Introduction
In their seminal article, Rowe and Kahn (Reference Rowe and Kahn1997) defined successful ageing as the avoidance of disease and disability, the maintenance of high physical and cognitive function, and sustained engagement in social and productive activities. These dimensions defined the outcomes for individuals, but not the changes in social structures and processes that would enable them. More recently, Rowe and Kahn (Reference Rowe and Kahn2015) called for clarity on how social institutions need to change, especially if they are to preserve and promote the human capital of individuals (including their wealth and health) to support and sustain a successful longer life. The labour market is a critical institution for successful ageing, because employment into older age offers opportunities for both social and productive engagement and both could benefit health across multiple dimensions (Zaidi et al., Reference Zaidi, Gasior, Hofmarcher, Lelkes, Marin, Rodrigues, Schmidt, Vanhuysse and Zolyomi2013; Arpino and Bordone, Reference Arpino, Bordone, Zaidi, Harper, Howse, Lamura and Perek-Bialas2018). However, employment could also undermine successful ageing, or only offer these benefits (and their health consequences) to a selected few, having a more uneven role in successful ageing than previously theorised.
This paper seeks to understand the limits of employment as an agent of successful ageing. We focus on work hours – a largely unregulated and unchanged aspect of employment that is important for health and wellbeing and closely connected to power relations and social inequity (Nyland, Reference Nyland and Hassard1990). We ask how many hours can older adults work before their health is compromised, and how mightthe relationship between hours, earnings and health interacts with and compound inequity in later life.
Hours, health, income and inequity in the ageing workforce
Ninety years ago, the International Labour Organization (ILO) set 48 hours as the maximum weekly work-hour threshold, arguing that hours worked beyond this were harmful to health. Subsequently, many countries set thresholds that were considerably lower, redefining standards for the full-time working week. In Australia, for example, the Australian Fair Work Act dictates that employees should not exceed 38 hours per week except for reasonable additional hours. Importantly, national and global working-hour thresholds evolved in the context of a younger workforce, when life expectancies and retirement ages were considerably lower. However, workforce composition has changed since these thresholds were set, and one key change is age. In Australia, a country ranked fifth in terms of life expectancy (Organisation for Economic Co-operation and Development (OECD), 2017a), boys born in 2014–2016 can expect to live past 80 years and girls past 84 years, three decades longer than boys or girls born when the ILO set its working-time standard. The percentage of people aged 50 and over rose from 22.1 per cent in 1970 to 33.5 per cent in 2019 in Australia, similar to the demographic change seen across the OECD (23.2 and 36.5%, respectively) (OECD, 2016). Similarly, life expectancy has steadily increased for all OECD countries by an average of 10 years since 1970 (OECD, 2017a). As a result, rising numbers of older adults are in the workforce needing the income earned to support a longer life, yet there is virtually no evidence on how long they can work to earn it.
Longer lives do not necessarily mean heathier lives, and there is very little age-focused analysis or debate on many hours workers could and should work as they age (ILO, 2011). Furthermore, longer lives do not mean more equal lives in terms of financial or health status. Indeed, it is becoming apparent that there are ‘two worlds of ageing’, reflecting inequities in both health and wealth (Crystal et al., Reference Crystal, Shea and Reyes2017). Employment is a critical contributor to these health and wealth inequities, because jobs which offer good pay, autonomy, flexibility and prestige generally are white collar, office based and health protective. These higher-status jobs, accompanied by better pay and conditions, are far more likely to have health-protective effects and offer a pathway to successful ageing (Marmot et al., Reference Marmot, Smith, Stansfeld, Patel, North, Head, White, Brunner and Feeney1991, Reference Marmot, Bosma, Hemingway, Brunner and Stansfeld1997; Hemingway et al., Reference Hemingway, Nicholson, Roberts, Stafford and Marmot1997; Rowe and Kahn, Reference Rowe and Kahn2015) coupled with financial security over the lifecourse. They are defining a group of workers who, as they age, have relatively good health, are financially secure, and the jobs they continue to work in offer health-protective conditions and minimal physical demands. In contrast, insecure, low-paid, low-autonomy and inflexible jobs are more common among pink- (e.g. hospitality and care) and blue- (e.g. trades, construction) collar sectors. These are jobs which involve physical as well as mental demands, and they are often poorly paid. This combination is likely to generate accumulating (and also compounding) health and financial risks which will undermine successful ageing. Many of these workers, therefore, have neither optimal health nor savings, comprising a group of less-healthy and less-wealthy older workers in jobs which pose continuing health risks as they age.
Work hours are critical to understanding ageing, health and inequity in the context of employment. Put simply, people exchange their time for income in the labour market, with longer hours usually yielding more income and shorter hours the converse (Reference O'Neill and O'ReillyO’Neill and O'Reilly, 2010). However, the ability to work longer hours, or full time, depends on health (as well as industry and job type), a well-documented process termed health selection (McDonough and Amick, Reference McDonough and Amick2001; Kim and DeVaney, Reference Kim and DeVaney2005; Wagenaar et al., Reference Wagenaar, Kompier, Houtman, van den Bossche and Taris2012; Subhasree, Reference Subhasree2018). Long hours can also harm health, as the ILO regulations attest. There are, therefore, reciprocal relationships between work hours, income and health; they interact over the lifecourse and all contribute to inequity. Ageing adds another dimension to the interplay between health, work hours and earnings. As people age, health generally declines, but this decline is uneven and socially patterned in extent and timing (Kim and DeVaney, Reference Kim and DeVaney2005; Benzeval et al., Reference Benzeval, Green and Leyland2011; Subhasree, Reference Subhasree2018). In the context of an ageing workforce, an average decline in capacity to work the same hours as younger counterparts may be expected. However, this average can hide wide differences in work hour–health thresholds (the number of hours someone can work before compromising their health), which map to social and health inequity, widening the ‘two worlds’ further. Thus, older workers with poorer health status – most likely to be working in blue- and pink-collar jobs (Ravesteijn et al., Reference Ravesteijn, van Kippersluis and van Doorslaer2018) – may be more constrained in terms of how long they can work, even while their financial need is greater. If this is the case, older-age employment systematically disadvantages the least healthy and most poorly paid, because working more hours to earn (needed) income differentially compromises their health.
