Introduction
Radiotherapy (RT) plays an important role in the management of carcinoma (Ca) breast, which includes irradiation of conserved breast, post mastectomy chest wall and supraclavicular fossa (SCF) nodal region. Reference Whelan, Olivotto and Parulekar1,Reference McGale and Taylor2 Acute oesophagitis (AE) is one of the toxicities that occur during SCF irradiation. Since oesophagus lies in close proximity to the SCF nodes, slightly towards the left from midline, there is a possibility to deliver greater doses of radiation to the oesophagus, which may result in acute radiation oesophagitis. Acute oesophagitis may affect the quality of life of the patient due to pain, difficulty in swallowing food and insufficient nutrition due to modification of diet. A previous study Reference Turkolmez, Atasever and Akmansu3 demonstrated that patients who received RT to the chest wall which included dose to oesophagus, experienced slower oesophageal transit times.
Several methods are described in literature to reduce the radiation dose received by oesophagus, which in turn reduce the severity of acute oesophagitis. Most of these studies are related to thoracic and head and neck radiation. Reference Werner-Wasik, Yorke, Deasy, Nam and Marks4–Reference Emami, Lyman and Brown9 The techniques used to reduce oesophageal dose include oesophagus avoidance by Intensity Modulated Radiotherapy (IMRT), Reference Woodford, Panettieri, Ruben and Senthi10,Reference Granton, Palma and Louie11 oesophagus sparing by simultaneous integrated boost intensity modulated radiotherapy (SIB-IMRT) Reference Ma, Qiu and Li12 and Contralateral Oesophagus-Sparing Technique by IMRT. Reference Al-Halabi, Paetzold and Sharp13
However, there are only limited studies related to the oesophageal dose and oesophagitis in radiotherapy of Ca Breast. Out of the very limited works that are available, West et al. Reference West, Schneider and Wright14 have evaluated the factors influencing acute oesophagitis and Yaney et al. Reference Yaney, Ayan and Pan15 have studied the dosimetric parameters associated with acute esophagitis. The aim of this work is to analyse the effect of oesophagus delineation on the dose received by oesophagus while treating Carcinoma Breast with 3DCRT.
Materials and Methods
Acquisition of clinical data
The study was conducted retrospectively by reviewing the radiation treatment plans of 44 patients (22 right-sided and 22 left-sided breast cancer) who were treated with 3DCRT for Ca Breast in Government T D Medical College, Alappuzha, Kerala, from January 2019 to April 2020. Post mastectomy patients with indications for chest wall and supraclavicular regional node irradiation simulated in straight neck position were included in this study. Patients with enlarged thyroid gland, and patients receiving radiation for conserved breast and post mastectomy chest wall only were excluded. Clearance from institutional review and ethical boards was obtained for this study (number B3/1573A)
Simulation and treatment planning
The patients were simulated on 16 slice Philips Big Bore CT with slice thickness of 2·5 mm. All patients were positioned supine on an angulated breast board with both arms elevated and head and neck in straight position with appropriate head rest. The breast board was angulated to align the chest wall parallel to the surface of the couch. Eclipse Somavision version 11 (Varian Medical Systems, Inc., Palo Alto, CA, USA) was used for contouring, and Eclipse Version 11 treatment planning system (Varian Medical Systems, Inc., Palo Alto, CA, USA) was used to generate the treatment plans for the patients. RTOG breast contouring atlas was followed for delineation of clinical target volume and planning target volume (PTV). Reference White, Arthur and Buchholz16 The OARs routinely contoured included both lungs, contralateral breast, heart and spinal cord. As practiced in a busy clinic with very high patient load, oesophagus was not contoured as OAR. Monoisocentric 3DCRT was used to treat both chest wall and SCF together. Treatment plans (44 numbers) in which oesophagus was not contoured as OAR were considered as group A for the study. The same CT simulation image sets of the 44 patients were used later, with the oesophagus contoured, to generate 3DCRT treatment plans considering oesophagus as an OAR. These set of plans were categorised as Group B. As there is no consensus for oesophagus contouring as OAR in SCF irradiation, oesophagus was delineated using the external oesophageal contour/surface on the mediastinal window on each axial plane of the planning CT scan from caudal border of cricoid cartilage to lower border of supraclavicular PTV.
