Introduction
Current treatments for post-traumatic stress disorder (PTSD), such as trauma-focused cognitive behavioural therapy, typically emphasise exposure to traumatic memories through re-living and updating maladaptive cognitions by cognitive restructuring (Brewin and Holmes, Reference Brewin and Holmes2003). Imagery rescripting (ImRs) is a therapy technique that, unlike traditional re-living techniques, focuses less on exposure and verbal challenging of cognitions and, instead, encourages patients to directly transform the intrusive imagery to change the depicted course of events in a more desired direction (Rusch et al., Reference Rusch, Grunert, Mendelsohn and Smucker2000). It is argued that working directly with imagery has a greater impact on the emotional and cognitive distress associated with intrusive images than verbal processing alone (Holmes et al., Reference Holmes, Grey and Young2005; Holmes et al., Reference Holmes, Arntz and Smucker2007; Wheatley et al., Reference Wheatley, Brewin, Patel, Hackmann, Wells, Fisher and Myers2007), and the evidence base for the effectiveness of ImRs for PTSD is growing (Morina et al., Reference Morina, Lancee and Arntz2017). Because it allows for alterations of imagery and inclusion of elements desired by the patient, ImRs is also viewed as more acceptable to both patients and therapists than exposure treatment alone (Arntz et al., Reference Arntz, Tiesema and Kindt2007). It is considered particularly indicated for patients primarily experiencing non-fear emotions such as anger or shame (Arntz et al., Reference Arntz, Tiesema and Kindt2007; Grunert et al., Reference Grunert, Weis, Smucker and Christianson2007).
Different theoretical mechanisms have been proposed for the effect of ImRs on memory representations. According to the retrieval competition hypothesis, ImRs creates a new, less problematic memory representation that competes with the original trauma memory for retrieval (Brewin et al., Reference Brewin, Gregory, Lipton and Burgess2010). Through rehearsal during treatment, the new memory eventually becomes more accessible and gains retrieval advantage, inhibiting the original memory (Brewin et al., Reference Brewin, Wheatley, Patel, Fearon, Hackmann, Wells and Myers2009; Wheatley et al., Reference Wheatley, Brewin, Patel, Hackmann, Wells, Fisher and Myers2007). An alternative explanation suggests that ImRs transforms the nature and semantic meaning of the original memory so that it no longer activates maladaptive responses (Arntz, Reference Arntz2012; Arntz and Weertman, Reference Arntz and Weertman1999; Kindt et al., Reference Kindt, Buck, Arntz and Soeter2007). Aside from effects on the trauma memory, ImRs may also facilitate emotional processing through the mutually reinforcing link between imagery and emotions as compared with purely verbal representation of the same memories (Arntz, Reference Arntz2012; Holmes and Mathews, Reference Holmes and Mathews2005). ln this regard, ImRs may offer a route for expressing emotional responses that have been suppressed or avoided after trauma (such as anger), as well as to fulfil unmet emotional needs (e.g. mastery, self-efficacy, or self-compassion), thereby permitting a shift away from the original emotional response and facilitating access to more adaptive emotions and cognitions (Long and Quevillon, Reference Long and Quevillon2009).
There is considerable variation among different ImRs approaches in terms of the length of the rescript, how rescripting is explained, at what point the memory is targeted, and how much input and guidance is provided by the therapist (Arntz and Weertman, Reference Arntz and Weertman1999; Hackmann, Reference Hackmann2011; Smucker and Niederee, Reference Smucker and Niederee1995; Wild and Clark, Reference Wild and Clark2011). The way in which the memory is manipulated, the level of activation of the original memory or characteristics of the new image (e.g. its vividness) are also considered as salient to bringing about change. However, a comprehensive account of how and in what circumstances ImRs brings about therapeutic change is required if treatment is to be optimised (Kazdin, Reference Kazdin2007), and this is yet to be developed (Arntz, Reference Arntz2012). There is a general lack of standardised means for studying psychotherapy treatment mechanisms (Kazdin, Reference Kazdin2007), and devising such a means is a particular challenge for capturing the complex processes involved in treatments such as ImRs.
