Attachment theory was originally conceived by John Bowlby to explain an important evolutionary function of the child–caregiver relationship (Reference BowlbyBowlby, 1969). Gene survival was thought to be enhanced by the selection of favoured attachment behaviours that increased child–caregiver proximity, leading to the greater likelihood of protection for the child (Reference Cassidy, Cassidy and ShaverCassidy, 1999). Attachment theory has been supported by much empirical research in a variety of settings. However, although attachment theory began as a clinical enterprise, and has been usefully applied in the field of child mental health, its wider application to the everyday clinical understanding of adult mental health and mental health problems has lagged behind the available research. Attachment concepts currently do not form part of the familiar discourse for the general psychiatrist. I believe that attachment theory can afford valuable insight not only into the developmental nature of common psychiatric disorders, but also into the development of the therapeutic relationship.
My two articles give an overview rather than a systematic review of the topic and I have not touched on the interface between attachment theory and psychotherapy, on which there is a burgeoning literature. For an introduction to that field the reader is referred to Reference Fonagy, Cassidy and ShaverFonagy (1999) and Reference HolmesHolmes (2001). For an introduction to the application of attachment theory to forensic psychiatry, see Reference Pfäfflin and AdsheadPfäfflin & Adshead (2004). I have also not considered the implications of parental mental ill health for a child’s attachment, as this broad topic would require an article to itself.
Conceptualisation of attachment in adulthood
In Bowlby’s view, to say that a child is ‘attached’ to someone means that he (or she) is ‘strongly disposed to seek proximity to and contact with a specific figure and to do so in certain situations, notably when he is frightened, tired or ill’ (Reference BowlbyBowlby, 1969: p. 371). In normal circumstances, the first attachment relationship will be the bond formed by the infant to her primary caregiver. By providing a ‘secure base’, the caregiver enables the growing child to explore the outside world; thus, early attachments have a significant effect on the child’s socio-emotional and cognitive development.
Attachment is now thought to be active throughout the human life span, as important relationships between individuals (e.g. that between romantic partners) may take on the quality of attachment relationships (Reference Ainsworth, Parkes, Stevenson-Hinde and MarrisAinsworth, 1991). However, behaviours that maintain attachments to significant others will change as the individual passes through different life stages. Physical proximity to the attachment figure(s) is important in early childhood. As the child grows, the availability and trustworthiness of her attachment figures become internalised psychologically as a sense of attachment security. Based on the responsiveness of early caregivers, ‘internal working models’ or cognitive-emotional representations of the self and significant others evolve, such that an individual may regard herself as deserving/undeserving of attachment, and regard others as more or less able to meet her attachment needs. Internal working models are important for understanding how psychopathology may develop (Reference Bretherton, Munholland, Cassidy and ShaverBretherton & Munholland, 1999).
Attachment relationships in adulthood provide feelings of security and belonging (Reference Crowell, Fraley, Shaver, Cassidy and ShaverCrowell et al, 1999). The measurement of attachment in adulthood, which depends more fundamentally on how adult attachment is conceptualised, has generated a sizeable literature in its own right (Reference Crowell, Fraley, Shaver, Cassidy and ShaverCrowell et al, 1999), which I can only touch on here. According to Reference Bartholomew, Shaver, Simpson and RholesBartholomew & Shaver (1998), one can broadly discern two strands, which I have labelled the ‘parenting’ and the ‘romantic attachment’ traditions (Table 1). The two traditions derive from different disciplinary subcultures. This distinction is important, as how attachment is conceptualised and measured will influence the findings of research into attachment and adult psychopathology.
