The cost of supporting people who are unable to work because of ill health is an international concern. Reference Kemp, Sunden and Bakker Tauritz1 In 2008 it was estimated that the total cost of sickness and disability-related worklessness among working-age adults in the UK was £100 billion, more than the annual costs of the NHS. Reference Black2 There is particular concern about the rising proportion of long-term claims. 3 Research suggests that in some areas of the UK, sickness and disability benefits act as a disguised form of unemployment, and that many claimants are willing and able to work if suitable work was available. Reference Beatty and Fothergill4,Reference Beatty, Fothergill and Gore5 Mental disorders are recognised to be one of the most common reasons why people claim sickness benefits worldwide, and evidence suggests their contribution is increasing. Reference Kemp, Sunden and Bakker Tauritz1,Reference Danziger, Frank and Meara6–Reference Waddell and Aylward8 In 2008, the government of the UK introduced measures to tighten eligibility and encourage work-seeking. Despite this, there has been no recent long-term analysis of trends in sickness benefits throughout the UK, nor analysis of the changing patterns of the major medical causes of claims. The current study analysed trends in claims for sickness benefits from 1995 to 2014 using data from the Department of Work and Pensions. We examined changes in the prevalence of claims attributable to mental disorders compared with other major categories of medical condition and changes in long-term claims. We explored the distribution of claims because of mental disorder in terms of gender, age and region of the UK, and the relative contribution of different types of mental disorder.
Method
Data
Source of data
Data from the Department for Work and Pensions regarding numbers of claimants of all sickness and disability-related benefits in England, Scotland and Wales were used (hereafter referred to as the UK for convenience, although Northern Ireland is not included since it has a separate system). Claimants are defined as people who have applied for, and been awarded, their respective benefit. The data are made available four times a year, and data from May each year were used for this analysis.
Benefits data are collected as part of the Work and Pensions Longitudinal Study, which links information on benefits and taxation data from Her Majesty's Revenue and Customs (HMRC). 9 Part of the data was accessed directly from the Department of Work and Pensions website, 10 but more detailed data on categories of mental disorder were obtained upon request under the Freedom of Information Act. Since 2000, data represent the total number of claimants of sickness-related benefits, but prior to this year data were derived from a 5% sample of claimants.
Causes of claims
The Department for Work and Pensions classifies the broad medical causes of ‘incapacity’ (the condition for which benefits are awarded) according to the International Classification of Diseases, tenth edition (ICD-10), published by the World Health Organization. 11 In people with multiple conditions, only the most significant is required to be recorded. The data on claimants are also grouped into specific selected disorders within each group. The latter reflects the terminology that is used by the medical practitioners who submit evidence to support claims and do not correspond exactly to any particular, official diagnostic system. The initial medical assessment is made by the claimant's general practitioner, but subsequently most claimants are required to be reviewed by a doctor employed on behalf of the Department for Work and Pensions.
Changes in the benefit system
Prior to 2008, people claiming state benefits for sickness or disability in the UK were awarded Incapacity Benefit. Prior to 2001, Severe Disablement Allowance was paid to people with long-term disability who had not paid sufficient National Insurance contributions to qualify for Incapacity Benefit. From 2001, Incapacity Benefit was extended to this group. In October 2008, a new benefit, Employment and Support Allowance (ESA), was introduced for new claimants. The system for claiming ESA differs from the old system of Incapacity Benefit to the extent that most people are required to undergo repeated ‘work capability assessments’ to be entitled to receive benefit payments. 12 From October 2010, claimants who received the pre-existing benefits (Incapacity Benefit and Severe Disablement Allowance) started to be assessed to see whether they qualified for ESA. This strategy was initially introduced in limited geographical areas, before being rolled out nationally to the rest of the UK from April 2011.
Analysis
Overall trends
From 2008, we amalgamated data for ESA claimants with data on claimants who remained on Incapacity Benefit or Severe Disablement Allowance. Since categorisation by medical condition was not available for the first 2 years of ESA data, we estimated the numbers of these claimants by medical category by applying the percentage of claimants in a particular category in 2010 to the data from 2008 and 2009. This enabled us to produce continuous trends in claimants by medical condition. These estimations made up only a small proportion of the figures for these years, however, since ESA was only awarded to new claimants during this time.