Toward this end, Salter (Reference Salter2014) developed a systematic coding scheme encompassing the relevant factors that are readily observable in ImRs sessions. She first identified factors proposed in relevant research and thematically analysed the therapy protocols of a sample of ImRs sessions across a cohort of patients seeking treatment for PTSD with regard to these factors. The resulting framework of 56 codes was then applied to a cohort of individual cases undergoing ImRs in a single-case experimental design. Links between individual codes and participant outcomes were explored at an individual and group level, and the results pointed to ten factors in particular, such as activation of thoughts and feelings, image vividness, cognitive and emotional shift, and level of belief in the rescript, as playing important roles in change.
The present study aims to build on the preliminary findings of Salter (Reference Salter2014) to develop a revised version of the coding scheme. The aim was to identify a core set of codes to investigate based on Salter’s (Reference Salter2014) initial work, to assess its psychometric properties, and to assess the relationship between the variables identified and outcome in individuals undergoing ImRs for PTSD.
Method
Participants
Participants were recruited over a 4-year period across three studies investigating various aspects of ImRs (Looney et al., Reference Looney, El-Leithy and Brown2021; Murray et al., Reference Murray, Medin and Brown2021; Salter, Reference Salter2014). Participants were recruited from the same settings with similar inclusion and exclusion criteria. All three studies aimed to examine ImRs processes as a component of their research. Salter (Reference Salter2014) aimed to develop and refine the coding scheme in question in the current study. Murray et al. (Reference Murray, Medin and Brown2021) investigated the efficacy of ImRs for survivor guilt, and Looney et al. (Reference Looney, El-Leithy and Brown2021) investigated the role of coherence in ImRs. Across the studies, 50 people with a PTSD diagnosis who experienced intrusive images and who were willing to undergo ImRs were approached about the initial studies. Of these, 35 met inclusion criteria; 30 of these consented to take part. Three participants dropped out either before commencement of, or during the study, leaving a final sample of 27 participants. While English was not required as a first language, those who required the use of an interpreter were excluded from the study. Further exclusion criteria were the presence of a psychotic disorder, brain injury, current substance abuse or those with high risk of self-harm or suicide. The final sample of 27 (14 female, 13 male) was heterogeneous, with co-morbidities including depression, anxiety, personality disorder diagnoses, complicated grief and additional unexplained physical complaints. Most had experienced or witnessed interpersonal violence, and 85% of participants had experienced multiple traumas in addition to the one chosen for the focus of the present study. The mean age was 43.0 years (SD 10.9; range 20–63) and participants were from a range of ethnic backgrounds. The average time since their index trauma was 14.6 years (SD 10.6; range 1–30), and participants had been seen for an average of 51 therapy sessions (SD 45.2; range 6–189, median 32.5) at the time of their participation.
Measures
Distress Visual Analogue Scale
Distress associated with the target image was measured on a visual analogue scale (VAS) ranging from 0 to 100. This measure had good test–retest reliability in similar studies (r = 0.71, p = 0.01; Wild et al., Reference Wild, Hackmann and Clark2008) and is the rating dimension (along with frequency) used on the Clinician-Administered PTSD Scale (CAPS), which has been extensively validated (Weathers et al., Reference Weathers, Keane and Davidson2001).
Procedure
Development and refinement of the Brief Coding Scheme
Ten themes from the larger coding framework were identified as the central elements in terms of their salience in the relevant research literature and within ImRs procedures. Codes from Salter (Reference Salter2014) that related to outcomes were identified and through discussions with the researchers who developed the original coding framework. Relevant codes were summarised into ten themes. One item was created for each theme using material from the original coding framework. Each item incorporated several codes subsumed under each theme, but codes that were particularly representative of themes were emphasised in the wording of items. The ratings scales were changed to 4-point scales to increase consistency between items.
