Healthcare students are exposed to a wide variety of stressors on a day-to-day basis. These include study-related stressors throughout their education, continuous exposure to human suffering and further work-related stressors towards the end of their professional education (Box 1) (Evans Reference Evans and Kelly2004; Gazzaz Reference Gazzaz, Baig and Al Alhendi2018; Hill Reference Hill, Goicochea and Merlo2018). Exposure to these chronic stressors has been reported to affect the physical and mental well-being of healthcare students, predisposing them to sleep disorders (Azad Reference Azad, Fraser and Rumana2015), burnout (Cecil Reference Cecil, McHale and Hart2014), depression and anxiety (Mao Reference Mao, Zhang and Liu2019). Furthermore, it can lead to a decline in their academic and clinical performance, sometimes to the extent that they discontinue their studies (Dyrbye Reference Dyrbye2011; Gazzaz Reference Gazzaz, Baig and Al Alhendi2018).
BOX 1 Common stressors for healthcare students
Previous evidence tells us that the healthcare students are highly likely to be exposed to three main types of stressors.
Academic stressors
Healthcare students have a laborious academic workload, with long hours of study, a huge volume of information to assimilate and strenuous academic work. This usually makes them struggle with time management for studies. They also sit frequent examinations in a tough and competitive atmosphere where the fear of failure is common.
Clinical stressors
Healthcare students are exposed to a wide range of clinical stressors, such as frequently witnessing human suffering and death. One might argue that this is what they voluntarily signed up for, but during their training they might lack the practical skills to handle such scenarios, reflecting a mental or physical gap in translating skills from theory to practice. The clinical environment is often perceived to be tense and filled with negative attitudes, particularly if the students are being openly, or even subtly, criticised in front of stakeholders – patients, relatives and healthcare professionals.
Psychosocial stressors
Healthcare students can find it hard to strike a balance between life at work and life outside of work, particularly because of the academic load. They are quite new to managing relationships at work and in their private lives and usually have concerns related to finances and their future
(Edwards Reference Edwards, Burnard and Bennett2010; Gazzaz Reference Gazzaz, Baig and Al Alhendi2018; Hill Reference Hill, Goicochea and Merlo2018)The ability to stay firm during adversity and then bounce back from difficult events is a part of the human psyche and is known as resilience. However, our day-to-day experience suggests that several human abilities need strengthening to keep pace with daily challenges. Since there are well-identified chronic stressors that have a significant impact on medical, dental, nursing, psychology and social work students, the concept of resilience has gained importance over the past few years in the field of health professional education (Wright Reference Wright and Richmond Mynett2019). Resilience is generally recognised as modifiable and, as such, can be enhanced by interventions (Southwick Reference Stahl and Goldstein2011). Although many interventions have been tested that are aimed at fostering resilience in healthcare students in various fields, the underlying evidence has not been rigorously assessed. This is the aim of the review in this issue's Cochrane Corner (Kunzler Reference Kunzler, Helmreich and Chmitorz2020a). In this commentary, we will discuss those findings and put them into further context.
Resilience interventions
The resilience interventions evaluated in the review are based on a number of psychotherapeutic approaches (Box 2).
BOX 2 Interventions aimed at fostering resilience
Underlying therapeutic approaches:
• cognitive–behavioural therapy (Abbott Reference Abbott, Klein and Hamilton2009)
• mindfulness-based therapy (Geschwind Reference Geschwind, Peeters and Drukker2011)
• acceptance and commitment therapy (Ryan Reference Schünemann, Brożek and Guyatt2014)
• problem-solving therapy (Bekki Reference Bekki, Smith and Bernstein2013)
• stress inoculation therapy (Farchi Reference Farchi and Gidron2010)
Resilience-training interventions have mostly been administered face to face in both individual and group-based settings. The methods commonly used in these interventions include:
• role-play
• discussions
• homework
• practical exercises
• psychoeducation (providing information about the concept of resilience) and specific training (providing information about a specific technique, such as reframing of thoughts)
Cognitive–behavioural therapy
Cognitive–behavioural therapy (CBT) teaches us that when people face difficulties, they show maladaptive actions and/or experience negative states of mood if their thought processes are not rational (Beck Reference Beck1979). This is supported by other theories related to stress and resilience which conclude that, surprisingly, it is not the stress itself, but how we think about it that leads to stress reactions (Lazarus Reference Lazarus and Folkman1987; Kalisch Reference Kalisch, Müller and Tüscher2015). Thus, if we modify how we think about difficult situations into more adaptive patterns, we will produce better adaptive stress responses (Beck Reference Beck1964). Hence, CBT-based resilience interventions work by challenging maladaptive patterns of thought and teaching healthy coping strategies. The resilience factors targeted by CBT-based resilience interventions are: (a) cognitive flexibility – having flexible thought processes in response to stressful situations; (b) active coping – having healthy coping skills ready for adverse situations (Kunzler Reference Kunzler, Helmreich and Chmitorz2020a).
