Today's workplaces are increasingly demanding. Organizations are expected to be innovative, provide fast and high-quality service to clients, and be transparent and accountable in their activities. These expectations are as relevant for the not-for-profit and public sectors (e.g., healthcare) as they are for commercial firms. In response to these pressures, cross-functional teams have become highly sought after as a way to increase innovation (McDonough, Reference McDonough2000), support change management initiatives (Piercy, Phillips, & Lewis, Reference Piercy, Phillips and Lewis2013), and enhance overall performance (Sparrowe, Liden, Wayne, & Kraimer, Reference Sparrowe, Liden, Wayne and Kraimer2001).
Cross-functional teams are especially present in the healthcare sector (De Janasz, Dowd, & Schneider, Reference De Janasz, Dowd and Schneider2018; Mercer, Haddon, & Loughlin, Reference Mercer, Haddon and Loughlin2018; Trastek, Hamilton, & Niles, Reference Trastek, Hamilton and Niles2014). With the growing emphasis on inter-professional collaboration in healthcare delivery (Weiss, Tilin, & Morgan, Reference Weiss, Tilin and Morgan2016), cross-functional teams comprised of clinicians such as registered nurses (RNs) and licensed practical nurses (LPNs), as well as non-clinical staff, are an inherently important part of work relationships (Sales, Estabrooks, & Valente, Reference Sales, Estabrooks and Valente2010). Cott (Reference Cott1997) details various environmental, organizational, and occupational factors, including the consolidation of medical power based on professional knowledge and the bureaucratization of hospitals into complex organizations, which have resulted in healthcare delivery being organized predominantly in teams. These teams must work collaboratively to meet patient needs, often in complex environments (Katzenbach & Smith, Reference Katzenbach and Smith1994). In fact Mitchell, Parker, Giles, and Boyle (Reference Mitchell, Parker, Giles and Boyle2014) found evidence that healthcare teams are often more complex than non-medical ones given their distinct cultures within professions, scopes of practices, and the interrelationships between professions, suggesting that they are a particularly useful research subject for increasing understanding of cross-functional team dynamics more broadly (Wagner, Reference Wagner2000).
The inherent complexity of the healthcare sector along with the increased pressure to work collaboratively (Mitchell et al., Reference Mitchell, Parker, Giles and Boyle2014) has prompted research attention toward understanding how leaders can enable teamwork effectively in this increasingly inter-professional environment (Mathieu, Maynard, Rapp, & Gilson, Reference Mathieu, Maynard, Rapp and Gilson2008; Mitchell, Boyle, Parker, Giles, Chiang, & Joyce, Reference Mitchell, Boyle, Parker, Giles, Chiang and Joyce2015). Leadership in team contexts can have major impact on whether the group is able to work effectively to meet its goals (Mitchell et al., Reference Mitchell, Boyle, Parker, Giles, Chiang and Joyce2015). Where formal leaders are present, they can influence team dynamics and resource allocations. For example, Boies, Fiset, and Gill (Reference Boies, Fiset and Gill2015) found that leadership influences outcomes through overall communications (e.g., knowledge sharing) among teammates. Perhaps even more so in healthcare settings, leaders need to be able to navigate effectively the challenges of competing views and perspectives and to steer decision-making and other team processes (D'aunno, Hearld, & Alexander, Reference D'aunno, Hearld and Alexander2019). Where formal leaders are not present and/or ineffective, power dynamics based on perceived legitimacy and bureaucracy can dominate, the groups can stall and become unable to make the decisions needed to move forward, or to resolve tensions among members (Cott, Reference Cott1997; Katzenbach & Smith, Reference Katzenbach and Smith1994; Mitchell et al., Reference Mitchell, Boyle, Parker, Giles, Chiang and Joyce2015).
Our study contributes to this important research on the role of leadership in healthcare teams by exploring formal decentralized leadership (i.e., leadership residing in close proximity to teams rather than teams being centrally controlled by managers high up in the organizational hierarchy [Tannenbaum, Mathieu, Salas, & Cohen, Reference Tannenbaum, Mathieu, Salas and Cohen2012]). We investigate whether and how this formal decentralized leadership influences resource exchange in cross-functional healthcare teams. We focus on the exchange of ‘positive’ resources (i.e., resources that enhance team functionality, e.g., knowledge sharing) and ‘negative’ resources (i.e., resources that inhibit team functionality, e.g., work hindrance behaviors), given that both are essential to a culture of quality in the healthcare sector (Joint Commission, 2008; Meltzer et al., Reference Meltzer, Chung, Khalili, Marlow, Arora, Schumock and Burt2010; Wagner, Reference Wagner2000). Understanding how formal decentralized leadership influences these kinds of exchanges is particularly helpful in addressing the unresolved problems associated with team collaboration currently plaguing the healthcare sector due to healthcare professionals having a tendency to operate in uni-professional silos (Ferlie, Fitzgerald, Wood, & Hawkins, Reference Ferlie, Fitzgerald, Wood and Hawkins2005).
Furthermore, given the recent trends in healthcare toward flatter and more decentralized structures (Embertson, Reference Embertson2006; De Janasz et al., Reference De Janasz, Dowd and Schneider2018; Yeatts & Seward, Reference Yeatts and Seward2000), studying the impact of decentralized leadership in this context is particularly timely. As De Janasz, Dowd, and Schneider (Reference De Janasz, Dowd and Schneider2018) noted, ‘healthcare management is steadily moving away from the hierarchical structure and traditionally independent practices of the past toward a culture of teamwork’ (p. 238). At the same time the concept of self-managed (and empowered) teams, whereby healthcare teams operate at arm's length from their centralized managers (Yeatts & Seward, Reference Yeatts and Seward2000), often as a result of the organization's elimination of its middle managers (Embertson, Reference Embertson2006), has become increasingly prevalent. Despite this, there is still much debate as to whether these teams might still benefit from having access to a formal decentralized leader to support their efforts (Belasen & Belasen, Reference Belasen and Belasen2016; Robbins & Davidhizar, Reference Robbins and Davidhizar2007).
