Climate change is the greatest public health threat of the 21st century. Reference Watts, Amann and Ayeb-Karlsson1 Healthcare is a major polluting industry, responsible for 8.5% of US greenhouse gas emissions. Reference Eckelman, Huang, Lagasse, Senay, Dubrow and Sherman2 Mitigating healthcare pollution is integral to first doing no harm. Heating, ventilation, and air conditioning (HVAC) accounts for 70%–97% of operating room (OR) energy usage. Reference Thiel, Eckelman and Guido3,Reference MacNeill, Lillywhite and Brown4 Healthcare HVAC systems could be safely manipulated to reduce energy use and environmental impact. Reference Sherman, Thiel and MacNeill5
The American Society for Health Care Engineering (ASHE) hospital HVAC recommendations for ORs (unchanged during our survey) include (1) minimum efficiency reporting value (MERV) filter ratings of ≥14, (2) positive pressure ORs, and (3) minimum of 20 air changes per hour (4 outdoor air changes per hour minimum). 6 In a 2019 review of ASHE HVAC recommendations, outdoor air changes per hour and minimum total OR air changes per hour were rated as needing ‘further investigation’ due to little supporting clinical evidence, and other hospital area parameters had little or poor-quality evidence. Reference Mousavi, Lautz, Betz and Grosskopf7 Current standards are based on staff comfort, odor control, fire prevention, and infection prevention; however, little evidence correlates air-change rates and outcomes including surgical site infections (SSIs). Reference Mousavi, Lautz, Betz and Grosskopf7
We surveyed current OR air-change rate practices, including any set-back transitions (ie, decreasing air changes during off hours), as well as attitudes about climate change, and OR change rates in light of the COVID-19 pandemic.
Methods
The Washington University School of Medicine Institutional Review Board approved the survey, and it was pilot tested with 5 experts. The 36-item anonymous survey was distributed to the American Hospital Association (AHA) by nondedicated e-mail and the Society for Healthcare Epidemiology of America Research Network (SRN) by dedicated e-mail from October 2020 to February 2021. Within the SRN, 67 US institutions (1 recipient per hospital) received 4 notifications. Data were collected using Qualtrics software (Seattle, WA). Descriptive statistical analyses were performed using SPSS version 27 software (IBM, Armonk, NY).
Results
The AHA survey recipients had response rates <1% and were excluded from analysis. Of 67 SRN participants, 30 (45%) opened the survey. Of these 30 participants, 10 (15%) completed the survey, and 20 (30%) partially completed it (Fig. 1).

Fig. 1. Flow diagram of participants’ survey completion.
Among respondents, 7 (70%) were male, 8 (80%) were white, 7 (70%) were aged >50 years, 8 (80%) were hospital epidemiologists, and 2 (20%) were infection preventionists. Six respondents were from academic hospitals, 3 were from a community-based hospital, and 1 was from a Veterans Affairs hospital. The hospiitals of 80% of respondents had >250 beds.
Climate
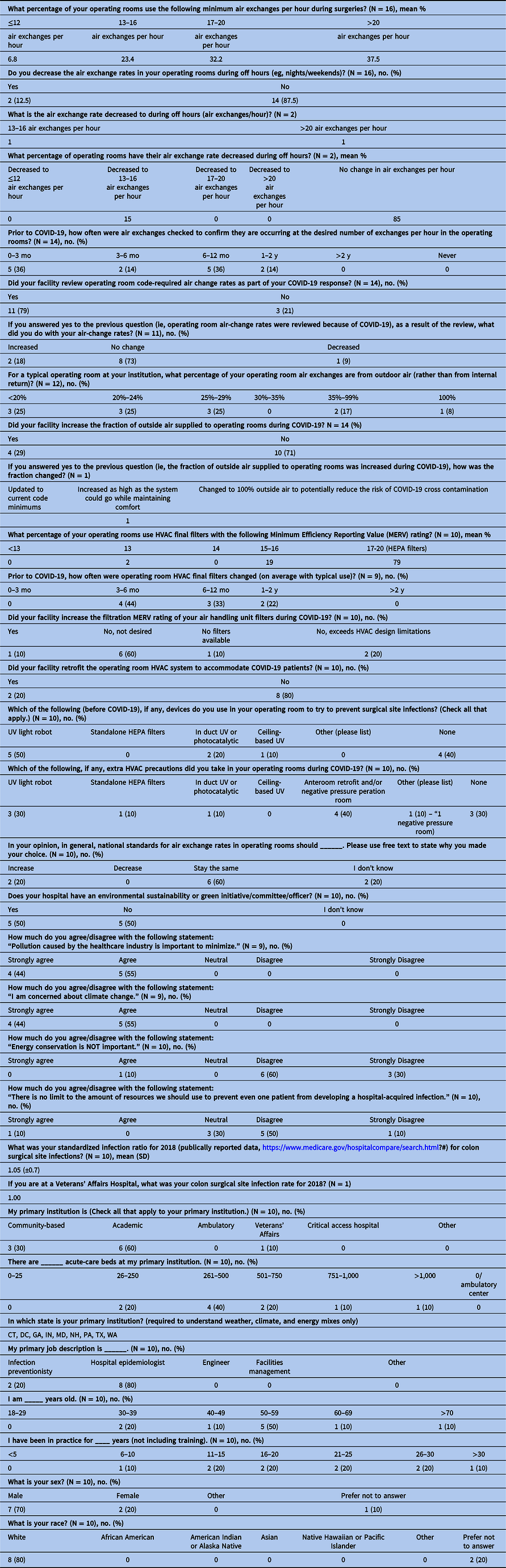
Overall, 10 (100%) respondents agreed or strongly agreed that “pollution caused by the healthcare industry is important to minimize” and “I am concerned about climate change” (Table 1). Regarding the statement “There is no limit to the amount of resources we should use to prevent even one patient from developing a hospital-acquired infection,” 1 (10%) agreed or strongly agreed, 3 (30%) were neutral, and 6 (60%) disagreed or strongly disagreed.
