Schizophrenia is a long-term condition. Many people continue to experience residual symptoms after the first episode. Some suffer relapses, or remain ill and functionally impaired (Reference Robinson, Woerner and McMenimanRobinson 2004). Any outcome measure for schizophrenia needs to be capable of delivering a meaningful assessment of an individual's experience across their lifespan as well as in the short term; episodic outcome measures may miss the long-term cumulative effects of schizophrenia. Outcome measures must be capable of informing clinical decision-making. They should contribute to reviews and care-planning. New recovery measures show promise, but they do not generally measure symptomatic improvement over the short and medium time scales involved in a hospital admission and immediate aftercare.
Outcome measures should provide healthcare funders with information about the effectiveness of interventions and services. For clinicians they should be quick and easy to use and have a solid evidence base. The outcomes themselves should be meaningful to mental health service users and their families. A single measure that satisfies all these stakeholders would be ideal.
A survey of 340 UK psychiatrists revealed a low rate of routine use of outcome measures and a general attitude that such measures are not useful. Its authors concluded: ‘Outcomes measurement is a “technology” that has opportunity costs and therefore must be shown to be beneficial in improving the quality of care as measured by actual outcomes of patients or communities. No direct evidence exists that there is a benefit in this respect for those working and being cared for in either primary care or specialist psychiatric services’ (Reference Gilbody, House and SheldonGilbody 2002).
Since the early 1990s, policy makers in the UK have taken an increasing interest in outcome measures and services are encouraged to introduce them (Department of Health 2005). However, the statement above may still be accurate. Clinicians may not be convinced that measuring outcomes improves patient care and may feel that the time taken to perform measurement is time that could be better used delivering that care.
Resolution and remission in schizophrenia
A good approach to studying the outcome of schizophrenia is to measure the disappearance or resolution of symptoms and signs (Reference Peuskens, van Vleymen and KaufmanPeuskens 2007). If someone who has had schizophrenia no longer has symptoms and signs then they are better. This is familiar territory for mental health professionals. Resolution of symptoms is often seen as the primary endpoint of acute interventions such as hospital admission or medication treatment. Yet this resolution of symptoms is a momentary achievement. For many people, it does not last (Reference Robinson, Woerner and McMenimanRobinson 2004). A lasting resolution of symptoms and signs is called a remission (Box 1). A person with schizophrenia in remission is clinically well. If this clinical outcome correlates with subjective well-being then it could be meaningful to patients. As we shall see below, schizophrenia sufferers in remission do better than those who achieve only brief symptom resolution (Box 2).
BOX 1 Resolution and remission

| Resolution | Remission | |
|---|---|---|
| Symptomatic requirement | Minimal symptoms below a set threshold on all symptom domains | Minimal symptoms below a set threshold on all symptom domains |
| Time requirement | No time specified | Lasting at least 6 months |
BOX 2 Reported benefits of remission over resolution
-
• Better quality of life
-
• Longer time symptom free
-
• Positive attitude to medication
-
• Lower doses of medication
-
• Fewer extrapyramidal symptoms
-
• Better global function
-
• Better insight
Standardised remission criteria: a Consensus Group solution
A research standard for remission in schizophrenia was described in 2005 by a Consensus Group led by Andreasen et al. This group included international experts and reached a consensus on a definition of remission that had two components (Reference Andreasen, Carpenter and KaneAndreasen 2005).
The severity component: resolution
The first component was a measure of the severity of symptoms and signs (i.e. resolution). For this component they chose a well-used, validated scale, the Positive and Negative Syndrome Scale (PANSS) (Reference Kay, Fiszbein and OplerKay 1987). Recognising a certain amount of redundancy in the full PANSS, they extracted eight PANSS items to represent three core domains of schizophrenia: positive symptoms, negative symptoms and disorganisation of thinking and behaviour (Box 3). Each item is defined within the PANSS and correlates very much with what most psychiatrists would expect by the terms used. For example, ‘hallucinatory behaviour’ refers to verbal report or behaviour indicating perceptions that are not generated by external stimuli. ‘Unusual thought content’ refers to strange, fantastic or bizarre ideas that are not necessarily delusional. Each item is rated separately on a scale of 1 to 7, with 7 the most severe rating. The group recommended that, to meet the severity criterion of remission, each of the eight items should score 3 or less (see Box 4): no symptom or sign should be rated more than mild.