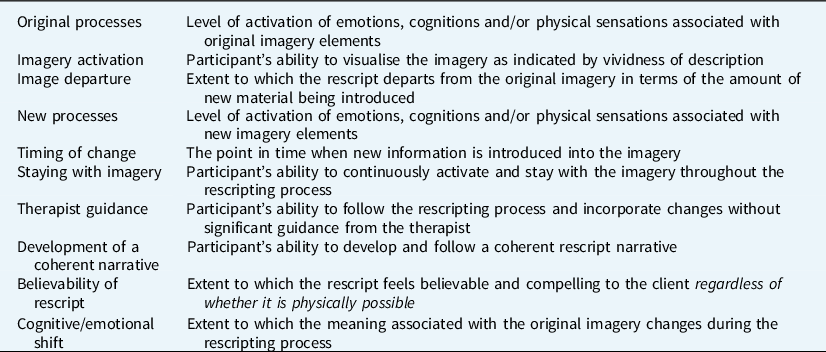
Ratings for each of the ten codes were based on four anchor points for each code (rated 0–3) reflecting degrees of applicability of the code to the target session (for example, whether there was [3] ‘high’, [2] ‘medium’, [1] ‘some’ or [0] ‘minimal/no’ change in a participant’s cognitive and emotional shift following rescripting). The new codes were inspected and refined through an iterative process between the authors. Feedback was also sought from two external researchers and experts in the field of ImRs and PTSD. The resultant coding scheme is shown in Table 1 and a full coding manual is included in the supplementary material. Inter-rater reliability of this brief version of the coding framework was assessed, with excellent agreement found between raters: the average measure interclass coefficient (ICC) was .92 with a 95% confidence interval from .81 to .97 (F 1,19 = 13.2, p<.001).
Table 1. Summary of session content codes
Relationship between rescripting codes and treatment outcomes
Each of the three component studies shared a common design in which data were collected across two or more ImRs treatment sessions embedded within routine treatment, and the content of the ImRs sessions was analysed using the ten-item coding framework. All participants were undertaking cognitive therapy for PTSD (CT-PTSD; Ehlers and Clark, Reference Ehlers and Clark2000) with an ImRs component. Their treatment was delivered in specialist traumatic stress services from clinical psychologists trained in both CT-PTSD and ImRs. Prior to commencing rescripting, all participants had undertaken one or more sessions of imaginal exposure and reliving of traumatic memories or images. The study was introduced to potential participants by their treating clinician at any point during their treatment, up until one week prior to when rescripting was due to commence on the agreed target image.
Data collection began at the beginning of the first session that would involve rescripting of a new target image. The Distress VAS was administered at the start of the session, prior to any rescripting. Participants then commenced rescripting of the target image. Due to the naturalistic design, no specifications about particular ImRs procedures were imposed, although the process was generally based on those previously used by Arntz and Weertman (Reference Arntz and Weertman1999), Hackmann (Reference Hackmann1998), Smucker and Niederee (Reference Smucker and Niederee1995) and Smucker and Dancu (Reference Smucker and Dancu1999). Distress VAS was measured again at the end of the session and again at the beginning of the following session as a follow-up point. Thus, distress data were collected at three time points: before rescripting, after rescripting and at the following session as a follow-up point. All sessions were coded using the brief coding scheme, producing ten separate codes rated from 0 to 3. The rescripted imagery sequence came at different points in treatment across the sample of participants, who had had a median of 32.5 prior sessions. The use of the Distress VAS permitted us to isolate one target image for rescripting and to be focused on the outcome with respect to the single image.