To accomplish our research objectives we used the social network approach (SNA). This methodology involves the mapping and measuring of relationships and flows among actors in a network (Borgatti, Everett, & Johnson, Reference Borgatti, Everett and Johnson2013). This approach is well-suited for our research aims given its usefulness in understanding how resources such as knowledge and work hindrance behaviors are exchanged among individuals in teams as well as the role of formal leaders in this process (Serrat, Reference Serrat2017).
The remainder of the paper is structured as follows: first, we present our theoretical framework and associated hypotheses. Next, our ‘Method’ section outlines details of our research design and SNA, research context, participants and procedures, and survey measures. This section is followed by our quantitative results, as well as findings from a series of follow-up interviews. Final sections include the discussion, limitations of the study, practical implications, suggestions for future research, and our conclusion.
Theoretical background and research framework
Empowerment, delayering, and decentralized leadership
Tannenbaum et al. (Reference Tannenbaum, Mathieu, Salas and Cohen2012) highlighted three significant changes affecting teams in organizations, one of which is empowerment or the ‘pushing of authority and governance down the organizational hierarchy, from central control outside the team to team leader control of the team to team self-control’ (p. 15). Despite the many reported benefits of adopting these new types of ‘empowered’ work structures (De Janasz et al., Reference De Janasz, Dowd and Schneider2018), challenges still arise. One such challenge, referred to as the ‘dark side’ of empowerment, is often observed in those instances where organizations are delayered, management ranks are thinned, and team members are subsequently required to assume too much responsibility, leading to a high degree of cynicism, lack of motivation, and inhibited teamwork (Marks & De Meuse, Reference Marks, De Meuse, Marks and Meuse2003; Silver, Randolph, & Seibert, Reference Silver, Randolph and Seibert2006). This type of situation is where the inclusion of a formal decentralized leader could offer value. Formal decentralized leaders work closely with teams for the purpose of guiding, coaching, and enabling their members (De Janasz et al., Reference De Janasz, Dowd and Schneider2018). These leaders are also responsible for providing teams with the resources necessary to perform their jobs effectively while also serving as liaisons between team members and upper management on important team matters (Hempel, Zhang, & Han, Reference Hempel, Zhang and Han2012; Mehra, Smith, Dixon, & Robertson, Reference Mehra, Smith, Dixon and Robertson2006; Wong, Ormiston, & Tetlock, Reference Wong, Ormiston and Tetlock2011). Thus, formal decentralized leaders provide team members with an additional layer of support when compared to those who report solely to a centralized manager. Belasen & Belasen (Reference Belasen and Belasen2016), Engle, Lopez, Gormley, Chan, Charns, and Lukas (Reference Engle, Lopez, Gormley, Chan, Charns and Lukas2017), and Birken, Lee, and Weiner (Reference Birken, Lee and Weiner2012) argue that decentralized leaders can be a vital resource for healthcare organizations by providing their teams with much needed resources and support. Due to their unique role in teams, formal decentralized leaders are in an ideal position to enhance positive resource exchanges (e.g., knowledge sharing) and to safeguard against negative resource exchanges (e.g., work hindrance behaviors) within teams. In the next section, we draw upon social exchange theory (SET) to explain this relationship further.
Social exchange theory
SET proposes that social behavior is the result of voluntary exchanges of resources between two or more actors (Homans, Reference Homans1958). These resources can be tangible (e.g., exchange of money), impersonal (e.g., transfer of knowledge), or socio-emotional (e.g., exchange of social support or trust; Aselage & Eisenberger, Reference Aselage and Eisenberger2003). A social exchange rests on the ‘norm of reciprocity’ (Blau, Reference Blau1964), in which obligations to reciprocate good faith behavior are evoked by ‘exchanges of benefits and favors among individuals’ (Graen, Reference Graen2003: 189). In his formative work on SET, Lévi-Strauss (Reference Lévi-Strauss1969) classified social exchanges into two broad categories: restricted (symmetric) and generalized (asymmetric). A symmetric exchange involves only two actors, where the first actor (e.g., a decentralized leader) gives resources to a second actor (e.g., a team member), who then gives resources back to the first actor (e.g., the decentralized leader). In contrast, a generalized or asymmetric exchange involves indirect reciprocity between three or more individuals. For example, one person (e.g., a decentralized leader) gives resources to another individual (e.g., a team member), who then gives to a third individual (e.g., another team member). In team contexts, generalized social exchanges are particularly important due to the benefits that extend beyond the dyadic leader–subordinate relationship and to the team as a whole instead (Lazega & Pattison, Reference Lazega and Pattison1999; Molm, Collett, & Schaefer, Reference Molm, Collett and Schaefer2007; Robert, Dennis, & Ahuja, Reference Robert, Dennis and Ahuja2008). Generalized social exchanges can lead to improved team functionality and performance by enhancing the team's overall access to resources (Farmer, Van Dyne, & Kamdar, Reference Farmer, Van Dyne and Kamdar2015; Zhao, Reference Zhao2015). Our study focuses on the role of decentralized leadership on the exchange of knowledge and work hindrance behaviors within healthcare teams. We begin with a discussion of knowledge sharing.
