In order to understand how to prevent conception, it is helpful to understand when, where and how it happens. Key to this is an understanding of the reproductive system and what happens during the menstrual cycle. This will support understanding of how contraception works. This chapter is a useful overview of the basics, to help with later chapters.
Reproductive Organs
The ovaries have two key functions: they store eggs (ova) and produce the hormones that control the menstrual cycle, reproduction and sexuality. Girls are born with some two million eggs in their ovaries, but the number gradually declines over time; by puberty, typically 250,000 remain. During each menstrual cycle, an egg (ovum) matures in one of the ovaries and is released into the fallopian tube (ovulation). The egg can only be fertilised by a sperm while it is in the first third of the fallopian tube. If fertilisation happens, a blastocyst is created, which is a growing ball of cells that will develop into a fetus.
The womb (uterus) is where a blastocyst implants and grows during pregnancy. The lining of the womb (the endometrium) thickens during the 14 days up to ovulation, in preparation for implantation. Following ovulation, the hormone progesterone released from the egg shell (corpus luteum) causes the number of glands in the lining of the womb to increase, in order to provide nutrients for the blastocyst. If fertilisation doesn’t occur, the lining of the womb is shed – this bleeding is a period (menstruation).
The womb is connected to the vagina via the cervix (the neck of the womb), as shown in Figure 1.
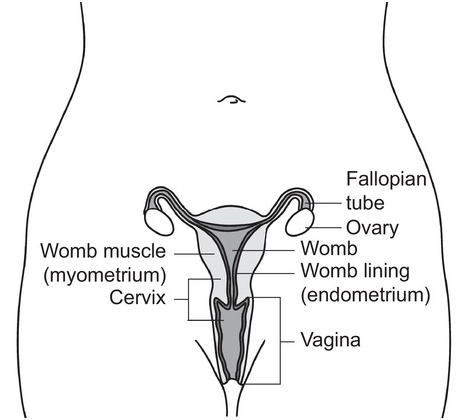
Figure 1 The reproductive organs are contained in the pelvis. The cervix lies between the vagina and the womb. Eggs are stored and develop (mature) in the ovaries and travel along the fallopian tube to the womb.
The Menstrual Cycle
Day 1 of the menstrual cycle is the first day of bleeding (menstruation – shedding of the lining of the womb). This is also when the next egg starts to develop (mature) in the ovary (so day 1 becomes a more logical designation). Figure 2 shows what happens to the egg and lining of the womb during each cycle.
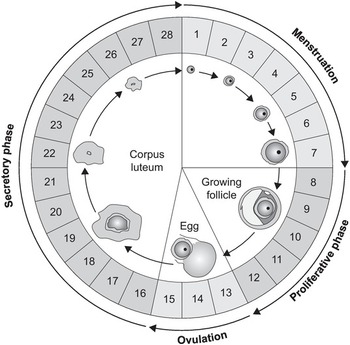
Figure 2 This diagram shows the changes in the womb during the menstrual cycle and the development of the egg. An egg starts to develop (mature) in the ovary while the womb lining is shed during menstruation, and continues through the proliferative stage, which is when the womb lining starts to thicken again. The mature egg is usually released (ovulation around day 13–15). The corpus luteum, which is left behind after ovulation, releases hormones that cause the lining of the womb to thicken and develop glands, in order to support a developing fetus. If the egg is not fertilised, however, the corpus luteum dies and menstruation starts.
The Egg
The maturing egg is known as a follicle. It gradually matures during the first 7 days of the cycle. Ovulation occurs around day 13–14 – the egg is released from the follicle into the fallopian tube and starts to travel towards the womb. The egg leaves a ‘shell’ in the ovary (the corpus luteum), which releases hormones. In reality, several follicles start to develop, but one generally becomes dominant and capable of releasing a mature egg, with the potential to become a pregnancy if fertilisation occurs.
The Womb
Once menstruation has ended, the lining of the womb starts to thicken again as the follicles develop – this is known as the proliferative phase. Following ovulation, the lining of the womb thickens further and also develops glands that will provide nutrients for a developing blastocyst, if the egg is fertilised. This is known as the secretory phase and predictably lasts 14 days (lifespan of the corpus luteum). If a blastocyst doesn’t implant, menstruation starts, marking the start of the next cycle.