We charted trends in the total number of sickness and disability benefit claimants and numbers of claimants by each major causal medical category for each year between 1995 and 2014. Data from 1995 to 1999 were only available for the 5% sample, but from 2000 onwards data were available for the total number of claims. We also calculated the proportion of total claimants accounted for by each major causal category of medical conditions in 1995 and 2014. We compared changes in the proportions of claims for each category between 1995 and 2014 using Z-tests for differences between independent groups. These were computed manually, using an alpha level of 0.5. For figures obtained from the 5% sample, we used the actual numbers obtained for the calculations, i.e. 5% of the estimated total. We assumed that claimants in 1995 were different individuals from claimants in 2014 because of the 20-year time difference.
Trends in long-term claims
We analysed trends in numbers of people claiming benefits for more than 5 years. It was not possible to obtain reliable data on duration of sickness claims prior to 2000, owing to unavailability of data, nor after 2011. When claimants started to be transferred from Incapacity Benefit (or Severe Disablement Allowance) to ESA in April 2011, claims were classified as starting from the point at which ESA started, regardless of how long people had been claiming other benefits prior to this point. There is, therefore, an artificial decrease in long-standing claims after this time. Hence we analysed trends in numbers of claimants claiming benefits for more than 5 years between 2000 and 2011. Since we were using data from May, the 2011 data were not yet affected by the changes introduced with the transfer of existing claimants to ESA. We did not apply significance testing to this analysis since the assumption that the 2000 data and the 2011 data are independent is unlikely to hold, especially since claimants were those on long-term benefits.
Age, gender and regional distribution
To explain the trends in claims for mental disorders, we examined the age and gender distributions of claimants with mental disorder diagnoses and compared them with the distributions for those with other conditions. We used the Department for Work and Pensions age categories, but merged the two oldest (age 55–60 and over 60) and two youngest age groups (age under 18 and 18–24) to obtain approximate 10-year age bands. The Department for Work and Pensions does not produce data on claimants’ socioeconomic status, but we examined the proportions of mental disorder claims in the different regions of the UK. Regional distribution of sickness and disability claims is known to vary with the socioeconomic characteristics of the region. Reference Beatty and Fothergill4,Reference Moncrieff and Pomerleau13