This paper tests the hypothesis that as workers age their capacity to work full-time work hours without compromising their health declines. We further hypothesise that these work hour–health tipping points vary among older workers, aligning with markers of social and health inequity linked to occupation and health status. Because health, work hours and earnings form a system with interacting, reciprocal relationships, we also model it as such, using simultaneous methods to estimate multiple and interacting pathways with longitudinal date. This approach addresses the complex processes shaping health and social outcomes in an ageing workforce, maximising the robustness of estimates, and addresses tensions and conflicts between key elements of successful ageing (work hours, earnings and health).
How work hours affect health
How work hours affect health is a key question for health economists and social epidemiologists, who have largely focused on the health risk from long work hours (e.g. Dembe et al., Reference Dembe, Erickson, Delbos and Banks2005; Virtanen et al., Reference Virtanen, Ferrie, Singh-Manoux, Shipley, Stansfeld, Marmot, Ahola, Vahtera and Kivimäki2011; Amagasa and Nakayama, Reference Amagasa and Nakayama2013; Bannai and Tamakoshi, Reference Bannai and Tamakoshi2014; Milner et al., Reference Milner, Smith and LaMontagne2015). Most studies assume a linear relationship – the more hours worked the worse the health effects. However, work hours are likely to have a complex and inverted U-shaped relationship with health, which more recent research is starting to model. Up to a point, working is generally beneficial, after which additional hours become harmful. Employment is an important source of social inclusion as well as income, both key in the protection of health (Dooley, Reference Dooley2003; Dooley and Prause, Reference Dooley and Prause2009; Karsten and Klaus, Reference Karsten and Klaus2009). Conversely, un- or underemployment negatively affects health (Dooley et al., Reference Dooley, Prause and Ham-Rowbottom2000; Milner et al., Reference Milner, King, LaMontagne, Aitken, Petrie and Kavanagh2017). Recent estimates from the United States of America (USA) and Australia suggest that an average work week of around 39 hours appears to be the limit beyond which health declines (e.g. Kleiner and Pavalko, Reference Kleiner and Pavalko2010; Dinh et al., Reference Dinh, Strazdins and Welsh2017). Milner et al. (Reference Milner, Smith and LaMontagne2015) considered the effect of long work hours on mental health by occupational skill level, and among the highly skilled, white-collar jobs, found longer work hour–health limits of closer to 49 hours.
These and other studies, including systematic reviews, have demonstrated the detrimental impacts of long hours on both physical health and mental health, supporting the presence of work hour–health tipping points (e.g. Sparks et al., Reference Sparks, Cooper, Fried and Shirom1997). Lepinteur (Reference Lepinteur2019) and Lee and Lee (Reference Lee and Lee2016) used quasi-natural experimental data to examine the causal effect of work hours on injuries, death rate, job satisfaction and leisure satisfaction. They made use of exogenous work-hour reductions introduced by the labour law reforms in Portugal, France and Korea, where work hours were reduced from 44 to 40 hours in Portugal and Korea, and from 39 to 35 hours in France. They found highly significant and positive effects of work-hour reduction on population health outcomes. However, these studies, and the work-hour policies they inform, generally consider the workforce in terms of averages. Very few studies consider different ages as well as jobs in the workforce, and both age and job type are likely to challenge how many hours people can work before they compromise their health.
Older people's health and labour market outcomes
A key assumption is that longer lives translate directly and universally into healthier lives and the potential to age successfully. In reality, the relationship between life expectancy and years lived without disability is complex and socially patterned. Thus, in the USA nearly half of recent gains in life expectancy are spent living with disability for both men and women. Furthermore, inequality in health and longevity is clearly documented in older populations (Buck and Maguire, Reference Buck and Maguire2015). This affects older adult employment in three ways. First, it means that older people with disadvantaged social histories have difficulty finding and retaining a job (Kachan et al., Reference Kachan, Fleming, Christ, Muennig, Prado, Tannenbaum, Yang, Caban-Martinez and Lee2015; Taskila et al., Reference Taskila, Shreeve, Laghini and Bevan2015; Welsh et al., Reference Welsh, Strazdins, Charlesworth and Kulik2016). Second, because the work–health–age relationship is dynamic and reciprocal, people whose health deteriorates are much more likely to leave the labour market or reduce their work hours, a health selection phenomenon that drives earnings, wealth accumulation and social status (West, Reference West1991; Kröger et al., Reference Kröger, Pakpahan and Hoffmann2015). Finally, poor health can be a function of poor-quality jobs, whereby low pay and poor conditions combine to impair health, be it physical or mental (Butterworth et al., Reference Butterworth, Leach, McManus and Stansfeld2013), thus the work–health–age relationship depends on job history and quality.