Hormonal Control of the Menstrual Cycle
The menstrual cycle is controlled by hormones.
At the beginning of the cycle, follicle-stimulating hormone (FSH) is released from the pituitary gland in the brain. This triggers growth of the follicles in the ovary, each of which contains an egg (ovum).
As the follicles develop, they secrete estrogen into the bloodstream. Estrogen causes the lining of the womb to thicken during the first half of the menstrual cycle.
When the level of estrogen in the bloodstream reaches a critical level, this feeds back to the brain to switch off the release of FSH so that no further eggs mature during that cycle.
Also, when a critical level of estrogen is reached, another hormone called luteinising hormone is released from the pituitary gland. This triggers the release of the mature egg from the dominant follicle.
The corpus luteum that remains in the ovary after the egg is released produces both estrogen and progesterone. Progesterone causes the secretory changes in the lining of the womb through its effects on glands, as described above.
If the blastocyst implants, the corpus luteum continues to produce hormones that support the pregnancy during the first 12 weeks (until the placenta develops and takes over). If implantation does not occur, the level of progesterone gradually falls and menstruation starts.
The changes in hormone levels during the menstrual cycle are shown in Figure 3.
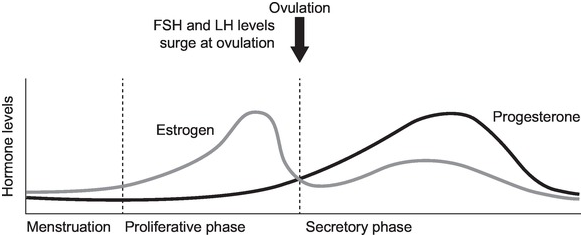
Figure 3 The menstrual cycle is controlled by hormones. Estrogen is released from the developing follicles during the first part of the cycle, so levels rise. Estrogen influences the levels of follicle-stimulating hormone (FSH), which causes the eggs to mature, although, usually, only one is released. Luteinising hormone (LH) triggers release of the egg at ovulation. After ovulation, progesterone is released from the corpus luteum.
Timing of Menstrual Cycles
While the ‘average’ menstrual cycle lasts 28 days, cycle length varies among women, and also at different times through a woman’s reproductive life; cycles of 25–32 days are considered normal. The second (secretory) part of the menstrual cycle predictably lasts about 14 days, whereas the first (follicular) part varies more widely. For example, in a regular 28-day cycle, ovulation occurs at about day 14 and the follicular and secretory stages are each about 14 days. Ovulation occurs earlier in shorter cycles. For example, in a 25-day cycle, menstruation and the follicular stage are likely to last about 11 days while the secretory stage will still be about 14 days, and ovulation is likely to occur at about day 11. This is illustrated in Figure 4.
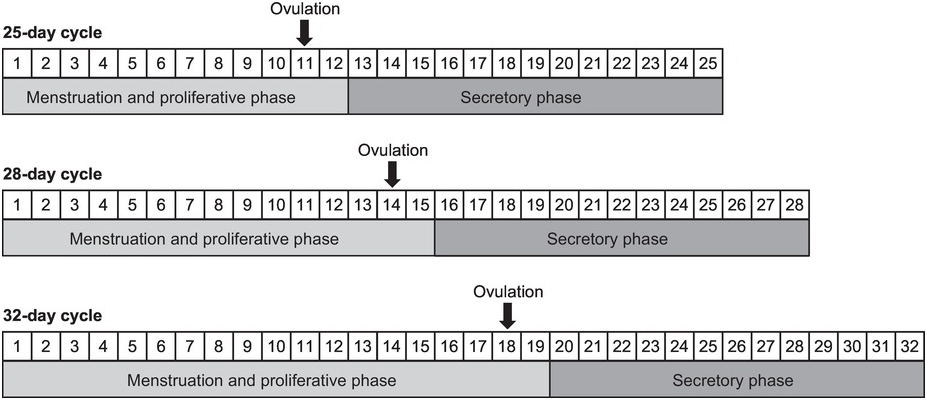
Figure 4 Timing of ovulation in cycles of different length. The secretory phase is predictably 14 days because this is how long the corpus luteum lasts. Women with shorter cycles ovulate earlier than day 14; women with longer cycles ovulate later than day 14.
