LEARNING OBJECTIVES
-
Appreciate the different ways in which acute and transient psychoses have been conceptualised historically and recognise how these relate to current nosologies
-
Identify clinical and epidemiological features of acute and transient psychoses and differentiate them from organic psychosis, schizophrenia-spectrum disorders and affective disorders on the basis of ICD-10 and DSM-5 criteria
-
Recognise the increased risk of premature mortality, particularly suicide, associated with acute and transient psychoses, and the difficulty in treating these varied conditions
Ever since Kraepelin introduced in 1896 the nosological dichotomy between dementia praecox (later renamed schizophrenia) and manic–depressive psychosis (i.e. bipolar disorder), efforts to delineate intermediate categories have been made in different psychiatric traditions (Reference WimmerWimmer 1916; Reference KleistKleist 1928; Reference KasaninKasanin 1933; Reference LangfeldtLangfeldt 1939; Reference LeonhardLeonhard 1957), but the evidence drawn on proved inconclusive. This has caused difficulties in classification and nomenclature, mainly for transient psychotic disorders that do not involve prominent affective features, and concealed Reference SchneiderKurt Schneider's (1959) basic question – namely, ‘whether [in such cases] a psychic reaction or a psychosis is present’.
In this article we outline early categories of European psychiatry and describe how acute and transient psychoses have been incorporated and differentiated from schizophrenia and affective disorders in current psychiatric nosography, such as ICD-10 (World Health Organization 1992) and DSM-5 (American Psychiatric Association 2013). We then present empirical data and discuss implications for classification, diagnosis and treatment of these conditions. We leave aside transient psychotic disorders subsumed under the heading of the so-called ‘culture-bound syndromes’, and other intermediate categories such as schizoaffective psychosis.
Early views
Bouffée délirante
The French concept of bouffée délirante was developed by Reference MagnanMagnan (1887) and followers (Legrain and Saury) in the wake of the late 19th-century theory of degeneration. They distinguished transient delusional states characterised by sudden onset and fleeting polymorphic features (délire d'emblée) from more persistent and uniform delusional disorders leading to mental deterioration (délire chronique à évolution systématique).
This description has striking similarities to Reference EyEy's (1954) category of ‘acute delusional psychosis’ based on his ‘organo-dynamic’ theory and listed in the French classification of mental disorders (Reference Garrabé, Cousin, Gelder, Lopez-Ibor and AndreasenGarrabé 2012). To improve diagnostic reliability, French psychiatrists (Reference Pull, Pull and PichotPull 1987) formulated explicit criteria for bouffée délirante, such as: (a) abrupt onset; (b) polymorphic delusions, emotional changes, mood swings, depersonalisation, derealisation and/or hallucinations; (c) complete remission within weeks or a few months; (d) exclusion of organic causation, alcohol and drug misuse; and (e) no psychiatric antecedent except bouffée délirante. Studies of the natural course of bouffée délirante reported varying transition rates to either schizophrenia and related disorders or affective disorders (Reference Weibel and MetzgerWeibel 2005). The use of the diagnosis bouffée délirante has decreased since the 1980s, and it is currently included in studies of first-episode psychosis (Reference Garrabé, Cousin, Gelder, Lopez-Ibor and AndreasenGarrabé 2012).
Cycloid psychosis
Kleist introduced the term zykloide Psychosen (cycloid psychosis) to designate ‘phasic illnesses which come and go autochthonously [sic] like manic depression, frequently in dual, contrasting phases of confused excitement and stupor, or hyperkinesis and akinesis, running their course and leaving behind no residual defects’ (Reference KleistKleist 1928: p. 300). Reference LeonhardLeonhard (1957) added ‘anxiety–happiness psychosis’, which resulted from the combination of ‘anxiety psychosis’ and ‘revelation psychosis’. In Leonhard's view, cycloid psychosis was different from both schizophrenia and manic depression (now called bipolar disorder), and comprised three clinical forms: anxiety–happiness psychosis, confusion psychosis and motility psychosis, which involved an impairment of affect, thinking and psychomotor activity respectively. In Anglophone psychiatry, Reference Perris, Brockington, Perris, Struwe and JanssonPerris & Brockington (1981) provided operational criteria for diagnosis of cycloid psychosis, such as sudden onset and polymorphic symptoms, which were eventually incorporated into the checklist of the ICD-10 category ‘acute and transient psychotic disorders’ (ATPDs; World Health Organization 1992).