Halleröd and Gustafsson (Reference Halleröd and Gustafsson2011), for example, through an analysis of Swedish panel data over 16 years, describes the way jobs and occupations are pivotal to the way health selection and inequity unfolds over time. Prestigious, well-paid jobs are related to good health at the outset (likely reflecting class gradients in education and opportunity) and to slower deterioration in health when ageing. In contrast, people with poor health may seek low-hour or intermittent employment, and this can generate a downward spiral away from well-paid and health-protective jobs (Kim and DeVaney, Reference Kim and DeVaney2005). This spiral is especially marked among older workers who reduce work hours (or exit altogether) in response to chronic conditions, mental and physical – evidence that work-hour thresholds are lower when health is less than optimal (Pit et al., Reference Pit, Shrestha, Schofield and Passey2013).
There is, therefore, a close interplay between ageing, health and labour market outcomes, and social resources which unfold and reinforce each other over the lifecourse. This suggests that relationships between health, inequity and workforce participation strengthen among older workers, limiting how and for whom employment supports successful ageing (Zaidi et al., Reference Zaidi, Gasior, Hofmarcher, Lelkes, Marin, Rodrigues, Schmidt, Vanhuysse and Zolyomi2013; Daley and Woods, Reference Daley and Woods2014). We propose that there is a weekly work-hour limit beyond which health outcomes such as mental health and vitality deteriorate, depending on age group and occupation or job (white, pink and blue collar). In this paper, we focus on older workers aged 50–70 and stratified by age, occupation and health status.
Our research aims to answer the following research questions (RQ):
RQ1: What is the relationship between weekly work hours and health outcomes (mental and vitality) for older workers who remain in the workforce?
RQ2: Do mental health and vitality work-hour tipping points vary by age and occupation?
RQ3: Do these work hour–health tipping points vary according to older workers' physical health-related status?
We found that the estimated tipping points for older workers (aged 50–70) were almost identical to those of the younger group (aged 25–49) for both mental health and vitality. However, the work-hour limit depends heavily on the type of job, and on physical health status. Our analysis demonstrates the protective health effects of white-collar working conditions, as these workers were able to work 7–9 hours longer than their blue- and pink-collar counterparts, without compromising their health. We also showed how important health status is for work hour–health tipping points, as there was a large disparity in work hour–health limits between those with poor health and those with good health. Our findings indicate it is health, not age, that is one of the most important factors for determining retention among older-age adults, as well as productivity and capacity to work.
Data and empirical method
Data
We used 12 waves of the Household, Income and Labour Dynamics in Australia (HILDA) survey data. HILDA is a nationally representative household-based panel study that began in 2001. Each wave has more than 7,000 households with more than 17,000 household members. Response rates have been consistently high (>90%; Summerfield, Reference Summerfield2011). The survey asks respondents about their employment, family circumstances, health and socio-economic characteristics through face-to-face interviews and self-completed questionnaires. We used data from Waves 5–16 as they contained measures of work conditions important to our modelling; some of the variables were not collected before Wave 5.
We limited the sample to employed adults aged 50–70, defined as older adults who worked in any wave (as long as they worked, they were included in our analysis sample) and who had data on mental health, vitality, wages, work hours and covariates. The maximum number of observations is 29,643 spanning 12 years (2005–2016). Due to missing data, attrition and recruitment of new respondents, the number of observations varies across waves, creating an unbalanced panel. As we used partner's employment and education as either control variables or instruments in models, the sample is further restricted to older workers with at least one partner employed. We tested our results by extending the sample to cover coupled and non-coupled observations in a sensitivity analysis.
Estimation method
Simultaneity between health, wages and work time – a modified Three Stage Least Squares (3SLS) approach
Health is both an input and an outcome of work hours and income, because healthy people are more likely to work longer hours and earn better wages (Doan et al., Reference Doan, Strazdins and Leach2020), while unhealthy people reduce their work hours or leave the labour market. In turn, work hours and income can affect health (O'Reilly and Rosato, Reference O'Reilly and Rosato2013). This creates a reciprocal effect or simultaneity across work hours, wage income and health that challenges conventional approaches such as Ordinary Least Squares (OLS). OLS estimates are likely to be upward biased because of the correlation between the error terms in the work hours and health equations, as well as being unable to disentangle the reciprocal relationships between work hours and health. Some confounders or unobservable factors can also affect work hours and health outcomes, e.g. time spent in physical activity may affect both an individual's work hours and their health, and the relationship between them. For these reasons, OLS estimation likely biases work hour and health associations, as evidenced by our sensitively tests (analyses available on request).
Viewing wages, hours and health as part of a system with reciprocal effects, we followed the Two Stage Least Squares (2SLS) technique used by Grossman and Benham (Reference Grossman, Benham and Perlman1974) and 3SLS to estimate the relationships among the three variables (Dinh et al., Reference Dinh, Strazdins and Welsh2017). The advantage of 3SLS over 2SLS is that it can correct for correlation between-equation error terms (Zellner and Theil, Reference Zellner and Theil1962). However, both methods assume the error terms are homoscedastic and non-autocorrelated, and this can lead to inconsistent estimates of standard errors. Although this can be addressed by applying a Generalized Method of Moments (GMM) (Baum et al., Reference Baum, Schaffer and Stillman2003), GMM models require large sample sizes to be reliable, and place high demands on computer storage and speed when there are multiple panels (as in our data). To overcome the disadvantages of GMM and conventional 3SLS, we employed a bootstrapping estimation technique to a 3SLS approach. The 3SLS bootstrapping estimation can produce unbiased and consistent estimates of coefficients and their standard errors. We applied this model to the couple sample and three sub-samples stratified by age, occupation and health status. We also conducted a sensitivity analysis which used the whole sample (coupled and non-coupled) with different instruments.
