The Question: What to do when comorbid anxiety disorders are resistant to polypharmacy treatment?
The Psychopharmacological Dilemma: NMDAR antagonists on top of standard-of-care treatment achieve quick remission for major depressive disorder (MDD) – however, may be less effective for comorbid anxiety disorders?
 Pretest self-assessment question
Pretest self-assessment question
Does ketamine or esketamine worsen dissociation in patients with post-traumatic stress disorder (PTSD)?
 Patient evaluation on intake
Patient evaluation on intake
31-year-old man with a chief complaint of being “chronically depressed since his teenage years”
 Psychiatric history
Psychiatric history
Father was American, and mother is a Chinese national
Well-adjusted childhood up until relocating to China at age 10 after his parents’ divorce
Had a hard time adjusting to Chinese culture and language
Went back to an American high school and had a hard time readjusting to American culture and relearning English
Confused about his identity as a biracial white/Asian man
Never felt he “fit in” and was “always bullied”
Sexually traumatized at the age of 14
Gradually developed depression, anxiety, and paranoid traits after this series of unfortunate childhood events
Admits to full chronic major depressive disorder (MDD) symptoms
° Feeling depressed since his teenage years without any remission
° Has frequent passive suicidal ideation with occasional active thoughts and plans, but no attempts
° Has fatigue, low energy, poor concentration, sense of guilt, worthlessness, and sleep problems
Admits to full generalized anxiety disorder (GAD) symptoms
° Feels generally anxious, on edge, fatigued
° Has poor concentration and difficulty making decisions
° Has extreme muscle tension in neck and shoulders, and tightness in his chest when anxious and agitated
Admits to mild social anxiety disorder symptoms
° Feels generally socially anxious most of time around people
° Reports anticipatory anxiety and fear of being scrutinized, or feeling as though he will not fit in
° Reports increased chest discomfort, sweating, palpitations with these events
Admits to moderate PTSD symptoms
° Reports childhood sexual trauma
° Was recently physically assaulted
° Reports intrusive flashbacks, daytime memories, and sleeping difficulties
° Reports hyperarousal and agitation
Has some dependent, avoidant, and paranoid traits
° Likely part of his temperament or personality
° Shaped through his life experiences and traumas
 Social and personal history
Social and personal history
Has a stable engineering job; however, relies on others for some instrumental activity support such as driving
Has a significant girlfriend of several years
Attended college
Estranged from his biological mother, stepfather passed away, biological father was never part of his life
Drinks about 500 mg of caffeine per day, usually energy drinks
Used to smoke about half a pack of cigarettes per day and switched to vaping
Does not misuse or overuse current medications or use any other drugs
Drinks alcohol only occasionally
 Medical history
Medical history
Irritable bowel syndrome (IBS), constipation predominant
Hypertension
 Family history
Family history
Denies any known mental illness in any family member
 Medication history
Medication history
Failed to respond to the norepinephrine–dopamine reuptake inhibitor (NDRI) antidepressant bupropion (Wellbutrin XL) 300 mg/d
Is on his first full-course trial of selective serotonin reuptake inhibitor (SSRI), now in combination with his NDRI above
Reports minor benefit with depression and irritable bowel symptoms on current regimen
 Current medications
Current medications
Bupropion (Wellbutrin XL) 300 mg/d
Sertraline (Zoloft) 200 mg/d
Alprazolam (Xanax) 1.5 mg/d
Zolpidem (Ambien) 5 mg/d
 Psychotherapy history
Psychotherapy history
Has never had weekly psychotherapy sessions
Attended monthly dialectical behavioral therapy (DBT) group sessions occasionally in the past
 Patient evaluation on initial visit
Patient evaluation on initial visit
Chronic depressive and anxiety symptoms associated with unfortunate series of negative life events
Had to move between two countries and adjust to two cultures and is biracial
Felt like he never fit in into either American or Asian culture
Likely did not have the opportunity to create own identity in teenage years and now has existential dilemma. This might be the root cause for most of his psychiatric symptoms
Also has moderate PTSD symptoms from being abused and being bullied
Currently has frequent passive suicidal ideation – however, had active thoughts and plans in the past but never acted on them
Seems very depressed, despondent with flat affect
Has risks of harming himself but has been resilient and able to maintain not acting on suicidal impulses
° However, currently guarded about committing to his safety plan
° Suggests possible need for inpatient stay
Reports no current side effects besides slight decrease of libido
 Question
Question
In your clinical experience, would you expect a patient such as this to recover?