Cycloid psychosis is prevalent in women and accounts for many cases of post-partum psychosis; antipsychotic medication must be used cautiously owing to elevated risk of neuroleptic syndrome and catatonia (Reference Beckmann, Franzek, Henn, Sartorius and HelmchenBeckmann 2001). Follow-up studies have shown that cycloid psychosis fares better than schizophrenia in both course and outcome (Reference LeonhardLeonhard 1957; Reference Jabs, Krause and AlthausJabs 2004). Reference CuttingCutting (1990) claimed that cycloid psychosis conforms more to an atypical variant of affective disorder. Twin and family studies have found that cycloid psychosis has only a modest hereditary basis; there seems to be greater evidence that it arises when complications during pregnancy and at birth affect the early stages of brain development (Reference Beckmann, Franzek, Henn, Sartorius and HelmchenBeckmann 2001).
Reactive (psychogenic) psychosis
Drawing on the methodological distinction between ‘explanation’ and ‘understanding’, Reference JaspersJaspers (1913) described the concept of reactive psychosis, encompassing clinical conditions with affective, confusional and paranoid features triggered by a psychological trauma. Symptoms in reactive psychosis were meaningfully connected to the extent of the traumatic event, the semantic or symbolic role (i.e. defence, escape, wish fulfilment) and the content. Although of clinical and heuristic value, Jaspers’ criteria were criticised for their subjective character (Reference SchneiderSchneider 1959).
The concept of reactive psychosis was further developed in Scandinavia (Reference WimmerWimmer 1916; Reference Hirsh and ShepherdStrömgren 1974), but its validity was hampered by follow-up studies showing high transition rates to either schizophrenia or affective disorders (Reference Ungvari, Mullen, Bhugra and MunroUngvari 1997). In continental (European) and British psychiatry, diffusion of the diagnosis of reactive psychosis was hindered by strong opposition to the notion of ‘psychological causation’ and controversies about the separation between reactive and endogenous depression (Reference LewisLewis 1972). Reference SchneiderSchneider's (1959) view that all psychoses have a ‘somatic’ basis was also influential and contributed to the neglect of reactive psychosis in modern psychiatric classifications. The concept of psychological reactivity, on which reactive psychosis was based, has been redefined in terms of stress vulnerability, life events, and social and cultural differences; nowadays interest in psychological trauma tends to concentrate on post-traumatic stress disorder.
Schizophreniform psychosis
The term ‘schizophreniform psychosis’ was coined by Reference LangfeldtLangfeldt (1939) to denote schizophrenia-like states with rapid remission in response to ‘shock treatment’. Acute onset, precipitating stress, mental confusion, affective symptoms and extroversion differentiated this category from schizophrenia. Related conditions are the ‘acute schizoaffective psychoses’ described by Reference KasaninKasanin (1933) in people presenting with mixed symptoms triggered by stressful events, and Reference LabhardtLabhardt's (1963) schizophrenieähnlichen Emotionspsychosen (schizophrenia-like emotion psychoses).
In North American psychiatry, research on outcome prediction helped to define the concept of ‘good-prognosis schizophrenia’ (‘remitting schizophrenia’) (Reference VaillantVaillant 1962). The DSM has, since its third edition, included the category of ‘schizophreniform disorder’, characterised by typical schizophrenic symptoms with a duration of 1–6 months. The following ‘specifiers’ have been added to indicate prognostic factors for schizophreniform disorder that may be associated with a favourable outcome: onset within 4 weeks; confusion or perplexity; good social and occupational functioning; and absence of blunted or flat affect. Yet, the diagnostic criteria for schizophrenia included occupational and social dysfunction and a tendency to a persistent course (at least 6 months).
Current psychiatric classifications
Influenced by findings of the World Health Organization (WHO) collaborative study on acute psychoses (Reference Cooper, Jablensky, Sartorius, Stefanis, Rabavilas and SoldatosCooper 1990), the category of ATPDs (Table 1) appeared in ICD-10 (WHO 1992) within the F2 group ‘schizophrenia, schizotypal and delusional disorders’. The ICD-10 stated that: ‘The limited data and clinical traditions […] do not give rise to concepts that can be clearly defined and separated from each other […]. The nomenclature of these acute disorders is as uncertain as their nosological status’ (WHO 1992: pp. 99–100). ATPDs were characterised by: (a) acute onset (within 2 weeks); (b) early remission (complete recovery is expected within 1–3 months); (c) polymorphic, schizophrenic or predominantly delusional syndromes; and (d) association with ‘acute stress’, regarded as events stressful to most people, such as bereavement, unexpected loss of a partner, job or marriage, or the psychological trauma of combat, terrorism or torture, occurring less than 2 weeks before the onset of psychotic symptoms.
