No CrossRef data available.
Published online by Cambridge University Press: 16 September 2024
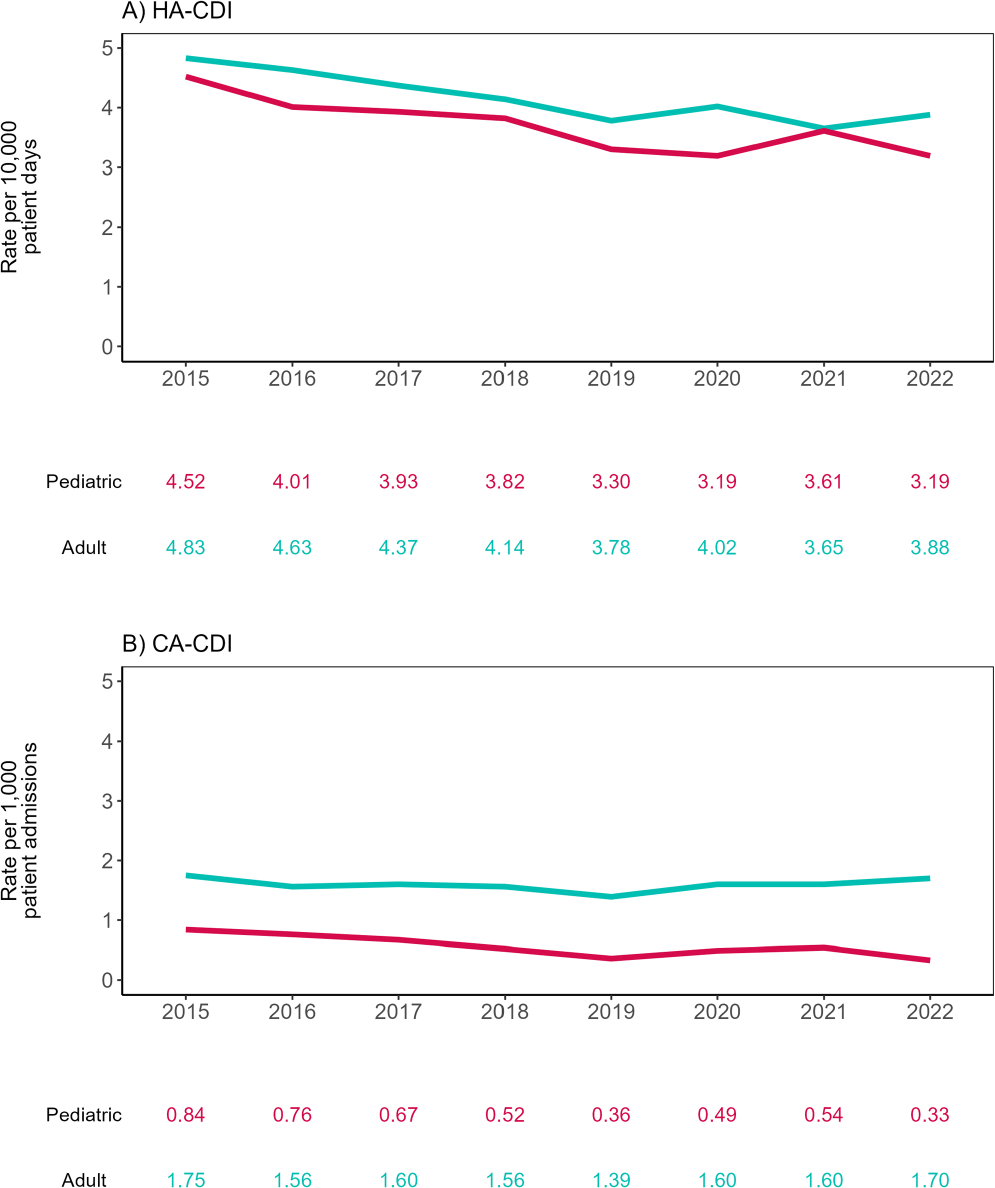
Background: The molecular and epidemiological landscape of C. difficile infection (CDI) has evolved markedly in the last decade; however, limited information is available contrasting differences between adult and pediatric populations. We describe a multicenter study evaluating healthcare-associated (HA) and community-associated (CA) adult and pediatric-CDI identified in the Canadian Nosocomial Infection Surveillance Program (CNISP) network from 2015 to 2022. Methods: Hospitalized patients with CDI were identified from up to 84 hospitals between 2015–2022 using standardized case definitions. Cases were confirmed by PCR, cultured, and further characterized using ribotyping and E-test. We used two-tailed tests for significance (p≤0.05). Results: Of 30,817 cases reported, 29,245 were adult cases [HA-CDI (73.2%), CA-CDI (26.8%)] and 1,572 were pediatric cases [HA-CDI (77.7%), CA-CDI (22.3%)]. From 2015 to 2022, HA-CDI rates decreased 19.7% (p=0.007) and 29.4% (p=0.004) in adult and pediatric populations, respectively (Figure 1). CA-CDI rates remained relatively stable in the adult population (p=0.797), while decreasing 60.7% in the pediatric population (p=0.013). Median ages of adult and pediatric patients were 70 (interquartile range (IQR), 58–80) and seven (IQR, 3–13) years, respectively. Thirty-day all-cause mortality was significantly higher among adult vs. Pediatric CDI patients (11.0% vs 1.4%, p < 0.0001). No significant differences in other severe outcomes were found. Ribotyping and susceptibility data were available for 4,620 samples: 3,558 adult (77.0%) and 1,062 pediatric (23.0%). The predominant adult and pediatric ribotypes (RT) were 106 (12.2/16.2%), 027 (11.4/3.2%), and 014 (8.8/8.2%). Overall, RT027 prevalence significantly decreased from 17.9% in 2015 to 3.2% in 2022 (p=0.003), while RT106 increased from 8.5% to 14.4%. Resistance rates among adult and pediatric isolates were similar for all antimicrobials tested except moxifloxacin (16.2% vs. 6.2%, p < 0.0001, respectively). Adult moxifloxacin resistance decreased from 30% to 6.3% from 2015 to 2022 (p=0.006). Adults with moxifloxacin-resistant CDI were older (median: 74 vs. 69 years, p < 0.001) and had higher thirty-day all-cause mortality (13% vs. 9.8%, p=0.041) and recurrence (10% vs. 5.7%, p < 0.001) compared to those with moxifloxacin non-resistant CDI, while these trends were not observed in pediatric patients. Among RT027 strains, moxifloxacin resistance decreased from 91.0% in 2015 to 7.1% in 2022. There was one metronidazole-resistant pediatric sample in 2018 and no resistance to vancomycin or tigecycline in either population. Conclusion: We have found differences in the epidemiological and molecular characteristics of adult and pediatric CDI, with higher thirty-day all-cause mortality among adults. Overall, RT106 has replaced RT027 as the predominant ribotype with a concomitant decrease in fluoroquinolone resistance.