Significant outcomes
-
1. There are some differences in the sociodemographic features of unipolar mania and bipolar disorder.
-
2. IL-6 and CRP levels were higher in the unipolar mania group.
-
3. There was no difference between unipolar mania and bipolar disorder in terms of serum BDNF, IL-1β, TNF-α or leucocyte levels.
Limitations
-
1. The diagnosis of unipolar mania may be inaccurate due to the inability to remember past depressive episodes or predict possible future depressive episodes.
-
2. Age, gender, smoking, alcohol use and various antipsychotic treatments may have affected cytokine, C-reactive protein, leucocyte and BDNF levels.
-
3. The presence of some chronic medical diseases and the drugs may have affected the levels of cytokines and BDNF in some patients.
Introduction
Unipolar mania is a bipolar disorder with recurrent manic and hypomanic episodes and without depressive episodes. Although earlier studies of unipolar mania indicated the minimum required number of manic episodes for diagnosis as one or two, more recent studies have shown that this number has increased to three or four episodes (Yazıcı, Reference Yazıcı2014). Yazıcı et al. (Reference Yazici, Kora, Üçok, Saylan, Özdemir, Kiziltan and Özpulat2002) reported that the absence of depressive or mixed episodes, at least 3–4 manic episodes, and at least 4 years of disease follow-up were accepted as decisive criteria for the diagnosis of unipolar mania.
Since most studies on unipolar mania have been conducted in non-Western countries, it appears as if it is more common in these countries. However, it was emphasised that this situation cannot be accepted with certainty due to the lack of intercultural studies (Mehta, Reference Mehta2014). In the first large-scale study conducted on the epidemiology and course of unipolar mania, the frequency of unipolar mania in patients with classical bipolar disorder ranged between 5 and 7.2%, and approximately 18% of unipolar mania patients had depressive episodes during the 3-year follow-up period (Baek et al., Reference Baek, Eisner and Nierenberg2014).
Studies have shown that unipolar mania differs from bipolar disorder in terms of sociodemographic characteristics, clinical characteristics and treatment response (Angst & Grobler, Reference Angst and Grobler2015). In a study including nine epidemiological studies, although men were more predominant in the unipolar mania group compared to the bipolar disorder group, no difference was found between the two groups in terms of age at the onset of the first episode. In the unipolar mania group, the number of patients who attempted suicide or who had comorbid generalised anxiety disorder, panic disorder, eating disorder and substance use disorders was found to be lower (Angst et al., Reference Angst, Rössler, Ajdacic-Gross, Angst, Wittchen, Lieb, Beesdo-Baum, Asselmann, Merikangas and Cui2019). Mehta (Reference Mehta2014), in a meta-analysis study, observed more psychotic symptoms, grandiosity, history of cannabis and amphetamine use and hyperthymic temperament in unipolar mania patients than in bipolar disorder patients; however suicide history and loss of social, familial and occupational functionality were experienced less in unipolar mania patients.
The differences between bipolar disorder and unipolar mania patients have been examined in the literature; the results are conflicting, and there are not enough studies on this subject. Moreover, until now, there have been no studies on neuroplasticity and inflammation in patients with unipolar mania. However, it has been suggested that impaired neuroplasticity and inflammation may play an important role in the etiopathogenesis of bipolar disorder (Post, Reference Post2007; Kalelioğlu et al., Reference Kalelioğlu, Genç and Karamustafalıoğlu2017). Brain-derived neurotrophic factor (BDNF) is one of the most common and studied neurotrophin in the brain, and it has been found to be significantly decreased in patients with bipolar disorder (Scola & Andreazza, Reference Scola and Andreazza2015). Cytokines that play an active role in the inflammatory response and can be measured in systemic circulation are polypeptide molecules that play a key role in inflammation (Kalelioğlu et al., Reference Kalelioğlu, Genç and Karamustafalıoğlu2017). Previous findings suggest that cytokines and BDNF may reflect the key pathophysiological mechanisms, disease activity and progression of bipolar disorder (Jacoby et al., Reference Jacoby, Munkholm, Vinberg, Pedersen and Kessing2016).