TABLE 1 Main differences between ICD-10 ‘acute and transient psychotic disorders’ and DSM-5 ‘brief psychotic disorder’
The ATPD category comprises six subtypes: ‘acute polymorphic psychotic disorder’ (F23.0) refers to bouffée délirante and Kleist's and Leonhard's cycloid psychosis, featuring varied delusions, hallucinations, perceptual changes, perplexity and emotional turmoil (i.e. intense feelings of happiness or ecstasy, or overwhelming anxiety or marked irritability) that shift daily or even more frequently, and can include ‘schizophrenic symptoms’ (F23.1); ‘acute schizophrenia-like psychotic disorder’ (F23.2) replaced the ICD-9 category ‘acute schizophrenic episode’; ‘acute predominantly delusional psychotic disorder’ (F23.3) involves relatively stable delusions, usually of persecution or reference, and auditory hallucinations; ‘other’ and ‘unspecified’ ATPDs (F23.8–9) are residual classes.
DSM-5 (American Psychiatric Association 2013) listed the category of brief psychotic disorder (Table 1), which features florid psychotic symptoms such as delusions, hallucinations, disorganised speech, and grossly disorganised or catatonic behaviour, lasting less than 1 month. It may follow ‘marked stressors’ or have its onset in the post-partum period. The diagnostic criteria for schizophreniform disorder are unchanged and symptom duration is intermediate between brief psychotic disorder and schizophrenia.
Differential diagnosis
The diagnostic criteria for both ATPD and brief psychotic disorder exclude substance-induced psychosis, organic psychosis due to medical conditions, and affective disorders. There may be states of perplexity and inattention, but not so marked or persistent as to suggest delirium, dementia or substance-induced psychosis; in these cases a differential diagnosis is often difficult. To rule out organic causation and substance misuse, a comprehensive clinical assessment, comprising laboratory testing and neuroimaging, is recommended.
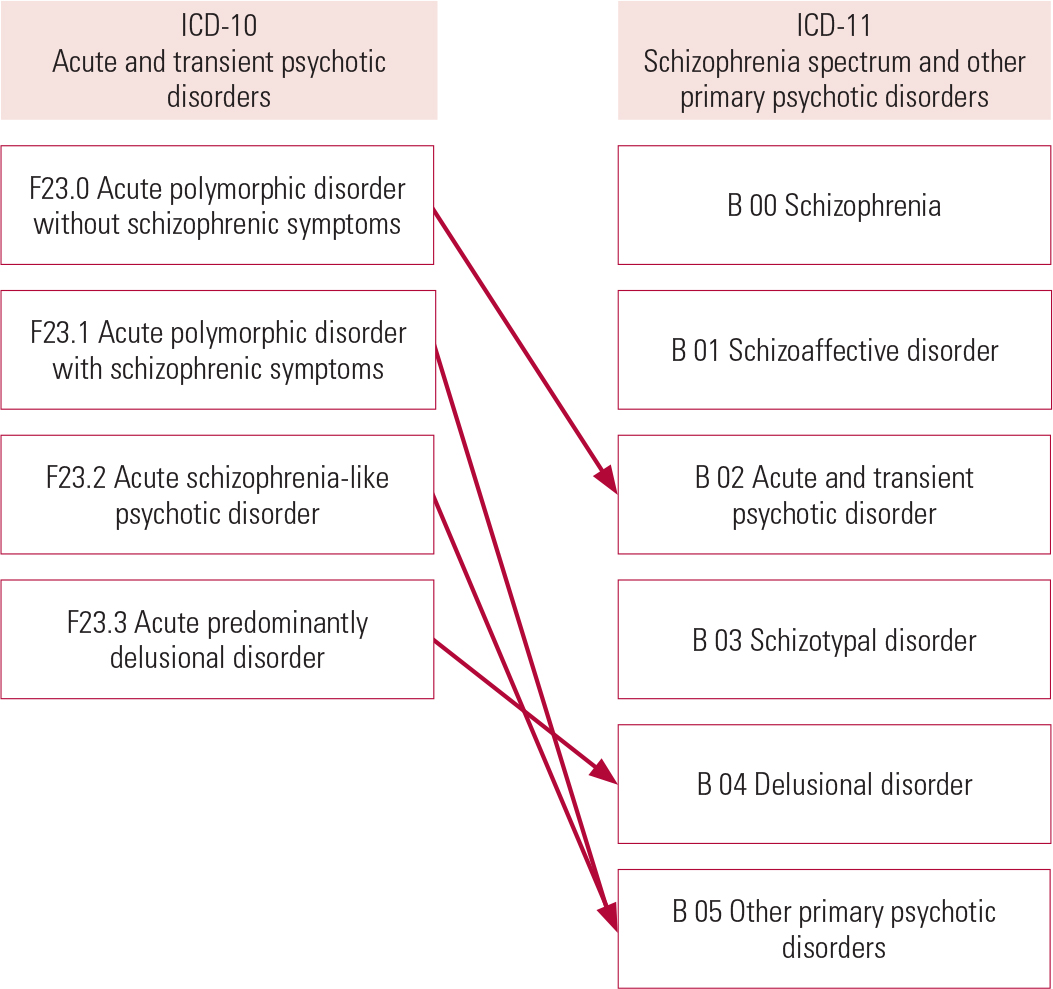
The ATPD subtypes (Fig. 1) with schizophrenic symptoms are set apart from schizophrenia by temporal criteria of less than 1 month's duration, as the ICD-10 diagnosis of schizophrenia requires duration longer than 1 month; the subtypes characterised by polymorphic and predominantly delusional features last less than 3 months. If delusions last longer, the diagnosis will change to ‘persistent delusional disorder’ (F22); if only hallucinations persist for more than 3 months, the diagnosis will be ‘other non-organic psychotic disorders’ (F28).

FIG 1 Differential diagnosis of acute and transient psychoses adapted from ICD-10 (World Health Organization 1992).
Differential diagnosis may also involve transient psychotic symptoms in post-traumatic stress disorder, borderline personality disorder, anorexia nervosa and panic attacks.
