disorders as a ‘whole person’,Reference Sampson, Cooper, Barbour, Polson and Wilson7,Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Snilstveit, Oliver and Vojikova19,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29 and offers a ‘collaborative’ approach to treatmentReference Sampson, Cooper, Barbour, Polson and Wilson7,Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Snilstveit, Oliver and Vojikova19,Reference Tierney21,Reference Linville, Brown, Strum and McDougal24,Reference Bravender, Elkus and Lange26,Reference Sheridan and McArdle27,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 that is ‘individualised and client-focused’Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Snilstveit, Oliver and Vojikova19,Reference Tierney21,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29 offering consultative and directional care.Reference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9,11,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33
At the same time, the ‘good professional’ needed to remain authoritative, reflecting confidence and professionalism13 and setting meaningful and appropriate treatment goals.Reference Moher, Liberati, Tetzlaff and Altman17,Reference Boughtwood and Halse28 It is suggested that a combination of ‘autonomy and direction’ equals ‘balance and success’ in eating disorder treatment.11 Some professionals also supported this ideal system, suggesting that although eating disorder experience, skill and knowledge are important in the treatment of eating disorders, building strong relationships with individuals with eating disorders and their family/friends, and delivering care holistically can have a greater impact of helpfulness than any type of treatment provided.Reference Grange and Gelman43,Reference Honey, Boughtwood, Clarke, Kohn and Madden59,Reference Cohn61,Reference Haigh and Treasure62
Specialised and/or complex? – So, who's responsible for eating disorders?
One of the issues raised by non-eating disorder specialists was that eating disorders is both specialised and complex in nature.Reference Honey, Boughtwood, Clarke, Kohn and Madden59,Reference Cohn61 Eating disorders are considered ‘rare, chronic and require intense care, high levels of treatment and high demand from HPs [health professionals]’.Reference Grange and Gelman43 Yet, it was regularly argued that eating disorder treatment should reflect its specialist need, and the best place for individuals with eating disorders is in specialist careReference Grange and Gelman43 that provides the time and expertiseReference Grange and Gelman43,Reference Cohn61 to build supportive relationships. Similarly, individuals with eating disorders and their family/friends perceived specialist eating disorder care as the ‘best’ or ‘better’ treatment for eating disorders,Reference Tierney, Goss and Fox6,Reference Sampson, Cooper, Barbour, Polson and Wilson7,10,Reference Moher, Liberati, Tetzlaff and Altman17,Reference Snilstveit, Oliver and Vojikova19,Reference Linville, Brown, Strum and McDougal24,Reference Nilsson and Hagglof34,Reference Zugai, Stein-Parbury and Roche35,Reference Fox and Diab37,Reference Grange and Gelman43 providing better understanding and knowledge of eating disorders,Reference Hay and Mond2,Reference Crow, Swanson, Raymond, Specker, Eckert and Mitchell3,Reference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9, 20,Reference Robinson, Mountford and Sperlinger25,Reference Grange and Gelman43 empathyReference Crow, Swanson, Raymond, Specker, Eckert and Mitchell3,Reference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9,Reference Robinson, Mountford and Sperlinger25 and personal recognition.Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18 Unsurprisingly, many non-specialist health professionals felt that they ‘should’ or ‘would rather’ refer individuals with eating disorders on to these services,Reference Grange and Gelman43,Reference Roots, Rowlands and Gowers55,Reference Winn, Perkins, Murray, Murphy and Schmidt57 and many individuals with eating disorders and their family/friends wanted this ‘best’ treatment too.Reference Tierney, Goss and Fox6,Reference Sampson, Cooper, Barbour, Polson and Wilson7,10,Reference Moher, Liberati, Tetzlaff and Altman17,Reference Snilstveit, Oliver and Vojikova19,Reference Linville, Brown, Strum and McDougal24,Reference Nilsson and Hagglof34,Reference Zugai, Stein-Parbury and Roche35,Reference Fox and Diab37,Reference Grange and Gelman43