Positive resource exchanges – knowledge sharing
Knowledge sharing is the process by which work-related information, skills, and expertise held by an individual is converted into a form that can be understood, absorbed, and used by other individuals (Ipe, Reference Ipe2003). In our study, we are most interested in teams' access to tacit knowledge that improves organizational learning and capacity for problem-solving (Leonard & Sensiper, Reference Leonard and Sensiper1998). Knowledge sharing is considered a ‘positive’ resource exchange due to the many favorable performance-based outcomes that have been found to be associated with this behavior. For example, in their meta-analysis on the relationship among information sharing, team performance, cohesion, decision satisfaction, and knowledge integration, the authors found knowledge sharing to predict each outcome positively across all levels of moderators considered in the study (Mesmer-Magnus & DeChurch, Reference Mesmer-Magnus and DeChurch2009). The positive effects of knowledge sharing have also been documented in the healthcare literature, whereby knowledge sharing has been found to be associated with high-quality health services (Joint Commission, 2008; Meltzer et al., Reference Meltzer, Chung, Khalili, Marlow, Arora, Schumock and Burt2010; Wagner, Reference Wagner2000).
Prior research has found that leaders play a key role in influencing positive resource exchanges such as knowledge sharing within teams (Balkundi & Kilduff, Reference Balkundi and Kilduff2006; Boies, Fiset, & Gill, Reference Boies, Fiset and Gill2015). These effects can be explained by the underlying logic of SET discussed earlier, whereby leaders provide resources to their teams, which then generates a felt obligation on the part of team members to reciprocate the exchange of positive resources to the rest of their team in the form of generalized exchanges (Settoon, Bennett, & Liden, Reference Settoon, Bennett and Liden1996). This pattern of resource exchanges triggered by the leader enhances the team's overall access to resources and ultimately its performance potential.
As discussed earlier, formal decentralized leaders are in a better position than centralized managers to be able to provide team members with resources due to their close proximity to teams and emphasis on coaching and other supportive behaviors (Hempel, Zhang, & Han, Reference Hempel, Zhang and Han2012; Mehra et al., Reference Mehra, Smith, Dixon and Robertson2006; Wong, Ormiston, & Tetlock, Reference Wong, Ormiston and Tetlock2011). We can therefore assume that team members that have a decentralized leader formally assigned to their team are more likely to have access to positive resources than those who do not. Drawing from SET tenets, we suggest that this outcome will generate a feeling of obligation in these team members to engage in more positive generalized social exchanges (i.e., knowledge sharing). As such, we hypothesize the following:
Hypothesis 1: Team members with a decentralized leader formally assigned to their team will engage in more positive resource exchanges (i.e., knowledge sharing) than those who report only to a centralized manager.
Negative resource exchanges – work hindrance behaviors
Along with positive resource exchanges, the exchange of negative resources, referred to as work hindrance behaviors, has also sparked interest in the literature, particularly when adopting a social network perspective (Sparrowe et al., Reference Sparrowe, Liden, Wayne and Kraimer2001). Work hindrance behaviors refer to resource exchanges that thwart, inhibit, and/or hinder team functionality (Sparrowe et al., Reference Sparrowe, Liden, Wayne and Kraimer2001). They include negative team behaviors such as interference, threats, sabotage, and rejection (Sahlins, Reference Sahlins1972). They also involve negative emotional responses to these behaviors, including annoyance, being upset, and feelings of anger (Pagel, Erdly, & Becker, Reference Pagel, Erdly and Becker1987). In our paper, we define work hindrance behaviors as ‘behaviors that make it difficult for team members to carry out their job responsibilities’ (see ‘Method’ section for further details on the measurement of this behavior). Prior healthcare studies have found collaboration across cross-functional healthcare teams to be highly problematic leading to negative outcomes such as friction, hostility, and poor performance (Atwal & Caldwell, Reference Atwal and Caldwell2005; Caldwell & Atwal, Reference Caldwell and Atwal2003). This has prompted a call for more research on understanding how to safeguard against work hindrance behaviors (Ferlie et al., Reference Ferlie, Fitzgerald, Wood and Hawkins2005; Mitchell et al., Reference Mitchell, Boyle, Parker, Giles, Chiang and Joyce2015) such as through the influence of a formal decentralized leader. The interest in work hindrance behaviors is also prompted by the arguments made in the literature that negative exchanges are often times more predictive of team outcomes than positive ones (Sparrowe et al., Reference Sparrowe, Liden, Wayne and Kraimer2001).
Drawing from the arguments presented in the previous section, we assume that team members who have a decentralized leader formally assigned to their team are less likely to engage in negative behaviors due to the added support received from these leaders. According to SET, this type of leadership will lead to a sense of obligation in team members to refrain from engaging in negative generalized exchanges (e.g., work hindrance behaviors). Mitchell et al. (Reference Mitchell, Boyle, Parker, Giles, Chiang and Joyce2015) support this argument in their study on the effects of inclusive leadership on status differences in healthcare teams in which they found negative team behaviors to be alleviated when the teams had the added support of their leader. Therefore, we hypothesize the following:
Hypothesis 2: Team members with a decentralized leader formally assigned to their team will engage in fewer negative resource exchanges (i.e., work hindrance behaviors) than those who report only to a centralized manager.