Concordance between ICD and DSM
Brief psychotic disorder is an uncommon condition, accounting for just 2–7% of presentations of first-episode psychosis (Reference Korver-Nieberg, Quee and BossKorver-Nieberg 2011; Reference Nugent, Paksarian and MojtabaiNugent 2011; Reference Kingston, Scully and BrowneKingston 2013). Brief psychotic disorder is often a provisional diagnosis (owing to high rates of transition to schizophrenia, schizoaffective disorders or affective disorders) (Reference Nugent, Paksarian and MojtabaiNugent 2011; Reference Kingston, Scully and BrowneKingston 2013), but for patients who do not develop longer-term illness, symptoms seem to be less severe than in schizophrenia and outcome for each episode is favourable (Reference Korver-Nieberg, Quee and BossKorver-Nieberg 2011).
Comparative studies have reported that ATPD extend beyond the category of brief psychotic disorder (Reference Jørgensen, Bennedsen and ChristensenJørgensen 1997; Reference van der Heijden, Tuinier and Kahnvan der Heijden 2004). Reference Marneros and PillmannMarneros & Pillmann (2004) found a closer overlap between the two categories, as nearly two-thirds of their series of patients with ATPDs met the criteria for brief psychotic disorder.
Epidemiology
The incidence of ATPDs ranges from 3.9 to 9.8 cases per 100 000 population, and the rates for the 2-year and 3-year stable ATPD diagnosis are 6.7 and 1.4 respectively (Reference Singh, Burns and AminSingh 2004; Reference Castagnini and FoldagerCastagnini 2013a). Incidence in males peaks early in their mid-20s, whereas the highest rates for women occur 10 years later and are significantly greater than those for men over 45 years old (Reference Castagnini and FoldagerCastagnini 2013a). This pattern is likely to reflect not only the putative effect of female sex hormones on the brain, but also diversities across the ATPD subtypes, as polymorphic psychotic disorder is more common in women; cases with acute schizophrenic features predominate in younger men; and acute predominantly delusional disorder has a later age at onset. Reports on the prevalence of ATPDs are also varied, with greater rates in low- and middle-income countries (Reference Esan and FawoleEsan 2014).
ATPDs have high mortality rates from both natural and unnatural causes (Reference Castagnini, Foldager and BertelsenCastagnini 2013b). The mortality risk is almost twice as high in men, and similar to that for schizophrenia, while there is a small but significant increase in overall and natural-cause mortality compared with bipolar disorder. Suicide is the major cause of premature death and accounts for a quarter of ATPD mortality. Moreover, late-onset ATPDs (over 60 years of age) are associated with a high risk not only of mortality, but also of dementia (Reference Kørner, Lopez and AndersenKørner 2009).