Table 1 A comparison of the parenting and romantic attachment traditions of attachment research
| The parenting tradition | The romantic tradition | |
|---|---|---|
| Orientation | Psychodynamic; focus on clinical problems | Social/personality psychology |
| Preferred method of attachment assessment | Interviews and behavioural measures in small groups of participants | Simpler questionnaires (including self-rated ones) in larger populations, but also interview measures |
| Focus | Caregiver–child relationships; attachment ‘state of mind’ | Social/romantic relationships (friendships, dating relationships, marriages) |
| Age groups | Across the life span | Initially in young adults, now extending to other age groups |
The parenting tradition
The parenting tradition originated from research into how adult attachment might influence parenting behaviour and the attachment patterns of parents’ young children (Reference Bartholomew, Shaver, Simpson and RholesBartholomew & Shaver, 1998). The most researched measure here is the Adult Attachment Interview (Adult Attachment Interview; Reference Main and GoldwynMain & Goldwyn, 1998), which measures the adult’s state of mind with respect to attachment, i.e. their current representations of their childhood relationships with their parents. The instrument is a semi-structured interview about early attachment history, with questions designed to ‘surprise the unconscious’ and hence yield clues as to the predominant underlying attachment strategies of an individual that influence current attachment relationships. Interviewees are asked about past attachment experiences and their current influence, and to give specific examples to support their statements. The interview yields both categorical and continuous data. In the Main & Goldwyn scoring system, the rating procedure is as dependent on how interviewees answer the questions (the discourse style) as on what they actually say (the content) (Reference Hesse, Cassidy and ShaverHesse, 1999). Interviewees are put into one of four broad adult attachment categories, which are analogous to the infant categories produced in Ainsworth’s Strange Situation procedure (Reference Ainsworth, Blehar and WatersAinsworth et al, 1978) (Table 2). Indeed, the Adult Attachment Interview draws its validity from the high correspondence between the attachment classification of parents and their infants’ classifications in the Strange Situation (Reference van IJzendoornvan IJzendoorn, 1995). Thus, ‘secure’, ‘ambivalent’, ‘avoidant’ and ‘disorganised’ infants tended to have primary caregivers who were respectively ‘autonomous’, ‘preoccupied’, ‘dismissing’ and ‘unresolved’ with respect to attachment. Many of the leading researchers in the parenting attachment research tradition were students of Mary Ainsworth.
Table 2 Summary of attachment categories1
| Infant attachment category | Observations of infant in the Strange Situation 2 | Corresponding adult attachment category | Discourse style on the Adult Attachment Interview |
|---|---|---|---|
| Avoidant (A) | Little protest on separation. On caregiver’s return, hovers warily nearby, cannot play freely | Dismissing (Ds) | Brief discourse, which normally idealises parents, with few supporting examples |
| Secure (B) | Protests when caregiver disappears. Protest continues on return, but soon pacified and continues exploratory play | Secure/autonomous (F) | Narrative coherence. Valuing of attachment, but seems objective regarding particular events and relationships. Able to give examples to support statements |
| Ambivalent/resistant (C) | Protests, and hard to pacify on caregiver’s return, clings to carer, buries head in lap, pushes away toys offered | Preoccupied (E) | Incoherent, vague and excessively long discourse. Preoccupied with past attachment experiences. Speaker appears angry, passive or fearful |
| Disorganised/disoriented (D) | ‘Freezes’ on separation, seems unable to sustain any organised pattern of behaviour on reunion. Behaviours may appear bizarre and stereotyped | Unresolved/disorganised (U)3 | Striking lapses in monitoring of reasoning during discussion of loss or abuse |
In infants, the avoidant and ambivalent patterns are said to be organised, as even these ‘insecure’ patterns may be adaptive in maximising care from broadly rejecting and inconsistent caregivers respectively. Disorganised attachment, however, may represent a more fundamental breakdown in attachment strategy. Unresolved loss and trauma in the caregiver predicts infant attachment disorganisation. When discussing past traumas or losses on the Adult Attachment Interview, such a caregiver will show striking lapses of ‘meta-cognitive reasoning’ and possible dissociation; she will accordingly receive an unresolved/disorganised classification. Disorganisation of infant attachment, more than ‘organised’ insecure attachment patterns (i.e. avoidant or ambivalent), is predictive of both externalising and internalising problems in childhood (Reference Lyons-Ruth, Jacobvitz, Cassidy and ShaverLyons-Ruth & Jacobvitz, 1999; Reference Green and GoldwynGreen & Goldwyn, 2002). Similarly, the unresolved attachment category in adults may be especially associated with psychopathology.