BOX 3 The eight PANSS symptoms and signs used to rate remission
| Symptoms and signs | Domain |
|---|---|
| Delusions | Positive symptom |
| Unusual thought content | Positive symptom |
| Hallucinatory behaviour | Positive symptom |
| Conceptual disorganisation | Disorganisation |
| Mannerisms/posturing | Disorganisation |
| Blunted affect | Negative symptom |
| Social withdrawal | Negative symptom |
| Lack of spontaneity | Negative symptom |
| (Reference Andreasen, Carpenter and KaneAndreasen 2005) |
BOX 4 Generic rating guide for PANSS symptoms
| Rating level | For all symptoms and signs |
|---|---|
| 1 Absent | Absent |
| 2 Minimal | Questionable pathology, extreme normal limits |
| 3 Mild | Symptoms are clearly present but vague and relatively unobtrusive. They do not interfere with thinking, social relations or behaviour |
| 4 Moderate | Symptoms are several and unquestionable but shifting and only occasionally interfere with thinking, social relations and behaviour |
| 5 Moderately severe | Symptoms clearly manifest and preoccupy patient, occasionally interfere with thinking, social relations and behaviour |
| 6 Severe | Symptoms extensive and manifest, preoccupy patient and clearly interfere with thinking, social relations and behaviour |
| 7 Extreme | Symptoms are severe and extensive and dominate major facets of life, leading to often inappropriate, irresponsible actions |
The original PANSS has specific rating criteria for each symptom or sign. Basic PANSS training can be completed in a single day. For those with less time, we have condensed the eight specific ratings into a generic rating system for ease of use in clinical settings (Box 4). Delusions rated on the original PANSS scale at severity grade 3 would have the following characteristics: ‘One or two delusions, which are vague, un-crystallized and not tenaciously held. Delusions do not interfere with thinking, social relations or behaviour’ (Reference Kay, Fiszbein and OplerKay 1987). On our generic rating system this becomes: ‘Symptoms are clearly present but vague and relatively unobtrusive. They do not interfere with thinking, social relations or behaviour’.
The time component: remission
The Consensus Group importantly put forward a second component of remission. This is a time component. The group wanted to move away from easily achieved targets of brief symptom reduction to a more demanding goal of prolonged wellness. They recommend that for remission to be considered achieved, all eight symptoms and signs should rate 3 or less for a period of 6 months.
Evaluation of the Consensus Group criteria
In their review of the Consensus Group's definition of remission, Reference van Os, Burns and Cavallarovan Os et al (2006) felt that the remission concept would be useful for clinical trials and could be easily used in clinical practice. They suggested that using the concept would increase expectations of treatment and facilitate discussions about treatment objectives. They hoped that the remission concept might inform decisions about discharge from hospital, but thought that the 6-month criterion for remission would make it difficult to facilitate service-level decisions in fast-moving clinical services. However, they considered the severity component of the definition (resolution) valuable in assessing readiness for discharge.