Yes, he has good social support and is functional at work
No, his depression and anxiety with comorbid PTSD are likely chronic and unremitting
 Attending physician’s mental notes: initial psychiatric evaluation
Attending physician’s mental notes: initial psychiatric evaluation
This patient currently has moderate to severe chronic MDD, moderate GAD, and moderate PTSD. They are likely generated by his long-term stressors and early negative life events
The traits and defense mechanisms he developed over the years have made him relatively resilient, and he can maintain a demanding job and a significant relationship with his girlfriend
He has been somewhat undertreated; only has had a full course of two antidepressant trials
He is at risk of harming himself now, based on his current presentation
His prognosis is fair to good if we can generate reasonable, appropriate, and aggressive psychotherapy, pharmacotherapy, and possibly neuromodulation interventions
Likely needs an inpatient stay or a faster-acting treatment with increased outpatient monitoring
 Question
Question
Which of the following would be your next step?
Increase zolpidem (Ambien) and alprazolam (Xanax) to a higher dose for his insomnia and anxiety disorders
Augment the current medications with psychotherapy to consolidate treatment results
Augment the current medications with 5-HT1A receptor partial agonist anxiolytic buspirone (BuSpar)
Augment the current medications with an atypical antipsychotic
Refer for inpatient electroconvulsive therapy (ECT)
Refer for outpatient esketamine (Spravato) nasal spray treatment
Do nothing additionally outside of wait for current medication regimen effectiveness to occur
 Attending physician’s mental notes: initial psychiatric evaluation (continued)
Attending physician’s mental notes: initial psychiatric evaluation (continued)
Patient was recently started on a standard-of-care treatment for his MDD with comorbid anxiety disorders using sertraline (Zoloft) and bupropion (Wellbutrin XL)
° This is likely not adequate as he has had a minimal response and he may need more aggressive treatment now
° His MDD presentation is of profound despair with increased suicidal thinking
Does meet criteria now for severe MDD, moderate GAD, and moderate PTSD
Zolpidem (Ambien) and alprazolam (Xanax) can be continued for now
Starting buspirone (BuSpar) or aripiprazole (Abilify) to augment sertraline (Zoloft) makes sense, but delayed response time likely
While one of these is being considered, will attempt to obtain esketamine (Spravato) prior authorization from his insurance company
 Further investigation
Further investigation
Is there anything else that you would like to know about the patient?
What about details concerning current medication regimen?
Currently on the maximum dose of sertraline (Zoloft) at 200 mg/d
° Has had some minor benefit for his MDD and IBS
° Tolerates the drug well but has decreased libido
Currently taking bupropion (Wellbutrin XL) 300 mg/d
° Tolerates well
° Could be increased further
Currently taking zolpidem (Ambien) and alprazolam (Xanax)
° Improves his sleep and agitation somewhat
° Both have been generally less and less effective over the years
 Attending physician’s mental notes: interim follow-up through 8 weeks
Attending physician’s mental notes: interim follow-up through 8 weeks
This patient has continuing symptoms and we can be more aggressive with the current medications
Also could consider rational polypharmacy, given the patient has had enough time on current drugs to see that they are not fully helping to reduce his symptoms
 Case outcome: interim follow-up at 8 weeks
Case outcome: interim follow-up at 8 weeks
Buspirone (BuSpar) 30 mg/d was gradually added to his bupropion (Wellbutrin XL) and sertraline (Zoloft) regimen by his primary care provider after the initial intake
° This rational polypharmacy approach adds 5-HT1A receptor partial agonism as a unique mechanism to treat his symptoms better
Patient has had more therapeutic time on the well-dosed SSRI and NDRI products
Still reports same severe MDD symptoms as 8 weeks ago
Specifically calls to request to start esketamine (Spravato) nasal spray treatment for his resistant MDD and suicidal thoughts
 Question
Question
How would you change his medication regimen?