The romantic attachment tradition
In the past two decades, an independent line of attachment measurement has originated from research into romantic relationships (Reference Bartholomew, Shaver, Simpson and RholesBartholomew & Shaver, 1998). This was based on the premises that romantic love could be conceptualised as an attachment process (Reference Hazan and ShaverHazan & Shaver, 1987) and that how one views and approaches romantic relationships might be an outgrowth of previous attachment experiences. Many in the romantic attachment tradition have been personality or social psychologists (Table 1). This strand of attachment research, which focused as a starting point on adulthood, is characterised by the use of self-report measures of attachment, although narrative interview can also be used.
Attachment measures
The Adult Attachment Interview and self-report questionnaires
To score the Adult Attachment Interview requires an extensive training that is not easily available to the average clinician. Self-report attachment measures, on the other hand, are more easily scored and analysed, which makes them easier to use in larger-scale research. They may also be useful in the clinical setting, whereas the Adult Attachment Interview, because of its complexity, has remained primarily a research tool.
The use of self-report questionnaires has been challenged on the basis of their (theoretically) limited ability to tap into unconscious attachment strategies and their vulnerability to defensive reporting. The Adult Attachment Interview, by its design, would not suffer from these deficiencies. However, in support of self-report measures, it can be counter-argued that adults are able to provide valuable information about their emotional experiences, that most adults have sufficient experience in close relationships to recount how they behave in them, and that conscious and unconscious processes normally operate together to achieve a goal. The construct validity of self-report measures of romantic attachment derives from their prediction of three domains: differential behaviours within relationships consistent with attachment theory (e.g. the use of a partner as a secure base); the differing attributions made by secure and insecure individuals within relational conflicts; and general adjustment and, as we shall see, psychopathology (Reference Crowell, Fraley, Shaver, Cassidy and ShaverCrowell et al, 1999). At the same time, self-report measures of romantic attachment show only moderate correlation with measures of personality and relationship satisfaction, suggesting sufficient discriminant validity (Reference Crowell, Fraley, Shaver, Cassidy and ShaverCrowell et al, 1999).
Bartholomew’s four-category model
One particular model in the romantic tradition that has been well validated and used in research into adult psychopathology is Bartholomew’s four-category model of attachment (Reference Bartholomew and HorowitzBartholomew & Horowitz, 1991). Figure 1 shows that this model is in fact conceptualised as different combinations of the internal working models of the self and of others, yielding the four attachment ‘prototypes’, or styles, of ‘secure’, ‘dismissing’, ‘preoccupied’ and ‘fearful’. These four attachment styles can be assessed using both interview methods and self-report questionnaires such as the Relationship Questionnaire (Reference Bartholomew and HorowitzBartholomew & Horowitz, 1991) and the Relationship Scales Questionnaire (Box 1) (Reference Griffin, Bartholomew, Bartholomew and PerlmanGriffin & Bartholomew, 1994).
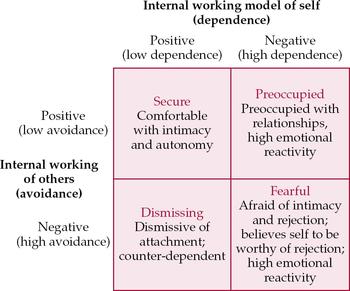
Fig. 1 Bartholomew’s four-category model of adult attachment (after Reference Bartholomew and HorowitzBartholomew & Horowitz, 1991).
Box 1 The Relationship Scales Questionnaire
-
• Contains 30 descriptive items about close relationships
-
• Interviewees score each item on a scale of 1–5 to show their degree of agreement
-
• Examples of these items include: ‘I find it difficult to depend on other people’, ‘I’m not sure that I can always depend on others to be there when I need them’, ‘I worry that others don’t value me as much as I value them’ and ‘I often worry that romantic partners won’t want to stay with me’
Many other self-report measures, devised by different research groups, now exist. A factor analysis of self-report measures (Reference Brennan, Clark, Shaver, Simpson and RholesBrennan et al, 1998) identified a latent two-factor structure underlying them. The two factors, attachment anxiety (i.e. anxiety over abandonment within attachment relationships) and attachment avoidance (avoidance of attachment relationships), are postulated to be affective–behavioural manifestations of the internal working models of the self and of others respectively.