Hypofractionated dose of 40 Gy in 15 fractions was prescribed to PTV for both chest wall and supraclavicular field irradiation. Reference Bentzen and Agrawal17 The acceptance criteria for the treatment plans were 95% isodose coverage to >95% of PTV. Dose constraints as suggested for hypo fractionation 18 were considered for treatment planning. The second set of plans were generated with oesophagus as OAR. The treatment plans were modified by angulating the SCF beams to avoid the oesophagus as much as possible (an average of 15–17 degrees).
Dosimetric parameters
Dosimetric parameters were acquired from the DVH. The recorded dosimetric parameters included D max and D mean to the oesophagus. Most of the available literature for the study of OAR in radiotherapy for Ca Breast is based on the conventional 2 Gy per fraction. Since the patients in this study were treated with hypo fractionation (2·7 Gy/fraction), biologically equivalent dose in 2Gy per fraction (EQD2) was calculated for D max and D mean to compare the study with the available literature. The percentage of oesophagus volume receiving dose ≥15 Gy (V15), ≥25Gy (V25) and ≥33 Gy (V33) were also recorded. In the comparison of the above-mentioned dose volumetric parameters the plan quality was quantified using the Homogeneity Index (HI) and the Conformity Index (CI). HI was calculated using the formula HI = D 5/D 95 Reference Kataria, Sharma, Subramani, Karrthick and Bisht19 where D 5 is the minimum dose in 5% of PTV indicating maximum dose and D 95 is the minimum dose in 95% of PTV indicating the minimum dose in the plan. The conformity index was calculated using the formula CI = V 95/V PTV where V 95 is the volume of the 95% isodose and V PTV is the volume of the PTV. Reference Feuvret, Noël, Mazeron and Bey20
Since dose to the ipsilateral lung is the major constraint in radiotherapy of Ca breast, the percentage volume of ipsilateral lung receiving doses ≥ 4Gy (V4), ≥8Gy (V8) and ≥16Gy (V16), as suggested in RTOG 1005, 18 was also collected from dose volume histogram (DVH).
Statistical analysis
Data were analysed using statistical package for social studies (SPSS ver.21). Group-wise comparison of all the dosimetric parameters was made using independent t-test. Results were interpreted by using P value ≤0·05 as significant. Difference between two groups was plotted using bar plot.
Results
This retrospective study included treatment plans generated with and without oesophagus delineation for 44 patients of whom 22 had right-sided breast cancer and the remaining 22 had left-sided disease.
Results of statistical analysis of the dose-volumetric parameters are as shown in tables and figures.
Right breast
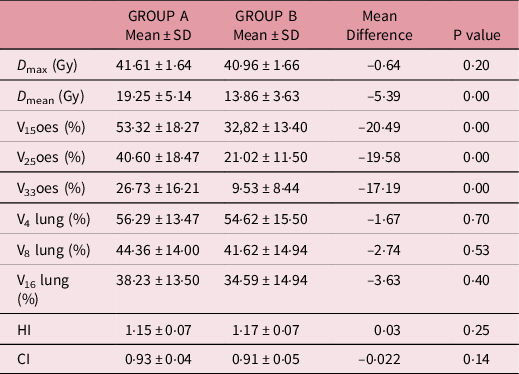
Statistical analysis of the dose volumetric parameters in Group A and Group B for Ca right breast shows that contouring of oesophagus reduces the D mean to oesophagus, as shown in Table 1 and Figure 1. The difference is statistically significant with P ≤ 0·05, favouring oesophageal delineation. Ipsilateral lung volume parameters V 4, V 8 and V 16 are different among the two groups with slightly higher values in Group B, but the difference is not statistically significant. The CI is approximately equal to 0·9 in all the cases with statistically non-significant difference between Group A and Group B (P ≥ 0·05.)
Table 1. Comparison of dosimetric parameters between groups A and B in right-sided plans

SD, standard deviation.

Figure 1. Comparison between group B and group A in Ca right breast plans.
Left breast
Table 2 and Figure 2 give the dose volumetric parameters for treatment plans for Ca left breast. D mean, V 15, V 25 and V 33 are significantly less in Group B favouring oesophageal delineation (P ≤ 0·05). The differences in lung volume parameters, even though slightly higher in Group A, are not statistically significant. The mean difference between HI of the two groups is 0·03 with P ≥ 0·05.