However, ‘referring on’ often was to under-resourced specialist service struggling to respond to demand.Reference Snilstveit, Oliver and Vojikova19,Reference Robinson, Mountford and Sperlinger25,Reference Zugai, Stein-Parbury and Roche35,Reference Grange and Gelman43 Eating disorder services created limited access,Reference Tierney21,Reference Rosenvinge and Klusmeier30,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 geographical barriers,Reference Tierney21 long waiting lists and delays,Reference Keel and Brown1,Reference Snilstveit, Oliver and Vojikova19,Reference Tierney21,Reference Rosenvinge and Klusmeier30 rigid admission rules based on single treatment modalities and eating disorder physical traits.Reference Tierney21,Reference Robinson, Mountford and Sperlinger25,Reference Rosenvinge and Klusmeier30,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 Lower body mass indexes took priority,Reference Bravender, Elkus and Lange26,Reference Rosenvinge and Klusmeier30 and referrals were only accepted for very serious cases.Reference Keel and Brown1,Reference Tierney, Goss and Fox6,Reference Tierney21,Reference Robinson, Mountford and Sperlinger25,Reference Rosenvinge and Klusmeier30 Furthermore, specialist eating disorder care provided no guarantee of treatment even after gaining access,Reference Rosenvinge and Klusmeier30 with the risk of losing a place if another patient took priorityReference Robinson, Mountford and Sperlinger25,Reference Rosenvinge and Klusmeier30 and immediate discharge occurring after weight restoration, with little if any aftercare.Reference Rosenvinge and Klusmeier30
Eating disorders requires a multidisciplinary approach and team involved, including a range of primary and secondary care professionals,Reference Grange and Gelman43,Reference Evans, Hat, Mond, Paxton, Quirk and Rodgers53,Reference Cohn61 with the inclusion of families.Reference Evans, Hat, Mond, Paxton, Quirk and Rodgers53 However, this multidisciplinary model could suffer misconceptions, such as the assumption of professionals that ‘some treatment is better than none’.Reference Grange and Gelman43
Out-patient care10,11,Reference Zugai, Stein-Parbury and Roche35 was favoured by some individuals with eating disorders as allowing a consultative and collaborative approach to treatment control,11 and when delivered by a professional with sufficient eating disorder expertise, family/friends tended to feel that out-patient care is the most beneficial, compared with any other treatment.Reference Zugai, Stein-Parbury and Roche35 To others, out-patient treatment was an unsuccessful, unsuitable or unskilled option.Reference Hay and Mond2,Reference Moher, Liberati, Tetzlaff and Altman17
Medical general ward admissions were reported by all professionals, individuals with eating disorders and families as the most negative setting for eating disorders and the ‘most inappropriate location’, ‘unsuitable and unhelpful’ for individuals with eating disorders, making them feel isolated and treated by general ward staff who lacked skill and specialist eating disorder knowledge.Reference Keel and Brown1,Reference Hay and Mond2,Reference Zipfel, Giel, Bulik, Hay and Schmidt4,Reference Sampson, Cooper, Barbour, Polson and Wilson7,Reference Moher, Liberati, Tetzlaff and Altman17,Reference Nilsson and Hagglof34,Reference Swain-Campbell, Surgenor and Snell40,Reference Grange and Gelman43,Reference Zaitsoff, Pullmer, Menna and Geller48 Professionals working on these medical general wards reported difficulties delivering care to individuals with eating disorders because of their ‘deceitful and non-compliant’ personalitiesReference Zaitsoff, Pullmer, Menna and Geller48 and reported a ‘struggle to understand the complex disorder’Reference Honey, Boughtwood, Clarke, Kohn and Madden59 that challenged their nursing values, often causing more harm than good to the patients with eating disorders.Reference Zaitsoff, Pullmer, Menna and Geller48,Reference Honey, Boughtwood, Clarke, Kohn and Madden59
Overall, specialist eating disorder care was considered the gold standard in eating disorder treatment. Unfortunately, this was not only often unobtainable, but emphasis as a ‘best’ care ultimately undermined other agencies, treating them as mere stepping stones to specialised services rather than potentially beneficial alternatives. It appeared to be the characteristics and techniques used – collaborative and patient-centred care that is knowledgeable yet sensitive to issues of control and ambivalence – that determined positive outcomes. Appendix 3 outlines the key points from theme 2.