The moderating effects of leader–member relationship quality
Although the mere presence of a decentralized leader is likely to influence resource exchanges positively within healthcare teams, the contingency model of leadership (Jones & George, Reference Jones and George2014) suggests that there are certain situational factors that might influence whether these positive effects can be realized. The situational factor on which our study focuses on is the relationship quality between leaders/managers and their team members, referred to as the leader–member exchange (LMX). First proposed by Graen and colleagues (Dansereau, Graen, & Haga, Reference Dansereau, Graen and Haga1975; Graen, Dansereau, Minami, & Cashman, Reference Graen, Dansereau, Minami and Cashman1973), LMX is a multi-level relationship-based approach to leadership. It is distinct from other traditional leadership theories in that it focuses on the dyadic relationship between a leader (or manager) and a follower (Gerstner & Day, Reference Gerstner and Day1997). Rooted in SET (Herdman, Yang, & Arthur, Reference Herdman, Yang and Arthur2017), LMX theory contends that subordinates reciprocate high-quality relationships from leaders, and that relationships and roles are negotiated over time through a series of interactions or exchanges (Ilies, Nahrgang, & Morgeson, Reference Ilies, Nahrgang and Morgeson2007).
Prior studies have uncovered various factors that lead to positive exchange relationships, among which leadership behavior and the resulting relationship quality with subordinates is particularly important. For example, in a recent meta-analysis of the antecedents and consequences of LMX, Dulebohn, Bommer, Liden, Brouer, and Ferris (Reference Dulebohn, Bommer, Liden, Brouer and Ferris2012) found that when leaders engage in supportive behaviors it signals to followers that they are willing to put extra effort into the relationship. In return, followers reciprocate the effort, leading to positive outcomes such as enhanced commitment to the supervisor and the enactment of organizational citizenship behaviors (OCBs; Walumbwa, Cropanzano, & Goldman, Reference Walumbwa, Cropanzano and Goldman2011). OCBs refer to innovative and spontaneous actions by employees that exceed job requirements and may include behaviors such as knowledge sharing or other forms of cooperative team behaviors (Ford, Myrden, & Jones, Reference Ford, Myrden and Jones2015), all of which can impact performance positively (Ilies, Nahrgang, & Morgeson, Reference Ilies, Nahrgang and Morgeson2007). Lapierre (Reference Lapierre2007) found that when managers demonstrated benevolence toward their employees it contributed to reciprocated exchanges in the form of employees performing extra-role efforts for their supervisor. Similarly, a study conducted by Yun, Pearce, and Sims (Reference Yun, Pearce and Sims2000) reported evidence of positive generalized exchanges taking place among coworkers in response to leaders' supportive behaviors. Omar, Zainal, Omar, and Khairudin (Reference Omar, Zainal, Omar and Khairudin2009) extended this concept to the study of self-managed teams, finding that leaders' supportive and individually considerate behavior had a positive influence on the social exchanges and behaviors of self-managed teams.
Arguments have also been made in the healthcare literature for the importance of leaders fostering high-quality leader–follower relationships (Hanse, Harlin, Jarebrant, Ulin, & Winkel, Reference Hanse, Harlin, Jarebrant, Ulin and Winkel2016). For example, Laschinger, Purdy, and Almost (Reference Laschinger, Purdy and Almost2007) found that high-quality (LMX) relationships with nurse managers and their immediate supervisors were positively related to empowerment and job satisfaction. Chen, Wang, Chang, and Hu (Reference Chen, Wang, Chang and Hu2008) showed that high-quality (LMX) relationships between nurses and their supervisors increased nurses' commitment and promoted OCBs. We expect that LMX will also play a role in the extent to which a formal decentralized leader is able to influence positive resource exchanges within healthcare teams. Specifically, we hypothesize:
Hypothesis 3: LMX will positively moderate the relationship between formal decentralized leadership and positive resource exchanges such that team members with decentralized leaders formally assigned to their team will be even more likely to engage in knowledge sharing when team members' report a high-quality LMX relationship.
Along with the influence of LMX on positive resource exchanges, prior research also suggests that LMX might affect the extent to which leaders can safeguard against negative resource exchanges (i.e., work hindrance behaviors) within teams. Although the research in this area is limited, work group diversity literature has been found that when leaders foster high-quality relationships with their team members through the enactment of ‘supportive’ transformational leadership and/or empowering leadership behaviors they are able to alleviate certain negative team behaviors such as social categorization/intergroup biases and knowledge hoarding (Kearney & Gebert, Reference Kearney and Gebert2009; Scheuer, Reference Scheuer2017). Research on turnover in the healthcare literature also suggests that LMX might help to safeguard against work hindrance behaviors since turnover is often associated with negative team experiences. For example, Chen et al. (Reference Chen, Wang, Chang and Hu2008) showed that high-quality (LMX) relationships between nurses and their supervisors lessened turnover and instead promoted positive team behaviors such as OCBs. Han and Jekel (Reference Han and Jekel2011) demonstrated a mediating effect of job satisfaction on the relationship between LMX and turnover intentions. Trybou, De Pourcq, Paeshuyse, and Gemmel (Reference Trybou, De Pourcq, Paeshuyse and Gemmel2014) similarly found LMX among nurses and nursing assistants to impact turnover intentions as well as other retention-related outcomes. We therefore hypothesize:
Hypothesis 4: LMX will negatively moderate the relationship between formal decentralized leadership and negative resource exchanges, such that team members with decentralized leaders formally assigned to their team will be even less likely to engage in work hindrance behaviors when team members' report a high-quality LMX relationship.
Figure 1 provides a summary of the hypotheses outlined in our theoretical framework.