Mindfulness-based therapy
In simple terms, mindfulness means having a judgement-free awareness of the present moment and of the mental phenomena being experienced (thoughts, bodily sensations and emotions) (Sood Reference Southwick, Pietrzak, White, Litz, Charney and Friedman2014; Stahl Reference Wilson, Hampton and Hensley2019). People who practice mindfulness are known to adapt efficiently to stress as they learn to accept all that happens in the present moment (Grossman Reference Grossman, Niemann and Schmidt2004; Shapiro Reference Sood, Sharma and Schroeder2005).
Acceptance and commitment therapy
Hayes et al noted that symptoms of mental illness, particularly during stressful situations, can arise because the individual has an inflexible mindset in that situation (Hayes Reference Hayes, Luoma and Bond2006). Thus, they concluded that interventions based on acceptance and commitment therapy might promote multiple resilience factors. It was noted that teaching acceptance and mindfulness skills as well as commitment and behaviour-change skills are fruitful for fostering resilience. It is thought that individuals are better adjusted to stressful conditions after interventions based on acceptance and commitment therapy because they are taught to accept a full range of emotions (Hayes Reference Hayes, Luoma and Bond2006).
Problem-solving therapy
In plain language, and as the name suggests, this form of therapy is based on problem-solving theory. Problem-solving theory suggests that solving problems effectively can decrease the harmful effects of adversity and stress on our well-being. It does so by mediating and/or moderating the effects of stressors on our emotional distress. Thus, interventions based on problem-solving can increase the ‘active coping’ resilience factor by enhancing one's positive orientation to problems and boosting planful problem-solving skills (Nezu Reference Nezu, Nezu and D'Zurilla2012).
Stress inoculation therapy
Stress inoculation therapy (also known as stress inoculation training) is a type of CBT that involves exposing people to milder forms of stresses so that they can learn to strengthen their coping strategies. It is also believed that such exposure can boost an individual's confidence in using coping skills. Thus, the resilience factor that is enhanced by resilience interventions based on stress inoculation therapy is self-efficacy (Meichenbaum Reference Meichenbaum2007).
The Cochrane review
Summary
The Cochrane review under consideration (Kunzler Reference Kunzler, Helmreich and Chmitorz2020a) evaluates the effects of resilience-training interventions on resilience, anxiety, depression, stress and quality of life or well-being in healthcare students. From 30 trials conducted mostly in high-income countries, the review draws the conclusion that there is evidence, although of very low level of certainty, that such interventions are beneficial in fostering resilience and related aspects of mental wellness.
The framework of the study
The population of interest in the review is healthcare students aged 18 and above. Two categories of healthcare students were involved but no subgroup analysis was performed because of the limited number of studies. One category included those who are training to become healthcare professionals and will be directly delivering clinical care (i.e. medical, nursing, midwifery and paramedical students). Although not explicitly stated, the search criteria included dental professional students as well (dentistry students and those training to become dental hygienists). The second category included those who are training to become allied healthcare professionals (i.e. psychology, social work and physical therapy students).
The review authors also included studies involving mixed samples of both healthcare and non-healthcare students. However, they justified this decision by saying that they either contacted the authors of trials for data clarification about healthcare students in those studies or the healthcare students’ data were reported separately in the studies.
The included interventions, as mentioned in Box 2, were well-defined, but had no limitations on duration, content, mode of delivery or setting in which they were delivered. The review authors further defined these interventions as ones aimed at fostering resilience or related concepts of post-traumatic growth or hardiness, by making modifiable resilience factors stronger than before. Although allowing for the inclusion of several more studies, this choice also leads to the significant heterogeneity observed in the results of this review.
The comparator conditions considered in the review were likewise heterogeneous and included no intervention, waiting-list controls, active controls, attention controls and treatment as usual (TAU).
Over half of the included studies (18/30) did not record participants’ baseline health status; this could be reason for bias because we do not know what their mental health before study enrolment was like or whether being chronically unwell was the reason for them enrolling in the first place.
