Case
A woman in her mid-20s, with no personal or family history of mental illness, presented to her general practitioner with anxiety and low mood. Sick leave from her stressful job provided no relief. Over 5 weeks, her mood, appetite and sleep rapidly worsened. She experienced severe panic attacks and later, an auditory hallucination on at least one occasion. Mirtazapine and zopiclone provided no immediate benefit, and an urgent referral to the community mental health team was made.
Her behaviour became acutely disturbed at home. She rapidly alternated between being angrily agitated and mutely staring. She spoke in strange voices, and the content could be nonsensical at times. Occasionally, she randomly burst into song. She repeatedly squatted and bit her lip. She followed her parents around the house, fearing harm could come to them. At different points in time, she complained of having a ‘sore head’ and ‘floppy’ legs.
Given the severe deterioration in her mental health, an emergency psychiatric admission using mental health legislation was arranged. On admission, routine physical observations (including temperature), examination and blood tests (including white cell count and C-reactive protein) were normal.
On the ward, she appeared profoundly depressed, with extremely impoverished and latent speech. At times, she also appeared fearfully hypervigilant or perplexed. She exhibited mutism, staring, stereotypy and mannerisms – features suggestive of catatonia. Her social judgement was impaired and she lacked insight. She required intense one-to-one nursing care and direction with washing and dressing, implying severe cognitive dysfunction (no formal testing was done).
The initial working diagnosis was a severe depressive episode with psychotic symptoms (ICD-10 code F32.3), given the prominence of her severely depressed mood, which preceded the disorganised behaviour, impoverished speech and psychomotor retardation.
Over 4 weeks on the ward, her mood partially lifted in response to treatment with venlafaxine, olanzapine (low dose) and regular lorazepam (for catatonia). After some uneventful passes home, early in-patient discharge was facilitated by her very supportive parents.
However, upon review in clinic a few days later, concerns were raised regarding an apparent worsening in her cognition (e.g. gross disorientation and poor memory) and motor skills, both fine (e.g. button opening) and gross (e.g. descending stairs). Furthermore, abnormal involuntary movements were observed in one hand.
Given the onset of new focal neurological deficits, it was decided to take blood tests to screen for autoimmune encephalitis. Fortuitously, results were returned within 24 hours (by the local neuroimmunology laboratory), and revealed the presence of serum N-methyl-D-aspartate receptor (NMDAR) antibodies.
Urgent admission to the neurology department was arranged, where work-up and treatment for probable anti-NMDAR encephalitis began. Cerebrospinal fluid (CSF) analysis also detected NMDAR antibodies, thereby confirming the diagnosis. Notably, magnetic resonance imaging (MRI) head and electroencephalogram (EEG) results were normal.
The encephalitis progressed despite treatment with steroids and intravenous immunoglobulins, resulting in fluctuating consciousness and autonomic instability for 1–2 weeks. Rituximab was then commenced, to which there was a gradual, marked and sustained response. Ovarian teratoma and other tumours were excluded through imaging. At 1 year after disease onset, the patient's recovery continued at home.
In Box 1, the patient in this case describes her experience.
Box 1 The experience of a patient with anti-N-methyl-D-aspartate receptor encephalitis (informed consent obtained).
I was in for a normal busy day at work, when I suddenly started to feel extremely overwhelmed and panicked. Stranger still, I completely blanked when I set about doing my usual work on the computer.
During my sick leave, having always been a very positive and social person, I was suddenly not interested in engaging with any of my friends or family. For instance, when my mum's hairdresser came over, someone I have always enjoyed chatting to, I avoided her entirely. I was also finding everyday tasks extremely difficult; for example, I couldn't wrap a towel around myself, I still had lots of shampoo and conditioner left in my hair when I came out of the shower, I couldn't put on my bra at all by myself and I kept putting two arms into a single top sleeve or two legs into a single trouser leg. Having always been a great sleeper, I was also finding it very difficult to sleep at night. I could not express to my parents how I was feeling and I couldn't fathom what was going on with me.
I grudgingly visited a local healthcare centre and met two psychiatrists who both told me I was severely depressed and then referred me to hospital, where I spent some time in the psychiatric ward. My mood initially was at the lowest it had been my entire life. I had no motivation to do anything at all. However, as stated, the doctor noticed my right hand twitching constantly, a physical behaviour I had never expressed prior to my admission, along with other symptoms, and made the decision to have my blood tested for autoimmune encephalitis.