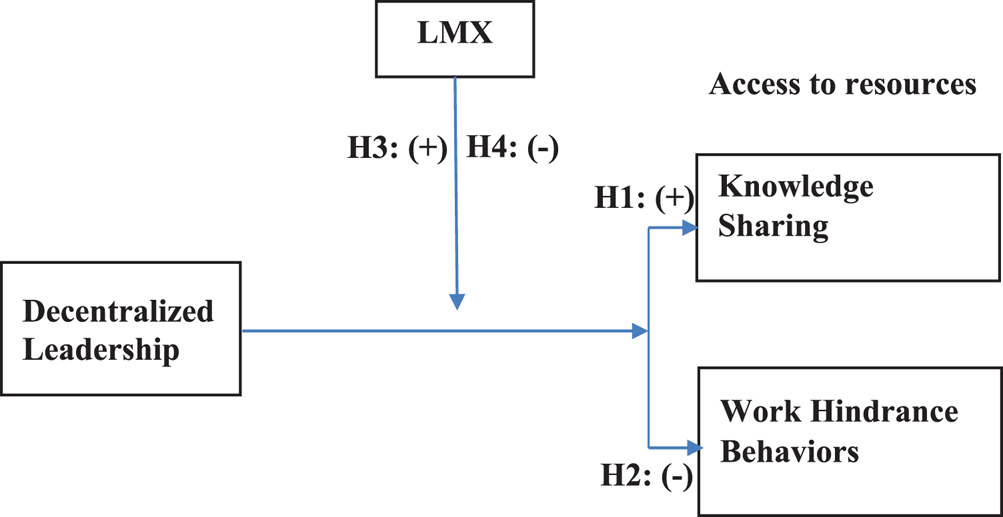
Fig. 1. Research model.
Method
Research design and approach
We adopted an explanatory sequential mixed method design (Cresswell, Reference Cresswell2003), consisting of two-phases – a quantitative phase, in which survey data were collected and analyzed according to our stated hypotheses, and a qualitative phase involving interviews, which were intended to provide more insight into our quantitative results. For the quantitative phase, we drew upon the SNA (Freeman, Reference Freeman2004; Scott, Reference Scott1988; Wellman, Reference Wellman1983). The SNA offers a wide array of theories, methods, and analytical tools for understanding, describing, and explaining patterns of relationships (e.g., resource exchanges) among actors (e.g., team members) in a given network (Scott & Carrington, Reference Scott and Carrington2011; Wasserman & Faust, Reference Wasserman and Faust1994). Given the relational nature of leadership and teams, the SNA is ideal for studying our research topic. As Carter, DeChurch, Braun, and Contractor (Reference Carter, DeChurch, Braun and Contractor2015) noted, the SNA is ‘highly suitable for studying leadership as relational, situated in specific contexts, involving patterned processes, and both formal and/or informal influence’ (p. 599), all of which are characteristics of our study.
Despite the unique strengths of the SNA, the number of team leadership studies that have adopted this methodology is still quite limited (Mendez & Busenbark, Reference Mendez and Busenbark2015). The healthcare context is no exception. According to van Beek, Wagner, Spreeuwenberg, Frijters, Ribbe, and Groenewegen (Reference van Beek, Wagner, Spreeuwenberg, Frijters, Ribbe and Groenewegen2011), studying social networks and team dynamics among healthcare workers has implications for care as well as resource management and therefore is in need of more attention. For example, greater communication flows among team members can have positive effects on the level of support received by dementia patients and other complex cases. Employee satisfaction and team performance can also be affected by knowledge sharing networks (Van Beek et al., Reference van Beek, Wagner, Spreeuwenberg, Frijters, Ribbe and Groenewegen2011). Until recently, the SNA has also been used to study healthcare teams in the for-profit sector. However, healthcare organizations reside both within the for-profit and public sectors. We address these research gaps in our study by examining the effects of formal decentralized leadership on resource exchanges taking place in teams at a publicly-funded long-term care facility in Canada.
Context
Our research is positioned within the long-term care context in Nova Scotia, Canada. Between 1971 and 2011, the median age of Canadians shifted from 26.2 to 39.9 years (Statistics Canada, 2010), making seniors the fastest growing demographic group in the country. This trend, and its concomitant effects, is particularly clear in rural communities, including those in Nova Scotia, where the proportion of seniors is greater than that in urban settings (Myette, 2019). These aging demographics point to the growing importance of long-term care in the health sector (Sales, Estabrooks, & Valente, Reference Sales, Estabrooks and Valente2010; Statistics Canada, 2010; van Beek et al., Reference van Beek, Wagner, Spreeuwenberg, Frijters, Ribbe and Groenewegen2011). From an organizational perspective, resource constraints coupled with increased service needs give rise to questions regarding the best options for delivering effective long-term care solutions for seniors. However, even as demand for high-quality long-term health care increases, it is a relatively understudied area of research (Sales, Estabrooks, & Valente, Reference Sales, Estabrooks and Valente2010), thereby justifying our decision to focus on this context.
Research site
Our research site is a not-for-profit, publicly-funded continuing care facility in rural Nova Scotia, Canada. The innovative element of the facility lies in the fact that it is divided into 10 ‘houses’ – named as such based on the resemblance to a typical home environment in comparison to other, more institutional settings previously found in long-term care facilities. These houses are grouped into four ‘neighborhoods’ – two of which have three houses (27 residents in each) and two of which have two houses (18 residents in each). These neighborhoods are essentially arms of the building where two or three houses are physically located next to each other. All staff members, regardless of position or job status, work in cross-functional teams (comprised of a combination of medical and non-medical staff) within one of four ‘neighborhoods’ in this facility.