Theme 3: collaboration versus opposition
The third theme that emerged in the data is collaboration versus opposition in the treatment of eating disorders. This theme had two subthemes. Healthcare should be a partnership between the patient, families and the health professional.Reference Tierney, Goss and Fox6,Reference Clarke and Polimeni-Walker8,13,14,Reference Nilsson and Hagglof34,Reference Honey, Boughtwood, Clarke, Kohn and Madden59 However, in the case of eating disorders, a shared partnership in healthcare can often be lacking, with hostility and opposition, the misuse of power relations and a lack of collaborative care.Reference Hay and Mond2,Reference Tierney, Goss and Fox6,Reference Sampson, Cooper, Barbour, Polson and Wilson7,Reference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9,11,13,Reference Honey, Boughtwood, Clarke, Kohn and Madden59
The weight versus well-being paradigm
Perceived oppositions between the physical and emotional aspects of eating disorder treatment and recovery were identified. There is an opposition between the ‘rarity’ and ‘recovery’ aspects of eating disorders, as the prospect of recovery from eating disorders is often unknown, underestimated or overestimated among health professionals.Reference Lindstedt, Neander and Gustafsson44,Reference Offord, Turner and Cooper49,Reference Evans, Hat, Mond, Paxton, Quirk and Rodgers53,Reference McMaster, Beale, Hillege and Nagy56 Anorexia nervosa was sometimes viewed as chronic with no recovery prospectsReference Lindstedt, Neander and Gustafsson44,Reference Offord, Turner and Cooper49,Reference Schoen, Lee, Skow, Greenberg, Bell and Wiese52,Reference McMaster, Beale, Hillege and Nagy56 whereas the prevalence and severity of bulimia nervosa was greatly underestimated.Reference Lindstedt, Neander and Gustafsson44,Reference Offord, Turner and Cooper49,Reference Evans, Hat, Mond, Paxton, Quirk and Rodgers53 In contrast, for individuals with eating disorders and their family/friends, the expectation of recovery drove help-seeking and treatment.Reference Keel and Brown1,14,Reference Mitchell, Burridge, Zhang, Donald, Scott and Dart16
Another opposition occurred between the professional and family members focusing on the ‘visible signs of eating disorders’ seeing physical status as the most valuable measure of treatment and recoveryReference Zipfel, Giel, Bulik, Hay and Schmidt4,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29 as compared with individuals with eating disorders focusing on psychological markers such as improved ‘well-being’ and feeling ‘normal’.Reference Keel and Brown1,Reference Clarke and Polimeni-Walker8,Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18 ,20,Reference Clinton, Almlof, Lindstrom, Manneberg and Vestin23,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29,Reference Rosenvinge and Klusmeier30 Overall, this lack of clarity resulted in a weight versus well-being paradigm and constituted a considerable barrier at the eating disorder healthcare interface frequently described by individuals with eating disorders and their family/friends as ‘too much focus on food and weight’,Reference Keel and Brown1,Reference Hay and Mond2,Reference Zipfel, Giel, Bulik, Hay and Schmidt4,Reference Sampson, Cooper, Barbour, Polson and Wilson7,15,Reference Snilstveit, Oliver and Vojikova19,Reference Clinton, Almlof, Lindstrom, Manneberg and Vestin23,Reference Robinson, Mountford and Sperlinger25,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29,Reference Rosenvinge and Klusmeier30,Reference Zugai, Stein-Parbury and Roche35,Reference Swain-Campbell, Surgenor and Snell40 reported in both primary and secondary care.Reference Rosenvinge and Klusmeier30 There is further conflation of completion of treatment with recovery,Reference Schoen, Lee, Skow, Greenberg, Bell and Wiese52,Reference Halvorsen and Heyerdahl54 with professionals measuring outcomes based on ‘completion’ of treatment, whereas individuals with eating disorders felt recovery should be based on ‘doing well’.Reference Evans, Hat, Mond, Paxton, Quirk and Rodgers53
Power relations versus collaboration
Oppositions existing within the weight versus well-being paradigm were also reported as part of a ‘power system’Reference Zipfel, Giel, Bulik, Hay and Schmidt4,Reference Clarke and Polimeni-Walker8,Reference Rosenvinge and Klusmeier30 throughout the eating disorder pathway, to the detriment of good practice.Reference Clarke and Polimeni-Walker8 Early in help-seeking and diagnosis, the overemphasis on ‘weight and food’ triggered a ‘drive’, because to ‘eat less food and lose more weight’ won individuals priority for treatment in specialist eating disorder services.Reference Rosenvinge and Klusmeier30 However, once entry was gained to eating disorder services, opposition between individuals with eating disorders and professionals continued, with healthcare professionals (for example secondary care staff in an in-patient unit) attempting to ‘hold all the power’.Reference Zipfel, Giel, Bulik, Hay and Schmidt4 Some in-patient units used ‘reward systems’ based on penalties and privileges,Reference Clarke and Polimeni-Walker8,15,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 making individuals with eating disorders feel that professionals ‘take all the power’.15