There is doubt as to how far interview and self-report measures converge (Reference Crowell, Fraley, Shaver, Cassidy and ShaverCrowell et al, 1999). Nevertheless, Reference Bartholomew, Shaver, Simpson and RholesBartholomew & Shaver (1998) argue that common ground does exist. They believe that there is some convergence among the secure, dismissing and preoccupied categories in the Main & Goldwyn (Table 2) and Bartholomew classifications (Fig. 1). The fearful prototype, which may be especially relevant to adult psychopathology, is unique to the Bartholomew system, which does not contain attachment disorganisation. It would be tempting to equate fearful attachment with attachment disorganisation, and some researchers have in fact done so. However, this practice has been challenged by, among others, Reference West and GeorgeWest & George (2002).
Attachment and psychopathology in adults
In explaining the putative link between attachment insecurity and psychopathology, Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al(1999) speak about the importance of insecure internal working models, or ‘strategies for processing attachment-related thoughts and feelings that compromise realistic appraisals’ (p. 497).
The issue here is that attachment strategies adaptive in early childhood (which might be the case even in avoidant and ambivalent attachment) will not necessarily be adaptive in later life. Furthermore, the ways in which insecurely attached individuals function in relationships may lead others to reinforce their internal working models. This may lead to a reduction in the social support available to them and also in the use they make of this reduced support. Problems within attachment relationships may in themselves be pathogenic. Attachment insecurity may thus be one risk factor for psychopathology (Reference Greenberg, Cassidy and ShaverGreenberg, 1999; Reference GoodwinGoodwin, 2003). Conversely, attachment security may be protective.
Several general points may be made. First, the majority of studies that have examined the association between attachment and psychiatric disorders have been cross-sectional, rendering the direction of causality impossible to determine. The longitudinal data available so far suggest that attachment insecurity does indeed serve as a risk factor. Second, owing to differences in attachment conceptualisation and measurement on the one hand and in how psychiatric disorders are diagnosed on the other (Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al, 1999), results across studies cannot be readily compared. This might explain in part some of the contradictory findings. Nevertheless, one broad generalisation has been put forward on the basis of the distinction between attachment strategies that ‘maximise’ and ‘minimise’ attachment needs and behaviours (approximately corresponding to attachment preoccupation and dismissal respectively) (Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al, 1999). Externalising psychopathology (which might involve acting-out behaviours, e.g. eating disorders) is hypothesised to be associated with minimising (or deactivating) strategies, whereas internalising psychopathology (such as depression, anxiety and borderline personality disorder) would be associated with maximising (or hyperactivating) strategies. As shown below, this generalisation has not been consistently supported. Finally, one might expect that the higher the genetic loading for a disorder, the less contribution social and/or environmental factors (including attachment) might make.
What does all this have to do with clinical psychiatry?
One might wonder about the clinical significance of any association between attachment insecurity and particular forms of psychopathology in general adult psychiatry. I would propose the following arguments.
An understanding of associated attachment patterns or styles might enable a better understanding of the aetiology of psychiatric disorders, especially from an interpersonal perspective. In this context, psychopathology might develop from the frustration or maladaptive expression of attachment needs, in circumstances where the attachment system is activated (e.g. divorce, bereavement). Attachment theory may provide an aetiological perspective not readily derivable from other theories.
Given that the attachment system is likely to be activated during a psychiatric disorder, the clinician may come to be seen as a temporary attachment figure (Reference AdsheadAdshead, 1998). Different attachment strategies may then differentially influence the patient–doctor relationship. I will discuss this area in the second of my two articles (Reference MaMa, 2007).
A corollary is that, through influencing the patient–doctor relationship, attachment patterns or styles may influence the outcome of illness management and healthcare utilisation.
Depressive disorder
Attachment theory may be highly relevant in the understanding of the aetiology of depression, as Reference BowlbyBowlby (1980) himself discussed. The experiences of early loss, separation and rejection by the parent or caregiver (conveying the message that the child is unlovable) may all lead to insecure internal working models (Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al, 1999). Internal cognitive representations of the self as unlovable and of attachment figures as unloving/untrustworthy would be consistent with parts of Beck’s cognitive triad in depression (Reference Beck, Rush and ShawBeck et al, 1979).