Approximately 6 months prior to the initial data collection for this study, this long-term care facility engaged in an ‘empowerment initiative,’ which involved the neighborhoods shifting away from a hierarchical reporting structure and instead operating as self-managed teams. Along with this change came the addition of formal decentralized leaders, which were assigned to two of the four neighborhoods. Those working in the other two neighborhoods continued to report to their respective, centralized managers without the aid of an additional decentralized leader. This initiative provided us the unique opportunity to test our stated research hypotheses in a quasi-experimental setting by comparing resource exchanges in cross-functional health teams with and without a formal decentralized leader.
Participants and procedures
Survey data were collected at two points in time, over a 24-hr period on each visit. The visits were scheduled approximately 2 weeks apart in order to accommodate the turnover of shifts. The total population of our sample was 104 employees, of which 65 employees completed the survey, resulting in a response rate of 63%. Five of the 65 participants completed the survey anonymously. These were excluded from the analysis since participant names were required to match cases and create networks (see ‘Results’ section for further details), resulting in a final sample of 60 team members.
Survey participants represented a variety of professions, ranging from administrative staff (4.3%) and managers (4.3%); direct care providers (RNs and LPNs) (14.4%); support staff (CCAs) (39.1%); and auxiliary service providers (kitchen and dietary staff, laundry staff, recreation staff, facilities management, and other support services) (25.8%). A summary of the participant demographics is presented in Table 1. No significant differences were found in any of these demographic or work history variables across the four neighborhoods, as determined by analysis of variance tests, thereby ruling out the possibility of these factors influencing any differences found across neighborhoods with and without a decentralized leader.
Table 1. Respondent demographics

Note: n = 60.
For the qualitative phase of the study, all survey participants who belonged to a neighborhood with a decentralized leader were invited to participate in follow-up interviews. The intent of these interviews was to gain deeper insights into the impact of the decentralized leaders on the resource exchanges taking place among cross-functional team members (see Appendix A for interview guide). The final sample consisted of four team members. Interviews lasted approximately 45 minutes, were recorded, and transcribed.
Survey measures
Decentralized leadership
As discussed earlier, the presence of formalized decentralized leaders was a ‘naturally occurring’ phenomenon at our research site as part of the facility's ‘empowerment initiative.’ Formal decentralized leaders were allocated to half of the neighborhoods whereas the other half reported to centralized managers. The healthcare director provided us with a list of team members who were allocated a decentralized leader. Following Fox's (Reference Fox1997) dummy coding procedures, team members without a decentralized leader assigned to their team (and who instead reported to a centralized manager) were dummy coded as zero and team members with a decentralized leader assigned to their team were dummy coded as one. This coding allowed us to assess the relationship between the dependent variables in our study and the absence (coded as 0) versus presence (coded as 1) of a given team characteristic (i.e., formal decentralized leadership).
LMX
LMX was measured using Graen and Uhl-Bien's (Reference Graen and Uhl-Bien1995) 7-item scale (sample item: ‘How well does your manager understand your job problems and needs?’). The scale has been well validated in the literature (Gerstner & Day, Reference Gerstner and Day1997; Schriesheim & Gardiner, Reference Schriesheim and Gardiner1992) and had an internal consistency reliability (Cronbach's α) of .92 in the current study. The LMX ratings included staff perspectives regarding their leaders (not vice versa). For the two neighborhoods with a decentralized leader, staff were asked to respond to the LMX items about their decentralized leader. For those without a decentralized leader, staff reported on their respective centralized managers.
Network measures
We included two network measures – knowledge sharing and work hindrance behaviors. To capture knowledge sharing, we asked: ‘Sometimes residents may express a desire to change their preferences and these changes can affect the operations of the entire neighborhood. When such changes occur, who would you share this new information with?’ To measure for work hindrance behaviors, we asked: ‘Among the individuals listed below, please indicate who makes it difficult to carry out your job responsibilities.’ These items were adapted from measures used in prior social network research (Balkundi & Harrison, Reference Balkundi and Harrison2006; Balkundi & Kilduff, Reference Balkundi and Kilduff2006; Sparrowe et al., Reference Sparrowe, Liden, Wayne and Kraimer2001). The wording of the items was also informed by conversations with the nursing home's senior leadership team regarding the kinds of exchanges that typically take place at the facility. Using the widely adopted roster method (Borgatti, Everett, & Johnson, Reference Borgatti, Everett and Johnson2013), participants were asked to report on each team member in their neighborhood for each network measure using a list provided by the organization.
Results
We utilized social network analysis to test our hypotheses. Drawing upon the underlying theory of social networks, social network analysis is one application of Euler's graph theory that visually articulates social actors (i.e., team members) as points on a sociogram and further details their relations (i.e., resource exchanges) as interconnected lines referred to as ties (Scott, Reference Scott2000). Following the procedures of social network analysis, two adjacency matrices (i.e., networks) were developed using the survey data collected from the knowledge sharing and work hindrance behaviors network measures. For each network, we calculated the individual network centralities for each of the 60 participants within their respective neighborhoods using UCINET 6.592 (Borgatti, Everett, & Freeman, Reference Borgatti, Everett and Freeman2002). Network centrality captures the extent to which team members exchange resources with one another via the measurement of ties (Sparrowe et al., Reference Sparrowe, Liden, Wayne and Kraimer2001). Since Freeman's (Reference Freeman1979) degree centrality (measured as the total number of ties reported by a given participant) has been widely accepted as being the most stable measure of ties in a network (Zemljič & Hlebec, Reference Zemljič and Hlebec2005), we utilized this measure in our analysis. As discussed earlier, when responding to the network questions on the survey, participants indicated with which of the team members they would exchange knowledge and/or work hindrance behaviors. Each time a participant listed another team member a tie was formed in that network. We normalized the degree centrality values to account for differences in team sizes across the neighborhoods. This is accomplished by dividing the degree centrality values by the maximum possible degree centrality value (as a result of team size) and is expressed as a ratio with possible values of 0–100 (Borgatti, Everett, & Freeman, Reference Borgatti, Everett and Freeman2002). Descriptive statistics and the correlations (Pearson) for all measures are reported in Table 2.