For some individuals with eating disorders, specialist eating disorder treatment was considered ineffective as this undermined engagementReference Zipfel, Giel, Bulik, Hay and Schmidt4,Reference Sampson, Cooper, Barbour, Polson and Wilson7 leaving them disempoweredReference Zipfel, Giel, Bulik, Hay and Schmidt4 distressedReference Keel and Brown1,Reference Moher, Liberati, Tetzlaff and Altman17,Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Robinson, Mountford and Sperlinger25,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29 and patronised,Reference Sampson, Cooper, Barbour, Polson and Wilson7,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 in a system that was too restrictive, structured and strict.Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Tierney21,Reference Clinton, Almlof, Lindstrom, Manneberg and Vestin23 This resulted in loss of personal control, identity and normality.Reference Keel and Brown1,Reference Hay and Mond2,Reference Sampson, Cooper, Barbour, Polson and Wilson7,Reference Clarke and Polimeni-Walker8,15,Reference Moher, Liberati, Tetzlaff and Altman17,Reference Snilstveit, Oliver and Vojikova19 Some individuals with eating disorders described these battles as triggering power systems, where rigid rules and unfair power relations forced individuals with eating disorders to become rebellious or deceitful, compelling them to ‘put on an act’Reference Clinton, Almlof, Lindstrom, Manneberg and Vestin23 as the ‘perfect patient’Reference Clarke and Polimeni-Walker8 to comply, resulting in an opposing identity of the rebel.Reference Sheridan and McArdle27 This is reported as being detrimental to the health and recovery of the person with eating disordersReference Clinton, Almlof, Lindstrom, Manneberg and Vestin23,Reference Sheridan and McArdle27 as it entrenched eating disorder symptoms and increased vulnerability.Reference Moher, Liberati, Tetzlaff and Altman17,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29 For other individuals with eating disorders, restrictive treatment could be a ‘safe haven’.Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18 The loss of control and normality were considered positiveReference Keel and Brown1,Reference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9,15,Reference Moher, Liberati, Tetzlaff and Altman17,Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18 because it helped set boundaries and relinquish control,15,Reference Gulliksen, Epeset, Nordbo, Skarderud, Geller and Holte33 relieving individuals of responsibility and allowing them to regain control ‘elsewhere’ as treatment progresses.Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18 However, regaining control was problematic after discharge, especially if there was little aftercare.15,Reference Mitchell, Burridge, Zhang, Donald, Scott and Dart16,Reference Moher, Liberati, Tetzlaff and Altman17,Reference van Ommen, Meerwijk, Kars, Elburg and Meijel29
Professionals (for example secondary care staff in an in-patient unit) felt that too much authoritative control in the eating disorder treatment settings caused considerable stress for people with eating disorders and their familiesReference Haigh and Treasure62 and obstructed trusting relationships, causing rebellious outbursts among those with eating disorders.Reference Honey, Boughtwood, Clarke, Kohn and Madden59 For professionals, judiciously managing control was crucial,Reference Honey, Boughtwood, Clarke, Kohn and Madden59,Reference Haigh and Treasure62 without ‘enforcing’ it and triggering ‘power in play’ between the patient with eating disorders and professionals with resultant ‘mutual mistrust’.Reference Zaitsoff, Pullmer, Menna and Geller48,Reference Honey, Boughtwood, Clarke, Kohn and Madden59 Family and friends of individuals with eating disorders reflected that shifting their role in the home ‘from power and authority to one of support and encouragement’ improved outcomes.Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 Family and friends felt all sides should work together as a teamReference Federici and Kaplan36 ‘on the same page’,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 with all affected by eating disorders mutually involved in treatment and the recovery process.Reference Federici and Kaplan36,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 Therefore, it was important to not remove all control and power from those affected by eating disorders11 and professionals should adopt directional not authoritative stancesReference Waller, Schmidt, Treasure, Marray, Aleyna and Emanuelli9 and be firm yet consistent.15 In eating disorders, if power relations were distributed more fairly in the eating disorder care setting, the ultimate wish of all parties for more room for greater collaboration in eating disorder treatment would result.Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers18,Reference Tierney21,Reference Escobar-Koch, Banker, Crow, Ringwood, Smith and Furth39,Reference Dimitropoulos, Toulany, Herschman, Kovacs, Steinegger and Bardsley41 Appendix 4 outlines the key points from theme 3.