Aims of the study
The main purpose of this study is to compare sociodemographic and clinical features, serum BDNF, C-reactive protein (CRP), leucocyte and cytokine levels in patients with unipolar mania and bipolar disorder.
Material and methods
The data of 495 patients who were hospitalised between 01 January 2005 and 02 January 2018 in the Department of Psychiatry of Trakya University Hospital with the diagnosis of bipolar disorder were retrospectively analysed. The hospital data showed that 40 patients met the diagnostic criteria for unipolar mania. These 40 patients were asked to participate in the study, and 38 agreed to participate. The diagnosis was reconsidered by psychiatric examination. Patients between the ages of 18 and 65 years who had no depressive episodes in the past, were followed up for at least 4 years, had at least four manic episodes and were still in the euthymic period were defined as the unipolar mania group. The bipolar disorder patient group consisted of 42 patients who agreed to be included in the study and met the inclusion criteria; these patients were randomly selected from among the patients who visited the outpatient clinic during the study period. The bipolar disorder patient group consisted of patients aged 18–65 years who were diagnosed with bipolar disorder type I according to diagnostic and statistical manual of mental disorders-5 (DSM-5) diagnostic criteria and who had manic and depressive episodes in the past are currently in the euthymic period. Those who were diagnosed with bipolar disorder type 2, had mixed episodes, had pregnancy, had known medical diseases (autoimmune diseases, acute infection, malignancy, dementia, neurodegenerative, and cerebrovascular diseases), had used anti-inflammatory drugs in the last 2 weeks, had used antibiotics in the last 4 weeks and had received immunosuppressive therapy were not included in the study. Lifetime history of antidepressant use was accepted as the exclusion criterion for the unipolar mania group.
The hospitalisation files and data of the patients in both groups were reviewed retrospectively, and all clinical signs of all manic episodes were checked. All symptoms of all past manic episodes were recorded to compare the symptoms during the manic episodes.
Sociodemographic data form, Young Mania Rating Scale (YMRS), Hamilton Rating Scale for Depression (HAM-D), Temperament Evaluation of Memphis, Pisa, Paris and San Diego-Autoquestionnaire (TEMPS-A), The Standardized Mini Mental State Examination (SMMSE) was administered to the participants.
Serum levels of BDNF, interleukin-1beta (IL-1β), interleukin-6 (IL-6), tumour necrosis factor-alpha (TNF-α), CRP and leucocytes were measured in blood samples of patients in the unipolar mania and bipolar disorder groups. Blood samples were taken in fasting condition between 08:00 and 10:30 am by nurses working in Trakya University Faculty of Medicine Department of Psychiatry. The blood samples were centrifuged at 3500 rpm for 10 min in the Biophysics Laboratory, and the resulting sera were divided into Eppendorf tubes and stored in a − 80°C deep freezer until ELISA was performed. After the patient enrolment process was completed, serum samples were analysed in the laboratory of the Physiology Department of Trakya University Faculty of Medicine using appropriate ELISA kits for, BDNF (Boster, Catolog: EK0307), TNF-α (Boster, Catalog: EK0525), IL-1β (Invitrogen, Catolog: KHC0011) and IL-6 (BioSource Europe SA, Catolog: KAC1261) according to the manufacturer’s instructions. CRP and leucocyte values were also measured in the laboratory.
Verbal and written consent was obtained from the patients who agreed to participate in the study. The study was approved by Trakya University Faculty of Medicine Ethics Committee.