Table 2. Descriptive statistics and correlations

Note: Decentralized leadership (0 = no decentralized leader assigned to team/team only reports to a centralized leader, 1 = decentralized leader assigned to team); LMX measured 1–5; knowledge sharing and work hindrance degree centrality variables measured 1–100; *p < .05; **p < .01.
Hypothesis testing
Our analyses were conducted using Mplus Version 7.4 (Muthén & Muthén, Reference Muthén and Muthén2014) and were constructed at the individual (team member) level of analysis. We relaxed significance levels to p < .10 for findings involving interactions because the statistical power for detecting moderators in field studies such as this one is inherently low, a recommendation that has been endorsed in prior research (Harrison, Price, & Bell, Reference Harrison, Price and Bell1998; Kearney & Gebert, Reference Kearney and Gebert2009; McClelland & Judd, Reference McClelland and Judd1993).
To test our first two hypotheses, we constructed two regression models. The first tested for the direct effect of decentralized leadership on the knowledge sharing network (Hypothesis 1). The second tested for the direct effect of decentralized leadership on the work hindrance behaviors network (Hypothesis 2). The results indicated that having a decentralized leader was significantly positively related to both the knowledge sharing [β = .31, t(49) = 2.26, p = .03, R 2 = .09], and work hindrance behaviors [β = .35, t(57) = 2.83, p = .006, R 2 = .12] degree centralities. In other words, team members with a decentralized leader formally assigned to their neighborhood were more likely to share knowledge with their colleagues. However, they were also more likely to engage in work hindrance behaviors. Therefore, Hypothesis 1 was supported, whereas Hypothesis 2 was not supported.
Figure 2 provides a visual representation of the knowledge sharing and work hindrance networks for a neighborhood with and without a decentralized leader. The networks were constructed with the assistance of Netdraw, a network visualization program (Borgatti, Reference Borgatti2002). The square nodes in the figures represent the team members. The lines connecting the nodes depict the ‘ties’ (Borgatti, Everett, & Johnson, Reference Borgatti, Everett and Johnson2013) or resource exchanges among team members. For example, in the knowledge sharing network, a tie between two nodes would indicate that knowledge is shared between those two team members. The arrows represent the direction of the exchange (e.g., one-way from Team Member A to Team Member B, one-way from Team Member B to Team Member A, or two-way, whereby both team members exchange resources with one another). As shown in the diagram, there are more ‘ties’ (i.e., resource exchanges) occurring in the knowledge sharing and work hindrance networks in the neighborhood with the decentralized leader than in the neighborhood without one. However, with this latter network representing ‘negative’ resource exchanges, only the knowledge sharing network was a desirable outcome.
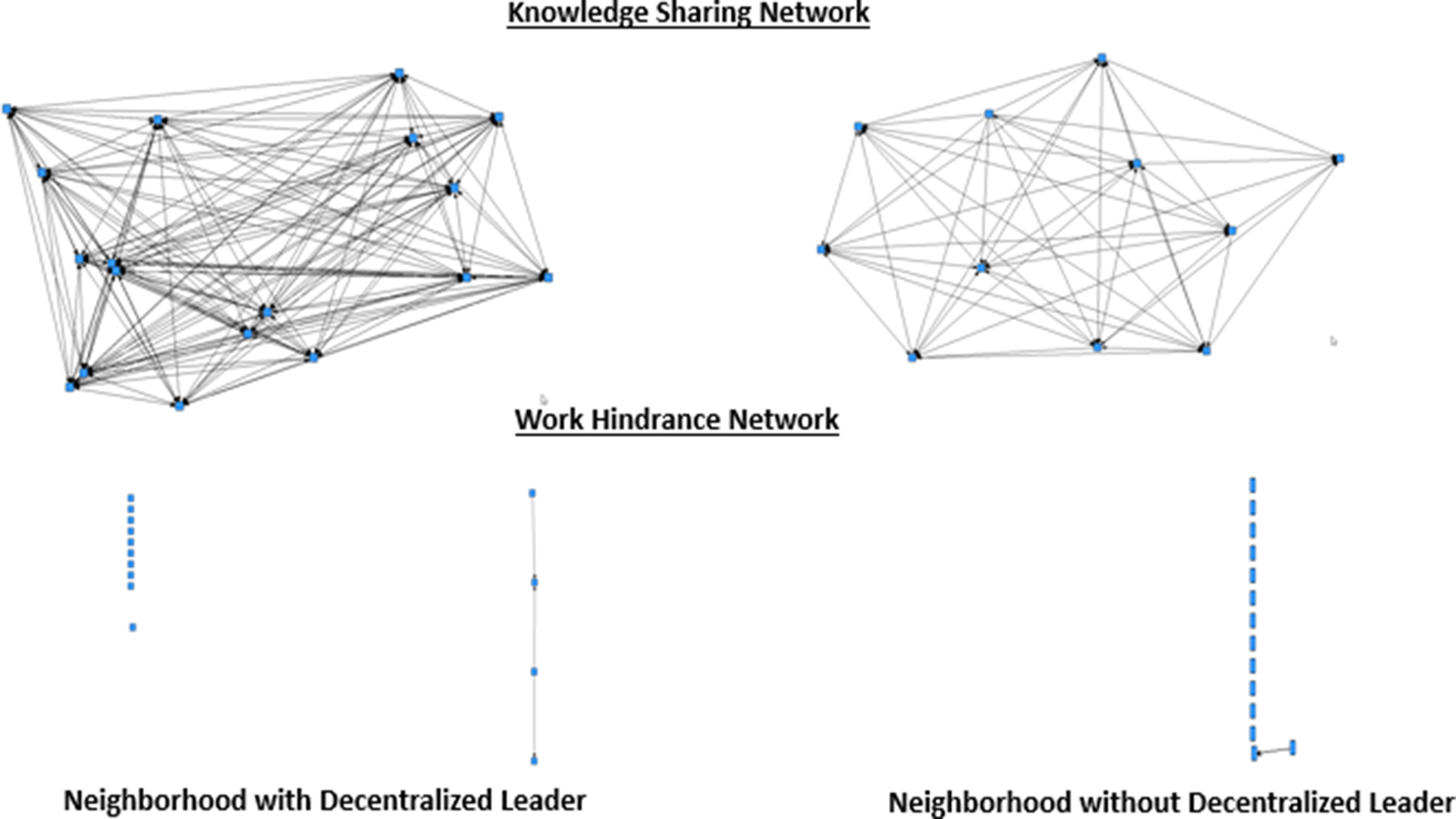
Fig. 2. Visualization of knowledge sharing and work hindrance networks.