Trends in mental disorders
We examined trends in the numbers of claimants claiming benefits for different mental disorders within the overall mental disorder category, combining diagnostic labels that appeared to represent similar conditions (as presented in Table 4). These data were derived from the 5% sample for the first year the data was available which was 1999, and thereafter it was derived from data on all claimants (the 100% sample). We used Z-tests to test for the difference in proportions of claims represented by different conditions between 1999 and 2014.
Confidence intervals were computed for all estimates based on the 5% sample data.
Results
Total numbers of claimants of any type of sickness benefit declined by 6.4% from 2 672 000 in 1995 to 2 501 000 in 2014 (Fig. 1). The decline started in the late 1990s, but then numbers rose again between 2000 and 2003, before falling year on year, apart from small increases in 2009 and 2014.
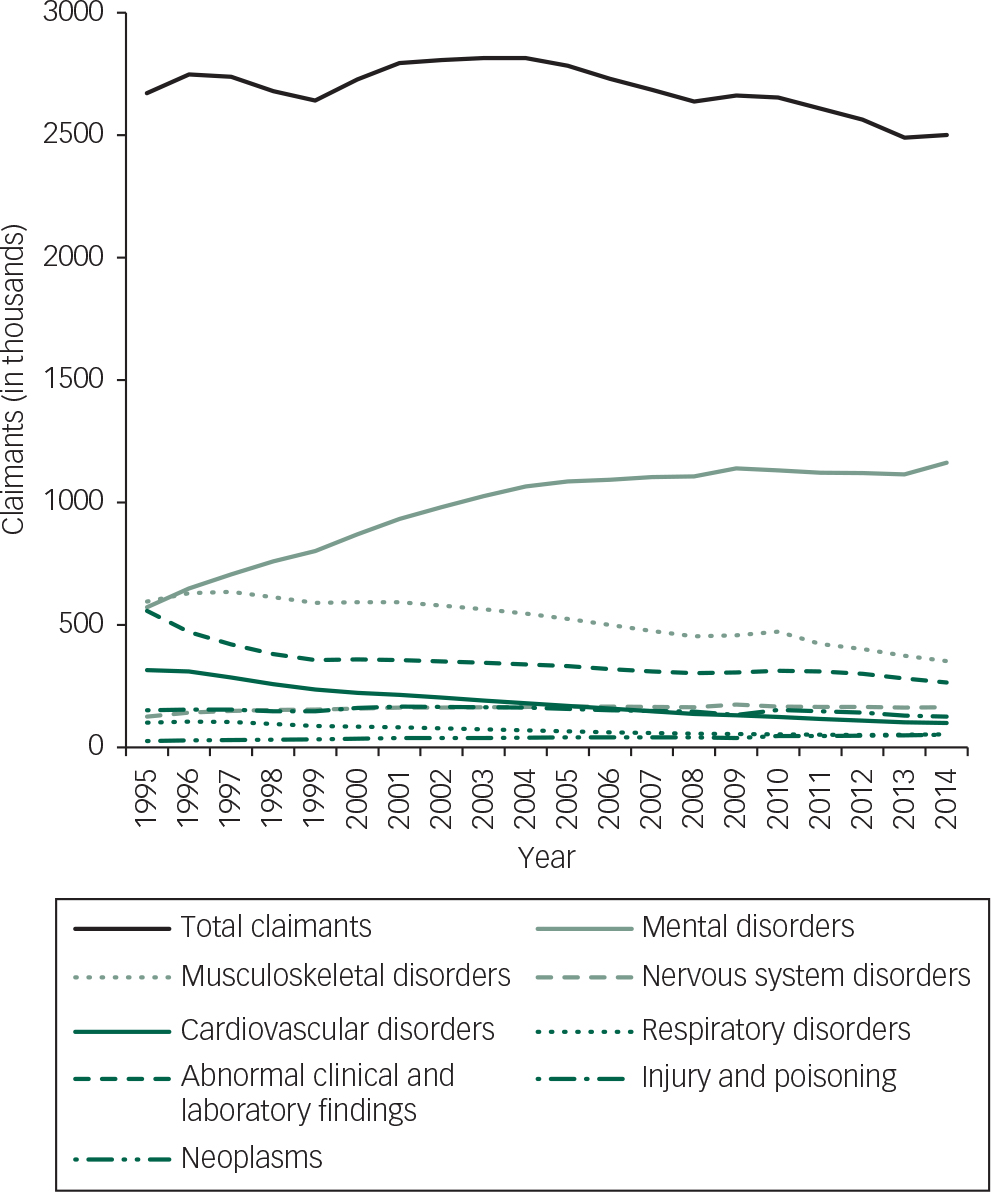
Fig. 1 Trends in claimants of sickness and disability benefits by medical category 1995–2014.
Figure 1 shows trends in the numbers of claimants for the eight most common causal categories of medical condition, including mental disorders. Whereas in 1995 musculoskeletal disorders were the most common cause of sickness benefit claims, with mental disorders close behind, numbers of claimants for musculoskeletal disorders diminished continuously thereafter, dropping by 40.8% overall from 595 900 in 1995 to 352 550 in 2014. In contrast, the number of claimants whose claim was attributed to a mental disorder more than doubled, rising by 103.4% over the period examined to over a million in 2014 (from 571 600 in 1995 to 1 136 360 in 2014). The number of claimants whose claim was because of other major causal categories, including cardiovascular disorders, respiratory disorders and disorders ‘not elsewhere classified’ also diminished by 68.5%, 47.1% and 52.6% respectively. Claimants diagnosed as having a ‘diseases of the nervous system’ increased by 29.5%, but from a lower baseline. Overall, claimants classified as having conditions other than a mental disorder fell by 35.0% between 1995 and 2014 (from 2 100 400 to 1 364 640).
Table 1 presents the number and proportion of claimants grouped according to the eight most common medical causes of incapacity in 1995 and 2014. The proportion of claimants represented by people with a mental disorder rose substantially. By 2014, almost half of claimants were claiming benefits for a mental disorder, up from 21.4% in 1995 to 46.5%. Changes in all categories of medical condition were highly statistically significant.