Clinical Global Impression–Schizophrenia scale
Another proposed measure of remission is the Clinical Global Impression–Schizophrenia (CGI–SCH) scale (Reference Haro, Kamath and OchoaHaro 2003). It is very brief and relies on the clinical impressions of the rater. It covers the domains of positive and negative symptoms and cognition. It also adds the domains of depression and of overall severity of illness. The CGI–SCH scale can be rated serially over time but it also allows the rater to use a ‘change’ scale for each domain instead of using serial measurements. This means that the rater can make an estimate of how much a patient's symptoms have changed at a single clinical contact. To mark remission, the authors suggest using the same cut off of 3 or less (mildly, minimally or not ill) on their 7-point scales (1, not ill; 7, among the most severely ill) on each of the positive, negative, cognitive and overall severity scales (Reference Haro, Ochoa and GervinHaro 2007). They do not require a particular period of time to have elapsed before remission status is considered to have been achieved. Therefore their definition is a measure of symptom resolution and is different from the standard required by the Consensus Group (Reference Andreasen, Carpenter and KaneAndreasen 2005). It is of course simple to add the 6-month criterion to make CGI–SCH remission comparable to the Consensus Group definition.
Summary of research
The literature investigating the concept of remission is growing. Studies have addressed both the severity component of the concept (resolution) and full remission with the important 6-month duration component. Several studies have compared patients achieving resolution with patients who maintain resolution for 6 months and achieve remission. One naturalistic cohort study examined the symptom severity component and the duration component of the remission criteria separately (Reference De Hert, van Winkel and WampersDe Hert 2007). Of the 341 Belgian participants involved, all of whom had schizophrenia or schizoaffective disorder, those who initially met just the severity criterion (resolution) had a poorer outcome at endpoint than those who had also met the 6-month duration criterion (remission). Those in remission had higher global function, fewer symptoms and better insight into illness at endpoint. In first-episode schizophrenia as well, remission is associated with better symptomatic and functional outcomes than non-remission (Reference Wunderink, Nienhuis and SytemaWunderink 2007; Reference Addington and AddingtonAddington 2008).
Symptom resolution proceeds to remission in many patients. In the naturalistic cohort study just discussed (Reference De Hert, van Winkel and WampersDe Hert 2007), 21% of the patients who had not met remission criteria at baseline achieved remission on treatment within a year. Another 1-year study, of long-acting risperidone injection for schizophrenia or schizoaffective disorder, found that two-thirds of the 578 clinically stable patients considered to be well were not in remission at baseline (Reference Lasser, Bossie and GharabawiLasser 2005). With risperidone treatment, one-fifth of those non-remitted at baseline felt that their health had improved and achieved remission for at least 6 months. This suggests that systematic enquiry into mental state reveals treatable residual symptoms for a significant number of patients.
Remission was also investigated as part of a retrospective observational study (the European Schizophrenia Outpatient Health Outcomes – SOHO) in Germany (Reference Lambert, Naber and SchachtLambert 2008a). Untreated patients with recent first episodes of clinically defined schizophrenia were included and followed for up to 3 years while receiving standard clinical care. Outcomes were measured using the CGI–SCH scale (Reference Haro, Kamath and OchoaHaro 2003). At baseline 6% of patients were in remission and at endpoint 60% were.
The importance of the time component of remission was demonstrated in a large study of medication treatment of 462 individuals with first-episode psychosis over 2–4 years (Reference Emsley, Rabinowitz and MedoriEmsley 2007). During the study, 323 (70%) participants achieved resolution according to the severity criteria and 109 (24%) maintained this status for 6 months, reaching remission. The best predictors of reaching remission were shorter duration of untreated psychosis and treatment response at 6 weeks. Patients in remission, in comparison with non-remitters, reported better quality of life, fewer relapses, a more positive attitude to medication and fewer extrapyramidal side-effects. They also received lower doses of medication. The two groups did not differ on composite cognitive scores.
The research to date shows that one of the key uses of remission assessment is to reveal patients with residual symptoms. From all the studies with controlled and naturalistic samples that we found in the literature, 20–60% of stable but unremitted patients can achieve remission with treatment. In the controlled research samples, 75–80% of patients do not proceed from resolution to remission. This is a key finding suggesting limitations to current treatment approaches when the high standards of remission are employed. Despite this overall finding, the significant minority (20–25%) who do achieve remission have better symptomatic improvement, better social function and improved quality of life.