It has been a long road towards recovery, most of which I do not remember, but over a year later I am still progressing and improving.
Learning objectives
(a) What is autoimmune encephalitis?
(b) What is anti-NMDAR encephalitis?
(c) When should anti-NMDAR encephalitis be suspected?
(d) How should suspected anti-NMDAR encephalitis be investigated?
(e) How should the practical management and treatment of anti-NMDAR encephalitis be approached?
(f) What is the prognosis for anti-NMDAR encephalitis?
Autoimmune encephalitis
Autoimmune encephalitis refers to autoantibody-mediated inflammation of the brain. It manifests with a pattern of psychiatric and/or neurological symptoms, dependent on the specific autoantibody involved. Red flags for autoimmune encephalitis in patients with psychosis are shown in Box 2; these are useful when considering differential diagnoses, the indication for immunological testing and guiding discussion on the most suitable initial admitting speciality.
Box 2 Red flags for suspicion of autoimmune encephalitis in patients with psychosis (reproduced with permission from Pollak et al, based on work by Al-Diwani et al and Herken and Prüss).Reference Pollak, Lennox, Müller, Benros, Prüss and van Elst1–Reference Herken and Prüss3
Red flags for suspicion of autoimmune encephalitis in patients with psychosis (one or more required):
(a) Infectious prodrome
(b) New-onset severe headache or clinically significant change in headache pattern
(c) Rapid progression
(d) Adverse response to antipsychotics or presence of neuroleptic malignant syndrome
(e) Insufficient response to antipsychotics
(f) Movement disorder (e.g. catatonia or dyskinesia)
(g) Focal neurological disease
(h) Decreased consciousness
(i) Autonomic disturbance
(j) Aphasia, mutism or dysarthria
(k) Seizures
(l) Presence of tumour or history of a recent tumour
(m) Hyponatraemia (not explained by side-effects of medications)
(n) Other autoimmune disorders (e.g. systemic lupus erythematosus, autoimmune thyroid disease)
(o) Paraesthesia
The number of known autoantibodies pathologically implicated in cases of autoimmune encephalitis expands every year, as new discoveries are made. Well-established ones include autoantibodies to the voltage-gated potassium channel (VGKC)-complexed proteins LGI1 and CASPR2, AMPA, and GABAB.Reference Endres, Maier, Leypoldt, Wandinger, Lennox and Pollak4 However, by far the most common type of autoimmune encephalitis, and the one most frequently associated with psychiatric symptoms at onset, is anti-NMDAR encephalitis.Reference Rogers, Pollak, Blackman and David5
Anti-NMDAR encephalitis
Pathophysiology
In anti-NMDAR encephalitis, the action of immunoglobulin G (IgG) autoantibodies specific to the GluN1 subunit of the NMDA glutamate receptor results in overall glutamatergic hypofunction.Reference Dalmau, Gleichman, Hughes, Rossi, Peng and Lai6,Reference Irani, Bera, Waters, Zuliani, Maxwell and Zandi7 This causes disruption of cortical and subcortical network activity, even in the absence of notable structural neuronal injury.Reference Finke, Kopp, Scheel, Pech, Soemmer and Schlichting8 The production of these autoantibodies can sometimes be triggered by an ovarian teratoma or infections (e.g. herpes simplex encephalitis); however, in the majority of cases the aetiology remains obscure.Reference Irani, Bera, Waters, Zuliani, Maxwell and Zandi7,Reference Dalmau, Lancaster, Martinez-Hernandez, Rosenfeld and Balice-Gordon9
Epidemiology
The demographic most commonly affected by anti-NMDAR encephalitis is female adolescents and young adults (median age 21 years; female:male ratio 8:2).Reference Dalmau, Armangué, Planagumà, Radosevic, Mannara and Leypoldt10 It is a rare condition, with an estimated incidence of just 1.5 cases per million per year.Reference Dalmau, Tüzün, Wu, Masjuan, Rossi and Voloschin11 Nevertheless, one in five cases in the UK (four in five in the USAReference Dalmau, Gleichman, Hughes, Rossi, Peng and Lai6) presented to psychiatry first.Reference Irani, Bera, Waters, Zuliani, Maxwell and Zandi7 Therefore, it is important that psychiatrists working in all contexts know about this disease.