It is interesting to note that not all trials of these resilience-training interventions assessed resilience among their outcomes. Nevertheless, primary outcomes of the review were ‘resilience’, as measured on resilience scales, ‘mental health and well-being’ (under the categories of depression, anxiety, stress/stress perception, and quality of life/well-being) and ‘adverse events’. Again, these primary outcomes seem very broad. The secondary outcomes were ‘resilience factors’: self-efficacy, self-esteem, active coping, optimism, positive emotions, hardiness and social support (Fig. 1).
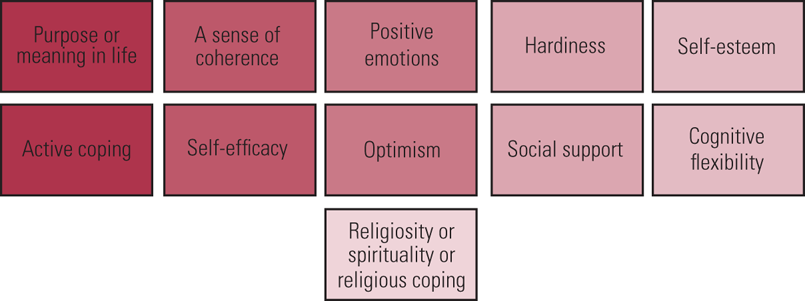
FIG 1 Well-evidenced modifiable psychosocial resilience factors identified in the review (Kunzler Reference Kunzler, Helmreich and Chmitorz2020a).
Study types and search strategy
The authors intended to use randomised controlled trials (RCTs) and cluster-RCTs in their review, but they could not identify any of the latter. They searched a wealth of research databases (Box 3). They first ran the search in 2016 for their protocol paper on resilience enhancement in adults (Helmreich Reference Helmreich, Kunzler and Chmitorz2017), then revised the inclusion criteria to focus on healthcare students and also performed top-up searches in 2019 before publishing the current review in 2020. A merit of their search strategy is that not only did they use the Cochrane Highly Sensitive Search Strategy to make sure they identified relevant trials in the major databases, but they also adapted their search syntax and items for several other databases, less commonly investigated, without restricting the searches by publication status, format or language.
BOX 3 Research databases
A research database is an organised collection of information on a website. Examples of such information include periodical articles, book chapters, graphics and multimedia, which can be easily searched on that platform to retrieve information. Databases can be subject oriented or general. The database may have summary of an article, the full text or just a citation. Some databases are free to access, but others charge a subscription fee or can be accessed through institutions and have a wealth of other features that make searching for articles easier. Commonly used research databases include PubMed, Scopus, Web of Science, Education Resources Information Center (ERIC) and the Institute of Electrical and Electronics Engineers’ IEEE Xplore.
The authors of this specific Cochrane review (Kunzler Reference Kunzler, Helmreich and Chmitorz2020a) conducted a very extensive search of numerous databases, including: the Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews (CDSR) and Database of Abstracts of Reviews of Effects (DARE), MEDLINE Ovid, Embase Ovid, PsycINFO Ovid, CINAHL EBSCOhost, PSYNDEX EBSCOhost, Web of Science Core Collection Clarivate, International Bibliography of the Social Sciences ProQuest (IBSS), Applied Social Sciences Index & Abstracts ProQuest (ASSIA), ProQuest Dissertations & Theses (PQDT), Epistemonikos, Education Resources Information Center (ERIC EBSCOhost), Current Controlled Trials (now the ISTRCN registry), ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP).
The authors justify including only studies from January 1990 onwards by mentioning that the concept and operationalisation of resilience was not developed before 1990s. However, resilience is an ancient concept which has been discussed by writers, philosophers, scholars and teachers informally for centuries (Agaibi Reference Agaibi2018). Nevertheless, they do provide the counterargument that even the studies they found from 1990 to 2014 lacked homogeneity, and having a broader time frame would have made it difficult for them to have definite outcome measures.
The authors went beyond their search strategy by inspecting the reference lists of all the RCTs and previous reviews retrieved, and by contacting the researchers of specific trials to confirm whether there were any ongoing or unpublished studies. They also contacted the authors of some studies if they felt that data were missing or simply unclear.
Risk of bias assessment
The review team allocated two authors to assess the risk of bias of all the studies they included. They used the criteria published in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins Reference Higgins, Altman and Sterne2011) and resolved any disagreements by discussing or consulting another author from their team. They assessed every study across the domains of selection bias, performance bias, detection bias, attrition bias and reporting bias.