Figure 2 outlines the key points in a diagram format of the three dominant themes and their additional subthemes
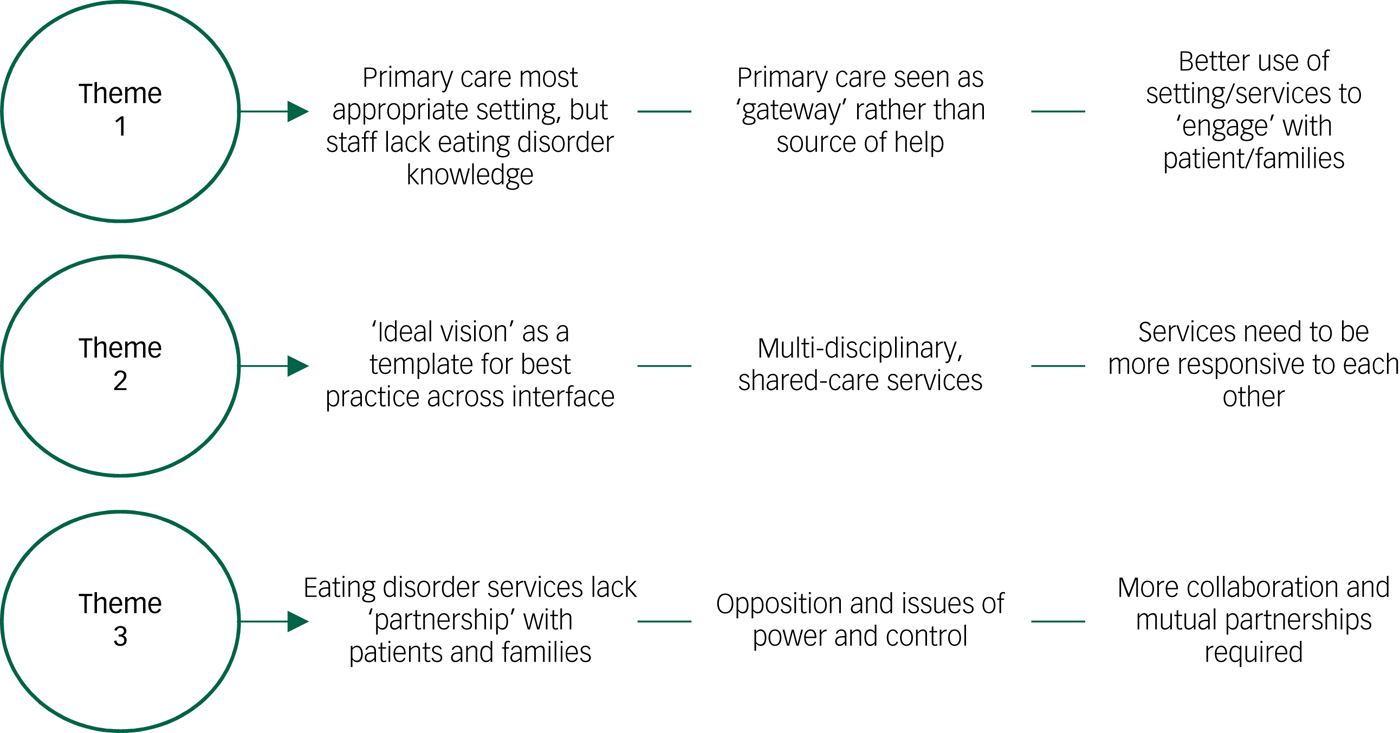
Fig. 2 Summary of themes.
Discussion
Main findings
This review provides an overview of the facilitators and barriers existing at the current eating disorder healthcare interface from a range of perspectives and experiences. Overall, the initial blame and responsibility for existing barriers tends to fall on professionals in primary care. Many individuals with eating disorders and their families/friends view primary care as a gateway to access more specialised services, rather than seeing primary care professionals as sources of help for eating disorders. However, for primary care professionals this acts as a double-bind as they are variously held responsible by all parties for failing to be knowledgeable, treating insufficiently or referring on too readily or inappropriately, reducing their sense of professional competency. In summary, primary care professionals would benefit from more understanding of the needs of both individuals with eating disorders and their families/friends, and how to neither over- nor under-refer. The analysis suggests that rather than just being a gateway to specialist care, primary care professionals can and should play a crucial role in engaging ambivalent in individuals with eating disorders while supporting and advising families/friends in promoting recovery.