Vulnerability factors
ATPDs are associated with neither specific personality disorders nor premorbid dysfunctions (Reference Jørgensen, Bennedsen and ChristensenJørgensen 1997; Reference Marneros and PillmannMarneros 2004; Reference Singh, Burns and AminSingh 2004). In addition, first-degree relatives of patients with ATPDs have higher rates of ATPDs than family members of patients with schizophrenia; yet the risk of schizophrenia is significantly increased in the family of those with schizophrenia (Reference Das, Malhotra and BasuDas 1999).
Further evidence from a large-scale family study (Reference Castagnini, Laursen and MortensenCastagnini 2013c) reveals that the risk of ATPDs was increased in patients with ATPDs who had first-degree relatives not only with ATPDs, but also with bipolar disorder, and particularly with schizophrenia. Only limited support was provided in terms of family predisposition for the different ATPD subtypes. By contrast, the risk of schizophrenia or bipolar disorder was markedly higher in patients with schizophrenia or bipolar disorder who had family members with the same condition. Similar findings were reported by Reference Kanazawa, Ikeda and GlattKanazawa et al (2013), who conducted a genome-wide association study of 47 individuals with ‘atypical psychosis’, a close variant of ATPDs described in Japan (Reference HatotaniHatotani 1996), and observed that the putative genes overlapped with those for schizophrenia.
Psychosocial factors
Psychological and social factors are more likely to be associated with ATPDs in low- and middle-income countries than in high-income ones, where only a relatively small number of cases are triggered by stressful events (Reference Das, Malhotra and BasuDas 2001; Reference Marneros and PillmannMarneros 2004; Reference Singh, Burns and AminSingh 2004; Reference Chakraborty, Chatterjee and ChoudharyChakraborty 2007; Reference Castagnini, Foldager and BertelsenCastagnini 2013d; Reference Esan and FawoleEsan 2014; Reference Rusaka and RancānsRusaka 2014). Reference Lau, Cheng and ChowLau et al (2009) found that the risk of ATPDs was two times higher among foreign domestic workers in Hong Kong; homesickness and marital problems were the most common life events. These findings support previous reports showing that refugees and immigrants have a greater risk of psychosis than native populations (Reference Parrett and MasonParrett 2010).
Furthermore, life events seem to be more often associated with ATPDs than with schizophrenia or manic episodes (Reference Marneros and PillmannMarneros 2004; Reference Chakraborty, Chatterjee and ChoudharyChakraborty 2007; Reference Möller, Jäger and RiedelMöller 2011), and patients with ATPDs who have a family history of mental disorder tend to have experienced fewer stressful events than those without family psychiatric antecedents (Reference Das, Malhotra and BasuDas 2001). In keeping with the stress–vulnerability model, family predisposition may exert its effects by increasing emotional reactivity, which renders individuals less likely to cope with adverse events.
Diagnostic stability, course and outcome
A literature review (Reference Castagnini and BerriosCastagnini 2011) reported that acute onset, short duration, absence of premorbid dysfunction and female gender were often associated with diagnostic stability and/or favourable outcome in ATPDs. It was also found that individuals with ATPDs fared better than those with schizophrenia, but no sharp distinction between the two categories can be drawn because about half of patients developed longer-lasting psychotic or affective disorders. In low- and middle-income countries, ATPDs seem to have lower rates of recurrence and higher diagnostic stability. Most studies, however, were small and used retrospective data, probably underpowered to produce meaningful findings. Differences in method, study design and distribution of ATPD subtypes also make comparisons difficult.
More recent studies have collected larger samples and mapped the course and outcome of ATPDs in greater detail. For example, Reference Björkenstam, Björkenstam and HjernBjörkenstam et al (2013) identified 1840 patients diagnosed with a first episode of atypical psychosis in the Swedish Psychiatric Register and found that a third of those affected with ATPDs had not been readmitted within 5 years. The risk of conversion to schizophrenia or schizoaffective disorder was twice as high for patients with ATPDs who had first-degree relatives with schizophrenia or bipolar disorder. Such findings compare favourably with a follow-up study by Reference Aadamsoo, Saluveer and KüünarpuuAadamsoo et al (2011) showing that about half of their patients retained the initial diagnosis of ATPDs, and many had enjoyed stable remission 2 years later. Younger age at onset and longer hospital admission were factors associated with transition to schizophrenia or schizoaffective disorder. Similar findings were reported by Reference Rusaka and RancānsRusaka & Rancāns (2014) in 294 first admissions with ATPDs followed up for 6 years. They observed that abrupt onset, polymorphic psychotic symptoms and anxiety were more common in those who did not develop another diagnosis. On this point, the McLean–Harvard International First-Episode Project (Reference Salvatore, Baldessarini and TohenSalvatore 2011) reported that patients with polymorphic psychotic disorders were less likely than those presenting with acute schizophrenic features to develop schizophrenia or affective psychoses. In keeping with findings of the Münich first-admission psychosis study (Reference Möller, Jäger and RiedelMöller 2011), ATPDs have a better long-term outcome than schizophrenia and delusional disorder.