Continue everything as is
Continue current medication regimen at higher doses, except for sertraline (Zoloft) since it is already at maximum dose
Start esketamine (Spravato) nasal spray 56–84 mg twice weekly treatment and continue his current medication regimen
Start esketamine (Spravato) nasal spray 56–84 mg twice weekly treatment, but discontinue all previous psychotropics as none was effective
 Case outcome: interim follow-up visit at 12 weeks
Case outcome: interim follow-up visit at 12 weeks
Patient started and has had seven consecutive esketamine (Spravato) treatment sessions in the past 4 weeks
° He took 56 mg/d for his first two sessions, which he tolerated well, but showed no improvement
° He now takes 84 mg/d routinely twice weekly
° During treatments, he experienced mild sedation only
Depression symptoms seemingly improving per the Patient Health Questionnaire (PHQ-9)
° PHQ-9 rating scale scores decreased from 22 4 weeks ago to 13 now
Reports remarkably less GAD and PTSD agitation
Now uses alprazolam (Xanax) and zolpidem (Ambien) only sparingly
No PTSD symptom improvement outside of hyperarousal, but also no exacerbation
 Question
Question
Would you expect PTSD symptoms to worsen with esketamine (Spravato)?
Yes, esketamine (Spravato) treatment is known to cause dissociation which is a hallmark symptom of PTSD
Yes, only to a minor degree, but the gains for alleviating his depression and suicidality would be worth it
No adverse effects for his PTSD are expected
 Case outcome: third interim follow-up visit at 16 weeks
Case outcome: third interim follow-up visit at 16 weeks
Continues sertraline (Zoloft), alprazolam (Xanax), zolpidem (Ambien), buspirone (Buspar), and bupropion XL (Wellbutrin XL)
The NDRI bupropion XL (Wellbutrin XL) now increased to 450 mg/d, to maximal dosing, as full remission not yet gained from esketamine (Spravato) use
Has had 13 esketamine (Spravato) intranasal spray treatment sessions in the past 2 months
Adjusted frequency and dosage of esketamine (Spravato) as needed
° 56 mg twice weekly for 1 week
° 84 mg twice weekly for 3 weeks
° 84 mg once weekly thereafter
After this course, opted to spread out his dosing schedule to every 2 weeks, 4 weeks, then 6 weeks, etc., to try to wean off this treatment
Blood pressure has been increasing, with diastolic hovering around 90 mmHg, which may be his new normal
° Possibly due to noradrenergic drive from the increased bupropion (Wellbutrin XL) vs. the beginning of idiopathic essential hypertension
° Unlikely due to esketamine (Spravato) as this drug now washes out between his treatment sessions
° Interestingly, his pressure lowers 10 points during esketamine (Spravato) treatment sessions, where esketamine (Spravato) is supposed to escalate blood pressure 10 points, per regulatory agencies, during a session
Patient is asking about further treatment options for PTSD
° Still complains of some insomnia and intrusive thoughts
 Attending physician’s mental notes: third interim follow-up visit (month 8)
Attending physician’s mental notes: third interim follow-up visit (month 8)
Patient’s MDD symptoms are remitted
° He has better range of affect, is psychomotor normal, no longer despondent nor suicidal
° Esketamine (Spravato) intranasal spray can eventually be tapered off
° He can continue SSRI/SNRI and buspirone (BuSpar) as his maintenance augmentation treatment
° Is not using any sedative/hypnotic agents now
PTSD and generalized anxiety symptoms persist
° His PTSD hyperarousal symptoms did respond to esketamine (Spravato) intranasal spray treatment sessions; however, his remaining reliving and avoidance PTSD symptoms continue
° No increases in dissociative PTSD symptoms noted
° Can see whether he has had specialized psychotherapy for his trauma vs. more complex polypharmacy for his residual PTSD symptoms may be needed
 Question
Question
What would you do next?