Table 1 Claimants classified according to major causal categories of medical disorder in 1995 and 2014
| Overall category of medical disorder (DWP classification) | Number of claimants 1995 a (thousands) | % of total claimants 1995 (95% CI) | Number of claimants 2014 (thousands) | % of total claimants 2014 |
|---|---|---|---|---|
| Mental disorders b | 571.6 | 21.4 (21.2–21.6) | 1162.4 | 46.5 |
| Musculoskeletal disorders b | 595.9 | 22.3 (22.1–22.5) | 352.6 | 14.1 |
| Cardiovascular disorders b | 315 | 11.8 (11.6–12.0) | 99.3 | 4.0 |
| Respiratory disorders b | 100.5 | 3.8 (3.70–3.90) | 53.2 | 2.1 |
| Nervous system disorders b | 126 | 4.7 (4.59–4.81) | 163.1 | 6.5 |
| Neoplasms b | 25.8 | 0.97 (0.92–1.02) | 51.0 | 2.0 |
| Injuries b | 151.6 | 5.7 (5.58–5.82) | 125.0 | 5.0 |
| Disorders not elsewhere classified b | 557.8 | 20.9 (20.7–21.1) | 264.5 | 10.6 |
| Total claims | 2672 | 2501 |
DWP, Department for Work and Pensions.
a Data from 5% sample.
b Z-test for difference between proportions of claimants in 1995 and 2014, P<0.0001.
Figure 2 shows trends in numbers of long-term claimants (defined as individuals claiming benefits for longer than 5 years) for claimants with mental disorders and claimants with all other conditions from 2000 to 2011. Overall, there was an increase in the number of long-term claimants of 26.4% from 1 173 680 in 2000 to 1 483 470 in 2011 (not shown). Numbers of long-term claimants for mental disorders rose by 87.4% from 346 770 in 2000 to 649 990 in 2011 and numbers with all other conditions rose by only 0.79% (from 826 910 to 833 480). In 2011, claimants whose claim was attributable to a mental disorder accounted for 43.8% of all long-term claimants, compared with 29.6% in 2000.
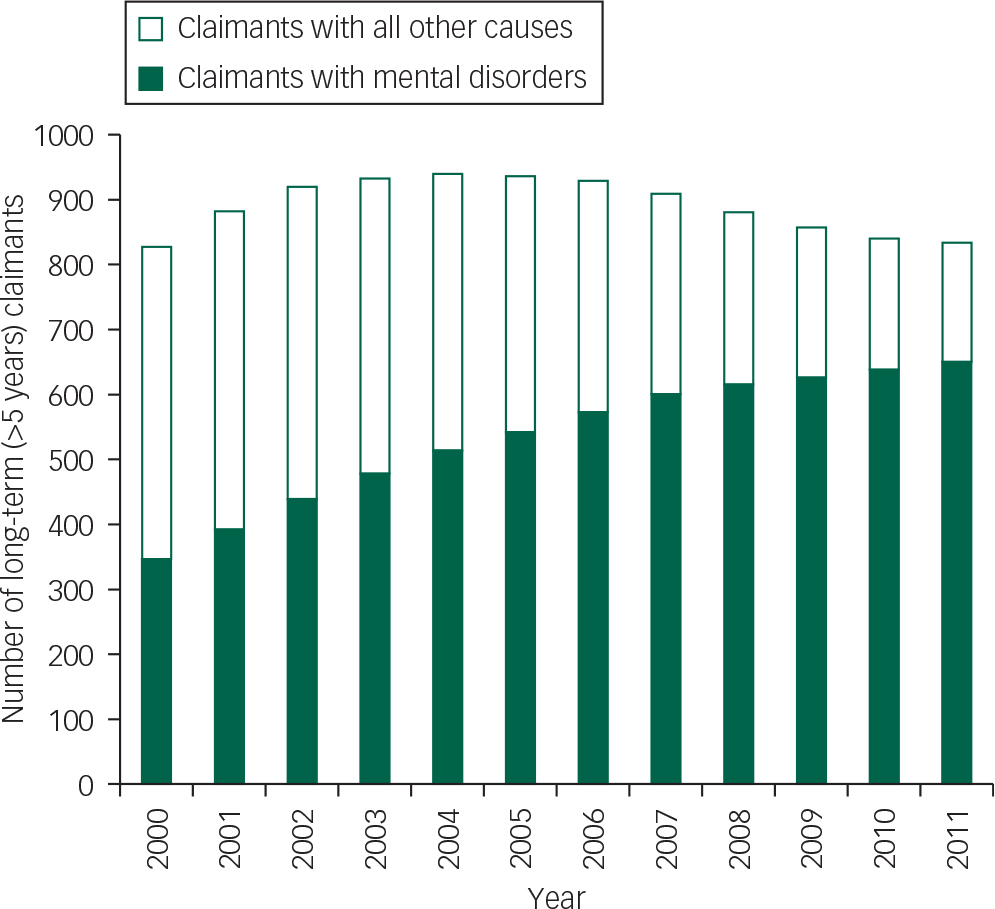
Fig. 2 Trends in long-term (>5 years) claimants of sickness and disability benefits.