Further evidence (Reference Castagnini, Foldager and BertelsenCastagnini 2013d, Reference Castagnini and Foldager2014) suggests that nearly half of 5429 patients first listed in the Danish Psychiatric Register with ATPDs did not change diagnosis over a mean 7.3 years, while in the other half there was a broad pattern of shifts in the first 24 months following the initial episode, mainly to either schizophrenia and related disorders (31%) or affective disorders (13%). Although polymorphic psychotic disorder fared better in terms of lower rates of relapse and higher diagnostic stability than the ATPD subtypes with acute schizophrenic or predominantly delusional symptoms, its predictive validity was relatively low.
Lastly, Reference Queirazza, Semple and LawrieQueirazza et al (2014) selected 2923 first admissions with ATPDs in Scotland and estimated that diagnosis remained unchanged in 54% of cases on average after 4 years. Schizophrenia was the most common shift and occurred on average 1.7 years later. Duration of first admission over 2 weeks, age under 30 years and male gender predicted increased risk and earlier transition to schizophrenia.
Treatment
Although patients with ATPDs are usually prescribed antipsychotic medications for acute symptoms and prevention of recurrences, very few clinical trials have addressed the efficacy and safety of treatment (Reference Nugent, Paksarian and MojtabaiNugent 2011). The guidelines for first-episode psychosis promote the use of antipsychotics for 1 to 2 years after remission of psychotic symptoms (International Early Psychosis Association Writing Group 2005), and the National Institute for Health and Care Excellence (NICE; 2014) clinical guidelines for psychosis and schizophrenia do not cover transient psychotic disorder. The NICE guidelines recommend psychosocial therapy (i.e. cognitive–behavioural therapy and/or family intervention) for 1 month or less for patients with psychosis who prefer it, then the offer of alternative treatments, including antipsychotics.
In the absence of specific guidance, protracted treatment with antipsychotics needs to be considered cautiously, as several side-effects have been described with both typical and atypical antipsychotics; the latter are also more likely to induce potential adverse effects, such as weight gain and metabolic syndrome, which are associated with increased risk of cardiovascular disease, diabetes and premature mortality (Reference Saha, Chant and McGrathSaha 2007). It would appear that the highest natural-cause mortality not only for schizophrenia – where the long-term side-effects of antipsychotics are known to be complicated by behavioural factors such as cigarette smoking, substance misuse, poor diet and a sedentary life-style – but also for ATPDs resulted from cardiovascular and endocrine/metabolic comorbidities (Reference Castagnini, Foldager and BertelsenCastagnini 2013b).
More to the point, a treatment trial involving patients with first-episode psychosis reported that those who discontinued or reduced medication 6 months after symptom remission fared better over the long term than those who remained on maintenance treatment for a further 18 months (Reference Wunderink, Nieboer and WiersmaWunderink 2013).
Many individuals with acute psychosis need hospital admission owing to disorganised behaviour, impaired insight, and aggressive and suicidal acts; they require careful risk assessment and a management plan.
Shortcomings of the ATPD category
ATPDs constitute a composite category
The ATPDs category includes disparate clinical syndromes with polymorphic, schizophrenic and predominantly delusional features. The ICD-10 field trials (Reference Sartorius, Üstun and KortenSartorius 1995) reported that many ATPD subtypes failed to achieve established standards of reliability, probably because of the fleeting nature of ‘polymorphic’ psychotic symptoms, the inclusion of provisional subtypes separated from schizophrenia only by temporal criteria, and the fact that the vaguely defined acute, predominantly delusional, disorder is a diagnosis by exclusion. In addition, no evidence supports the subdivision of the polymorphic psychotic subtypes into those ‘with’ and ‘without’ schizophrenic symptoms on the basis of 1 or 3 months’ duration. Only negative symptoms distinguish schizophrenia from ATPDs, as Schneiderian first-rank symptoms of schizophrenia seem to be common to both categories (Reference Marneros and PillmannMarneros 2004; Reference Möller, Jäger and RiedelMöller 2011; Reference Salvatore, Baldessarini and TohenSalvatore 2011).