This section is summarised in Key points 1.
The usefulness of remission
The above studies suggest that if people who have experienced schizophrenia achieve 6-month remission, their well-being and function advances beyond those of people with shorter symptomatic improvement. If mental health organisations wish to work towards these outcomes, they might consider the use of remission assessment in routine practice. In an ideal world, clinicians and managers would want to use the same measures, and remission is a candidate for such a universal measure.
Using remission assessment in practice
Let's accept for now that a standard remission measure based on the 8-item modified PANSS score is practical. It takes about 5 min to complete using the generic rating guide in Box 4. We can measure whether patients with a diagnosis of schizophrenia are ill (any item scores ≥ 4) or whether they are in resolution (all items ≤ 3) or in remission (all items ≥ 3 for 6 months). Let's assume we can collect the data in an analytical program such as a spreadsheet or database. What can we do with them? We could see how long it takes patients to achieve resolution, the first stage of remission. This is a useful measure for acute services. We could follow this up after discharge by measuring how many people then achieve remission in the community. We could measure how long it is before patients relapse (if they do). These are helpful measures for community services and primary care.
To see which service activities appear to be associated with resolution and remission, a measure of adherence would be helpful. Evidence suggests that treatment adherence is generally lower than we assume (Reference Coldham, Addington and AddingtonColdham 2002; Reference Keith and KaneKeith 2003). Medical treatment may vary in effectiveness, depending on whether it is given orally or by injection and whether it is supported by good clinical care.
If a service user has a persistent illness, the lack of remission could trigger a treatment review. We might ask our teams, ‘Why is this person not getting well?’ If we expect remission to occur, that could make us more ambitious to help achieve it (Reference Nasrallah and DursunNasrallah 2006). Perhaps more pragmatically, if we notice that remission is slow in coming, we could match that progress to an appropriate treatment stream. Some patients might do better in a stream with more psychosocial work, or more carer support. We could use remission to redirect resources, to give up on ineffective treatment, to reformulate our clinical understanding of service users and to change care plans (Reference MortimerMortimer 2005).
The extent of non-remission and its quality could help us characterise illness experiences using the three symptom domains of positive and negative symptoms and disorganisation. The PANSS scale will show whether negative symptoms are more problematic than positive or disorganised ones and how severe each symptom is. A partial remission with only severe hallucinations could be considered differently from a partial remission with social withdrawal, blunted affect and lack of spontaneity. If we systematically monitor remission then this should help us detect and treat relapses early, as exemplified in the following fictional case study.
Case study
Richard is a 28-year-old man with a diagnosis of schizophrenia since the age of 20 and five hospital admissions for acute psychosis between the ages of 20 and 22. He lives with his parents and has never been able to work. He appears to be asymptomatic for positive symptoms and disorganised thinking but has negative symptoms, including social withdrawal. He has been on depot medication for 6 years. He is unwilling to engage in recovery work. In the course of a remission rating, Richard revealed that he had started hearing a voice several months ago telling him to cut off his fingers to prevent contaminating his parents with evil. A risk assessment concluded that self-harm was likely and he was admitted to hospital to reduce risk and change his care plan. He was able to speak about his concerns to nurses, but remained unwell and apathetic. An alternative depot medication was started, and after 4 weeks Richard reported that the voice had gone and he no longer wanted to cut off his fingers. He no longer thought that he could contaminate anyone with evil. Remission ratings 6 months after discharge confirmed minimal positive and disorganised symptoms but moderately severe negative symptoms. Richard continues to decline all offers of recovery work, but has taken up playing the piano at home. He says he thinks the medication is worthwhile (‘I feel more relaxed’) although he does not think it is connected to the reduction in positive symptoms.