Table 2. Comparison of dosimetric parameters between groups A and B in left-sided plans
SD, standard deviation.
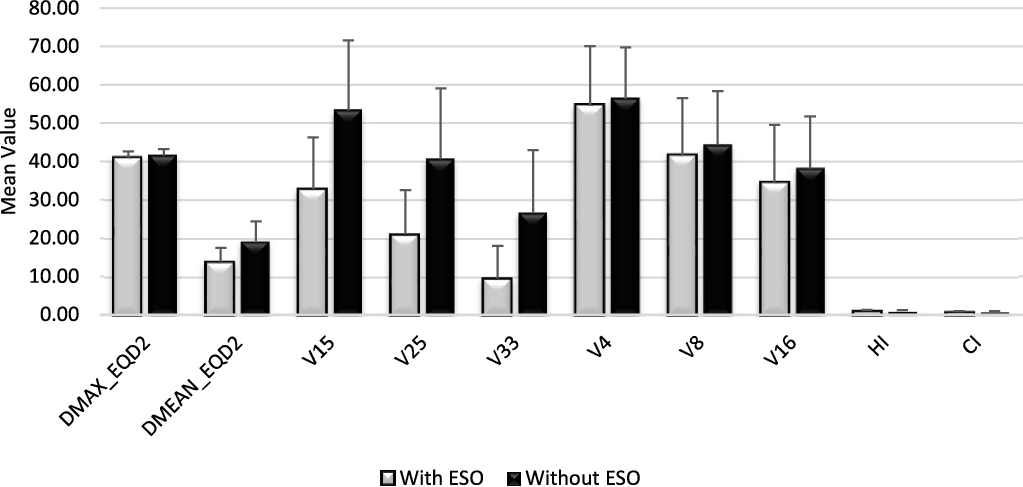
Figure 2. Comparison between group B and group A in Ca left breast plans.
Right breast versus left breast
Table 3 and Figure 3 and 4 show a comparison of the dose volumetric parameters of oesophagus and ipsilateral lung for Ca right breast cases with that of Ca left breast. As is evident from Table 3, the D mean and the volumetric parameters for oesophagus are higher in the Ca left breast patients for both groups with a P value ≤0·05. The plan quality is comparable in both right-sided and left-sided disease with mean CI > 0·9, the difference being statistically nonsignificant.
Table 3. Comparison of dose volumetric parameters between right- and left-sided plans for group A and group B.

SD, standard deviation.

Figure 3. Comparison of Ca left breast and Ca right breast plans in group A.

Figure 4. Comparison of Ca left breast and Ca right breast plans in group B.
Discussion
With the introduction of sophisticated radiation delivery equipment and techniques, the concept of sparing OAR as much as possible has gained importance. Majority of studies about acute radiation oesophagitis are related to lung cancer treatment, and only limited studies are available with regard to Ca Breast. It has been proven in these studies that acute oesophageal toxicity depends on various oesophageal dose volume parameters including D mean. Reference Yaney, Ayan and Pan15 In one of the studies, Li Ma et al. Reference Ma, Qiu and Li12 retrospectively reviewed records of 87 lung cancer patients treated by SIB-IMRT. D mean of oesophagus in their study was significantly less in oesophagus sparing group and patients had statistically significant lower incidence of Grade3 Radiation Oesophagitis (G3RE) in the oesophagus sparing group. Hani Al-Halabi et al. Reference Al-Halabi, Paetzold and Sharp13 in their study of radiation treatment of lung malignancy contoured the cross-sectional half of oesophagus opposite to the gross tumour as avoidance. Contralateral oesophagus sparing had more favourable dosimetry in comparison with the whole oesophagus, showing effective oesophagus cross-section sparing. The median total radiation dose was 70·2Gy. Despite the high total doses used in this study, there were no cases of severe AE (G3) and less incidence of grades 1 and 2 oesophageal toxicities.
Relevant studies related to this study are of West et al. Reference West, Schneider and Wright14 and Alexander Yaney et al. Reference Yaney, Ayan and Pan15 Both have evaluated the dosimetric parameters associated with radiation-induced oesophagitis in Ca breast patients undergoing regional nodal irradiation (RNI). In both the aforementioned studies, dose prescribed was 50 Gy in 25 fractions. To the best of our knowledge, this is the first study in which hypo fractionated dose of 40 Gy in 15 fractions has been prescribed.