ATPDs have little continuity with earlier categories in European psychiatry
Reference Marneros and PillmannMarneros & Pillmann (2004) reported that slightly more than half of their series of ATPD cases fulfilled Perris & Brockington's criteria for cycloid psychosis; yet it was found that cycloid psychosis typically lasts longer than 3 months and only a minority of cases share the ATPD diagnosis (Reference Peralta and CuestaPeralta 2003; Reference van der Heijden, Tuinier and Kahnvan der Heijden 2004). A closer overlap emerged between cycloid psychosis and the polymorphic psychotic subtypes (Reference Marneros and PillmannMarneros 2004), or when cases with prominent affective symptoms were omitted (Reference Peralta and CuestaPeralta 2003). A further study comparing ATPDs with bouffée délirante showed a positive diagnosis in a third of cases for both disorders (Reference Marneros and PillmannMarneros 2004). There also seems to be little continuity between the category of reactive psychosis and ATPDs, owing to changes in the concept of psychosis in modern psychiatric classifications (Reference Castagnini and BerriosCastagnini 2009).
ATPDs do not conform to any specific DSM category
ICD-10 was developed in parallel with DSM-IV, but the ATPD category overlaps only partially with the DSM categories of brief psychotic disorder and schizophreniform disorder, owing to differences in onset, duration and symptomatology.
Stress is an additional diagnostic feature
A fifth code may be used to indicate whether or not ATPDs are associated with ‘acute stress’ (F23.×1/0); likewise, the DSM category of brief psychotic disorder may follow ‘marked stressors’ (it was previously described as ‘brief reactive psychosis’). The temporal relationship between stress and ATPDs is limited to 2 weeks, which is probably so restrictive as to have underestimated the number of cases associated with life events. Examination of the 1904–1905 Welsh religious revival revealed a significant increase in hospital admissions for what would now be diagnosed as ATPDs, indicating that transient psychotic disorders may, at least in part, be caused by environmental factors (Reference Linden, Harris and WhitakerLinden 2009). These issues raise the need of defining stress more adequately and specifying further its temporal association with illness onset.
The relationship of ATPDs and mood disorders
Although the ATPD criteria require exclusion of both depressive and manic episodes, emotional changes and affective symptoms may be frequent and transitions tend to occur not only to schizophrenia, but also to affective disorders over the short and longer term (Reference Jørgensen, Bennedsen and ChristensenJørgensen 1997; Reference Marneros and PillmannMarneros 2004; Reference Aadamsoo, Saluveer and KüünarpuuAadamsoo 2011; Reference Castagnini, Foldager and BertelsenCastagnini 2013d, Reference Castagnini and Foldager2014; Reference Queirazza, Semple and LawrieQueirazza 2014; Reference Rusaka and RancānsRusaka 2014). Patients presenting with polymorphic psychotic symptoms are also more likely to develop bipolar disorder than those with schizophrenic or predominantly delusional features, indicating a closer kinship to mood disorders (Reference Marneros and PillmannMarneros 2004; Reference Aadamsoo, Saluveer and KüünarpuuAadamsoo 2011; Reference Salvatore, Baldessarini and TohenSalvatore 2011; Reference Castagnini, Foldager and BertelsenCastagnini 2013d, Reference Castagnini and Foldager2014). Genetic epidemiological studies have challenged a sharp demarcation between ATPDs and schizophrenia, while their relationship to affective disorders deserves clarification (Reference Castagnini, Laursen and MortensenCastagnini 2013c, Reference Castagnini, Munk-Jørgensen and Bertelsen2016).
Clinical implications
ATPDs have been excluded from major epidemiological surveys of first-episode psychosis, and hence the number of people likely to experience acute, florid onset of psychotic symptoms and early remission remains uncertain. The available evidence suggests that ATPDs are rare mental disorders and more often affect women in early to middle adulthood. It is not easy to identify cases in practice, as ATPDs’ distinctive features, such as delusions, hallucinations and emotional turmoil, can change in both type and intensity daily or even faster, and some episodes culminate in impulsive or suicidal acts.