The proportions of claimants claiming benefits for mental disorders according to age group and gender are presented in Table 2. In 1995, the proportion of women claiming benefits for a mental disorder was higher than the proportion of men, but proportions had equalised by 2014. Claims for a mental disorder made up a greater proportion of claims in younger age groups in both 1995 and 2014. There were increases in the proportion of mental disorder claims in all age groups, but differences between the age groups were less marked in 2014, due in large part to a greater increase in the proportion of mental disorder claims in people aged over 55. Table 3 shows the regional distribution of the proportion of mental disorder claims within the UK. The proportion of mental disorder claims was highest in London and southern regions in 1995, and in Scotland in 2014. Other than Scotland, areas traditionally associated with industrial decline, such as Wales, the North East and the North West, did not show particularly high proportions of mental disorder claims compared with other areas.
Table 2 Proportion of mental disorder claimants by gender and age group
| Mental disorder claimants as a percentage of total claimants (%) | ||
|---|---|---|
| 1995 a (95% CI) | 2014 | |
| Men | 18.4 (18.5–18.7) | 46.8 |
| Women | 26.9 (26.8–27.0) | 46.1 |
| Age group <24 | 31.7 (31.5–31.9) | 57.2 |
| Age group 24–34 | 35.9 (35.7–36.1) | 61.2 |
| Age group 35–44 | 31.5 (31.4–31.6) | 55.4 |
| Age group 45–54 | 22.8 (22.7–22.9) | 45.1 |
| Age group >55 | 11.0 (10.9–11.1) | 32.0 |
a Data from 5% sample.
Table 3 Proportion of mental disorder by UK region
| Mental disorder claimants as a percentage of total claimants (%) | ||
|---|---|---|
| 1995 a (95% CI) | 2014 | |
| Scotland | 29.8 (29.6–30.0) | 48.8 |
| Wales | 24.5 (24.3–24.7) | 45.5 |
| North East | 24.9 (24.7–25.1) | 45.2 |
| North West | 28.2 (28.1–28.3) | 47.6 |
| Yorkshire | 26.1 (25.9–26.3) | 45.4 |
| West Midlands | 26.7 (26.5–26.9) | 45.2 |
| East Midlands | 25.6 (25.4–25.8) | 44.8 |
| East of England | 29.0 (28.8–29.2) | 45.7 |
| London | 33.2 (33.0–33.4) | 46.3 |
| South East | 31.7 (31.5–31.9) | 47.0 |
| South West | 30.6 (30.38–30.82) | 47.7 |
| Abroad | 18.7 (18.7–18.8) | 32.6 |
a Data from 5% sample.
Table 4 presents numbers of claimants according to the different types of mental disorders recorded in 1999, when these data were first available, and 2014. In both years, the collective category of ‘depressive disorders’ accounted for almost half of all claimants whose claim was attributed to a mental disorder. In 1999 there were 344 700 claims, representing 41.5% (CI 41.0–42.0) of all mental disorder claims, and in 2014 there were in 513 900 claims, representing 44.2%. There was a decline in the proportion of claimants diagnosed as having an anxiety disorder (including claimants coded as having an ‘extreme reaction to stress’). Combined with the first category, however, anxiety and depressive disorders were the diagnosis recorded for a total of 74.7% (74.3–75.1) of claimants whose claim was classified as because of a mental disorder in 1999, and 66.8% in 2014. There was little change in the proportion of claimants recorded as having a learning disability or ‘developmental disorder’, which was the next most numerous diagnosis of claimants with a mental disorder. Psychotic disorders, which was the diagnosis recorded in 8.36% (8.09–8.63) of claimants classified as having a mental disorder in 1999, declined to 6.9% in 2014. There was an increase in claimants whose diagnosis was not specified. Although numbers were much smaller, there were statistically significant increases in claimants diagnosed as having eating disorders or a personality disorder and a decrease in claimants recorded as having ‘disorders of the puerperium’.