It may be important to challenge the gold-standard expectation attached to specialist eating disorder care, as its current status in the eyes of individuals with eating disorders, their families and health professionals as the ‘best’ ultimately undermines all other services, dismissing primary care as a mere conduit, when it could potentially be a better alternative for some. This would require more training and support for primary care professionals to address their anxieties and difficulties in diagnosing, treating and supporting people with eating disorders. Specialist services need to be more responsive to primary care and improve shared care across the primary–secondary care interface for eating disorders. For example, as previously discussed in the background section of this paper, GPs in particular currently feel unequipped to identify and manage an eating disorder and prefer to pass the patient on to specialist services.Reference Clarke and Polimeni-Walker8 But, as this review suggests, if primary care were better supported by specialist services, they would feel more confident in their professional ability to work with patients with eating disorders.
The review suggests a complex function of the primary–secondary interface found in current eating disorder healthcare. This review adds to the knowledge-base and provides recommendations for moving forward in research and practice, these are in line with the generally accepted principles and values to deliver a better integrated service for all with shared partnerships and mutual responsibility.
The tensions identified in the final theme of collaboration versus opposition in the treatment of eating disorders are familiar. What is less familiar is the exploration of how this has an impact on the primary–secondary healthcare interface. The issues of power differentials and use of authority and control has ramifications when patients are discharged before they wish to be, or when medical responsibility is handed back to primary care. It is not clear in this review how the alterations in balance between collaboration and authoritativeness or emphases on weight versus well-being are negotiated between specialist and primary care professionals, and this is an area for further research.
The geographic locations of the included papers were higher-income countries; it would be important to examine middle- or lower-income countries in future research. Furthermore, despite a 20-year publication range, there was consistency of themes across all papers, which suggests that little has been done in the past two decades to address these reported problems. Therefore, work is needed to address difficulties with the primary–secondary care interface for eating disorder services.
Recommendations for an improved eating disorder service
Based on our research our recommendations are as follows.
(a) More training and support for professionals is needed across the interface, especially in primary care settings to address the anxieties and difficulties in diagnosing and treating eating disorders.
(b) Primary care professionals would benefit from more understanding of the needs of both individuals with eating disorders and family/friends, and how to neither over- nor under-refer.
(c) While being a gateway to specialist care, primary care professionals need to better engage with and support individuals with eating disorders and their families/friends between waiting times and referrals.
(d) It may be important to challenge the gold-standard ‘best’ expectation that is attached to specialist eating disorder care, as it may be undermining other services.
(e) The ‘ideal’ vision of an eating disorder professional, setting and technique may be someone/something that can be used as a ‘good practice’ template.
(f) It is important to link up services across the interface, adopting a multidisciplinary, shared-care approach.
(g) This ‘linked up’ approach would require services across the interface to be more responsive to each other and upskill a range of professionals to fit the ‘ideal’ and ‘best’ care vision of services.
(h) More collaborative understanding of eating disorders and mutual partnerships is needed across the primary–secondary interface to avoid the use of power and control, resulting in hostility and mistrust between partnerships.
(i) More research is needed in this area to address the difficulties and challenges within the primary–secondary interface for eating disorder services.
Strengths and limitations
This systematic review has identified many areas for improvement in clinical practice, and its findings can lead to concrete recommendations. The strengths of this study are the wide range of perspectives and experiences analysed from three groups of people, including people with eating disorders, families and health professionals across international healthcare systems. The limitations for this review are the lack of primary papers available focusing principally and/or specifically on the facilitators and gaps at the interface. As a result, these findings were gleaned from papers that had a main focus elsewhere. To ensure greater in-depth analysis of the data, a much larger set of primary data would be required.
In conclusion, this systematic review looks at a range of experiences and perspectives of the eating disorder primary and secondary care healthcare interface. Three dominant themes of ‘the help-seeking process at primary care’, ‘expectations of care and appropriate referrals’ and ‘opposition and collaboration in treatment of and recovery from eating disorders’ identify many facilitators and barriers existing at the interface. We suggest that attention to these issues could improve the quality of care and experiences of individuals with eating disorders and their families and the role of health professionals.
Funding
This systematic review is part of a research project entitled ‘Mind the Gap! An examination of the interface between primary and secondary healthcare for eating disorders’. This work was supported by the Welsh Government through Health and Care Research Wales (HRA grant number: HRA-15-1079).
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2019.48.
Appendix 1
Study eligibility checklist
Appendix 2
Key point summary theme 1
Appendix 3
Key point summary theme 2
Appendix 4
Key point summary theme 3









eLetters
No eLetters have been published for this article.