Presentation
At first, a non-specific prodromal phase of flu-like symptoms (e.g. headache, fever, vomiting, diarrhoea and upper respiratory tract symptoms) occurs in the majority of cases.Reference Dalmau, Gleichman, Hughes, Rossi, Peng and Lai6
Within several days, wide-ranging psychiatric symptoms then develop, which typically prompts initial contact with health professionals. This highly variable phase usually lasts 1–2 weeks. It is marked by major coexisting psychopathology in the categories of behaviour, psychosis, mood, catatonia and sleep, with the complexity of psychiatric presentation being a consistent and distinctive feature of anti-NMDAR encephalitis.Reference Al-Diwani, Handel, Townsend, Pollak, Isabel Leite and Harrison12 The three most common presenting psychiatric symptoms are agitation (59%); psychosis (e.g. auditory/visual hallucinations, persecutory paranoid delusions and disorganised behaviour; 54%); and catatonia (42% in adults),Reference Sarkis, Coffey M, Cooper, Hassan and Lennox13 typically fluctuating between the classic bed-bound rigidity form and the hyperkinetic type. Major mood symptoms (e.g. anxiety, mood instability, depression and mania) are reported in a third of cases.Reference Sarkis, Coffey M, Cooper, Hassan and Lennox13 Short-term memory loss is considered a hallmark feature, but is often obscured by other symptoms.Reference Gultekin, Rosenfeld, Voltz, Eichen, Posner and Dalmau14
Subsequently, there is development of clear neurological features, such as seizures (e.g. generalised tonic-clonic and partial complex), dyskinesias and movement disorders (e.g. orofacial dyskinesia and choreoathetosis), severe cognitive dysfunction, autonomic instability (e.g. fluctuations in cardiac rhythm, thermoregulation and blood pressure), central hypoventilation, and fluctuating consciousness or coma.Reference Dalmau, Gleichman, Hughes, Rossi, Peng and Lai6,Reference Dalmau, Armangué, Planagumà, Radosevic, Mannara and Leypoldt10 In a large international cohort study of 577 cases, 77% of patients were admitted to an intensive care unit in the first month of illness; most often in cases where treatment is given late in the disease course.Reference Titulaer, McCracken, Gabilondo, Armangué, Glaser and Iizuka15
Identification
Given the substantial overlap in the typical age at onset and the presenting symptoms of anti-NMDAR encephalitis with primary psychiatric disorders (such as first-episode psychosis/schizophrenia and bipolar disorder), a pressing challenge for psychiatrists is its early identification,Reference Dalmau, Armangué, Planagumà, Radosevic, Mannara and Leypoldt10 which is made possible only if a high index of suspicion is applied from the outset. Timely diagnosis is especially important because prompt treatment with immunotherapy (e.g. started within 40 days of symptom onset) improves long-term outcomes.Reference Dalmau, Gleichman, Hughes, Rossi, Peng and Lai6,Reference Titulaer, McCracken, Gabilondo, Armangué, Glaser and Iizuka15 In addition, early identification can minimise harm from use of antipsychotics, which are usually poorly tolerated in anti-NMDAR encephalitis and have been associated with neuroleptic malignant syndrome.Reference Lejuste, Thomas, Picard, Desestret, Ducray and Rogemond16
To help promote earlier recognition of anti-NMDAR encephalitis in patients presenting with new-onset psychiatric symptoms, a mnemonic for diagnostic clues was conceived: ‘SEARCH For NMDAR-A’ (Box 3).Reference Dalmau, Armangué, Planagumà, Radosevic, Mannara and Leypoldt10
Box 3 The mnemonic ‘SEARCH For NMDAR-A’ for diagnostic clues suggesting possible anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis (reproduced with permission from Dalmau et al).Reference Dalmau, Armangué, Planagumà, Radosevic, Mannara and Leypoldt10
SEARCH For NMDAR-A:
(a) Sleep dysfunction (typically insomnia at disease onset)
(b) Excitement, disinhibition or manic behaviour alternating with depressive behaviour
(c) Agitation or aggression
(d) Rapid onset (symptoms develop suddenly in days or weeks, whereas in acute psychosis there is usually a history of preceding behavioural changes)