Discussion
Richard had seemed stable for years and reported no positive symptoms in the course of routine contact with the community mental health team. Only on systematic enquiry did he reveal his concerns about hearing a voice, contamination and self-harm. Hospital treatment was associated with a lasting reduction in distress mirrored by the remission assessment for positive symptoms after discharge. The remission assessment also emphasised the extent of persistent negative symptoms. Richard has not achieved resolution or remission, but understanding the nature of the non-remission has led to better treatment outcomes for positive symptoms and established the severity of negative symptoms. The care team is now working to encourage Richard to spend time in a community-based, residential voluntary sector service that is successful at developing independent living and social skills.
Using timelines with remission
If we determine the time, from illness onset, that it takes to achieve remission we get another measure of treatment effectiveness. The faster someone achieves remission the better. Not only do patients suffer fewer traumas from the horrific experiences of psychosis, but services are likely to spend less money on each person, allowing more people to be treated. Services can use resolution and remission to gauge entry to and exit from service components. Discharge from hospital to community services when ill could lead to expensive readmission. Discharge in resolution or remission could lead to better long-term outcomes and fewer relapses. Remission could signal readiness for primary care and voluntary sector services to take an active role in long-term care.
Figure 1 shows a clinical monitoring approach to remission. Four cases are presented as timelines. In the chart, the time component is given priority and is shown on the horizontal axis. Each of the four cases has a very different timeline. Case D has a good outcome: the patient had a short illness with a greater proportion of time (60%) spent in remission. The extended measure of the proportion of time spent in remission since onset of schizophrenia could be the framework in which remission is used as a commissioning standard. It is easy to see that case B has a better outcome than cases A and C. The patient in case C has spent no time in remission in a 10-year period.
It appears likely from the studies conducted so far that subjective wellness and function would mirror extended remission. Clinicians and service funders can audit the difference in outcomes between cases. At 6 years since onset, the patient in case A has had more relapses and achieved 25% of time in remission compared with 75% in case B. Why? If we add treatments and other service inputs to the timeline we could infer how inputs are linked to outcome. We should also consider case-mix, which is the variation in patient presentations: patients with fewer, milder symptoms may achieve remission more easily than those with more severe symptoms and comorbid substance misuse. Treatment adherence should be considered. Failure to progress to full remission could be addressed clinically with step-wise reevaluation and treatment adaptations such as those described by Reference Lambert, Martin and NaberLambert et al (2008b).
Figure 2 shows a simple care pathway using remission. For some patients who do not achieve remission, a change in their care plan will enable them to do so. From the evidence base it is certain that some patients would not achieve remission despite care plan changes. This lack of remission does not mean that they cannot recover (Reference Robinson, Woerner and McMenimanRobinson 2004), but the recovery might be better if they had achieved remission (Reference Emsley, Rabinowitz and MedoriEmsley 2007). Commissioners could ask whether it is more cost-effective to fund approaches that lead to sustained remission into wellness, or repeated high-intensity treatments for recurrent illness.
The usefulness of evaluating resolution and remission is summarised in Key points 2.
Limitations of the remission concept in schizophrenia
In their critique of the concept of remission, Reference Leucht, Beitinger and KisslingLeucht et al (2007) raised technical questions about measuring the time component in clinical trials. They also noted that the CGI–SCH severity score of ‘not more than mild’ appears to be as stringent a measure in researchers' hands as Andreasen's Consensus Group criteria.
Relapse
The issue of the time component is important in judging relapse, but this has not been operationalised for the PANSS. If someone in remission briefly rates 4 on a single PANSS item, is that enough to end the remission? If this were the case, the persistence of remission may be less likely the more often one checks for symptoms. Can remission be assumed to continue if it is not monitored for a year? Should remission only take into account symptoms on the day of assessment or should it also include patient and carer historical reports? A less stringent definition of relapse is that proposed for depression by Reference Frank, Prien and JarrettFrank et al (1991). They defined relapse as a return of symptoms satisfying the full syndrome criteria for an episode. For schizophrenia this requires a period with persistent multiple symptoms. More work needs to be done to clarify a definition of relapse in relation to remission in schizophrenia.