Table 4 Claimants classified according to major causal categories of mental disorder in 1999 and 2014
| Category of disorder | DWP data classification | Number of claimants 1999 a (thousands) | % of total mental disorder claimants 1999 (95% CI) | Number of claimants 2014 (thousands) | % of total mental disorder claimants 2014 |
|---|---|---|---|---|---|
| Depressive disorders b | -Depressive
episode -Recurrent depressive disorder -Persistent mood disorder -Unspecified mood disorder |
344.7 | 41.5 (41.0–42.0) | 513.9 | 44.2 |
| Anxiety and other neurotic disorders b | -Phobic
disorder -Other anxiety disorder -Reaction to severe stress -Dissociative disorder -Somatoform disorder |
231.1 | 27.8 (27.4–28.2) | 263.1 | 22.6 |
| Psychotic disorders b | -Schizophrenia -Persistent delusional disorder -Manic episode -Unspecified non-organic psychosis |
69.4 | 8.36 (8.09–8.63) | 80.1 | 6.90 |
| Learning disability c | -Unspecified mental
retardation -Specific developmental disorders of scholastic skills -Pervasive developmental disorder |
87.7 | 10.6 (10.3–10.9) | 125.5 | 10.8 |
| Alcohol and drug dependence d | 60.4 | 7.27 (7.02–7.52) | 89.7 | 7.71 | |
| Dementia e | 0.90 | 0.11 (0.08–0.14) | 1.14 | 0.1 | |
| Personality disorder b | 2.20 | 0.26 (0.21–0.31) | 6.72 | 0.59 | |
| Eating disorders b | 1.00 | 0.12 (0.09–0.15) | 2.48 | 0.21 | |
| Mental disorders not otherwise specified b | 28.7 | 3.46 (3.28–3.64) | 77.8 | 6.7 | |
| Mental and behavioural disorders associated with puerperium b | 4.10 | 0.49 (0.42–0.56) | 2.06 | 0.18 | |
| Total mental disorders | 830.4 | 1162.4 |
a Data from 5% sample.
b Z-test for difference between proportions of claimants in 1995 and 2014, P<0.0001.
c Z-test for difference between proportions of claimants in 1995 and 2014, P=0.12.
d Z-test for difference between proportions of claimants in 1995 and 2014, P=0.0006.
e Z-test for difference between proportions of claimants in 1995 and 2014, P=0.52.
Discussion
Although the total number of people claiming state benefits for sickness and disability in the UK has declined since 2003, the number of people claiming benefits because of a mental disorder has been rising steadily, with current numbers at approximately 1.1 million. Mental disorders are now the largest single medical cause of claiming such benefits and by 2014 they accounted for almost half of all claims. They outstripped musculoskeletal disorders as the largest cause of claims from 1995 onwards, and claims for the two types of disorders continued to diverge, with claims for musculoskeletal disorders falling by 40%, and those for mental disorders more than doubling. Claims attributed to cardiovascular disorders, the next most common medical cause of benefit claims, also fell by more than half.
In contrast to the fall in overall claims, the number of people claiming benefits for more than 5 years has increased since 1995. This increase is almost entirely because of the rise in long-term claims because of a mental disorder.
The pattern of rising claims for mental disorders is consistent with a report on UK data from a decade ago, Reference Waddell and Aylward8 an analysis of data from Scotland from 2000–2007, Reference Brown, Hanlon, Turok, Webster, Arnott and Macdonald7 and with data from other developed countries, including Denmark, the Netherlands, Sweden, Israel and the USA. Reference Kemp, Sunden and Bakker Tauritz1,Reference Danziger, Frank and Meara6 Thus, it appears to represent a trend that applies across developed nations.