Statistical analysis
Statistical analyses were performed in Trakya University Faculty of Medicine, Department of Biostatistics and Medical Informatics, using the IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp. (License No: 10240642) package program. The compatibility of the quantitative data to normal distribution was examined with a single sample Shapiro–Wilk test. Student t test was used for comparing the quantitative values showing normal distribution between unipolar and bipolar groups, and Mann–Whitney U test was used to compare variables that did not show normal distribution. One-way ANOVA test was used for the comparison of quantitative values consisting of three or more categories and showing normal distribution, and the Kruskal–Wallis test was used to compare those that did not show normal distribution. Spearman correlation analysis was used to examine the relationships between quantitative variables. P < 0.05 value was accepted as statistical significance limit value.
Results
In this study, we found that 40 (8.08%) of 495 patients diagnosed with bipolar disorder met the diagnostic criteria for unipolar mania. In the patient group with a diagnosis of unipolar mania, 16 (42.1%) were female and 22 (57.9%) were male, while 28 (66.7%) of the bipolar disorder patients were female and 14 (33.3%) were male. The mean age was 41.94 ± 8.94 years in the unipolar mania group and 42.64 ± 0.56 years in the bipolar disorder group, with no statistically significant difference in the mean ages of the two groups (p = 0.753). The comparison of the sociodemographic and clinical characteristics of the two groups is shown in Table 1.
Table 1. Comparison of unipolar mania and bipolar disorder groups by sociodemographic and clinical characteristics*

* Student t test, Mann–Whitney U test and χ2 test were used to calculate the data in this table.
A comparison of the two groups in terms of comorbid psychiatric diseases revealed no significant difference (p = 0.56). Eight patients (21.1%) in the unipolar mania group and eight patients (19.0%) in the bipolar disorder group had a diagnosis of hypothyroidism. There was no statistically significant difference between the groups in terms of hypothyroidism (p = 1.000).
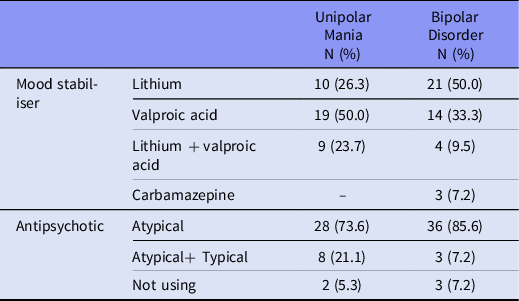
The most commonly used mood stabilisers were lithium (50%) in the bipolar disorder group and valproic acid (50%) in the unipolar mania group, and the results were statistically significant (p = 0.032). The mood stabilisers and antipsychotics used by the patients are shown in Table 2.
Table 2. Drugs used by patients in both groups
We found that among all manic symptoms during manic episodes, euphoria (p = 0.004), increased sexual interest (p = 0.004), delusions (p = 0.006) and grandiosity (p = 0.017) were more common in the patients in the unipolar mania group compared to the bipolar disorder group, and the differences were statistically significant. Manic symptoms, such as elevated mood, irritability, decreased sleep, pressured speech, increased speech, flight of ideas, agitation, hostility and increased goal-directed activity, were similar in both groups during manic episodes. Depressive mood and anxiety symptoms were significantly higher in manic episodes in the bipolar disorder group (p = 0.000). The distribution of the two groups according to their clinical characteristics is shown in Table 3.