(e) Children and young adult predominance (median age at onset of 21 years; female:male ratio of 8:2)
(f) History of psychiatric illness absent
(g) Fluctuating catatonia (periods of catatonia alternating with extreme agitation)
(h) Negative and positive psychotic symptoms at presentation
(i) Memory deficit
(j) Decrease of verbal output or mutism
(k) Antipsychotic drug intolerance
(l) Rule out neuroleptic malignant syndrome
(m) Antibodies and additional paraclinical tests (electroencephalogram, magnetic resonance imaging or cerebrospinal fluid antibody testing) (NMDAR antibodies are always present in the cerebrospinal fluid)
NMDAR antibody testing
Once the differential diagnosis of anti-NMDAR encephalitis is considered, the priority investigation should be to test for the presence of NMDAR antibodies in the (blood) serum. Practically, this is easily achievable in mental health settings by means of a simple blood draw in a yellow-/gold-topped (serum separating tube; SST) bottle. For gold-standard testing, a paired CSF sample should also be obtained (and tested) at the same time; however, it is acknowledged lumbar puncture mandates acute hospital admission, and for this reason, in reality, it is often tested at a later stage . Regarding the prospect of routine screening for autoantibodies in patients presenting with psychiatric symptoms, see Box 4.
Box 4 Routine screening for autoantibodies in patients presenting with psychiatric symptoms.
Given the challenges of distinguishing the initial stages of autoimmune encephalitis from primary psychiatric disorders, there is a growing body of evidence researching the potential for routine screening for autoantibodies in patients presenting with psychiatric symptoms.Reference Scott, Gillis, Ryan, Hargovan, Gundarpi and McKeon17–Reference Steiner, Walter, Glanz, Sarnyai, Bernstein and Vielhaber20 Thus far, drawing clear conclusions from this evidence has proven difficult, primarily because of study heterogeneity. Therefore, currently, there is no widely enacted recommendation or clinical guideline regarding routine autoantibody screening in the UK. However, a large, multi-site UK study is currently ongoing, which gives potential for change in this regard in the future.Reference SINAPPS Group21 Also of interest and linked to this study, a randomised controlled trial is investigating outcomes of immunotherapy (intravenous immunoglobulins and rituximab) in patients with ‘antibody-associated psychosis’.Reference SINAPPS Group22
Notably, recently published clinical guidelines on schizophrenia in Australia, New Zealand and Germany recommend targeted autoantibody testing at initial presentation.Reference Galletly, Castle, Dark, Humberstone, Jablensky and Killackey23,24
Importantly, rates of seropositivity of anti-NMDAR antibodies (of all Ig classes targeting GluN1, including IgG) in healthy individuals are surprisingly high, at over 10%.Reference Hammer, Stepniak, Schneider, Papiol, Tantra and Begemann25 Moreover, rates of seropositivity in healthy individuals are not significantly different from those in affected individuals; blood brain barrier permeability and activation of intrathecal antibody production are thought to be the major determining factors in whether disease develops.Reference Hammer, Stepniak, Schneider, Papiol, Tantra and Begemann25–Reference Yu, Wu, Cao, Li, Liao and Wei28 Therefore, in practice, a positive serum result – even in a patient with psychosis – does not automatically equate to a diagnosis of anti-NMDAR encephalitis.Reference Martinez-Martinez and Titulaer29 However, it does mean further investigation is warranted – at a minimum with CSF analysis, EEG and MRI of the head – and expert neurology evaluation should be sought.Reference Pollak and Lennox30
In the majority of anti-NMDAR encephalitis cases, both the serum and CSF have detectable NMDAR antibodies. However, at least one in ten cases are seronegative but CSF-positive.Reference Masdeu, Dalmau and Berman31,Reference Gresa-Arribas, Titulaer, Torrents, Aguilar, McCracken and Leypoldt32 Therefore, irrespective of the serum result in cases of high clinical suspicion, CSF testing is indicated to either support or exclude the diagnosis.