Empirically, the association between attachment and depression has been assessed cross-sectionally using both the Adult Attachment Interview and self-report instruments, affording different facets of aetiological understanding. Studies using the Adult Attachment Interview, which have examined both adults and adolescents, have yielded inconsistent results (Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al, 1999). However, small sample sizes and different diagnostic, inclusion and exclusion criteria have probably contributed to the contradictory findings. For example, the study by Reference Cole-Detke and KobakCole-Detke & Kobak (1996) looked at depressive symptoms rather than disorder, and found that college women who reported depressive symptoms were more often hyperactivating in their attachment strategies than were controls with no eating disorder/depressive symptoms or a sample with only symptoms of eating disorder. This study used Kobak’s Q-set method of scoring (further details available on request) rather than the Main & Goldwin (1998) system. The two systems do not give directly comparable results; disorganisation is not measured by the Q-set method, thus affecting the interpretation of results.
The comparatively large and much quoted study by Reference Fonagy, Leigh and SteeleFonagy et al(1996) did operationalise diagnoses according to the DSM–III–R (American Psychiatric Association, 1987). They assessed the relation between attachment and psychopathology using the Adult Attachment Interview in 82 non-psychotic psychiatric in-patients and 85 case-matched non-psychiatric controls. More than 80% of both groups were women. Applying the Main & Goldwyn scoring system, the authors analysed results using the three-way and four-way classificatory systems for the Adult Attachment Interview (excluding and including unresolved attachment respectively). Unfortunately, all affective disorders (including major depressive disorder, bipolar disorder and dysthymia) were analysed together, and comorbidity was significant among the psychiatric patients. The findings were therefore hard to interpret. They did identify a large proportion of patients who were in the ‘unresolved/disorganised’ U category on the Adult Attachment Interview (Table 2); this result could be attributed to the sample, which comprised in-patients referred to a national centre for the treatment of personality disorder (see below).
Studies using Bartholomew’s classification (Fig. 1) and self-report attachment measures have produced more consistent results. In non-clinical populations, where research has benefited from larger samples, depressive symptoms are positively associated with both self-reported preoccupied and fearful attachment, and negatively associated with secure attachment. Depressive disorder in clinical populations tends to be more associated with fearful attachment (e.g. Reference Carnelley, Pietromonaco and JaffeCarnelley et al, 1994; Reference Reis and GrenyerReis & Grenyer, 2004). In a study of 71 individuals with DSM–IV major depression, Reference Reis and GrenyerReis & Grenyer (2004) found an association between fearful attachment and depression severity, at least for the women. They note that whereas a negative internal working model of the self (seen in both preoccupied and fearful attachment) may be associated with milder, subclinical depressive symptoms, ‘the experience of major depression may be more intense or severe if others are simultaneously viewed as hostile, uncaring or rejecting’, as would be the case in fearful attachment.
Causality
To begin to determine whether a causal association exists between self-reported attachment style and depressive disorder, Reference Haaga, Yarmus and HubbardHaaga et al(2002) compared 50 people who all scored < 9 on the Beck Depression Inventory; 25 of them had recovered from at least one previous episode of major depression and 25 had never had depression. The ‘recovered depressed’ group scored significantly higher on Bartholomew’s fearful and preoccupied attachment styles, and significantly lower on the secure style. The findings suggest that these insecure attachment styles may be a stable vulnerability factor for depression, not a mood-dependent artefact. Similarly, Reference Cyranowski, Bookwala and FeskeCyranowski et al(2002), in their study of maintenance interpersonal psychotherapy for depression, found that over 40% of their sample of 162 women had a fearful attachment style at remission of acute symptoms. However, one cannot deduce the direction of any causal relationship between attachment insecurity and depression on the basis of these findings. It is possible that depressive disorder may have led to attachment insecurity in these cases (so-called scarring). However, Reference Haaga, Yarmus and HubbardHaaga et al(2002) identified no correlation between the number of previous depressive episodes and preoccupied or fearful attachment to support the scarring hypothesis. Larger prospective studies are now needed to delineate the relationship between depressive disorder and self-report attachment styles, paying particular attention to gender differences which have been suggested in some previous research (Reference Reis and GrenyerReis & Grenyer, 2004).