Table 3. Distribution of both groups according to their clinical features in manic episodes*
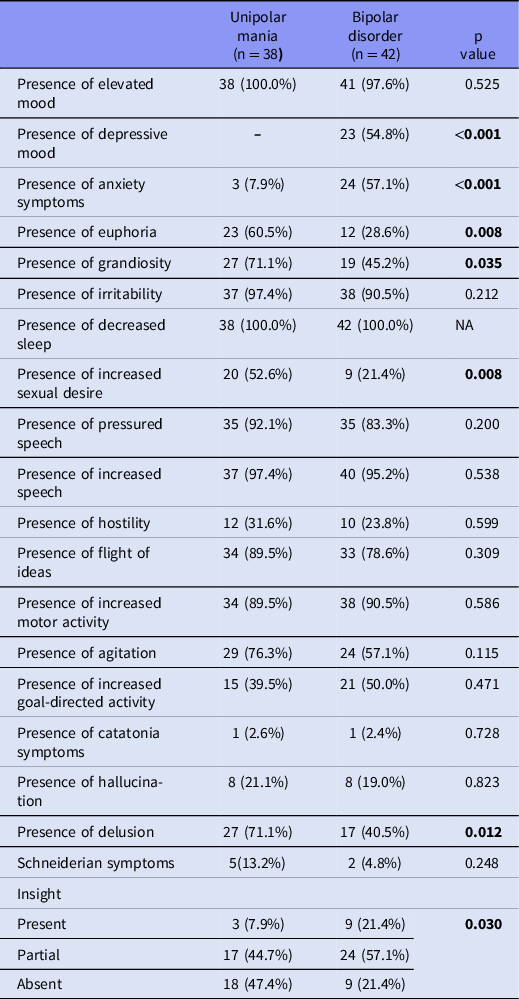
* Chi-square test was used to calculate the data in this table.
There was no statistical difference in the mean HAM-D, YMRS and SMMSE scores between the two groups. A comparison of the temperament types evaluated with the TEMPS-A scale showed that depressive (p = 0.004), cyclothymic (p = 0.005) and hyperthymic (p = 0.001) temperaments were significantly more predominant in the unipolar mania group than in the bipolar disorder group. There was no significant difference between the two groups in terms of irritable and anxious temperaments.
IL-6 levels (median [min–max], in pg/ml) were significantly higher in the unipolar mania group (17.23 [0.29–235.78]) than in the bipolar disorder group (10.74 [0.71–67.63], p = 0.046). CRP levels (median [min–max], in mg/dl) were significantly higher in the unipolar mania group (0.47 [0.30–2.58]) than in the bipolar disorder group (0.30 [0.15–1.56], p = 0.026). The mean values of TNF-α, IL-1β, leucocyte and BDNF were not statistically significantly different between the two groups. The comparison of the BDNF, TNF-α, IL-1β, IL-6, CRP and leucocyte levels of the two groups is provided in Table 4.
Table 4. Comparison of leucocyte, CRP, BDNF and cytokine levels of unipolar mania and bipolar disorder groups*

BDNF, brain-derived neurotrophic factor; CRP, C-reactive protein; IL-1β, interleukin 1 beta; IL-6, interleukin 6; TNF-α, tumour necrosis factor alpha.
* Mann–Whitney U test was used to calculate the data in this table.
We evaluated the relationship between suicide attempt history and the TNF-α, IL-1β, IL-6 and CRP levels of all patients (n = 80) included in the study. IL-6 levels (median [min–max], in pg/ml) were significantly lower in the patients with a history of suicide attempts (10.32 [2.38–54.25]) than in the patients who did not attempt suicide (17.02 [0.29–235.78], p = 0.020).
Discussion
In the literature, the prevalence of unipolar mania in patients diagnosed with bipolar disorder ranges between 1.1% and 65.3% (Yazici et al., Reference Yazici, Kora, Üçok, Saylan, Özdemir, Kiziltan and Özpulat2002; Dakhlaoui et al., Reference Dakhlaoui, Essafi and Haffani2008; Baek et al., Reference Baek, Eisner and Nierenberg2014; Stokes et al., Reference Stokes, Yalin, Mantingh, Colasanti, Patel, Bellivier, Leboyer, Henry, Kahn and Etain2020). In our study, it was found that 8.08% of 495 patients diagnosed with bipolar disorder met the diagnostic criteria for unipolar mania.