Other CSF findings in support of anti-NMDAR encephalitis are a lymphocytic pleocytosis, mildly raised protein concentration and presence of oligoclonal bands restricted to CSF (indicating intrathecal IgG synthesis).Reference Dalmau, Lancaster, Martinez-Hernandez, Rosenfeld and Balice-Gordon9,Reference Blinder and Lewerenz33
In conjunction with medical/neurology colleagues, careful consideration needs to be given to the practical challenges of safely conducting lumbar puncture (and MRI) in a patient who may be agitated and experiencing psychosis. Heavy sedation or general anaesthesia is sometimes required. Psychiatrists can help by ensuring the legal framework pertaining to detention, capacity and consent issues is satisfactorily addressed. Also, the provision of trained mental health nursing staff is conducive to optimising care.
Importantly, these challenges must be overcome to ensure equitable access to crucial investigations for all patients. The overwhelming benefits of early diagnosis and correct treatment with immunotherapy must be prioritised throughout, regardless of the patient's initial treating speciality or hospital location.
Currently, antibody testing via highly specialised national reference laboratories is the only option in many contexts, and can necessitate a turnaround time of several weeks. In the future, accessibility of testing will grow as local laboratories develop their own testing capabilities for the neuronal antibodies most commonly implicated in autoimmune encephalitis.Reference Goodfellow and Mackay34
If delay in obtaining results is encountered in the context of a patient with a worsening presentation (e.g. new neurological signs) and/or the suspicion of an organic aetiology is high, do not wait for the result.Reference Rössling and Prüss35 Arrange a medical admission in liaison with neurology, so the patient can benefit from specialist evaluation (including other investigations) and monitoring, and preliminary treatment can be commenced.Reference Venkatesan and Geocadin36
Other investigations
Routine blood test results (including C-reactive protein and white cell count) are most often within normal limits in cases of anti-NMDAR encephalitis.Reference Liu, Liang, Liu, Luo, Liu and Fan37 Neuroimaging results are also most often normal. For example, MRI of the head was found to be normal in 67–89% of cases.Reference Irani, Bera, Waters, Zuliani, Maxwell and Zandi7,Reference Titulaer, McCracken, Gabilondo, Armangué, Glaser and Iizuka15 When abnormalities are found, they are non-specific, e.g. mild or transient white matter changes in any region of the brain.Reference Lee and Lee38 Compared with MRI, computed tomography imaging of the head provides inferior detail for detection of any central nervous system inflammatory changes that may be seen in autoimmune encephalitis, and therefore MRI is much preferred.Reference Granerod, Davies, Mukonoweshuro, Mehta, Das and Lim39 Notwithstanding, as a widely and rapidly accessible modality, computed tomography remains useful for urgent exclusion of gross central nervous system pathology, such as space-occupying lesions and intracranial haemorrhage. EEG findings are abnormal in 90% of anti-NMDAR encephalitis cases,Reference Titulaer, McCracken, Gabilondo, Armangué, Glaser and Iizuka15 but are generally non-specific (focal or diffuse slowing, disorganised or epileptic activity). Nevertheless, it is suggested that an ‘extreme delta brush’ pattern is a unique feature of anti-NMDAR encephalitis.Reference Schmitt, Pargeon, Frechette, Hirsch, Dalmau and Friedman40
Crucially, therefore, normal results from any, or even all, of these investigations (routine blood tests, computed tomography, MRI and EEG) do not rule out a possible diagnosis of anti-NMDAR encephalitis. This reinforces the diagnostic importance of antibody testing in serum and CSF in suspected cases.
In confirmed anti-NMDAR encephalitis cases, whole-body imaging for tumours should be conducted.Reference Dalmau, Lancaster, Martinez-Hernandez, Rosenfeld and Balice-Gordon9,Reference Lee and Lee38 Specifically, ovarian teratoma in female adolescents and young adults should be searched for by means of ultrasound scan and MRI of the pelvis.