As his PTSD symptoms persist, refer him to eye movement desensitization and reprocessing (EMDR) therapy for his persisting PTSD symptoms
As his PTSD symptoms persist, add another psychotropic agent for PTSD, such as an atypical antipsychotic or noradrenergic-dampening blood pressure lowering agent
Continue to wait on the current regimen for full effectiveness to occur as he doesn’t have severe side effects
 Case outcome: fourth interim follow-up visit at 20 weeks
Case outcome: fourth interim follow-up visit at 20 weeks
 Case debrief
Case debrief
This patient had unfortunate early life experiences
This likely contributed to his chronic MDD, PTSD, social anxiety disorder, and GAD since his teenage years
His symptoms were relatively undertreated, until there was maximization of his SSRI and NDRI antidepressants
Despite this, plus a buspirone (BuSpar) augmentation, his symptoms persisted
Given his remarkable depression and increased suicidal thoughts, his insurance company allowed him to start weekly esketamine (Spravato) nasal spray treatment, which likely helped to avoid an inpatient stay
MDD symptoms drastically improved during his several-month esketamine (Spravato) intranasal spray trial, with some frequency and dosage adjustments in between
GAD symptoms also improved but not as significant as the improvement of his MDD symptoms
PTSD symptoms did not exacerbate and actually mildly improved
In practice, this patient plans to continue to spread out the esketamine (Spravato) treatments and eventually taper off
He asked to try EMDR therapy for his PTSD
 Take-home points
Take-home points
The Food and Drug Administration (FDA) and other guidelines suggest a few drugs and devices be used for treatment-resistant depression (TRD) or MDD augmentation
° Olanzapine–fluoxetine combination (Symbyax)
° Aripiprazole (Abilify)
° Quetiapine (Seroquel)
° Brexpiprazole (Rexulti)
° Cariprazine (Vraylar)
° ECT
° Transcranial magnetic stimulation (TMS)
° Vagal nerve stimulation (VNS)
Most antidepressants can take weeks before starting to alleviate MDD
Ketamine is a non-competitive antagonist of glutamate receptors of the N-methyl-D-aspartate (NMDA) type and has compelling off-label data for use in TRD
Esketamine (Spravato) is the S-enantiomer of ketamine that has stronger affinity to antagonize NMDARs, which was recently approved by the FDA for TRD
° Intranasal esketamine (Spravato) given in conjunction with standard-of-care antidepressant treatment may result in rapid improvement in MDD symptoms compared to standard-of-care treatment alone and is considered an augmentation strategy
° Esketamine (Spravato) can also lower suicidal thinking from MDD according to the FDA
PTSD has a prevalence of 8.7% in the United States and is often treatment resistant
Individuals with PTSD are 80% more likely than those without PTSD to be diagnosed with at least one other psychiatric disorder, commonly including MDD, substance use disorders (SUDs), and anxiety disorders
SSRIs are the only psychotropic class approved for treating PTSD – however, many patients tend not to achieve full remission with SSRI therapy
There is some evidence that ketamine IV infusion can lead to rapid reduction in symptom severity in patients with chronic PTSD, albeit with slight increased risk of dissociation
In our case, the patient’s resistant MDD symptoms achieved remission gradually after a 2-month initial trial of esketamine (Spravato). However, his PTSD definitely did not worsen
 Performance in practice: confessions of a psychopharmacologist
Performance in practice: confessions of a psychopharmacologist
What could have been done better here?
Should more psychotherapy (CBT, psychodynamic, or EMDR) have been given sooner?
° This may have alleviated the MDD, GAD, and PTSD symptoms if started in conjunction with the esketamine (Spravato) intranasal spray
° However, it was felt that his level of MDD and PTSD may have actually interfered with the provision of and benefit from psychotherapy
Should more aggressive medications be prescribed for his insomnia, GAD, and PTSD?