Many women experience irregular cycles, particularly when they first start having periods, and again in later life when they reach the perimenopause, which usually starts from the mid-40s onwards. During these life stages, ovulation does not necessarily occur in every cycle. However, it is important to remember that even when cycles are irregular, ovulation may still occur, so contraception is needed to prevent an unplanned pregnancy. This includes when breastfeeding – many women don’t have periods while breastfeeding, but they may still ovulate.
Conception
The term conception refers to implantation, which, in medical terms, is when pregnancy is considered to start. However, some people consider that pregnancy starts at fertilisation – when the sperm and egg combine. The egg survives for no more than 24 hours after ovulation, and the period when fertilisation can occur is just a few hours, when the ovum is in the first third of the fallopian tube (nearest the ovary). However, sperm can survive in the fallopian tubes for several days, so if sperm are already in the fallopian tube at ovulation, fertilisation may occur. This means that the fertile window (i.e., the time when fertilisation is possible) is much longer than the few hours when the egg is viable. If the timing of sexual intercourse, the egg, sperm, fallopian tubes and lining of the womb are all optimal, the chance of achieving a pregnancy in any one cycle is about 25%. Figure 5 shows the most fertile and least fertile parts of the menstrual cycle. While the likelihood of conception varies through the menstrual cycle, contraception should always be used to prevent an unplanned pregnancy – for many women there are too many variables to reliably predict a ‘safe’ time. This is discussed in more detail in Chapter 7.
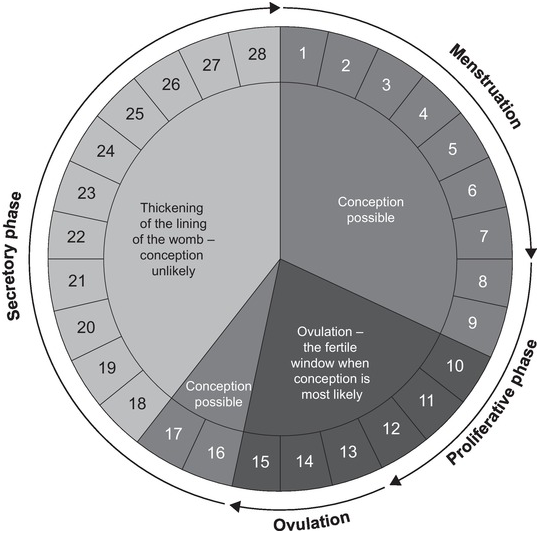
Figure 5 Fertility varies during the menstrual cycle. The most fertile time (which is when conception is most likely) is around ovulation. However, the timing of ovulation is hard to predict, and sperm can live for several days, so there is a risk of conception if a woman has sex without using contraception in the days leading up to ovulation. However, the egg is only viable for 24–48 hours, after which conception is unlikely.
Contraception – the prevention of conception – can be achieved in three key ways, described in the subsequent chapters:
by preventing ovulation – this is how the injection, implant and pills work
by preventing fertilisation – this is how barrier methods work and methods based on the timing of sexual intercourse
by preventing implantation – this is how the coil works (in addition, the copper in the copper coil is toxic to sperm, which can prevent fertilisation).
Fact: Even if you aren’t having a regular period, you may still be ovulating, for example, when breastfeeding or during the menopause transition – two common misunderstandings. Fact: As shown on Figure 5, you are most fertile around the time of ovulation, but this may not necessarily be on day 13/14 – the timing of ovulation can vary. It is also important to remember that sperm can survive for up to 7 days, which extends the fertile window. Fact: You can become pregnant in any menstrual cycle, even if it is the first time you have sex. Fact: As described above, conception depends on the timing of ovulation and the viability of sperm. Whilst implantation cannot occur while the lining of the womb is being shed during your period, sperm are viable for several days and may therefore survive until you ovulate, particularly if you ovulate early or have a short cycle. Myth 1: I don’t have periods (or my periods are irregular) so I can’t get pregnant
Myth 2: I am most fertile on day 13/14 of my cycle
Myth 3: You can’t get pregnant the first time you have sex
Myth 4: You can’t get pregnant if you have sex during your period