Diagnostic criteria
Clinical criteria for probable and definite anti-NMDAR encephalitis were developed by expert consensus in 2016, with the aim of advancing earlier diagnosis and immunotherapy (Box 5).Reference Graus, Titulaer, Balu, Benseler, Bien and Cellucci41
Box 5 Diagnostic criteria for anti-NMDAR encephalitis (reproduced with permission from Graus et al).Reference Graus, Titulaer, Balu, Benseler, Bien and Cellucci41
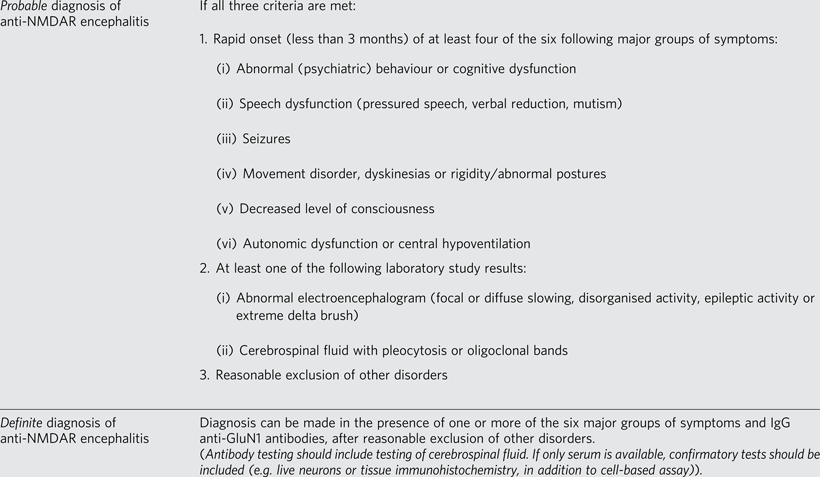
Notably, these criteria adopt a neurology focus, giving rise to questioning of their practical utility for psychiatrists in a mental health setting.Reference Pollak, Lennox, Müller, Benros, Prüss and van Elst1 Of specific concern is the fact that they do not support diagnosis in those presenting with primarily or exclusively psychiatric symptoms, despite evidence that such individuals exist.Reference Kayser, Titulaer, Gresa-Arribas and Dalmau42
Treatment of anti-NMDAR encephalitis
Treatment of encephalitis
Thus far, treatment of anti-NMDAR encephalitis has been based on expert consensus experience (rather than higher-quality evidence such as randomised controlled trials).Reference Rössling and Prüss35,Reference Bartolini43 On the whole, early and aggressive treatment results in better outcomes.Reference Nosadini, Mohammad, Ramanathan, Brilot and Dale44
First-line therapy is usually high-dose corticosteroids (initially intravenous then oral) and intravenous immunoglobulins or plasma exchange.Reference Bartolini43 If there is an inadequate response (typically seen in 50% of casesReference Titulaer, McCracken, Gabilondo, Armangué, Glaser and Iizuka15), rituximab (a monoclonal antibody treatment that targets B cells, thus reducing antibody production) is given as second-line therapy.45 Cyclophosphamide is reserved as a further line of therapy in treatment-resistant cases.Reference Shin, Lee, Park, Jung, Jung and Lee46
Parallel to immunotherapy, if a tumour (e.g. ovarian teratoma) is found, surgery is performed to excise it.Reference Bartolini43
Acute behavioural management
Liaison neuropsychiatry may be called upon to advise on symptomatic management of agitation or psychosis, the mainstay of which will be ensuring the safety of the patient with specialist one-to-one nursing. As mentioned, detention under mental health legislation and treatment under mental capacity legislation will likely be required.
Caution must be employed with regards to the use of psychotropic medication, as this can complicate the fluctuating clinical picture; for example, benzodiazepines may exacerbate respiratory depression and impaired consciousness.Reference Kuppuswamy, Takala and Sola47–Reference Monteiro, Barreto, Rocha, do Prado, Garcia and Correa49 In addition, there may be an association between use of antipsychotics and neuroleptic malignant syndrome in anti-NMDAR encephalitis.Reference Lejuste, Thomas, Picard, Desestret, Ducray and Rogemond16 Overall, these risks need to be balanced against the potential benefit of alleviating distressing symptoms and hazardous behaviour. Importantly, if antipsychotics are used, it is best to gradually discontinue them once the encephalitis is under control, so as to reduce the risk of metabolic side-effects (compounded by steroids).
Prognosis
A validated predictive prognosis tool exists, called the anti-NMDAR Encephalitis One-Year Functional Status (NEOS) score.Reference Balu, McCracken, Lancaster, Graus, Dalmau and Titulaer50 It is scored on five categorical variables, with the presence of each worsening prognosis: intensive care unit admission, treatment delay of >4 weeks, lack of clinical improvement within 4 weeks, abnormal MRI and CSF white blood cell count of >20 cells/μL.