Empirical estimation model
The 3SLS bootstrapping estimation as applied to a three-equation simultaneous model is as follows:



In this simultaneous equation system, the dependent variables are health (Hi ,t: mental health, vitality), weekly work hours (Ti ,t) and log of hourly wage rate (lnWi ,t) of individual i in year t. We also controlled for a set of covariates (Xh, Xt, Xw) in the corresponding equations. The time-specific effects on health, work hours and wages were captured in αt, βt, γt. The lagged dependent variable is also entered as a predictor to adjust for large variation between observations due to its historical trend and auto-correlation (Arellano and Honore, Reference Arellano, Honore, James and Edward2001). The error terms (e, u, v) capture measurement errors and unobserved factors. Details of variables used in each equation are described below.
In health Equation 1, apart from work hours (T) and wage rate in logarithm (lnW), we added work hours squared (T 2) to test for non-linear relationships between work hours and health. We also included potential work experience, ethnicity, marital status, work flexibility, work intensity, employment type, occupation, gender, smoking, drinking, and lag of physical activity and lag of general health (all likely to be predictors of health). We added urbanity, state and year dummies to capture the differences in health due to geographic and time factors. In this paper, we focused on mental health and vitality rather than general or physical health because we used weekly work hours. The effects of work hours on mental health and vitality are likely to be observed in a relatively short period of time, whereas any impacts on general health and physical functioning may take several years before they become observable.
The potential endogenous variables of Equation 1 were weekly work hours and wage rate. Instruments for these variables should be correlated with work hours and wage rate but not correlated with the error term of this equation (i.e. the excluded instruments have no direct effect on health outcome). The potential instruments were partner's employment status, partner's education and household non-wage income. We assume that these variables were likely to directly influence an individual's employment, work hours and wages, but only indirectly affect their health. We acknowledge that these instruments may violate the exclusion restriction, Cov(z, error terms) = 0. Under the 3SLS approach, we are unable to directly test this possibility, however, we provide first-stage F-statistics and instrumental variable (IV) test results for the excluded instruments we used (see Table S1 in the online supplementary material). These tests are equivalent to the weak instrument and relevant IV tests (for relevance conditions) – Cragg-Donald Wald F-statistics in 2SLS/IV models (Finlay et al., Reference Finlay, Magnusson and Schaffer2013). The very high F-values (ranging from 92.6 to 604) for the first-stage estimates (significantly greater than 10, a commonly used threshold for weak IV and relevance restriction test) and the test results for excluded instruments being jointly equal to zero in the first stage (all statistically significant at the 1% level) suggest that our instruments satisfy the relevance condition.
In work-hour Equation 2, we included both wage rate (log) and health on the right-hand side of the equation. We also controlled for marital status, gender, prior general health, occupation, location, state and year dummies. The potential instruments for the work-hour equation must have no direct effect on work hours, but be correlated with wages and health. We therefore used lag of log wage, lag of health outcome and socio-economic status such as financial distress as instruments.
In wage Equation 3, we followed the Mincerian earnings equation (Mincer, Reference Mincer1974) to build the wage model. This equation included education and potential experience (its squared term was not added as our sample includes older people (aged 50–70), the non-linear relationship between age or experience with income no longer exists). Gender, ethnicity, location, state and year dummies were also included to capture wage differences across groups, states and years. The prior health (or lagged health) variable was included to capture the influence of workers' health on their productivity and wages. The health variable also represents job-related hazards which may sometimes attract additional pay as a result (Haveman et al., Reference Haveman, Wolfe, Kreider and Stone1994). Work hours were also added in the wage equation as a predictor for wage rate, via wage premiums, overtime and penalty rates. Longer work hours lead to longer (equivalent) work experience that can alter wage rate. Commonly used instruments for the wage equation are those that predict education, but do not directly affect wages. These include father's education, mother's education, sibling's education, partner's education and parents' socio-economic status. In our case, partner's education level was a stronger predictor of other partner's education than father's education and mother's education, and we selected it as our excluded instrument.
Variables and measures
Dependent variables
Five items from the Medical Outcomes Survey 36-item Short Form (SF-36) were summed to assess mental health (Ware, Reference Ware2000). Three items assess nervousness and depression (‘Have you been a very nervous person?’, ‘Have you felt so down in the dumps that nothing could cheer you up?’ and ‘Have you felt downhearted and blue?’) and the other two happiness and calm (‘Have you felt calm and peaceful?’ and ‘Have you been a happy person?’). Vitality was constructed from four questions to assess energy, fatigue and exhaustion (‘Feel full of life’, ‘Have a lot of energy’, ‘Felt worn out’ and ‘Felt tired’). Item responses ranged from 1, ‘none of the time’, to 6, ‘all of the time’. The raw scale scores for both measures were calculated by summing and then transforming to a 0–100 scale, with a higher score meaning better health. Weekly work hours were measured by respondents' reported hours worked in all jobs. Hourly wage rate (log wage) was calculated by dividing weekly wages and salary from all jobs by weekly work hours. All the monetary variables in this paper were discounted to the 2016 price.