Results
Associations between the codes
Table 2 shows bootstrapped Spearman’s correlations between the ten codes, with the codes ordered in a sequence reflecting the approximate order in which they emerge over the course of the rescripting. Activation of original processes (i.e. those relating to the trauma memory/image) was largely uncorrelated with other codes. In contrast, degree of activation of the new imagery was associated with the degree to which its content was deemed to depart from the original image. Greater activation was also more characteristic of the images produced when the participant, rather than the therapist, guided the process, and when the participant was more successful at staying engaged with the new image. Participant-led images were associated with more coherent and more believable rescripts than more therapist-led images. Cognitions, emotions and physical sensations associated with the new imagery appeared more strongly activated when it coincided closely in time with the original target image/memory, and when the participant was more able to stay engaged in the new imagery. Activation of new imagery processes was associated with a greater shift in the meaning and emotionality of the original image. Finally, the believability of the imagery rescript was associated with greater coherence of the narrative and a greater shift in the meaning and emotions attached to the original image/memory.
Table 2. Intercorrelation of codes
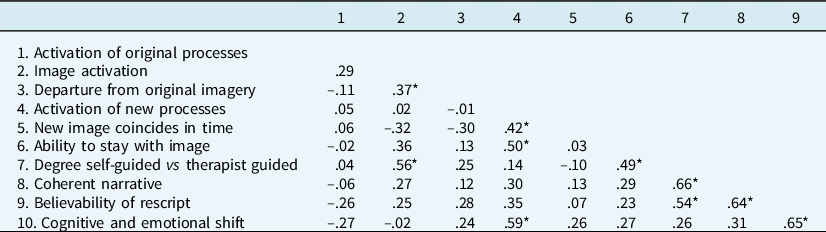
N = 27; *bootstrapped 95% confidence interval does not include 0.
Measurement properties of the coding framework
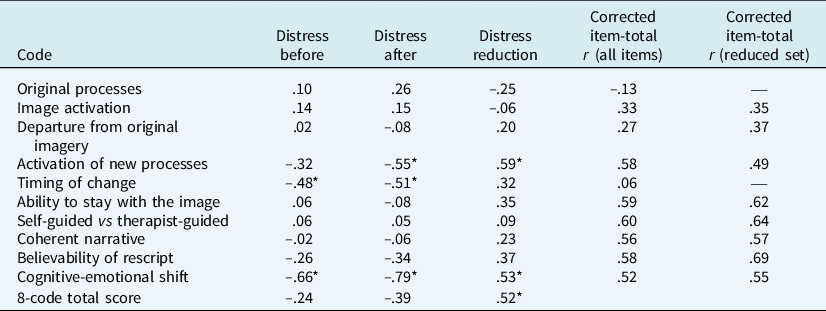
Exploratory psychometric analyses were carried out to examine whether the set of codes was sufficiently internally consistent to be scored as a scale (please see Table 3). Cronbach’s α and item-total correlations were calculated. Codes were removed where they reduced the overall alpha. This was true of ‘Original processes’ and ‘Timing of change’. As a final check before removing these codes, the scores were reversed in case they were inversely related to the other items, but this did not improve alpha. The alpha for the remaining eight items was .81 (bootstrapped 95% confidence interval = .69 to .90).
Table 3. Internal consistency of codes and their association with distress and change in distress

N=27; bootstrapped Cronbach’s alpha=.81 for the 8-code total score; *95% bootstrapped confidence interval does not include 0.
Relationship of coding scores to outcome
Scores for the Distress VAS were available at three time points: at the beginning of the session of interest (T1), at the end of the session of interest (T2), and at the beginning of the following session (T3). Of the 27 participants, T1 and T3 scores were available for all 27 participants; T2 data was only available for 22 due to slight difference in design across the three studies from which the data were drawn. To determine the comparability of T2 and T3 scores, an intraclass correlation coefficient was calculated for the n = 22 for whom both scores were available. The coefficient of .71 suggested that the scores were comparable. Therefore, the average of T2 and T3 scores was used when both were available. T3 scores were used when participants only had this score recorded. Distress scores reduced for all but two participants from pre (T1) to post (T2/T3 average) therapy session; those two participants’ scores worsened by 20 and 30 rating points, respectively.