The views of service users, carers and psychiatrists
How do service users and carers view remission? In 2007, a survey sponsored by the pharmaceutical industry found that three-quarters of carers of people with schizophrenia thought that remission is a realistic treatment goal (European Federation of Associations of Families of People with Mental Illness 2007). Service users in another study (Reference Lasser, Bossie and GharabawiLasser 2005) felt that their health improved when they achieved remission. However, there has not been a study focusing on evaluating the usefulness of remission to service users. Some people may have a concern about the term remission, which is more familiar in connection with cancer treatment.
Critical psychiatrists may view remission as little more than another cog in a system of constructed false knowledge designed to sustain the power of professionals and the pharmaceutical industry (Reference MoncrieffMoncrieff 2007). However, remission judged on the basis of symptoms is quite capable of showing the ineffectiveness as well as the effectiveness of drugs and other interventions. Psychiatrists might be concerned about using a measure that can demonstrate poor outcomes if they believe that this would lead to disinvestment in existing services. However, an alternative view is that poor outcomes could demonstrate the need for services to be improved rather than removed.
It is possible that widespread use of remission could be stigmatising. If patients felt labelled as ‘non-remitters’, they might feel pessimistic about the future. Achieving remission could also be problematic for some service users dependent on social security programmes. Those who achieve remission could lose welfare benefits and without recovery-oriented approaches to establishing employment as the source of income, this may be sufficient reason for some service users to be wary of achieving remission.
Factors linked to remission
We have already considered the problem of non-concordance with treatment plans. If we attribute remission to a treatment that was not taken, we might make a systematic error that over-emphasises the value of treatments. This in turn may encourage over-zealous medical treatment when other approaches might be helpful. It is worth attempting some form of adherence monitoring alongside remission measurement. There are many aspects to symptom resolution and remission. Practitioners cannot assume that clinical improvement is linked only to treatment variables. It would be sensible to keep an open mind about the relative contribution of service user personal strengths, family support, occupational stress, physical illness, substance use and chance events. Clinicians also need to bear in mind that comorbid conditions such as depression can persist and prevent recovery even if schizophrenia remits.
Assessment of remission can be complemented by functional measures. Short scales such as the Global Assessment of Functioning (American Psychiatric Association 1987) and the Social Inclusion Scale (Reference Priebe, Watzke and HanssonPriebe 2008) are appropriate for this purpose. These scales record factors such as relationships, housing status and employment. Complemented in this way, remission can be part of a measure of recovery.
The main limitations of remission are summarised in Key points 3.
Recovery
Although remission is a valid goal of treatment, it is not always the final goal. This is usually considered to be recovery (Table 1). In some outcome schemes, such as the stages of depression described by Reference Frank, Prien and JarrettFrank et al (1991), recovery is described as the next stage after remission. Thus defined, recovery usually embodies long-term remission and a good functional outcome. Remission is a foundation for this kind of recovery. Reference Robinson, Woerner and McMenimanRobinson et al (2004) have given recovery in schizophrenia an operational definition using the Social Adjustment Scale (Reference Schooler, Hogarty, Weissman, Hargreaves, Attkisson and SorensonSchooler 1979). They found that 5 years after a first episode of schizophrenia or schizoaffective disorder, nearly half of patients had achieved remission for 2 years. Only 14% had also achieved sustained recovery. Another 12% had achieved recovery without full remission. Recovery as a standard is more difficult to achieve than remission.
However, recovery can be conceptualised not as a standard, but as a process of self-discovery and self-management. Recovery is then a journey that does not require symptom abatement as a starting point (Reference Roberts and WolfsonRoberts 2004; Reference Schrank and SladeSchrank 2007). This ‘rediscovery’ of recovery has been criticised by Reference OyebodeOyebode (2004) who cautions against using ‘ordinary words [such as recovery] to describe the world in ways totally opposed to the original meaning’. Reference SladeSlade (2009) has resolved this debate by defining two types of recovery. Clinical recovery is defined by practitioners in their professional terms, including symptom resolution and remission and the restoration of social function. Personal recovery is an individual process of changing values and meaning leading to a satisfying way of living with, or after, mental illness. Even if some forms of recovery do not need remission, people who make that journey may travel more easily with fewer symptoms.
