A rarely seen arrhythmia is the p-wave asystole also mentioned ventricular asystole, ventricular standstill or third-degree atrioventricular block with no ventricular escape rhythm. It is the result of the lack of impulse formation in ventricles (absence of idioventricular automaticity) or the failure of impulse transmission to ventricules (conduction disturbance). Reference Vassalle1 As the name implies, the ventricles stop pumping, resulting in no effective cardiac output during the phenomenon. It is a potentially fatal rhythm disorder and need immediate diagnosis and treatment. We planned to present a case of p-wave asystole, which devoleped after tetralogy of Fallot total correction surgery.
Case report
Three-year old girl, two-dimensional echocardiogram performed tetralogy of Fallot. A large malalignment ventricle septal defect, 50% aortic dextroposition, normal tricuspid and aortic valves, and infundibular, and pulmonary valve stenosis with a maximum gradient of 80 mm Hg were detected. On angiography, both pulmonary arterial branches were confluent and McGoon index was 1.9. Total correction decision was taken at the cardiology and cardiovascular surgery council.
Under general anaesthesia, a median sternotomy was performed. The ventricular septal defect detected after right atriotomy. Ventricle septal defect was closed with an autologous pericardial patch fixed with glutaraldehyde. Then, muscle groups in the right ventricle were resected. It was observed that 13 bougies were not exceeded for the age-appropriate pulmonary valve. A limited ventriculotomy was performed by crossing the pulmonary arteriotomy annulus. The resulting defect was closed with an autologous pericardial patch in accordance with the diameter of the bougie. Warming was initiated while closing the right atriotomy. The aortic cross-clamp was removed after de-airing. Upon observing total AV block in the patient, two ventricular chamber pacemaker leads were placed. The patient was connected to the pacemaker device. After low cardiac output syndrome was observed, the patient was discharged from cardiopulmonary bypass flow, and patient was connected to the ECMO and taken to the ICU. Although the reason for the low cardiac output that developed in the patient is not known, it was thought that the right ventricular restrictive physiology might have developed in the patient. Complete AV block developed during ventricle septal defect closure also worsened the clinic. Steroid was started in the patient whose ventricular rhythm was 60/min in the first 3 days post-operatively. However, it was observed that there was no ventricular rhythm on the post-operative 4th day. In the ECG, p-wave asystole pattern was observed in which the QRS complex did not follow the p-wave (Fig. 1). When we tried to disconnect from the short-term pacemaker, it was seen that the patient could not create blood pressure. After epicardial pacing (Fig. 2), the patient’s normal blood pressure was observed.