Should failure of the SSRI and NDRI warrant a trial on other FDA-approved medication for TRD before starting esketamine (Spravato)?
° This is unclear. He has not tried tricyclic antidepressants (TCAs) or monoamine oxidase inhibitor (MAOI) antidepressants
° Some may argue that these agents are riskier in overdose and carry a higher side-effect burden than the regimen used in this case
What are possible action items for improvement in practice?
Research information available for treatment guidelines regarding TRD with comorbid PTSD and GAD
Research data or clinical trials on effectiveness of esketamine (Spravato) for treatment-resistant PTSD
Further exploration on other future indications for esketamine (Spravato), such as bipolar depression
Research information on potential side effects of esketamine (Spravato) when combined with other medications
° This patient had a mildly elevated systolic and diastolic blood pressure while taking esketamine (Spravato) trial plus an increased dose of bupropion XL (Wellbutrin XL)
 Tips and pearls
Tips and pearls
About one-third of patients with MDD do not respond to available antidepressants and suffer from TRD
Current treatment options for TRD are limited
Intranasal esketamine (Spravato) has rapid antidepressant effects within 4 hours to 1 day after a single dose, and the response rates are ultimately comparable to 8-week trials of monoaminergic-based antidepressants
Esketamine (Spravato) plus oral antidepressant is more effective than oral antidepressants alone per regulatory trials
Most common side effects include nausea, headache, sedation, and sometimes mild dissociation
Abuse and misuse of esketamine (Spravato) is a concern of this newly approved medication but it is held and dispensed by the provider, so addiction and diversion in reality are quite negligible
Esketamine (Spravato) can also transiently increase patient’s blood pressure, with some occasionally increasing more than 40 mmHg, while the average is 10 mmHg, and it may lower breathing rate
° The blood pressure increase usually peaks around 40 minutes after administration
A Risk Evaluation and Mitigation Strategy (REMS) was implemented by the FDA for esketamine to ensure safe use
PTSD can often be treatment resistant and SSRIs have limited efficiency
Ketamine and esketamine (Spravato) might be a novel treatment for PTSD; however, more data is needed
Clinicians should likely supplement PTSD pharmacologic treatment with psychotherapy
 Mechanism of action moment
Mechanism of action moment
Why might NMDA antagonists potentially be able to treat both depression and anxiety disorders?
Glutamate is an important excitatory neurotransmitter in the brain
° Glutamatergic system dysfunction is likely related to the pathophysiology of multiple psychiatric disorders, such as MDD, GAD, PTSD, and schizophrenia (SP)
° Reduced glutamate levels in the prefrontal cortex have been associated with failed antidepressant treatment
N-methyl-D-aspartate receptors (NMDARs) are ionotropic glutamate receptors
° Allow calcium ions to enter the cell from extracellular space
▪ Calcium influx through the NMDARs leads to long-term potentiation and synaptic plasticity
° Composed of subunits NR1, NR2 (NR2A–NR2D), and NR3 (NR3A and NR3B)
▪ NR1 binds glycine and NR2 binds glutamate
° Ketamine is a non-competitive NMDA antagonist and decreases the opening frequency of NMDARs
° NMDAR blockade allows downstream disinhibition of glutamate signaling of alpha-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid receptors (AMPARs) as well