Participants were classified as responders or non-responders on the basis of reliable change scores (please see Figure 1). This was calculated using the test–retest reliability of the post and follow-up scores (r = .71) for the subsample who had both, which required a minimum change of 25.8 rating points. There were eight reliable responders and 19 non-responders. As shown in Table 3, total coding framework score was inversely related to post-session distress and positively related to distress reduction.
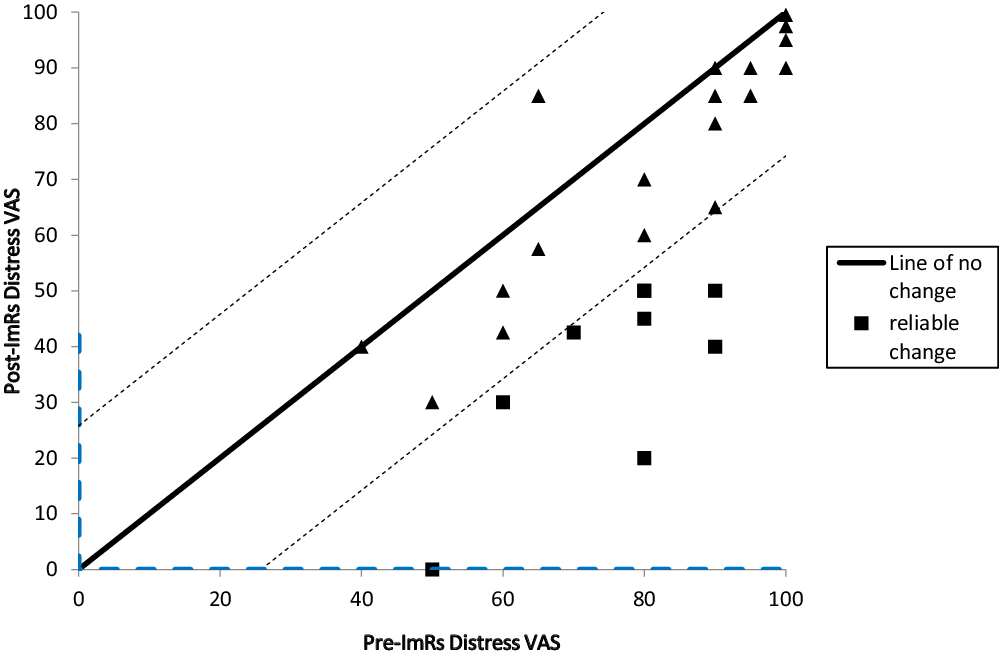
Figure 1. Reliable change in distress.
Discussion
Imagery rescripting has shown considerable promise for the treatment of PTSD and other disorders, such as chronic depression (Wheatley and Hackmann, Reference Wheatley and Hackmann2011), social anxiety (Strohm et al., Reference Strohm, Siegesleitner, Kunze, Ehring and Wittekind2021; Wild et al., Reference Wild, Hackmann and Clark2008) and obsessive-compulsive disorder (Veale et al., Reference Veale, Page, Woodward and Salkovskis2015). However, without a better idea of its underlying mechanisms of change, practitioners need to rely on anecdotal accounts of what constitutes best practice (Kazdin, Reference Kazdin2007). The present study demonstrated that a revised version of the coding scheme developed by Salter (Reference Salter2014) may be a helpful and psychometrically sound tool for examining key aspects of the rescripting process. The current results identified the timing of the change in the image, degree of activation of the new image and associated cognitive, emotional and physiological processes, self-guided rescripting, rescript believability, narrative coherence and cognitive and emotional shift as potentially important and related factors for the rescripting process.