Although some studies have (Shulman & Tohen, Reference Shulman and Tohen1994; Yazici et al., Reference Yazici, Kora, Üçok, Saylan, Özdemir, Kiziltan and Özpulat2002, Dakhlaoui et al., Reference Dakhlaoui, Essafi and Haffani2008; Baek et al., Reference Baek, Eisner and Nierenberg2014) reported that patients who meet the diagnostic criteria for unipolar mania have an earlier age of disease onset than those meeting the bipolar disorder diagnostic criteria, many studies (Srinivasan et al., Reference Srinivasan, Ray and Gopinath1985, Makanjuola, Reference Makanjuola1985, Aghanwa, Reference Aghanwa2001, Pfohl et al., Reference Pfohl, Vasquez and Nasrallan1982) have shown that the age of disease onset of the two groups is similar, consistent with our study.
In our study, no difference was detected between the two groups in terms of the total number of episodes, but we found that the number of manic episodes was lower in the bipolar disorder group than in the unipolar mania group. Although these results are consistent with previous studies (Stokes et al., Reference Stokes, Yalin, Mantingh, Colasanti, Patel, Bellivier, Leboyer, Henry, Kahn and Etain2020), Perugi et al. (Reference Perugi, Passino, Toni, Maremmani and Angst2007) reported more manic episodes in the unipolar mania group; however, the total number of episodes in this group was found to be lower than in the bipolar disorder group.
A study that evaluated the temperament characteristics of unipolar mania patients (Yazici et al., Reference Yazici, Kora, Üçok, Saylan, Özdemir, Kiziltan and Özpulat2002) found that these patients had hyperthymic temperament. In another study, depressive temperament was never seen in the unipolar mania group, while 20.6% of the bipolar disorder group showed depressive temperament characteristics (Perugi et al., Reference Perugi, Passino, Toni, Maremmani and Angst2007). Another study revealed that anxious personality was two to three times more common in predominantly manic and bipolar disorder I patients than in patients with major depressive disorder and bipolar disorder II (Angst et al., Reference Angst, Gerber-Werder, Zuberbühler and Gamma2004). Similarly, we found that the anxious temperament scores of the bipolar disorder group were not higher than those of the unipolar mania group, and the mean anxious temperament scores were similar between the two groups. We further found that depressive, cyclothymic and hyperthymic temperaments were more predominant in the unipolar mania group than in the bipolar disorder group.
Patients with unipolar mania have more grandiosity (Abrams et al., Reference Abrams, Taylor, Hayman and Krishna1979; Pfohl et al., Reference Pfohl, Vasquez and Nasrallan1982) and delusions (Pfohl et al., Reference Pfohl, Vasquez and Nasrallan1982) than patients with bipolar disorder. In this study, we found that unipolar mania patients showed more euphoria, increased sexual interest, delusions and grandiosity among manic symptoms in their manic episodes compared to patients with bipolar disorder. Further, depressive mood and anxiety symptoms were found to be significantly higher during manic episodes in the bipolar disorder group. Perugi et al. (Reference Perugi, Passino, Toni, Maremmani and Angst2007) found that the rates of symptoms, such as increased sexual interest, grandiosity and delusions during manic episodes, were similar in both groups, but euphoria was more common in the unipolar mania group, while depressive mood, anxiety symptoms and hostility were significantly higher in the bipolar disorder group.
In our study, BDNF levels were similar in the unipolar mania and bipolar disorder groups. Since the total disease duration of both groups was equal and the BDNF levels were not different, we suppose that the episode type had no effect on BDNF levels and that the duration of the disease might have more effect on BDNF. However, Kauer-Sant’Anna et al. (Reference Kauer-Sant’anna, Kapczinski, Andreazza, Bond, Lam, Young and Yatham2009) observed lower BDNF levels in bipolar disorder patients with longer disease durations than those with shorter disease durations.