° Increased downstream glutamate activity may increase neuronal dendritic growth, synaptogenesis, brain-derived neurotrophic factor (BDNF) availability, vascular endothelial growth factor (VEGF), and mTOR signaling, all of which seem to be biomarkers of good antidepressant activity
Alpha-amino-3-hydroxy-5-methyl-4-isoazolepropionic acid receptors (AMPARs) are ionotropic glutamate receptors
° Composed of subunits GluR 1–4
° Ketamine rapidly increases downstream glutamate activity in the medial prefrontal cortex (mPFC), leading to increased synaptic transmission of AMPARs in the mPFC
° Ketamine can also upregulate AMPAR subunit (GluR1 and GluR2) expression, and increase synaptogenesis and connectivity in the prefrontal cortex (PFC) and hippocampus through activating BDNF and mTOR pathways
° This reverses stress- and depression-induced loss of connectivity between the PFC and other structures in the limbic system, which may also explain the antidepressant action of ketamine
Esketamine is the S(+)-enantiomer of ketamine and has greater affinity and anesthetic potency than R-ketamine, and therefore also seems to rapidly resolve MDD symptoms
GAD and PTSD symptoms are also linked to NMDAR overactivity
° Impaired connection in glutamatergic synapses in corticolimbic circuits can lead to hypothalamic–pituitary–adrenal (HPA) axis dysfunction, which is implicated in development of PTSD and other anxiety disorders
° BDNF then may decrease while under social stress which may lead to anxiety symptoms when there’s loss of top-down cortical control over limbic structures which are felt to control fight or flight responses in mammals
° Treatment with some antidepressants, CBT, ECT, VNS, and NMDA antagonists can increase BDNF expression, ideally reversing this process
° This may explain the potential for NMDA antagonists such as esketamine (Spravato) to be effective for anxiety disorders
° This potential mechanism still needs to be further investigated with translational and clinical trials
 Two-minute tutorial
Two-minute tutorial
Treatment for PTSD
SSRIs are the first-line recommendation for patients with PTSD
° There is great phenotypic symptom overlap between DSM-5-diagnosed MDD and PTSD and GAD (Figure 2.1)
° Among all the SSRIs, only sertraline (Zoloft), paroxetine (Paxil), and fluoxetine (Prozac) were recommended based on evidence for efficiency by the 2017 Veterans’ Affairs / Department of Defense Clinical Practice Guideline (CPG)
° Only sertraline (Zoloft) and paroxetine (Paxil) are approved for PTSD treatment by the FDA
° All other medications, including the ones mentioned below, are used “off label” with practice guideline support only
° Maximum benefit from SSRI treatment depends on adequate dosages, duration of treatment, and treatment adherence
Other antidepressant options for PTSD
° Venlafaxine, an SNRI, is a promising medication with both serotonergic and noradrenergic characteristics that balances serotonergic and noradrenergic neurotransmission via dual monoaminergic reuptake inhibition
° Nefazodone may also be effective
▪ Blocks serotonin-2A receptors and serotonin reuptake
▪ Not utilized much due to liver toxicity and unavailability
° TCAs can be beneficial too since some are serotonergic/noradrenergic-balanced as well
▪ A potential alternative only if a patient fails to respond to SSRI/SNRI
▪ Must observe EKG for QT prolongation, check plasma levels, and watch for remarkable anticholinergic effects
° MAOIs can be effective, because they increase serotonin, dopamine, and norepinephrine simultaneously
▪ Requires dietary restriction
▪ Interaction with other serotonergic agents can be fatal
Beta blockers (BBs) (noradrenergic β1 and β2 receptor antagonists)