Previous research using experimental means for dismantling ImRs sessions has focused on single elements. In this connection, Dibbets and Arntz (Reference Dibbets and Arntz2016) found that ImRs sessions that began rescripting prior to the key trauma-producing aversive aspects was less effective than rescripting that incorporated these aversive elements. This accords with the present findings that timing of the new image relative to the trauma memory was a key factor. Initial subjective level of distress was associated with how close the participant managed to situate their rescript relative to the most aversive original processes. Similarly, Siegesleitner et al. (Reference Siegesleitner, Strohm, Wittekind, Ehring and Kunze2020) found that, while more distressing than passive ImRs, active ImRs led to greater ultimate increase in positive affect, in agreement with the present findings for preference for patient- versus therapist- guided ImRs. Looney et al. (Reference Looney, El-Leithy and Brown2021) studied a subset of the present sample using a single case experimental design. They found a significant correlation between the extent to which sessions were self-guided and changes in symptom severity but also that some high-responders progressed from therapist- to self-guided rescripting across sessions. Thus, initial therapist prompting and guidance may facilitate subsequent independent rescripting and associated relief of symptoms. This may suggest that more therapist guidance in early ImRs sessions helped participants acquire skills necessary to generate compelling images. Accordingly, recent clinical guidance stipulates initial therapist guidance followed later by patient guided rescripting (Bosch and Arntz, Reference Bosch and Arntz2021; Simpson and Arntz, Reference Simpson and Arntz2020). This last finding illustrates the relative strengths and weaknesses of experimental studies versus small-scale intensive longitudinal designs. While critical for isolating effects and controlling for potential confounds, experimental studies are susceptible to the possibility that the targeted experimental manipulation produces its effects through other parallel processes that are in operation but unaccounted for. As such, the present more observational approach that closely focuses on a range of variables across a relatively small group complements this experimental research and has the added benefit of potentially generating additional targets for future experimental investigations and providing a basis for more precisely controlling for potential confounds.
Interestingly, activation of the original processes did not appear to be related to other factors. This is surprising, given that traditional re-living methods emphasise the importance of cognitive and emotional activation (e.g. Ehlers and Clark, Reference Ehlers and Clark2000). If, as this study suggests, rescripting requires only a link to the meaning of the original image, rather than full activation of highly aversive emotions and cognitions, then ImRs may provide a much more tolerable treatment method for clients with PTSD. These findings are also in line with those of Looney et al. (Reference Looney, El-Leithy and Brown2021) on a subset of the present sample who found that, while activation of new processes was significantly correlated with outcome, activation of original processes was not. Furthermore, at an observational level, high responders tended to display activation of both original and new processes but with a pattern of higher levels of new process activation relative to original.
The current findings also point to the importance of narrative coherence and rescript believability. Previous findings in both clinical and non-clinical literature suggest that narrative coherence predicts subjective probability (Kahneman and Tversky, Reference Kahneman, Tversky, Kahneman, Slovik and Tversky1982; Tversky and Kahneman, Reference Tversky and Kahneman1973) and that it can enhance one’s ability to interpret past events and alter emotional states (Taylor and Schneider, Reference Taylor and Schneider1989). Indeed, Looney et al. (Reference Looney, El-Leithy and Brown2021) found ‘goodness of simulation’, a measure of narrative coherence, to show the strongest correlation with treatment outcomes. The current findings further point to an association between rescript coherence and the level of believability of the rescript, supporting the notion that higher levels of narrative coherence may facilitate the believability of the rescript for participants, in turn leading to reduced distress. Of course, given the cross-sectional nature of these findings, causation cannot be inferred.
Previous studies have identified potential candidates for ImRs success (e.g. Looney et al., Reference Looney, El-Leithy and Brown2021; Siegesleitner et al., Reference Siegesleitner, Strohm, Wittekind, Ehring and Kunze2020). The current study offers further support to some of these previous findings and furthers our knowledge by demonstrating potential links between these factors. ImRs is a complex and nuanced process. Not only does it involve multiple factors, but the interplay between these factors is likely to play a significant role in whether ImRs is effective or not. The current study represents an important step to understanding this interplay. For example, while both self-guided rescripting and believability were identified as important factors, the current results suggest that they may also be related such that one may facilitate the other. At a practical level, this level of information is key as it can guide clinicians to focus on key elements that may have a positive, knock-on effect on other aspects of the ImRs process.