Many studies have examined the relationship between IL-6 and bipolar disorder. In our study, IL-6 levels were higher in the unipolar mania group than in the bipolar disorder group. In a meta-analysis, increased IL-6 levels were found during the manic, depressive and euthymic periods of bipolar disorder, and a significant increase in the cytokine was observed, especially in manic and hypomanic episodes (Sayana et al., Reference Sayana, Colpo, Simoes, Giridharan, Teixeira, Quevedo and Barichello2017). Lu et al. (Reference Lu, Rao, Mou, Chen, Lou, Zhang, Zhang, Xie, Hu and Fang2019) found that serum IL-6 levels were higher in patients with bipolar disorder than in patients with major depressive disorder, and they suggested that this cytokine could be used in the differential diagnosis of depressive episodes in bipolar disorder and major depressive disorder. Wiener et al. (Reference Wiener, Moreira, Cardoso, Mondin, Da Silva Magalhães, Kapczinski, De Mattos Souza, Da Silva, Oses and Jansen2017) found that IL-6 and IL-10 levels did not differ among patients with major depressive disorder, bipolar disorder, and their healthy control counterparts. A recent meta-analysis showed that IL-6 appeared to be a trait marker for bipolar disorder (Solmi et al., Reference Solmi, Sharma, Osimo, Fornaro, Bortolato, Croatto, Miola, Vieta, Pariante, Smith, Fusar-Poli, Shin, Berk and Carvalho2021).
CRP levels have been indicated as an indicator of mood episodes in bipolar disorder and may be associated with disease severity (Dickerson et al., Reference Dickerson, Stallings, Origoni, Boronow and Yolken2007; Dargél et al., Reference Dargél, Godin, Kapczinski, Kupfer and Leboyer2015; Wysokiński et al., Reference Wysokiński, Margulska, Strzelecki and Kłoszewska2015). In a study by Becking et al. (Reference Becking, Boschloo, Vogelzangs, Haarman, Riemersma-Van Der Lek, Penninx and Schoevers2013), high CRP levels observed in patients with a diagnosis of depression were thought to be an early warning sign for manic switch. In our study, CRP levels were found to be significantly higher in patients with unipolar mania than in the bipolar disorder group. This is primarily attributable to the higher levels of IL-6 in the unipolar mania group because CRP is released in response to proinflammatory cytokines (Chung et al., Reference Chung, Huang, Wu, Chen, Hsu and Tsai2013). Further, the fact that unipolar mania patients have more manic episodes may explain their higher CRP levels, as CRP has been associated with manic symptoms (Dickerson et al., Reference Dickerson, Stallings, Origoni, Boronow and Yolken2007; Uyanik et al., Reference Uyanik, Tuglu, Gorgulu, Kunduracilar and Uyanik2015).
Limitations
Given that the definition of unipolar mania is unclear and the number of studies examining the underlying biological differences is insufficient, our study is important in that it is the first to examine the serum cytokine and BDNF levels of patients with unipolar mania and bipolar disorder. Nevertheless, our research has some limitations that may be opportunities for future studies. The diagnosis of unipolar mania may be inaccurate due to the inability to remember past depressive episodes or predict possible future depressive episodes. The small sample size and the use of some scales based on self-reports are other limitations of our study. Further, age, gender, smoking, alcohol use and various antipsychotic treatments might have affected cytokine and BDNF levels. The presence of some chronic medical diseases (hypertension, DM, hypothyroidism) and the drugs they use may have affected the levels of cytokines and BDNF in some patients. Although there was no statistically significant difference in the number of patients with hypothyroidism in either group, the fact that hypothyroidism was not excluded might have affected the CRP and other results. The observation of depressive temperament in patients defined as unipolar mania can be further investigated in future studies.
Acknowledgement
We would like to thank Prof. Dr. Necdet Süt (Trakya University Faculty of Medicine, Department of Biostatistics) for his assistance in the statistical analysis of our study.
Authors contributions
YG, MKU and OP designed the study. YG and MKU collected the data. YG and MKU wrote the first draft. All authors (YG, MKU, and OP) participated in analysis and interpretation of data and revised the manuscript. All authors approved the final version of the manuscript.
Financial support
This work was supported by a research grant from Trakya University Scientific Research Project Committee (grant number: TUBAP2018/06). This work was not an industry-supported study. Each author declares that they have no financial conflict of interest.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.