The distribution of claims for different types of mental disorders has changed little over the last 15 years. The proportion of claims attributed to depressive and anxiety disorders as a whole fell slightly, but they still account for two-thirds of mental disorder claims. The proportion of claims associated with psychotic disorders also fell slightly. Data from the 1990s also showed that depressive and ‘neurotic’ disorders accounted for the vast majority of benefits paid for sickness and disability in the UK, Reference Moncrieff and Pomerleau13 and a more recent analysis of Scottish data showed a similar weighting towards these types of conditions. Reference Brown, Hanlon, Turok, Webster, Arnott and Macdonald7
Benefits and employment
There has been considerable debate about the significance of increasing levels of sickness benefit claims. Research from the UK indicates a 10-fold variation in rates of claims between regions and districts, with highest rates being found in the areas of the north of England, Scotland and Wales, which have seen the greatest levels of industrial decline. Reference Beatty and Fothergill4,Reference Beatty, Fothergill and Gore5,Reference Green and Owen14 This evidence has led some authors to suggest that sickness benefit claims represent disguised unemployment in some areas and some groups. Reference Beatty, Fothergill and Macmillan15 In other words, despite their health problems, some claimants may be willing and able to perform some sort of work, but suitable work is not available. The fall in demand for low-skilled labour has affected lower socioeconomic groups more than others, Reference Nickell and Quintini16 and disability is also associated with lower socioeconomic status. Reference Adamson, Ebrahim and Hunt17,Reference Gannon and Nolan18 In most countries, disability benefits are more generous than unemployment benefits, even with recent changes. Evidence from the USA suggests that disability benefit rates have risen in relation to incomes for unskilled workers, making dropping out of work more attractive, especially for workers living in low-wage states. Reference Autor and Duggan19
Claims for common mental disorders may be particularly sensitive to labour market conditions, since these disorders are more prevalent in lower socioeconomic groups, Reference Scott, Al-Hamzawi, Andrade, Borges, Caldas-de-Almeida and Fiestas20 the groups most affected by job losses. Some mental disorders, like less severe musculoskeletal disorders, may be manageable in the right work environment, with accommodating employers and security of employment, but intolerable in less secure workplaces. The greater work intensity demanded in the post-industrial economy has also been suggested to be a source of stress. Reference Kemp, Sunden and Bakker Tauritz1 Hence as employment options contract, workers may opt to claim disability benefits rather than compete for work that would be difficult for them to sustain.
We did not, however, find greater proportions of mental disorder claims in regions of high unemployment and economic inactivity (excepting Scotland), or changes suggestive of greater proportional increases in these areas between 1995 and 2014. Moreover, the overall and relative trends in mental disorder claims were not obviously affected by the recent economic recession.
Mental disorder trends
There are, therefore, likely to be other drivers for the dramatic divergence in claims for mental disorders compared with other conditions in recent years. The decline in claims among older people is likely to account for some of this pattern. Incapacity benefit and the new ESA are not available to people over the state pension age (in contrast to Severe Disablement Allowance), and claimants with other medical conditions are older than those claiming benefits for mental disorders. However, numbers of people on Severe Disablement Allowance were small, since it was discontinued in 2001. Moreover, the divergent trends were visible in every age category, and claims for mental disorders among older people rose regardless.
Evidence from the UK suggests a modest increase in the reported prevalence of common mental disorders since the early 1990s, but this is not large enough to account for the increase in disability claims, and may represent increasing recognition and identification of such disorders as much as their actual occurrence. Reference Maybin and Thorlby21
It seems likely that the decreasing stigma associated with mental health problems following media campaigns is significant. Individuals who might previously have been diagnosed as having other conditions, such as back pain, for example, may now be more readily classified as depressed. Indeed, evidence suggests that back and neck pain are often associated with mental disorders such as depression and anxiety. Reference Demyttenaere, Bruffaerts, Lee, Posada-Villa, Kovess and Angermeyer22 Moreover, changing approaches to the treatment of back pain, with an emphasis on recovery and activity, may have discouraged long-term claims for this condition, facilitating the relative rise in mental disorder claims. Reference Cattrell, Harris, Palmer, Kim, Aylward and Coggon23,Reference Buchbinder, Jolley and Wyatt24 This thesis is supported in the current data by the fact that the distribution of mental disorders across age groups and gender became more similar to the distribution of other disorders over the period examined. Our data also support a previous suggestion that the cultural changes that influenced the change from musculoskeletal disorders to mental disorders started in London and the South, and subsequently spread to other regions. Reference Cattrell, Harris, Palmer, Kim, Aylward and Coggon23 Further research is needed, however, to explore the contrasting trends in claims for mental disorders and claims for other common medical conditions.