UK health policy currently favours a recovery approach to illness and a personalised approach to healthcare. An English Green Paper with the title Independence, Well-being and Choice: Our Vision for the Future of Social Care for Adults in England presents a list of outcomes, the first of which is improved health (Department of Health, 2005: p. 10). In schizophrenia, the remission concept may be a useful way of monitoring improved health.
Using the generic modified PANSS
We have been using the Andreasen Consensus Group remission criteria in clinical practice for some time. We have been able to use the severity component alone (resolution) and in combination with the time component (remission). The generic modified PANSS can be administered in standard clinical settings in about 5 min. It is not an additional task since it measures mental state. A simple record sheet such as that shown in Fig. 3 can collect four ratings at different times. Using this, we can readily identify patients who have unremitted symptoms in any of the core domains of schizophrenia (positive and negative symptoms and disorganisation) and review care plans accordingly. For example, one patient had been reducing antipsychotic medication because of side-effects and began to show prominent negative symptoms. The dose of the antipsychotic was increased a little, which resulted in an improvement in negative symptoms without the return of side-effects.
We have used the ratings collaboratively with patients, sharing the results and discussing with them what to do. The ratings have also shown medical students that a consultation is more than an informal meeting; they demonstrate how symptoms are assessed in a structured manner. The ratings are a memory aid for clinicians, encouraging us to check the core symptom domains at each visit. Our teams have shown interest in measuring remission and this has facilitated discussions of care plans to improve outcomes.
All clinicians and health services have a duty to help patients get well and stay well. Resolution and remission give us a way to monitor these outcomes.
Remission in future
Remission is a promising measure for outcome research (Box 5) (Reference MortimerMortimer 2007). However, it is unclear whether the concept can be transferred into clinical practice, where routine outcome measurement is currently rare. In future, patients and their families should be able to choose services based on meaningful standard outcomes. Services able to demonstrate that they help more people get well and stay well for long periods (remission) should prove popular. Some services have already picked alternative approaches to outcome monitoring. Health professionals need to help decide which measures offer best value. It is unlikely that psychiatrists will be able to avoid all forms of outcome measurement in future. Health policies such as Independence, Well-being and Choice (Department of Health 2005) and Putting People First (HM Government 2007: p. 2) require measures of well-being and rapid recovery. The advantage that resolution and remission have compared with other measures is that they represent wellness as a simple, meaningful and evidence-based outcome in schizophrenia.
BOX 5 Potential benefits of remission
-
• It is a standardised outcome measure
-
• It can be applied swiftly in a clinic setting
-
• It could help to demonstrate good-quality care
-
• It could help demonstrate limitations of care
MCQs
-
1 Essential features of remission in schizophrenia as defined by Andreasen et al include:
-
a treatment adherence
-
b having a job
-
c not being an in-patient
-
d mild symptoms (or better) for 6 months or more
-
e no side-effects attributable to treatment.
-
-
2 Remission in schizophrenia is not associated with:
-
a better subjective health
-
b better insight
-
c better functioning
-
d reduced symptoms
-
e better physical health.
-
-
3 The remission concept would not be improved by:
-
a considering a definition of relapse
-
b finding out whether patients value remission
-
c trialling the remission standard in more clinical settings
-
d reluctance to measure clinical outcomes
-
e standardising monitoring intervals.
-
-
4 Remission is:
-
a a well-evidenced standard
-
b a continuous measure
-
c time-consuming to assess
-
d a measure of change
-
e adjustable to suit each patient.