Analysis
Two authors, working independently, selected the studies, extracted data and rated the quality of evidence certainty utilising the GRADE approach (Schünemann Reference Schünemann2013). The feasibility of the selection criteria was assessed by screening 500 studies to obtain an acceptable interrater reliability (Box 4) and the review team felt there was a decent agreement between the review authors and therefore no need to clarify or refine the selection criteria. Similarly, data extraction and management were tested on 10 random studies, and this showed significant agreement between the authors who were reviewing the studies. In cases where they felt no consensus was reached after discussion, a third review author provided arbitration.
BOX 4 Interrater reliability
Interrater reliability is the level of agreement between authors or raters of a study. If everyone agrees, the interrater reliability is 1 or 100%. If everyone disagrees, then the interrater reliability is 0 or 0%. To compute the interrater reliability simple methods such as percentage agreement are used. Calculating this value can be complex, depending on the number of raters and the type of data.
It was clear to the authors that a variety of measurement scales were used to measure resilience and its related constructs. Hence, for continuous data, they used standardised mean difference (s.m.d.) with 95% confidence intervals (CIs), and calculated effect sizes (Cohen's d) in all pairwise meta-analyses. They determined the magnitude of effect using the following values: 0.2, indicating small effect; 0.5, indicating a moderate effect; and 0.8, indicating a large effect (based on the Cochrane Handbook; Schünemann Reference Shapiro, Astin and Bishop2019).
The authors employed the chi-squared test, tau-squared and I 2 statistic for the assessment of statistical heterogeneity between the studies. However, it is important to note that the inherent nature of these studies is that they had small sample sizes, and chi-squared has limited power in such cases.
The authors used funnel plots to assess any publication bias and Egger's test to test for asymmetry of funnel plots.
The authors synthesised results in tabular as well as narrative form and used the Cochrane Collaboration Review Manager 5 (RevMan 5) or R for statistical analyses. They then summarised the numerical results of the studies in pairwise meta-analyses to get pooled effects of the resilience interventions. The authors used GRADEpro software (Schünemann Reference Schünemann2013) to generate a summary of findings table. Owing to the limited number of studies that could be included, the authors were not able to perform a subgroup analysis to examine key characteristics of the studies that might be linked to the substantial heterogeneity found for many outcomes. They were also not able to perform a subgroup analysis for training intensity or most of their planned sensitivity analyses to test how robust the findings of the review were, and this was again due to the limited number of studies.
Results
The authors included 30 RCTs in the review, only 6 of which were set in the middle-income countries – the rest were set in high-income countries. So, we can say that the findings of the review cannot be fully generalised to all the nations of the world. In our opinion, the unavailability of resources as well as the lack of access to training and supervision are common barriers to conducting trials of these types of mental health intervention in low- and middle-income countries. Besides, the mental health and social needs are quite complex in such nations, and there is often lack of knowledge and negative beliefs about such interventions. These views are supported by a systematic review in which the authors explored barriers to the implementation of mental health programmes in low- and middle-income countries (Esponda Reference Esponda, Hartman and Qureshi2020).
Twenty-two of the RCTS included by Kunzler et al were solely focused on healthcare students, with 50% of them conducted in a school (e.g. nursing school, school of medicine) or university setting. One of the biases that is evident in this review is that about two-thirds of the trials’ participants were female, possibly reflecting a degree of ‘gynocentrism’ (Box 5) in the study conclusions. This might be because there are higher numbers of women studying to be healthcare professionals, as was evident in an analysis of 104 countries by the World Health Organization, which found that women form 70% of the workers in the health and social sector (Boniol Reference Boniol, McIsaac and Xu2019).
BOX 5 Androcentrism and gynocentrism in research
Androcentrism is a term used to describe a bias in research when the researchers consider mostly the perspectives of men while excluding other perspectives, particularly if a greater number of men took part in the study compared with women. Gynocentrism has the opposite meaning: the focus is on the woman's perspective. Both phenomena can be prevented by having an equal proportion of men and women in research studies.
In almost half of the studies in this review (Kunzler Reference Kunzler, Helmreich and König2020a) 63.3% of participants were women; that proportion rose to 67.3% in around a quarter of the studies. Since the outcomes were questionnaire based and considered participants’ perspectives, almost three-quarters of such perspectives came from females. Thus, it becomes difficult to generalise the results of these studies to the real world.
There was a difference in the intensity and mode of delivery of the interventions across the trials. Seven studies did not specify the funding body, raising questions as to whether the outcomes might have been influenced by the training body. Most trials were at unclear or high risk of bias, and the key issues were in terms of detection, performance, reporting and attrition biases.