Apart from changes in auditory P300 amplitude, brain scan and cerebral blood flow associated with cycloid psychosis (Reference Beckmann, Franzek, Henn, Sartorius and HelmchenBeckmann 2001), neither structural nor functional brain alterations have been observed in ATPDs. Yet there seems to be greater evidence of psychosocial factors, especially in low- and middle-income countries and migrant populations.
Further evidence indicates that ATPDs have little prognostic validity, as around half of patients developed either schizophrenia and related disorders or, to a lesser extent, affective disorders. While schizophrenic symptoms, young age at onset and male gender are more likely to be associated with subsequent transition to schizophrenia and/or schizoaffective disorders, the effect of acute onset, early remission and shifting polymorphic features on outcome of ATPDs has yet to be established.
Conditions such as the ‘non-affective acute remitting psychoses’ (Reference Susser and WanderlingSusser 1994) have an uneven geographical distribution, with a higher frequency in low- and middle-income countries, particularly in women, and are often associated with stress, fever or systemic infections and fewer negative symptoms than schizophrenia, but seldom fulfil the criteria for ATPDs (Reference Mojtabai, Varma and SusserMojtabai 2000; Reference Nugent, Paksarian and MojtabaiNugent 2011). Transcultural studies suggest a parallel with the socioclinical conditions that characterised the early stages of industrialisation in 19th-century Europe, when bouffée délirante and reactive psychosis were described (Reference GuinnessGuinness 1992).
Nosological implications
Recently published papers have put the study of ATPDs on a new empirical footing and challenged the classification of ATPDs into different subtypes. The proposed revision for ICD-11 (Reference Gaebel, Zielasek and ClevelandGaebel 2012) would introduce a major change by restricting the ATPD category to acute polymorphic psychotic disorder defined by criteria similar to those currently used and a duration shorter than 3 months. The remaining subtypes with schizophrenic and predominantly delusional symptoms would be redistributed into other categories of the newly renamed F2 section ‘schizophrenia spectrum and other primary psychotic disorders’ (Fig. 2). Such changes are expected to bring the ATPDs category closer to the ‘non-affective acute remitting psychoses’, which are reported to have typically 2–4 months’ duration (Reference Mojtabai, Varma and SusserMojtabai 2000). Also under discussion is the proposal to add ‘qualifiers’ for symptoms, course, cognition and functional impairment in order to identify further distinctive features and provide useful information about patients. This reveals more about the technicalities of psychiatric diagnostics than about the disease itself, and it seems questionable whether polymorphic psychotic disorder may constitute a reliable diagnosis because of the lack of clearly defining features.

FIG 2 Proposed changes to ICD-10 F23 category ‘acute and transient psychotic disorders’ and the newly renamed section ‘schizophrenia spectrum and other primary psychotic disorders’ for ICD-11 (adapted from Reference Gaebel, Zielasek and ClevelandGaebel 2012).
An alternative option, by analogy with the DSM-5 category of brief psychotic disorder, would be to select the clinical features that lend themselves to easier assessment, such as acute onset, florid psychotic symptoms and short duration. Close overlap between the two diagnostic categories might have benefits for practice, research and the wider understanding of these conditions.
Conclusions
Acute and transient psychoses have resisted specific description, and case identification has proved difficult. This argues against a clear demarcation of these conditions from schizophrenia and related disorders, but it is desirable that they are kept separated for both clinical practice and research.
MCQs
Select the single best option for each question stem
-
1 Current diagnosis of acute and transient psychosis is based on:
-
a aetiology
-
b symptoms
-
c prognosis
-
d reliability
-
e validity.
-
-
2 Pathognomonic features of acute and transient psychoses include:
-
a Schneider's first-rank symptoms of schizophrenia
-
b shifting polymorphic symptoms
-
c negative symptoms
-
d confusion or perplexity
-
e none of the above.
-
-
3 The frequency of acute and transient psychoses per 1 000 00 population is estimated at:
-
a 1–10
-
b 10–20
-
c 20–50
-
d 50–100
-
e >100.
-
-
4 Factors associated with favourable outcome in acute and transient psychoses include:
-
a onset within 4 weeks
-
b female gender
-
c precipitating stress
-
d affective symptoms
-
e family history of psychosis.
-
-
5 Treatment and management of acute and transient psychoses is based on:
-
a specific guidelines
-
b NICE guidelines for psychosis and schizophrenia
-
c first-episode psychosis guidelines
-
d clinical experience
-
e expert consensus.
-
MCQ answers
| 1 | b | 2 | e | 3 | a | 4 | b | 5 | d |




eLetters
No eLetters have been published for this article.