Covariates and variables
The covariates, variables and their definitions are presented in Table 1.
• Stratification and interaction variables.
In models for occupation (a ‘white’ dummy variable: white- versus pink/blue-collar workers), the white-collar group includes managers, professionals, clerical and administrative workers, and the pink/blue-collar group includes the remaining occupations. The white-collar jobs are high-status/well-paid jobs, while pink/blue-collar jobs are lower-status jobs which are often physically demanding (Schreuder et al., Reference Schreuder, Roelen, Koopmans and Groothoff2008). The ‘white’ dummy variable was interacted with work hours and its squared term to capture the shift of the coefficients between the occupations. We created four categories for age comparisons of the estimates: younger workers (aged 25–49), older workers (aged 50–70) and then two subgroups of older workers (50–59 and 60–70 years) (Table 2).
Table 1. Covariate and variable definition and coding

Notes: OECD: Organisation for Economic Co-operation and Development. ANZSCO: Australian and New Zealand Standard Classification of Occupations.
We also model for health status using physical function distribution cut-offs at the 20th percentile (pc), 30th pc and median to see if the mental health and vitality tipping point varies by workers' physical health status. Physical health impacts of work hours are likely to be chronic, cumulative and longer term and so require different models to 3SLS. However, we expected that mental health and vitality tipping points would be at least partly a function of physical health status, and it is important to estimate this because of the ‘healthy worker’ bias implicit in older employed samples. For example, Medic et al. (Reference Medic, Wille and Hemels2017) showed that sleep disruption causes short-term effects on mental health-related health including increased stress responsivity, somatic pain, reduced quality of life, emotional distress and mood disorders, and cognitive, memory and performance deficits. However, it takes a much longer time to affect physical health outcomes. The long-term consequences of sleep disruption include dyslipidemia, cardiovascular disease and weight problems.
In our models, we were aware of potential reverse causality between general health and our health outcome variables (mental health and vitality). As such, we controlled for prior general health to avoid such possible reverse causality biases. We use physical functioning to stratify for health status.
Descriptive statistics
Table 2 displays differences in some key variables across age, occupation and health status groups. In relation to younger workers (25–49), older workers (50–70) have slightly better mental health and vitality, but worse general health, they worked about 2 hours less each week, and spent 1.4 hour less on unpaid work. They were better off in terms of non-wage income and financial distress, and they smoked and drank less.
Table 2. Sample characteristics by age, occupation and health strata (employed people sample)

Notes: Means were adjusted for sample weights. Ethnicity, state and year dummies were used in the models but are not shown. <30th pc PF: a group whose general health is below the 30th percentile of physical functioning distribution for employed people aged 50–70. >50th pc PF: a group whose physical functioning is on or above the 50th percentile of physical functioning distribution.
White-collar workers worked longer hours than their pink- and blue-collar counterparts and received a significantly higher weekly wage (Aus $1,276 versus $917). They had higher non-wage income, were more educated and faced less financial distress than pink- or blue-collar counterparts. White-collar workers also enjoyed more favourable working conditions including flexible work, and job security (fixed-term and permanent jobs) and job control, and they smoked and drank less than their pink/blue-collar counterparts. Workers with better health (physical functioning) were more advantaged than the poorer health status group in almost all aspects, even though they had quite similar paid hours and work experience.
Empirical results
Work-hour heath tipping points by age
In Table 3, only the summarised estimates for work hours and its squared term were reported to remain succinct (for full set of estimates, see Table S2 in the online supplementary material). A non-linear relationship between work hours and health (mental health and vitality) was found. The estimates of work hours and its squared terms are highly statistically significant (p < 0.001). An inverted U-shaped relationship was observed due to the positive coefficient of work hours and negative coefficient of its squared terms (the tipping point is where the first derivative of the health function equals zero, solution to this problem is the value of work hours or tipping point). Accordingly, the tipping point for mental health was 39.4 and 39.8 hours for the groups aged 25–49 and 50–70, respectively (Table 3; Figure 1). The vitality tipping point was 38.8 and 39 hours for the groups aged 25–49 and 50–70, respectively (Table 3; Figure 1, bottom panel). The thresholds for both groups were close to the overall workforce (25–64 years) estimations (see Dinh et al., Reference Dinh, Strazdins and Welsh2017). Overall, the estimated tipping points for both age groups were almost identical with no significant difference for both mental health and vitality. Table S1 in the online supplementary material provides the first-stage estimates and IV test results.

Figure 1. Work hour–health tipping points by age.
Table 3. Summary of work hour–health tipping points, by age

Notes: Bootstrapped standard errors (SE) in parentheses with 1,000 replications. Apart from the model specification in Equations 1–3 and variables mentioned in the ‘Variables and measures’ section, the health equation was further adjusted for work flexibility, work intensity, ethnicity, marital status, employment contract type, work experience, gender, unpaid time, occupation, lag of general health status, smoking and drinking status, lag of physical activity, and state, urbanity and year dummies. The work-hour equation was controlled further for marital status, gender, lag of general health, occupation, and state, urbanity and year dummies. The wage equation was controlled further for education level, work experience, ethnicity, gender, and state, urbanity and year dummies. Tables 4, 5 and 8 also have the same set of covariates.
Significance levels: * p < 0.01, ** p < 0.05, *** p < 0.01.
