No CrossRef data available.
Article contents
Temporal decreases in pathogen colonization and infection among hospitalized neonates following routine skin antisepsis with chlorhexidine gluconate: Botswana 2022 – 2023
Published online by Cambridge University Press: 16 September 2024
Abstract
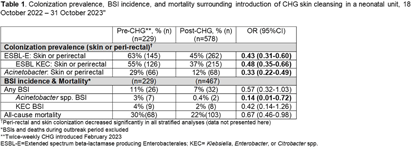
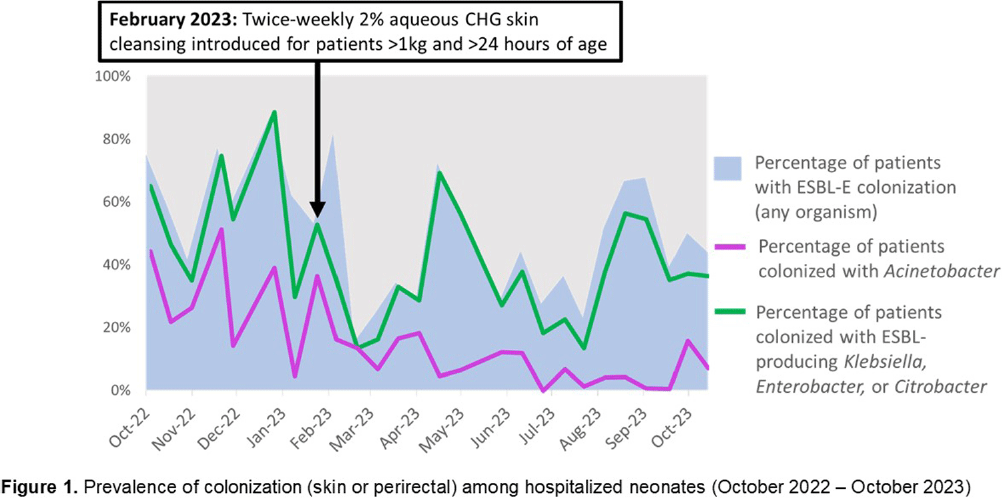
Background: Multidrug-resistant Gram-negative bacteria are a major cause of sepsis among hospitalized neonates globally. Aqueous chlorhexidine gluconate (CHG) skin antisepsis has been shown to be safe for use in infants; however, its sustained effectiveness in preventing Gram-negative pathogen colonization, bloodstream infection (BSI), and mortality is unclear. Methods: We conducted a period prevalence survey, with 26 sampling events over 12 months (18 October 2022 – 31 October 2023) at a 33-bed neonatal unit in a tertiary public hospital in Botswana where ESBL-producing Klebsiella pneumoniae and carbapenem-resistant Acinetobacter baumannii are leading causes of BSI. Perirectal and periumbilical skin swabs were collected every two weeks from all inpatients. Swabs were inoculated onto chromogenic media selective and differential for extended-spectrum beta-lactamase producing Enterobacterales (ESBL-E) and Acinetobacter spp. (CHROMagar™ ESBL, Acinetobacter). Colonization status was determined based on culture growth and colony morphology. Contemporaneous data on all-cause mortality and BSI were abstracted from routine surveillance records. Pre- and post-CHG prevalences were compared using a simple Chi-square test. During the surveillance period, an outbreak of K. pneumoniae linked to contaminated multi-use vials was detected, thus BSIs and deaths during the outbreak period (2 February–6 April, 2023) were excluded. In February 2023, the hospital infection prevention and control (IPC) team introduced twice-weekly whole-body cleansing with commercially available 2% aqueous CHG, performed by caregivers and healthcare workers on neonates >24 hours old and weighing ≥1 kg until discharge. Results: There were significant decreases in ESBL-E and Acinetobacter skin and perirectal colonization following the CHG intervention (Table 1; Figure 1). After the CHG intervention, the incidence of Acinetobacter BSIs declined significantly and there was a trend toward a decline in other BSIs and mortality. No adverse events associated with CHG were reported. Conclusions: Twice-weekly CHG application was temporally associated with significant reductions in neonatal ESBL-E and Actinetobacter skin and perirectal colonization and Acinetobacter BSI. This analysis was limited by a short pre-intervention surveillance period and thus may have been influenced by confounders such as seasonality, and intensified IPC efforts following the outbreak. Analysis of the routine CHG use in other settings and over longer surveillance periods are needed to better understand its effectiveness as an IPC strategy in settings where neonatal sepsis incidence is high. Table 1. Colonization prevalence, BSI incidence, and mortality surrounding introduction of CHG skin cleansing in a neonatal unit, 18 October 2022 – 31 October 2023.
- Type
- Decolonization Strategies
- Information
- Antimicrobial Stewardship & Healthcare Epidemiology , Volume 4 , Issue S1: SHEA Spring 2024 Abstracts , July 2024 , pp. s12
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2024. Published by Cambridge University Press on behalf of The Society for Healthcare Epidemiology of America