West et al. using IMRT found an average mean dose (±SD) of 32·87 Gy (±7·4 Gy) to the oesophagus for patients who underwent SCF treatment. The mean dose to the oesophagus for right sided disease was 28·9 Gy (±6·59 Gy) and for Ca left breast was 38 Gy (±6·03 Gy). On comparison of the left versus right breast, they found that left-sided treatment reported a higher frequency of G2RE. However, this was not statistically significant. They found an overall mean dose to oesophagus of ≥31 Gy which was associated with increased frequency of G2RE. In our study, the Dmean EQD2 oesophagus is 11·11 Gy (±4·27). The reason for the higher dose in IMRT as compared to this study, which used 3DCRT for treatment planning, may be because, in IMRT efforts are taken to achieve the set constraints only.
Alexander Yaney et al. Reference Yaney, Ayan and Pan15 compared oesophageal dose volume parameters in IMRT vs. 3DCRT plans retrospectively. Their results show that >15% of patients receiving RNI with IMRT develop G2RE. Using normal tissue complication probability (NTCP) modelling, they found that the most robust constraints related to acute radiation oesophagitis were oesophageal mean dose < 11 Gy, V10 < 30% and V20 < 15 %. In contrast to the 31% G2RE rate by West et al., their study shows 16% G2RE.
In this study, the D mean EQD2 oesophagus is 8·36 Gy (±2·89) for right-sided disease and 13·86 Gy (±3·63) for patients with Ca left breast in oesophagus contoured group (group B) in contrast to 14·11 Gy (± 4·24) for Ca right breast and 19·25 Gy (±5·14) for Ca left Breast in group A. The differences between D mean of Group A and Group B are statistically significant with P ≤ 0·05. The average D mean is 11·11Gy in oesophagus contoured group (irrespective of side) which is comparable to the robust constraint proposed by Alexander Yaney et al. using biological modelling. This suggests that oesophagus contouring helps in the reduction of mean dose to oesophagus. Our study is retrospective and hence clinical correlation with the occurrence of acute esophagitis has not been evaluated. Since many of our patients complain of esophagitis, further prospective studies have to be conducted by contouring oesophagus as an OAR to analyse the adequacy of the constraint prescribed by Alexander Yaney et al. amongst the population of Kerala, India.
To achieve the required coverage of the PTV while sparing the oesophagus, the SCF beams were angulated 5 to 7 degrees more as compared to the plans without oesophagus contouring. However, this did not have any statistically significant effect on the Ipsilateral lung dose (volume of ipsilateral lung receiving ≥4 Gy (V4), ≥8 Gy (V8) and ≥16 Gy (V16)). The HI and CI are also comparable in Group A and Group B with the difference in HI not exceeding 0·03 and P ≥ 0·05. This proves that to spare the oesophagus, the changes brought to the treatment plans did not reduce the dose homogeneity or introduce any additional hot in the PTV.
As is evident from Table 3, the oesophagus receives higher D mean when the disease is left sided. This is because the oesophagus is inclined to the left as far as the root of the neck after which it gradually returns to median plane near the fifth thoracic vertebra. 21 Hence, the angulation given to the SCF beam is not sufficient to spare the oesophagus as much as in Ca right breast cases.
These results indicate the necessity of contouring oesophagus in Ca breast RT and also the effectiveness of contouring in reduction of oesophageal dose during RT. However, since there are no available guidelines regarding dose constraints for oesophagus in Ca breast RT, the dose volumetric parameters analysed in this paper for oesophagus are based on the limited papers available. Prospective studies with larger sample size will be required to further assess and arrive at the constraints for oesophagus as an OAR in Ca breast RT.
Conclusion
Oesophagitis depends on mean dose received by oesophagus. Contouring of oesophagus and 3DCRT planning can reduce the mean dose received by the oesophagus without significantly affecting ipsilateral lung dose and the plan quality. Hence, contouring of oesophagus is preferable in RNI in ca breast to decrease the mean dose to oesophagus and thus improve the quality of life of the patients.
Acknowledgements
The authors thank Prof. Dr P L Rema Head of Department of Radiotherapy, Government TD Medical College Alappuzha.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
The authors declare none.