Sub-age group analysis was undertaken for the 50–59 and 60–70 age groups. All estimates of work hours and its squared terms were statistically significant except for squared work hours for the 60–70 age group. Significance declined by age group due to reduced sample size. The tipping point for the 60–70 age group was slightly lower (3–4 hours per week) than for the 50–59 age group. This was somewhat less than we anticipated as we expected deteriorating physical health amongst those age 60–70 would significantly reduce their work hour–health limit.
The predicted health curves for the older subgroups were above younger group curves for both mental health and vitality, suggesting that they have better mental health and vitality compared to the youngest group (25–49 years) across all work hours (Figure 1).
Work hour–health tipping points by occupation
Table 4 and Figure 2 display the work hour–health threshold by occupation (white-collar versus pink/blue-collar workers) (for full set of estimates, see Table S3 in the online supplementary material). The work hour–health tipping point for white-collar workers aged 50–70 was 44 and 46 hours for vitality and mental health, respectively, compared to 37 and 37.3 hours for pink/blue-collar workers. The large difference (around 8 hours) in tipping points between white- and blue/pink-collar occupations was considerably greater than differences between age subgroups.

Figure 2. Work hour–health tipping points by occupation.
Table 4. Summary of work hour–health tipping points among workers aged 50–70, by occupation
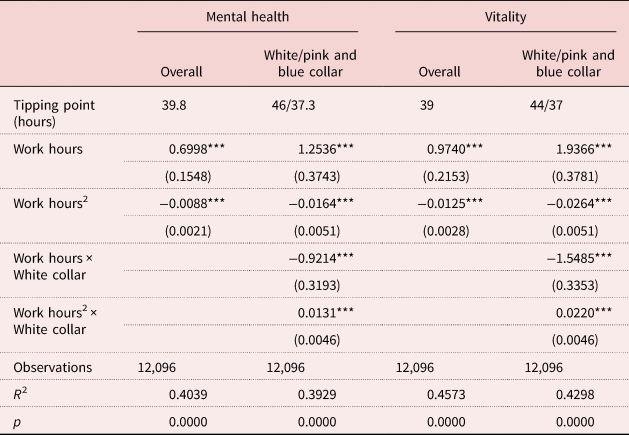
Note: See Notes of Table 3.
Significance level: *** p < 0.01.
More interestingly, the curvilinear relationship is stronger for pink/blue-collar workers than white-collar workers, suggesting that longer work hours have a greater effect (in both positive and negative directions) on their mental health and vitality (Figure 2).
Work hour–health tipping points by health status
Work hour–health tipping points for health subgroups – relatively poor health (under the 20th pc, under the 30th pc) and better health (over the 50th pc or above the median health) – for physical functioning are displayed in Table 5 and Figure 3 (for full set of estimates, see Table S4 in the online supplementary material). Those in the groups of <20th pc and <30th pc health distribution (physical functioning) were considered to have relatively poor health, with those in the >50th pc group health were considered to have relatively good health or ‘better health’, compared to the 50–70 group average. Our estimates show a large difference in tipping points between those with relatively poor health and those with better health. The gap was 7 hours for mental health and 11 hours for vitality when stratified by physical functioning (Table 5). Further, workers with relatively poor health (physical functioning) had significantly lower predicted mental health and vitality scores (lower curves) (Figure 3).

Figure 3. Work hour–health tipping points by physical functioning status.
Note: pc: percentile.
Table 5. Estimated tipping points for mental health and vitality by physical functioning status (ages 50–70)

Notes: See Notes of Table 3. pc: percentile.
Significance levels: ** p < 0.05, *** p < 0.01.
Health selection bias and sensitivity analysis
Health selection
Our sample likely represents a particularly healthy group due to health selection (which increases as people age) and is not representative of the population aged 50–70. Consequently, our work-hour–health limit estimates may be inflated and not generalisable to older adults who have already exited the labour market. Therefore, we performed some exploratory analysis, comparing our (relatively healthy) employed sample to counterparts not in the labour market after they turned 50.
Simple estimates in Table 6 show clear health gaps between our sample and non-working counterparts, with employed people aged 50–70 reporting better health for all health measures. Furthermore, the standard deviations for the non-working group were larger, indicative of health variation within this group.
Table 6. Health differences between working and non-working, aged 50–70

Source: Authors’ estimation from the Household, Income and Labour Dynamics in Australia (HILDA) survey, 2005–2016, adjusted for sample weights.
Using a longitudinal logistic model, all prior health measures strongly affected the probability of labour market participation for those aged 50–70, thereby supporting the occurrence of health selection (Table 7).
Table 7. Health conditions and working status, longitudinal (Random Effect) logistic model, aged 50–70

Notes: Standard errors in parentheses. Models also controlled for lags of net wealth, financial distress, non-wage income, age, unpaid time, marital status, gender, education level, ethnicity, state and year dummies.
Significance level: *** p < 0.01.
Sensitivity analyses
To test the robustness of our estimates, some model specifications were altered. First, we excluded work hours from the wage equation (Equation 3), to be in line with the labour supply and wage equation in labour economics literature, resulting in almost no change to tipping points. Second, as contemporary weekly work hours may not capture the regularity of working long (or short) hours, we used ‘percentage of time spent in jobs in last 12 months’ to approximate actual annual work hours, which yielded similar results (available upon request). Third, the use of partner's employment and individual characteristics, such as education, as either covariates or instruments in the main analysis restricted the sample to coupled people. Thus, to improve generalisability, partner's variables were excluded, and our sample expanded to include both coupled and non-coupled people aged 50–70. We used lags of log wage, non-wage income, financial distress index, lags of health outcomes and lags of weekly work hours as instruments in the first stage of estimation. Tipping points remained relatively unchanged (Table 8 versus Table 2).