° May be used for comorbid conditions with PTSD, such as performance anxiety or social anxiety disorder
° Tends to improve hyperautonomic symptoms (palpitations) and tremulousness
° Not supported by evidence in treating core PTSD symptoms
Alpha blockers (noradrenergic α1 receptor antagonists)
° Specifically studied and utilized for nightmares associated with PTSD
° Not supported by evidence in treating core PTSD symptoms
BZs
° Studies have not shown that they are effective overall in treating core PTSD symptoms
° Concerns including falls, addiction, danger in driving, having trouble integrating the traumatic experience, and withdrawal are well noted in the literature
° PTSD outcome may worsen with BZs and unfortunately increase overall mortality
° Interestingly, some reports suggest that their use may lower the effectiveness of ketamine and esketamine treatment in MDD
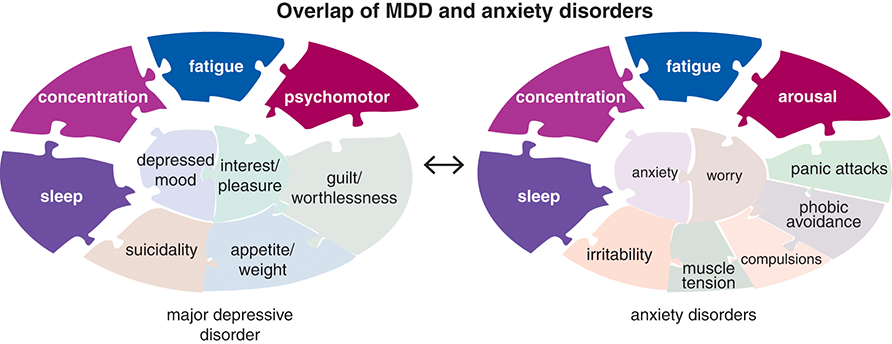
Figure 2.1 Overlap of MDD and anxiety disorders. Although the core symptoms of anxiety disorders (anxiety and worry) differ from the core symptoms of major depression (loss of interest and depressed mood), there is considerable overlap among the rest of the symptoms associated with these disorders (compare the “anxiety disorders” puzzle on the right to the “MDD” puzzle on the left). For example, fatigue, sleep difficulties, and concentration difficulties are common to both types of disorders. If certain SSRI antidepressants are able to alleviate both depression and anxiety symptoms, it makes intuitive sense that ketamine and esketamine may also share in an ability to treat both disorders. In this case, for example, we saw a remarkable reduction in psychomotor agitation and insomnia.

Figure 2.2 PTSD. The characteristic symptoms of PTSD are shown here. These include the core symptoms of anxiety while the traumatic event is being re-experienced as well as worry about having the other symptoms of PTSD, such as increased arousal and startle responses, sleep difficulties including nightmares, and avoidance behaviors. It would be interesting to see whether future research into esketamine use for PTSD will show an ability to treat all PTSD symptom clusters or just the hyperarousal components as seen in this case.
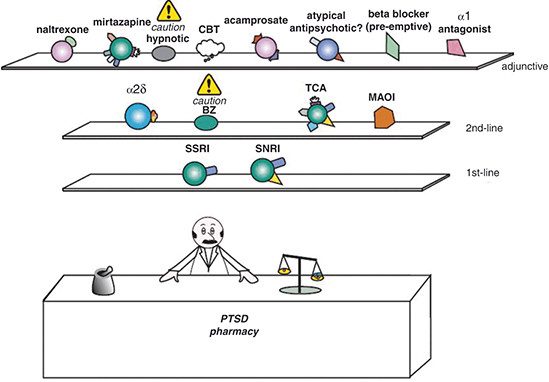
Figure 2.3 PTSD pharmacy. First-line pharmacological options for PTSD are SSRIs and SNRIs. In PTSD, unlike other anxiety disorders, BZs have not been shown to be as helpful, although they may be considered with caution as a second-line option. Other second-line treatments include α2 ligands, TCAs, and MAOIs. Several medications may be used as adjuncts for residual symptoms, and cognitive behavioral therapy (CBT) is typically recommended as well.
 Post-test question
Post-test question
Does ketamine or esketamine worsen dissociation in patients with post-traumatic stress disorder (PTSD)?
The data for use in PTSD is limited but, given that doses are kept low to avoid dissociative effects, there has not been much worsening of PTSD noted so far in trials.


 Patient evaluation on intake
Patient evaluation on intake  Medical history
Medical history  Current medications
Current medications  Attending physician’s mental notes: initial psychiatric evaluation
Attending physician’s mental notes: initial psychiatric evaluation  Further investigation
Further investigation  Take-home points
Take-home points  Performance in practice: confessions of a psychopharmacologist
Performance in practice: confessions of a psychopharmacologist  Tips and pearls
Tips and pearls  Mechanism of action moment
Mechanism of action moment  Two-minute tutorial
Two-minute tutorial 