Following acute recovery from anti-NMDAR encephalitis, transfer to a specialist neuro-rehabilitation facility is often appropriate. Baseline and repeated neurocognitive assessments assist in comprehensive monitoring of the patient's functional recovery. Over 18 to 24 months, with treatment, eight out of ten cases make a gradual, but significant recovery.Reference Titulaer, McCracken, Gabilondo, Armangué, Glaser and Iizuka15 Prolonged deficits can include executive dysfunction, impulsivity, disinhibition and sleep abnormalities. Patients often have little memory of their illness.
Relapses occur (12% risk within 2 years), more often in cases not associated with a tumour at presentation, and the majority are of a less severe nature compared with the index illness.Reference Titulaer, McCracken, Gabilondo, Armangué, Glaser and Iizuka15 Relapses require further treatment with immunotherapy. Notably, a quarter of relapses present with psychiatric symptoms only.Reference Kayser, Titulaer, Gresa-Arribas and Dalmau42 Therefore, psychiatrists need to be alert to this fact in someone with a past medical history of anti-NMDAR encephalitis.
Case reflections
In retrospect, the case described many of the red flags for autoimmune encephalitis, and nearly all of the ‘SEARCH For NMDAR-A’ diagnostic clues were indeed present. This emphasises the importance of raising awareness of features suggestive of anti-NMDAR encephalitis among psychiatrists, to enable its early recognition.
Furthermore, this case demonstrates the importance of a fully comprehensive and systematic specialist work-up, including serum/CSF antibody testing, in suspected cases of anti-NMDAR encephalitis. In this instance, the patient's MRI head and EEG results were normal, despite the relatively advanced stage of the encephalitis at the time of these investigations. The true diagnosis was only revealed by antibody testing of serum and CSF.
Finally, doctors must be mindful of the risk of diagnostic overshadowing in such cases where psychiatric and physical elements coexist, and be prepared to advocate for their patients to ensure they receive appropriate medical care.
Conclusion
Anti-NMDAR encephalitis typically first presents with a complex constellation of acute-onset psychiatric symptoms, such as agitation, psychosis and catatonia. As in the case described, those with the condition can first present to psychiatry. Therefore, psychiatrists have a crucial role in the early recognition of anti-NMDAR encephalitis, and should be familiar with the features suggestive of it in the patient's history, mental state and neurological examination. Clinical suspicion should trigger early discussion with neurology colleagues, and prompt testing of serum (and ideally CSF) for NMDAR antibodies. Collaborative working supports early diagnosis and timely immunotherapy, resulting in improved long-term outcomes.
In future, routine screening for autoantibodies in patients presenting with psychiatric symptoms may become common practice, and studies are ongoing assessing the potential role of immunotherapy within psychiatry.
About the authors
Matthew Beattie is a specialty doctor with the Adult Mental Health Liaison Service at Queen Elizabeth University Hospital, NHS Greater Glasgow & Clyde, Scotland, UK. John Goodfellow is a consultant neurologist based in the Neuroimmunology Laboratory at Queen Elizabeth University Hospital, NHS Greater Glasgow & Clyde, Scotland, UK. Maria Oto is a consultant neuropsychiatrist with the Adult Mental Health Liaison Service at Queen Elizabeth University Hospital, NHS Greater Glasgow & Clyde, Scotland, UK. Rajeev Krishnadas is a consultant psychiatrist with Esteem (Early Intervention in Psychosis Service) at Stobhill Hospital, NHS Greater Glasgow & Clyde, Scotland, UK.
Data availability
Data availability is not applicable to this article as no new data were created or analysed.
Acknowledgement
Written informed patient consent was obtained for publication of the de-identified case, its discussion and Box 1. We are grateful to the patient for kindly sharing her experience.
Author contributions
M.B. developed the concept of the article, planned and prepared the initial draft, and was primarily responsible for subsequent redrafting and revision of the final manuscript. J.G., M.O., and R.K. provided expert input, and reviewed and edited the inital and final manuscript..
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
J.G. is Chief Executive Officer of Infimmune Ltd, a biotechnology company developing treatments for autoimmune disorders. The other authors have nothing to disclose.





eLetters
No eLetters have been published for this article.