The authors found evidence that healthcare students who received resilience training reported higher resilience levels compared with controls (s.m.d. = 0.43, 95% CI 0.07 to 0.78), as well as lower levels of anxiety (s.m.d. = −0.45, 95% CI −0.84 to −0.06) and lower levels of stress or perception of stress (s.m.d. = −0.28, 95% CI −0.48 to −0.09). All evidence was assessed to be of very low certainty and the main reasons for downgrading were study limitations, unexplained inconsistency and indirectness.
Interestingly, no impact on depression (s.m.d. = −0.20. 95% CI −0.52 to 0.11) or quality of life or well-being (s.m.d. = 0.15, 95% CI −0.14 to 0.43) was found – although again with very low certainty.
Adverse events were assessed in only four studies, three of which reported their findings. Those three found no adverse effects occurring during the study.
Discussion
This study has clarified a few points about the overall mental health of healthcare students in high-stress study- or work-related environments. First, there is an acknowledgement that resilience is modifiable and so are the levels of anxiety and stress or perception of stress. Connor & Zhang mention that resilience is modifiable on both the individual and the cultural level (Connor Reference Connor and Zhang2006).
Second, as evidenced by several trials included in the review, many researchers and training bodies across the world are trying to engage healthcare students in resilience-building interventions that may be useful for them. It is good to know that some researchers are setting up multicentre trials, for instance a study on resilience of nursing students as well as faculty staff conducted in six universities in the USA (Wilson Reference Wright and Richmond Mynett2021).
Third, no adverse events were found to be associated with the training interventions for healthcare students included in this review (Kunzler Reference Kunzler, Helmreich and Chmitorz2020a). Another systematic review by the same authors which focused on effectiveness of resilience interventions in healthcare professionals, rather than students, also reported no adverse effects of the interventions (Kunzler Reference Kunzler, Helmreich and König2020b). Therefore, even in the absence of a good evidence base supporting training interventions to boost resilience in healthcare students, the lack of any harmful effects appears reassuring. Indeed, mental health apps and virtual reality programs are already used by university students, who report gaining benefit from them, although this often appears to be subclinical or to lack an adequate evidence base (Flett Reference Flett, Hayne and Riordan2019). Furthermore, some psychiatrists suggest that their patients use similar apps alongside standard treatments, although this needs to be done in collaboration with patients, keeping in view their individual considerations (Chiauzzi Reference Chiauzzi and Newell2019). Psychiatry is moving towards prevention through technological interventions rather than just secondary and tertiary treatment (Fusar-Poli Reference Fusar-Poli, Correll and Arango2021).
This review assesses the evidence for the efficacy of resilience-promoting interventions in a population of healthcare students, traditionally known to be under significant stress. It found evidence, although of very low certainty, for a positive effect of resilience training on measures of resilience, anxiety and stress or perception of stress.
The interventions under examination were quite heterogeneous, raising questions about whether they should have been pooled in the first place. Moreover, there was a lack of data on short-, medium- and long-term outcomes, and no mention on whether these interventions are financially viable and sustainable. Finally, the results are difficult to generalise because most of the studies included were carried out in high-income nations. Many healthcare professionals working in high-income countries completed their studies in low- or middle-income countries (O'Dowd Reference O'Dowd2019). So, it may be in the interest of high-income countries to support the resilience training of these students by, for example, investing in or supporting universities in low-income countries.
Nevertheless, the promising findings of this review suggest that further trials are merited, with improved study design (e.g. using a consensus definition of resilience, assessing individual exposure to stressors, including more attention controls and using longer follow-up) and conducted in a greater variety of geographical locations.
Conclusions
The authors have made a commendable effort by collating a large amount of evidence in the field of resilience interventions for healthcare students. If this Cochrane review's findings (Kunzler Reference Kunzler, Helmreich and Chmitorz2020a) were replicated in further, well-conducted, methodologically robust studies, that might provide crucial evidence for the use of resilience training to protect the mental health of people who study or work in high-stress environments. Prevention of mental disorders through such interventions, especially in young people, would lead to several further benefits in terms of staff well-being, less sickness and a related reduction in sick leave. The impact of academic, clinical and psychosocial stressors on healthcare students would be minimised if interventions shown to be efficacious were offered.
Author contributions
S.T. is responsible for the conception, design and the write up of the manuscript. B.K.A. is responsible for the boxes, the literature review, and for supporting with the manuscript design and its revision.
Funding
This article received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.





eLetters
No eLetters have been published for this article.