Table 1. Statement and Responses Regarding Climate Change, Energy, and Infections
Air change rates
Of 16 respondents, 14 (88%) did not decrease OR air-exchange rates during off hours before the pandemic. Before the COVID-19 pandemic, among these 14 respondents, 86% checked air exchanges more frequently than annually.
The percentages of air change from outdoor air varied. Overall, 1 respondent reported 100% external (outside) air changes (the most energy-intensive strategy); 2 respondents reported 35%–99% external air changes; and 3 respondents reporting each of the following: <20% external air, 20%–24% external air, and 25%–29% external air. Of 10 respondents, 9 (90%) used HEPA final filters in some ORs, and final filters were changed at least every 2 years in the institutions of all respondents (100%). In response to COVID-19, 6 (60%) of 10 did not increase MERV filter rating because it was not desired, 1 (10%) did not because filters were unavailable, 2 (20%) did not because it exceeded HVAC design, and 1 (10%) increased MERV filter rating (this respondent had <100% OR HEPA filter use at baseline).
Regarding opinions on national standards for OR air change rates, 6 (60%) of 10 felt that they should remain unchanged, 2 (20%) had no opinion or did not know, and 2 (20%) thought that they should increase. None felt that rates should decrease. This question did not specify whether respondents should include consideration of the coronavirus disease 2019 (COVID-19) pandemic.
COVID-19
Among 14 respondents, 11 (79%) reviewed code-required air-change rates because of COVID-19; 8 (73%) made no changes, 18% increased air-change rates, and 9% decreased air-change rates. Among these 14 respondents, 10 did not increase the fraction of outside air supplied to ORs. Of these 10, 2 (20%) were retrofitted OR HVACs to accommodate COVID-19 patients (ie, turned ORs from positive to negative pressure). Table 1 lists further details.
Discussion
Despite little evidence to support their use from an infection control perspective, Reference Mousavi, Lautz, Betz and Grosskopf7 US healthcare institutions use high energy-intensive air-change rates, even exceeding recommended minimums. Reductions in air changes in acute care has the potential for large energy, financial, and carbon savings. Reference Sherman, Thiel and MacNeill5,Reference Sheppy8 Our survey’s respondents indicated that climate change, pollution, and the healthcare industry’s impact thereon were considered important. Despite absence of evidence of benefit, the extent to which HVAC energy resources should be used to prevent infections varied. For example, ∼90% of respondents did not engage in set-back practices in ORs during off hours.
Approximately 80% of respondents reported that they checked OR air-change rates and filters because of COVID-19, some altered air changes or other presumptive infection prevention measures. There was little agreement about whether or how air-change rate standards should be changed. Such uncertainty perhaps resulted from the paucity of evidence for relationships between air-change rates and infections, Reference Mousavi, Lautz, Betz and Grosskopf7 guideline unfamiliarity, or both.
HVAC standards and set-back opportunity
Evidentiary gaps exist on optimal air-change settings for healthcare facilities. Reference Mousavi, Lautz, Betz and Grosskopf7 The current standard (ASHRAE 170) recommends a minimum OR rate of 20 air changes per hour including ≥4 outside air changes. Minimum air-change values are required only while the room is occupied. Shutting off OR ventilation systems off hours results in energy or cost savings without exceeding particle-count thresholds. Reference Dettenkofer, Scherrer and Hoch9 Yet, our survey response (85% respondents) suggests that facility operators do not decrease air changes during off hours. This finding may reflect unfamiliarity with the lack of evidence on the relationship between OR ventilation rates and SSI prevention.
Future studies should ascertain relationships between air-change rates and SSIs, using the extant natural experiment of institution-to-institution variability to elucidate opportunities for energy, pollution, and cost savings.
Pandemic response
ASHRAE created an epidemic task force (https://www.ashrae.org/technical-resources/resources) to collect emerging evidence and guidance. Recommendations ultimately followed current ventilation standards (ASHRAE 62.1 and 170) and encouraged additional air filtration when possible.
Numerous institutions tried reducing risks associated with operating on COVID-19 patients. Overalll, 79% of respondents reviewed air-change rates because of COVID-19, and 73% of these made no changes. This finding inplies that prescribed standard flow rates had already been achieved and/or that the system could not be updated. Moreover, 60% responded that mandated air-change rates should remain unchanged. Outside air fractions varied, and 71% made no changes.
Our survey had several limitations. We had low response rates (30% partial response rate, 15% complete), though this rate is similar to that of other surveys (response rates, ∼20%). Reference Sarfaty, Bloodhart and Ewart10 Response rates raise these questions: What gaps in air-change rate understanding remain unfilled, and how can this improve?
In conclusion, high air-change rates in ORs are financially costly and have commensurate, possibly unjustified environmental impacts. With uncertain HVAC efficacy on one hand and certain high financial and environmental impacts on the other, we require evidence indicating whether current OR air-change rates influence SSIs. Even with current standards, opportunity exists for off-hour setbacks to reduce energy expenses, to prevent pollution, and to protect public health.
Financial support
J.D.S. reports support from the Yale Program on Healthcare Environmental Sustainability.
Conflicts of interest
R.A.M. reports that he is a member of the Board of Directors of the International Ultraviolet Association. All other authors report no conflicts of interest relevant to this article.