Consequences of worklessness
Concerns about the disadvantages associated with worklessness were part of the motivation for the reforms to the benefits system introduced by the British Government in 2008. 3 This coincided with the worldwide economic crash. Neither event appears to have had much impact on long-term trends in total claims for sickness and disability benefits in the UK, which were falling prior to 2008, nor on rates of mental disorder claims, which had long been rising. However, it is likely that numbers of claimants would have risen further over the economic recession in the absence of the new procedures. Reference Beatty, Fothergill and Gore5
Non-employment among those with mental health problems has individual as well as social costs. Work has been shown to be beneficial for mental health, and people with severe mental disorders who find secure employment show improvements in symptom levels, self-esteem, social disability and quality of life. Reference Burns and Catty25,Reference Schneider, Slade, Secker, Rinaldi, Boyce and Johnson26 Although research with people with severe mental disorders suggests they want to work, the barriers are substantial and include symptoms of the mental condition, effects of treatment, a poor sickness record and lack of confidence. Reference Marwaha and Johnson27,Reference Boycott, Akhtar and Schneider28 There is a complex trade-off between providing security and dignity for people who are mentally incapacitated and unable to work, and creating a ‘disability trap’ that produces a culture of dependence and demoralisation. Reference Drake, Bond, Thornicroft, Knapp and Goldman29 It is a particular concern that individuals with mental disorders show an increasing tendency to be claiming sickness and long-term disability benefits, since it has been shown that such people are unlikely ever to rejoin the workforce. Reference Berthoud30
Although some argue that the most important intervention to reduce benefit claims is the provision of suitable job opportunities for lower socioeconomic groups, Reference Beatty and Fothergill4 others, including the UK Government, advocate individual-level interventions. Thus, the ESA benefit provides people who are thought to be capable of returning to work with support from an Employment Service Advisor. The success of this approach has not yet been formally evaluated, but more intensive employment support schemes have been trialled for people with severe mental disorders. Their success also depends on the local context of employment rates, economic growth and welfare systems, however, Reference Heslin, Howard, Leese, McCrone, Rice and Jarrett31,Reference Burns, White and Catty32 and they have not so far been offered to people with less severe, but more common, mental health problems.
Limitations
The way that mental disorders are classified by the Department for Work and Pensions does not correspond to official classification systems and the reliability of the classification has not been established. The information on diagnosis comes initially from general practitioners, who may provide only vague descriptions of the reasons for the claim (such as ‘stress’). Whereas this is less likely to affect categorisation of claims into broad medical categories, it may affect the quality of data on different mental disorders. General practitioners may have a tendency, for example, to classify schizophrenia as something less severe to avoid the use of what is perceived as a stigmatising diagnosis. The introduction of more stringent procedures for obtaining benefits may produce the opposite pressure, requiring evidence of more serious problems to justify a claim. Moreover, some diagnoses such as bipolar disorder were not included, so that some people with this diagnosis may have been included in the ‘depressive disorders’ category under the Department's label of ‘chronic mood disorders’. It is notable, however, that the relative contributions of different types of mental disorder, broadly conceived, have not changed substantially since the 1990s.
Despite these issues, the Department for Work and Pensions data are collected nationally, using the same protocols year on year. Since 2000, diagnostic information has been provided for 100% of all claimants nationwide, except for the early years of the introduction of ESA. Prior to this date, detailed information, such as diagnostic category, was only available for a 5% sample of claimants. Overall numbers of claimants and proportions of claimants prior to 2000 therefore represent estimates. Because of the large size of the sample, the estimates are extremely precise, however, as indicated by the narrow confidence intervals. Moreover, unlike some other countries, for example, the USA where there are multiple types of public assistance for people with ill-health, the system of sickness and disability benefits in the UK is relatively simple. Even with the changeover to the new ESA, it is possible to examine long-term trends in the total number of people who receive public welfare payments because of ill-health.
Implications
According to the current analysis, mental disorders constitute a major burden on social resources, and one that is increasing. Moreover, the burden is largely attributable to common mental disorders, such as anxiety and depression, rather than conditions like schizophrenia that are generally regarded as being more severe and persistent. The increasing use of all types of drugs for mental disorders, and especially antidepressants, in England since the 1990s does not appear to have ameliorated the rising trends in disability claims for these conditions. Reference Ilyas and Moncrieff33 Moreover, long-term use of antidepressants is reported to be increasing, Reference Moore, Yuen, Dunn, Mullee, Maskell and Kendrick34 just as long-term disability claims because of mental disorders are rising. These corresponding trends may indicate greater chronicity of depression and other common mental disorders than is usually thought to be the case.
The disguised unemployment hypothesis suggests that socioeconomic changes, not individual-level treatment, are required to reduce sickness benefit claims, particularly the provision of suitable employment opportunities where health and mental health-related limitations are accommodated. Supported employment interventions may complement such measures, but further research is needed to evaluate their effectiveness for people with severe, and less severe, mental health problems in the context of the UK.
Acknowledgments
We would like to thank the staff of the Department for Work and Pensions for supplying and clarifying aspects of the data, and Dr Rebecca Jones of the Division of Psychiatry, University College London for statistical advice.









eLetters
No eLetters have been published for this article.