Among the limitations of the current research, aside from the relatively small sample, is the fact that the code ratings are necessarily based solely on what is manifest in the session. As such, it could be the case that what has been found has less to do with underlying processes and is simply an artefact of the raters being able to divine the likely distress VAS scores based on expressed relief and other signs of diminished distress. This also means that processes that are not as readily observable might mistakenly be de-emphasised. Future research could incorporate the views of therapists and clients with regard to perception of change factors in ImRs. Furthermore, different imagery rescripting procedures are usually regarded as largely comparable, and so we would expect the repertoire of responses to be largely the same but that they might occur at different points in treatment depending on the precise version of ImRs that is implemented or may take slightly different forms. This is a further question for future research that could be carried out using the present framework.
It should also be noted that, although the outcome data presented in this study were collected across two sessions of rescripting of one target image, the length of the overall treatment offered to participants, within which imagery rescripting took place, is longer than is usual in many services and the point in course of treatment therefore likely varied considerably across participants. This reflects the severity and complexity of the participants’ PTSD, with the majority of participants experiencing multiple, severe traumas. It would be interesting to repeat the study using participants with single event traumas to explore whether the same results stand. Similarly, it may be helpful to repeat the study with larger and more heterogeneous samples to determine whether there are differences in processes between different subsets of trauma patients as well as with non-English speaking participants.
The present study focused only on reduction of distress. While this is an important marker of improvement, other outcomes, such as frequency of intrusions or the ‘nowness’ of the old image, might also be considered. Furthermore, future research should aim to determine whether codes relate differentially to different outcomes. A final limitation of this study relates to the correlational nature of the data and the fact that there may well be additional factors that influence both outcome and the factors included in the current study. That said, the coding scheme used in this study started out with 56 codes before being reduced to those considered most relevant to change. However, the development of this scheme was based on readily observable session characteristics and so, similar to Looney et al. (Reference Looney, El-Leithy and Brown2021), there may be additional, less readily observable factors at play. Finally, ‘Timing of change’ was associated with change in distress but was not internally consistent with other items and so was excluded from the overall index. Future studies with larger samples should consider whether it has incremental predictive validity.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1352465822000479
Data availability statement
Data are available on request due to privacy/ethical restrictions.
Acknowledgements
None.
Author contributions
Gary Brown: Conceptualization (lead), Formal analysis (lead), Investigation (equal), Methodology (lead), Project administration (lead); Caroline Salter: Conceptualization (lead), Formal analysis (equal), Investigation (equal), Methodology (equal); Eleanor Parker: Investigation (supporting); Hannah Murray: Conceptualization (equal), Methodology (equal); Kathy Looney: Writing – original draft (supporting), Writing – review & editing (supporting); Sharif El Leithy: Conceptualization (equal), Methodology (equal), Writing – review & editing (equal); Evelina Medin: Conceptualization (equal), Methodology (equal); Barbora Nováková: Writing – original draft (supporting), Writing – review & editing (supporting); Jonathan Wheatley: Investigation (supporting), Writing – review & editing (supporting).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
Gary Brown is an Associate Editor of Behavioural and Cognitive Psychotherapy. He was not involved in the review or editorial process for this paper, on which he is listed as an author. The other authors have no declarations.
Ethical statements
This research adheres to the Ethical Principles of Psychologists and is in line with the Code of Conduct as set out by the BABCP and BPS. Ethical approval was sought through the NHS National Research Ethics Service, with REC references 13/NW/043, 14/LO/0192, and 13/NW/0432. Participants gave informed consent to participate in the study and any subsequent publication.






Comments
No Comments have been published for this article.