-
-
5 Carers are likely to find the following clear and meaningful:
-
a collecting data that are never analysed
-
b trying to achieve a high standard of wellness for their relatives/friends
-
c reducing scores on complicated research rating scales
-
d not recording outcomes at all
-
e measures of activity relating to interservice transfers.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | f | a | f | a | f | a | t | a | f |
| b | f | b | f | b | f | b | f | b | t |
| c | f | c | f | c | f | c | f | c | f |
| d | t | d | f | d | t | d | f | d | f |
| e | f | e | t | e | f | e | f | e | f |
TABLE 1 Comparison of resolution, remission and recovery assessments in schizophrenia
| Recovery | ||||
|---|---|---|---|---|
| Resolution as a standard a | Remission as a standard a | As a standard b | As a process c | |
| Focus | Symptoms | Symptoms and time | Functional capacity | Person |
| Time to assess | Brief | Brief | Moderate | Lengthy |
| Involves patient | No | No | Somewhat | Yes |
| Well defined, measurable and comparable | Yes | Yes | Somewhat | Not yet |
KEY POINTS 1 Research findings on remission
|
KEY POINTS 2 Usefulness of resolution and remission to managers and commissioners
|
KEY POINTS 3 Limitations of remission assessment
|

FIG 1 Time in remission as a proportion of time since onset of schizophrenia.
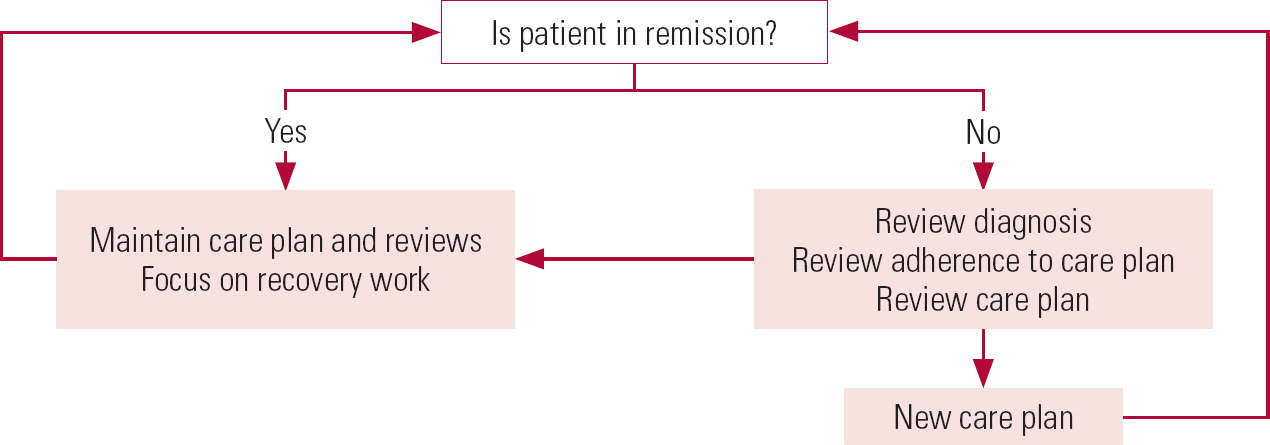
FIG 2 Clinical pathway using remission in schizophrenia.
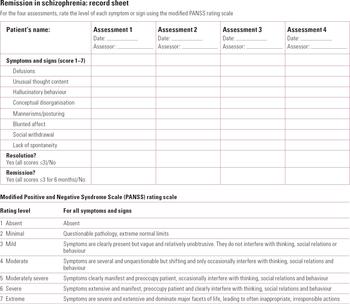
FIG 3 This record sheet uses Andreasen's Consensus Group standardised remission criteria (Reference Andreasen, Carpenter and KaneAndreasen 2005).
Acknowledgement
Thanks to Dr Angélica Santiago for her comments on a draft of this article.









eLetters
No eLetters have been published for this article.