Research should also question whether any causal relationship between attachment style and depressive disorder is mediated by the influence of internal working models on cognitive schemas. Preliminary research looking at depressive and anxiety symptoms partially supports such an influence (Reference Williams and RiskingWilliams & Risking, 2004). Reference Rogers, Reinecke and SetzerRogers et al(2004) found a strong association between attachment experience and cognitive vulnerability in adults with clinical depression; this association was independent of mood state and social desirability. One clinical implication of these findings might be the differential response to cognitive–behavioural therapy of patients with different attachment styles. Specifically, compared with those who are insecurely attached, securely attached patients might have greater ease in identifying and modifying their maladaptive cognitions and assumptions. This hypothesis requires empirical verification.
Anxiety
Anxiety disorders are heterogeneous in nature, characterised by a combination of fear and avoidance. Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al(1999) suggest that when fear predominates, the disorder involves primarily internalising symptoms, and will be expected to be associated with maximising attachment strategies (e.g. ambivalent/preoccupied attachment). Reference BowlbyBowlby (1973) proposed that anxiety disorders are best accounted for by anxiety regarding the availability of attachment figures, and delineated early family environments that might predispose to their development. These include environments in which the child worries about the parent’s safety in the child’s absence, or worries about parental rejection. An insecurely attached child may thus frequently become anxious, even in benign circumstances. Chronic vigilance and anxiety will then increase the probability of a future anxiety disorder (Reference Warren, Huston and EgelandWarren et al, 1997).
Given the theoretical links between attachment insecurity and anxiety disorders, there has been surprisingly little empirical research examining the association (Reference GoodwinGoodwin, 2003). However, Reference Warren, Huston and EgelandWarren et al(1997) conducted one of the few studies on attachment and psychopathology that benefits from a longitudinal design. They recruited 267 mother–baby dyads and assessed each infant’s attachment using the Strange Situation procedure. Current and past anxiety disorders were assessed in 172 of these children when they reached 17.5 years. Twenty-six (15%) had at least one past or current anxiety disorder, including separation anxiety and social phobia; 51% had a disorder other than anxiety disorder. Results showed the contribution of anxious/ambivalent attachment to anxiety disorders, which conferred a twofold increase in risk. However, the study did not consider attachment disorganisation as a risk factor, nor did it attempt to assess the adolescents’ attachment style at follow-up.
In the aforementioned study by Reference Fonagy, Leigh and SteeleFonagy et al(1996), 66% of the patients with anxiety disorder were classified as preoccupied (E) in the three-way Adult Attachment Interview classification. When unresolved/disorganised attachment (U) was taken into account, there was a significant association between the U category and anxiety disorders, with 86% of individuals receiving this attachment classification.
Neither of the above studies examined specific anxiety diagnoses. More recently, Reference Myhr, Sookman and PinardMyhr et al(2004) compared three groups (individuals with obsessive–compulsive disorder (OCD), with depression and with no psychiatric disorder) on a self-report measure of attachment, the Revised Adult Attachment Scale (Reference Collins and ReadCollins & Read, 1990), which differs from the Bartholomew measures. Both the OCD and the depression group scored significantly higher on the anxiety sub-scale of this attachment measure, which suggests an insecure self-model. Interestingly, the OCD group did not differ from the control group on recollection of parental bonding; the depression group, however, had more negative recollections. Parental bonding has been used by some researchers as a proxy measure of early attachment; such practice is of questionable validity (Reference Manassis, Owens and AdamManassis et al, 1999).
Stress-related disorders
Research has begun to address the relationship between post-traumatic stress symptoms and attachment. It is hypothesised that attachment insecurity would compromise an individual’s ability to cope with traumatic life events and would therefore predispose to the formation of post-traumatic stress symptoms and/or disorder. However, longitudinal data to test this hypothesis are lacking. In one Canadian sample of 66 individuals who self-reported childhood abuse, the Relationship Scales Questionnaire was administered along with a measure of post-traumatic stress symptoms (Reference Muller, Sicoli and LemieuxMuller et al, 2000). Only 24% of the sample were classified as having a secure attachment style. Those with preoccupied or fearful attachment reported the highest level of post-traumatic stress symptoms, and multiple regression analyses demonstrated the predictive power of a negative self-model, but not of a negative other-model. Theoretically, individuals with a negative internal working model of the self may use affect rather than cognition to guide their behaviour; faced with traumatic events, they may have difficulty in regulating ’raw’ emotions. The study by Muller et al did not test this point empirically. It was also a small study that was cross-sectional in design and was prone to recruitment bias, as volunteers had responded to flyers in the community. More recently, in a sample of 284 adults, attachment and dissociation were shown to mediate the relationship between childhood abuse and post-traumatic stress disorder following the terrorist attacks on New York’s World Trade Centre (Reference Twaite and RodriguezTwaite & Rodriguez, 2004).