Table 8. Summary of estimated tipping points for mental health and vitality using the whole working sample

Note: See Notes of Table 3.
Significance level: *** p < 0.01.
Fourth, one may argue that individual mental health/vitality may also affect choice of occupation and job characteristics (flexibility, intensity). That is, these job characteristics are not exogenous to mental health and vitality, particularly in the long term. For example, a person may move from their main occupation/job in the long term due to economic structure change or a significant change to their health status, but may not in the short term, which is our current paper's focus. To consolidate our findings, we have tried models with lags of the occupation and job characteristics to make sure they are exogenous in the health equation; the estimated tipping point did not change much (a small change in tipping point may be due to a shrunk sample size). Financial distress affects mental health in the very short term, and may also affect work hours, likely over a longer timeframe as people need time to adjust their work hours. We also tried models with lags of financial distress as an instrument in the work-hour equation, and the results did not change much (results available upon request). Finally, we explored Tobit models and propensity score matching to estimate tipping points on the non-working 50–70 years group. These models required extensive imputation of all employment-related data, problematic for both approaches. Under the matching or propensity score matching approach, however, we were able to estimate tipping points that covered the whole sample. These were between 1 and 2 hours per week lower, likely due to the poorer health status of the non-working group. These results supply suggestive evidence that our estimates, because they are based on a selected, healthy 50–70 years sample, are over-estimating the population work hour–health tipping points. They confirm the stratified models by health status which showed that among the less than optimally healthy older adults, tipping points are considerably lower (see Table 5; Figure 3).
Findings summary, discussion, contribution, study limitations and conclusion
Findings summary and discussion
Using Australian population-representative data to estimate work hour–health thresholds for older workers (aged 50–70), we found that their estimated tipping points were almost identical to those of younger workers (aged 25–49) for both mental health and vitality. We find, on average, working a full-time week of 39–40 hours does not compromise older workers' mental health or vitality. Thus, many older-age adults can work as long as younger adults. Our study supplies further evidence that an ageing workforce has potential to be equally productive, and employment needs to be re-engineered to enable this (Riley and Riley, Reference Riley and Riley1994). However, there are important caveats and contexts to these findings; we further show that the work hour and health relationship depends heavily on the type of job, and on the physical health status of an older worker.
Our estimates show that among the optimally healthy, a full-time working week appears to be both feasible and health supporting, and good health enables older adults to maintain similar levels of engagement as to when they were younger. For these older adults, extended employment can be a potential pathway for financial security as well as better engagement socially, and underscores the significance of labour markets as key institution for successful ageing (Zaidi et al., Reference Zaidi, Gasior, Hofmarcher, Lelkes, Marin, Rodrigues, Schmidt, Vanhuysse and Zolyomi2013; Rowe and Kahn, Reference Rowe and Kahn2015). However, optimal health is found among only a proportion of all older adults and is closely related to occupational history, status and earnings. Among the less-healthy, lower-status older workforce, large gaps in work-hour capabilities were observed. When we stratified by physical functioning we found that, for these older adults, their working week was shortened by between 7 and 11 hours and they were also earning, hour for hour, lower wages. Less-healthy workers therefore face a dilemma as they age: working longer hours to increase financial security confronts them with further health trade-offs. For the growing group of less than optimally healthy older adults, employment offers a mixed bag of supports for successful ageing.
Similarly, occupation had a significant influence on work hour–health thresholds, due to variation in work environments and health demands that connect jobs with earnings and status. Blue- and pink-collar occupations are usually associated with more physically demanding and hazardous environments (Ravesteijn et al., Reference Ravesteijn, van Kippersluis and van Doorslaer2018), offering less pay, control, flexibility and security (Costa and Sartori, Reference Costa and Sartori2007; Eurofound, 2017), all of which negatively impact health. By contrast, higher-status white-collar jobs generally offer greater job security, control and higher wage rates (Matthews and Weaver, Reference Matthews and Weaver1996; Schreuder et al., Reference Schreuder, Roelen, Koopmans and Groothoff2008). Our analysis demonstrates the protective health effects of white-collar working conditions, as these workers were able to work between 7 and 9 hours longer than their blue- and pink-collar counterparts without compromising health. As is the case for older workers with poorer health, the value of extending employment to support successful ageing is qualified by the job conditions and status of workers. There is a major challenge emerging for successful ageing if it is to be widespread and fair, as contemporary labour markets are increasingly polarising into ‘good’ and ‘bad’ jobs (with a corresponding polarisation in income and health). The structural lag in this instance is selective, unequal and increasingly pernicious to the already vulnerable. Our findings indicate that age-integrated reform needs to target employment inequality if it is to achieve a structural change that addresses population ageing (Riley and Riley, Reference Riley and Riley1994).