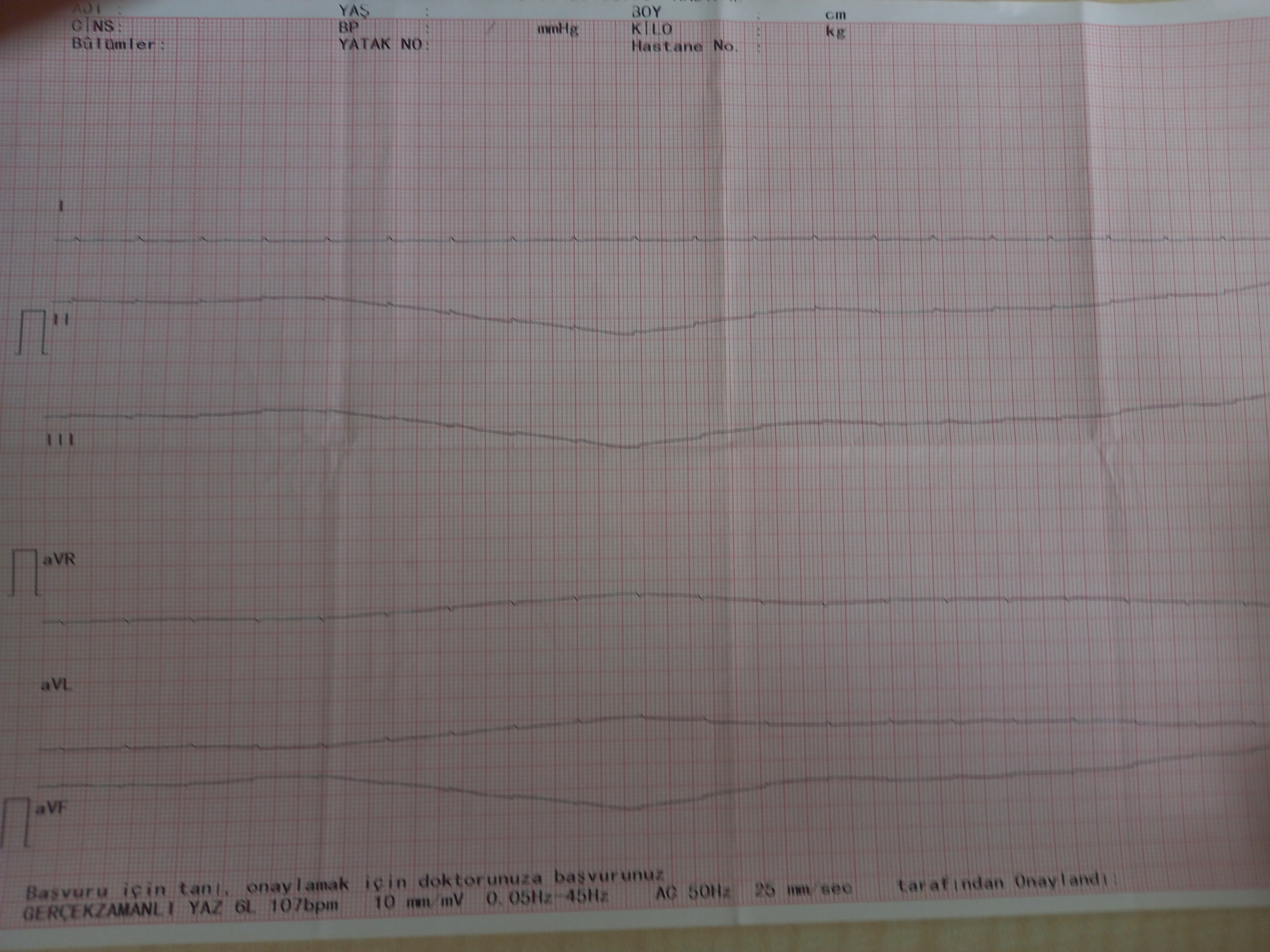
Figure 1. Electrocardiogram demonstrating p-wave asystole.

Figure 2. Epicardial pacemaker rhythm is observed in the ECG.
Discussion
P-wave asystole is a rare phenomenon with an unclear prevalence. The number of studies in child is limited. Studies in adult patient group, of 2333 patients with non-shockable rhythm cardiac arrest, 6,13% have been described to have p-wave asystole as their initial rhythm. Reference Hulleman, Mes, Blom and Koster2 Here, atrial depolarisation is being displayed on the ECG as the only cardiac activity resulting in a patient with no palpable pulses and no consciousness. Although the cause of p-wave asystole is not known exactly, it was thought that p-wave asystole was due to possible ventricular conduction damage in our patient.
Whenever a diagnosis of asystole is made, the ECG should be checked carefully for the presence of p waves because this will likely respond to cardiac pacing. The use of epicardial wires to pace the myocardium following cardiac surgery is effective. Pacing for asystole should not be attempted unless p waves are present; it does not increase short- or long-term survival in or out of hospital. Reference Soar, Böttiger and Carli3
In p-wave asystole, the patient is in clinical arrest. Cardiopulmonary resuscitation should be initiated immediately for acute management. Although it is not an algorithm for treatment approaches, it has been published as case reports and case report reviews. Reference Richason, Paulson, Lowenstein and Heard4,Reference Chan, Reid and Taylor5 Pacing is a well-recognised treatment in asystolic arrest with residual p-wave activity. This can be achieved by transvenous, transthoracic, or manual external (cardiac percussion) pacing techniques. Reference Chan, Reid and Taylor5 In our patient, the haemodynamics of the patient stabilised after epicardial pacing. Since the patient was on ECMO support, clinical arrest did not occur. Temporary pacemakers maybe a bridging therapy. In our patient, since p-wave asystole was observed after surgery, permanent pacemaker was planned for the patient. Our patient could have died due to sudden cardiac arrest if she was not on ECMO support. It should be kept in mind that serious rhythm disorders may develop in the follow-up after the operation.
Acknowledgements
The authors would like to express their sincere gratitude to all members who worked together to provide technical and writing assistance and to the departmental heads for their general support.
Competing interests
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.