Personality disorders
Attachment theory may provide significant insight into the developmental origins of personality disorders. Personality refers to enduring patterns of thought, motivation, emotional and impulse regulation, and interpersonal functioning. Attachment is related to these domains, albeit in the more specific context of personal relationships. Both personality disorders and attachment insecurity are associated with early adversity (Reference Meyer, Pilknos and ProlettiMeyer et al, 2001; Reference Nakash-Eisikovits, Dutra and WestenNakash-Eisikovits et al, 2002). With specific regard to borderline personality disorder (the personality disorder in which attachment has been most researched), Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al(1999) note that:
‘Borderline pathology is generally associated with the exaggeration of symptomatology and of negative affect …The readiness to report distress is consistent with … [preoccupation] with regard to attachment’ (p. 511).
Two large-scale studies have been conducted which show overlap between different personality disorders and attachment dimensions. In the first, Reference Brennan and ShaverBrennan & Shaver (1998) found in a non-clinical sample of 1407 undergraduates an association between attachment insecurity and self-reported personality disorders; of the 13 disorders studied, only psychopathy was unrelated to attachment insecurity. The study by Reference Fossati, Feeney and DonatiFossati et al(2003) assessed 487 psychiatric in-patients with a range of diagnoses. Through canonical correlation analysis, the data suggested that attachment avoidance might be associated with avoidant, depressive, paranoid and schizotypal personality disorders. Attachment anxiety might be associated with dependent, histrionic and borderline personality disorders. Similar but not identical results had been found in an earlier study of adolescent personality pathology (Reference Nakash-Eisikovits, Dutra and WestenNakash-Eisikovits et al, 2002).
Returning to Reference Fonagy, Leigh and SteeleFonagy et al(1996), the authors found that 75% of their patients diagnosed with DSM–III–R borderline personality disorder (27 out of 36) were classified as preoccupied on the Adult Attachment Interview, when the three-way classification (excluding U) was used (Table 2). Furthermore, a significant proportion received the sub-classification E3, which indicates ‘fearful preoccupation with traumatic events’. When the four-way classification (including category U) was used, nearly 90% (32 out of 36) of the sample with borderline personality disorder received an unresolved/disorganised U classification. The limitations of the study have been mentioned above.
In an Italian study of 40 patients with borderline personality disorder on a psychotherapy waiting list, Reference BaroneBarone (2003) found that 20 patients in her clinical sample (50%) were classified as unresolved/disorganised, compared with 3 out of 40 healthy controls (7%). Through sub-analysis of the Adult Attachment Interview sub-scales, she identified an ‘actively rejecting’ father and a ‘neglecting, poor-loving’ mother as especially relevant to the understanding of borderline personality disorder, and construed the personality disorder as a combination of maximising attachment strategies in the face of unresolved traumata.
Developmentally, unresolved loss or trauma in the parent predicts attachment disorganisation in the infant. Follow-up studies have shown that disorganised infants show ‘controllingness’ at 6–7 years of age, with both mothers and peers. Through role-reversal with their caregivers, these children may be providing a ’pseudo-secure base’ for themselves. At the same time, controlling children, often with helpless parents, are often unable to resolve frightening scenarios on picture completion tests. Reference HolmesHolmes (2004) hypothesises that:
‘[in] adolescence and adulthood … the individual is controlling, aggressive, unable to self-soothe when faced with emotional turmoil and loss, liable to dissociation, and cannot extricate herself from pain-producing relationships’ (p. 183).
This attachment-informed developmental model of borderline personality disorder needs to be tested with much more (longitudinal) research, and has important implications for psychotherapeutic treatment (Reference HolmesHolmes, 2004).