A key context and caveat to our findings is that all models were estimated on relatively healthy older workers who are not representative of the population. When we stratified by health status among those who were working (an imperfect solution to deal with health selection), we showed how important health status is for work hour–health tipping points, as there was a large disparity in work hour–health limits between those with poor health and those with good health. We further show how important poor health is for workforce exit in a series of regressions, and our exploratory work reported in the sensitivity analyses indicate that tipping points would be considerably lower if they were not estimated on optimally healthy mature-age adults. Together, our findings indicate it is health and job status, not age, that are the most important factors for determining retention among older-age adults, as well as their productivity and capacity to work. It is vital to recognise that good health and good jobs are requirements for remaining in the labour market and enabling successful ageing.
Contribution
This study represents the first demonstration of work hour–health tipping points for older Australian workers. It consists of an in-depth analysis by age, occupation and health status to illustrate the complex and dynamic relationship between work time, wages and health as they relate to extended working lives and population ageing. We used 3SLS to deal with reverse and reciprocal relationships and applied the bootstrapping 3SLS estimation technique to address heteroscedasticity in the equation errors. This enabled us to estimate a system of three simultaneous equations of health, work hours and wages, in what we believe to be the most robust way possible. Although the HILDA data are insufficient to control for sample selection bias, we were able to demonstrate the health selection bias in our estimates by conducting a series of extra analyses that found large differences in health outcomes between our analysis sample and the excluded sample. These findings provide further evidence of the impact of poor health on labour market participation amongst older workers, and the need for reforms of both the labour markets and the health system to redress it.
Our approach combines political economy and sociological insights into structural processes in labour markets (work hours and job status) with epidemiological and econometric methods and theory on work and health relationships. This inter-disciplinary analysis sheds light on social inequality processes as they relate to a key institution – the labour market – in the context of ageing. Our findings support current theory on the critical role of employment as a mechanism for successful ageing, but challenge assumptions that it offers a pathway for all. We also show that two key elements of successful ageing – mental and physical health and continued engagement in social and productive activities – are neither simply nor equally related. They can be in conflict, for example, when mature-age adults are working hours that compromise their health, if their health is already deteriorating or if they work in poor-quality jobs. Re-engineering labour markets to be age-integrated requires making them more equal and more health promoting in the jobs and conditions they offer (Rowe and Kahn, Reference Rowe and Kahn2015).
Study limitations and future research
The 3SLS approach with the bootstrapping estimation technique was used to address simultaneity, reciprocal relationships and heteroscedasticity in the error terms. This approach enables us to estimate robustly tipping points for the work hour–health relationship because it can address reciprocal relationships. However, inferences on causality cannot be made from this model because the 3SLS model does not allow us to test the exclusion restriction. Furthermore, the estimated tipping points are likely upward biased due to health selection (as suggested by sensitivity tests using OLS, fixed-effects approaches), which may have an increasingly strong effect on an older workforce, thus making the employed sample non-representative of the overall population aged 50–70.
Unlike previous studies, we adjusted for time spent in care and domestic work in our modelling, which is likely to affect overall work hour–health tipping points (Dinh et al., Reference Dinh, Strazdins and Welsh2017). However, time in unpaid work (e.g. caring) remains highly gendered even among older workers, and likely contributes to differences in tipping points by gender. These complex connections between time on and off the job, age, gender and care-giving are therefore worthy of future research. Furthermore, the impact of accumulated work time over long periods (annual hours rather than weekly hours as used in this study) could provide greater insight into health impacts and associations with chronic, physical health conditions including overweight and obesity which may take several years to become evident. Finally, our study does not address the role played by motivations and incentives, from employers in particular, to reward or limit older workers' work hours.
Conclusion
A predicament is arising for older workers. They are experiencing longer life expectancies, but retirement policies encouraging older workers to remain employed into older age do not take into account the importance of having optimal health and jobs to do so. As we have shown, health status and occupation significantly influence weekly work-hour thresholds beyond which mental health and vitality amongst older workers decline. Poor health amongst older workers reduces the work-hour threshold by 7–11 hours for mental health and vitality, respectively, when compared to the capabilities among those in good general health. The work-hour threshold for older blue- and pink-collar workers is 7–8 hours less than for their white-collar counterparts. These gaps in work hour–health thresholds indicate that ‘older workers’ are not a monolithic group, with important differences in weekly work-hour abilities according to health status and occupation type.
Across the OECD, life expectancies are increasing, and longer working lives are being encouraged and promoted as the way to resource them. However, simply extending the pension eligibility age, or implementing policies which treat older workers as uniformly able to extend their working lives, fails to recognise the complexity and inequalities of factors influencing labour participation for these workers. Those in high-status and high-paying jobs may well be able to work longer into older age, but those in less-privileged and poorer-paid occupations, with poorer health, are unlikely be able to fulfil this policy expectation. If the agenda to promote older-worker employment is to be achieved, and achieved equitably, the focus on changing the retirement age as a mean to address the costs of an ageing population must be shifted. Instead, addressing poor health and poor working conditions, which generate increasing work hour–health tradeoffs as people age, should be a priority for employment and ageing policy.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0144686X22000411.
Acknowledgements
This paper uses unit record data from the Household, Income and Labour Dynamics in Australia (HILDA) survey, 2005–2016. The HILDA Project was initiated and is funded by the Australian Government Department of Social Services (DSS) and is managed by the Melbourne Institute of Applied Economic and Social Research (Melbourne Institute). The findings and views reported in this paper, however, are those of the authors and should not be attributed to either the DSS or Melbourne Institute.
Financial support
This work is part of a larger project supported by the Australian Research Council (linkage grant number LP160100467).
Conflict of interest
The authors declare no conflicts of interest.