Eating disorders
Many explanations have been proposed for the aetiology of eating disorders, some of which have emphasised the importance of family factors. From an attachment point of view, eating disorders are theorised to be associated with deactivating strategies that minimise attachment needs. Eating disorders may be associated with a lack of attention to or inability to discriminate one’s inner distress cues, along with a focus on dieting and body appearance that may provide a diversion from such cues (Reference Cole-Detke and KobakCole-Detke & Kobak, 1996; Reference Dozier, Stovall, Albus, Cassidy and ShaverDozier et al, 1999). It has also been postulated that the symptoms of eating disorders maintain proximity to the attachment figure, albeit in a maladaptive way (Reference Orzolek-KronnerOrzolek-Kronner, 2002).
Empirical results to date have not consistently supported theory, which may again be a function of the differences across studies in the attachment measures/scoring systems, diagnostic criteria and samples used. The cross-sectional design of the key research on the topic needs to be borne in mind. As noted above, the study by Reference Cole-Detke and KobakCole-Detke & Kobak (1996) used the Adult Attachment Interview, but with the Q-set method of scoring, rather than the Main & Goldwyn system. The authors showed eating disorder symptoms (as opposed to the clinical syndromes) to be associated with attachment deactivation (dismissal) in a sample of college women, when depressive symptoms had been controlled for. On the other hand, Reference Fonagy, Leigh and SteeleFonagy et al(1996) found that 9 out of the 14 people (64%) with an eating disorder in their sample were preoccupied in their attachment in the three-way Main & Goldwyn classification; 13 out of the 14 (93%) showed attachment disorganisation in the four-way classification. No distinction was made between the different eating disorders.
In a clinical sample of 19 women (aged 15–46 years) with anorexia nervosa assessed using DSM–IV criteria and the Adult Attachment Interview, 15 were dismissing in their attachment (Reference Ward, Ramsay and TurnbullWard et al, 2001). Interestingly, although there was no association between the patients’ attachment patterns and those of their mothers, there was a high incidence of unresolved status in the latter group. The authors postulate that difficulty in emotional processing in these parents may have been transmitted to their daughters, serving as a risk factor for the development of anorexia nervosa.
Some research has examined the correlation between eating disorders and self-reported attachment. Using Bartholomew’s classification, Reference Broberg, Hjalmers and NevonenBroberg et al(2001) in Sweden compared a large sample of female out-patients who had eating disorders with a control group. Those with eating disorders were more insecure in their attachment. The authors further noted that the severity mattered more than the type of eating disorder in predicting the association between eating disorder symptomatology and self-rated attachment.
Conclusions
Attachment is a clinically relevant concept in adulthood. It can be measured in a number of ways, some of which are discussed in this article. Attachment theory may afford valuable insight into the developmental trajectories of at least some common psychiatric disorders. Although most research has focused on depressive disorder, the aetiology of anxiety, eating and personality disorders may also benefit from being examined through the lens of attachment theory. My second article (Reference MaMa, 2007) will look at some of the applications of attachment theory in the everyday clinical setting.
Declaration of interest
None.
MCQs
-
1 With respect to the assessment of attachment:
-
a Ainsworth devised the Relationship Scales Questionnaire
-
b the Relationship Scales Questionnaire was devised originally to assess the attachment of psychiatric patients
-
c interview measures may be better than self-report measures in tapping into unconscious attachment strategies
-
d the Adult Attachment Interview requires little training to administer and to score
-
e self-report measures should not be used because of their uncertain validity.
-
-
2 Research on the association between attachment and psychopathology:
-
a has tended to be cross-sectional in nature
-
b has found an association between borderline personality disorder and unresolved attachment
-
c has uniformly used large samples
-
d has focused mainly on psychotic disorders
-
e has been carried out mainly using the Adult Attachment Interview.
-
-
3 Unresolved attachment:
-
a may be seen in individuals whose underlying attachment is secure/autonomous
-
b is equivalent to fearful attachment in the Bartholomew classification
-
c may be especially relevant to the understanding of psychopathology
-
d is evident purely from the content of discourse on the Adult Attachment Interview
-
e is seen only in women who were sexually abused in childhood.
-
MCQ answers
| 1 | 2 | 3 | |||
|---|---|---|---|---|---|
| a | F | a | T | a | T |
| b | F | b | T | b | F |
| c | T | c | F | c | T |
| d | F | d | F | d | F |
| e | F | e | F | e | F |





eLetters
No eLetters have been published for this article.