To test for Hypotheses 3 and 4, we constructed two moderation models. The first specified the effect of decentralized leadership on the knowledge sharing network, the effect of LMX on the knowledge sharing network, and the effect of the interaction term between decentralized leadership and LMX on the knowledge sharing network. The second specified the effect of decentralized leadership on the work hindrance behaviors network, the effect of LMX on the work hindrance behaviors network, and the effect of the interaction term between decentralized leadership and LMX on the work hindrance behaviors network. LMX was mean centered prior to computing the interaction term for each model (Aiken, West, & Reno, Reference Aiken, West and Reno1991).
Although the interaction between decentralized leadership and LMX on the knowledge sharing network was not statistically significant, the results of simple slope analysis, which involved testing the interaction at conditional values one standard deviation above and below the mean of LMX (Aiken, West, & Reno, Reference Aiken, West and Reno1991), did offer some support for Hypothesis 3. As expected, at high levels of LMX, decentralized team leadership was moderately significantly positively related to knowledge sharing network degree centralities (b = 16.75, p = .05). By contrast, when LMX was low, decentralized team leadership was not significantly positively related to knowledge sharing network degree centralities (b = 11.91, p = .16).
The interaction between decentralized leadership and LMX on the work hindrance network was significant and in the predicted (negative) direction (b = −.33, p = .06, R 2 = .21). Simple slope analyses (Aiken, West, & Reno, Reference Aiken, West and Reno1991) revealed that at high levels of LMX, decentralized leadership was not significantly related to work hindrance behaviors degree centralities (b = 1.7, p = .47). By contrast when LMX was low, decentralized team leadership was significantly positively related to work hindrance behaviors degree centralities (b = 7.13, p = .001). Therefore, Hypothesis 4 was supported. Collectively, the moderation results align with our arguments presented in our theoretical framework such that the extent to which decentralized leaders can enable ‘positive’ resource exchanges (i.e., knowledge sharing) and safeguard against ‘negative’ resource exchanges (i.e., work hindrance behaviors) is contingent on their relationship quality (i.e., LMX) with their team members. It is also possible that the decentralized leaders in our study may have been susceptible to other situational factors (e.g., status hierarchies) due to the unique healthcare context that they operate within, which inhibited their ability to positively influence work hindrance behaviors, especially under low LMX conditions. We elaborate on this argument in the ‘Interview results’ and ‘Discussion’ sections.
Interview results
The interviews both corroborated and expanded upon our findings from the surveys. Consistent with the survey results, the interview participants spoke to the potential positive effects of decentralized leaders on knowledge sharing. Interview participants attributed these effects primarily to the decentralized nature of the position augmenting the effective use of existing forms of knowledge sharing, such as huddles and communication binders. Decentralized leaders were also described as helping to facilitate knowledge sharing by being more visible and readily accessible to the team members and by acting as an efficient point person for receiving and re-disseminating information. Interview participants discussed how decentralized leaders improved upon knowledge sharing by ‘leading by example.’ Through modeling positive team behaviors, decentralized leaders fostered an environment where ‘problems are solved as a team.’
Interview participants also discussed a variety of situational factors that affected whether decentralized leaders were able to influence resource exchanges positively. These factors also help to explain the negative effects of decentralized leaders on work hindrance behaviors detected in Phase 1 of our study. Similar to our survey results, the team members' relationship quality with their leaders was described as playing a key role in whether positive resource exchanges were reciprocated and/or team members refrained from engaging in negative resource exchanges. Another prominent situational factor discussed involved the status-based hierarchies of healthcare teams. There appeared to be a rigid hierarchy between those in the RN/LPN role versus non-clinical workers, which led to power struggles with the decentralized leaders and ultimately more work hindrance behaviors occurring within these teams. These negative effects were exacerbated when the decentralized leader also had a non-clinical background. When the decentralized leader lacked this expertise, it limited his/her ability to support his/her team, thereby lowering LMX quality, and also inhibited his/her status and influence among the clinical workers, e.g., LPN/RN. When the decentralized leader was younger and/or had lesser tenure relative to some team members it also undermined his/her credibility and status, and ultimately his/her ability to positively influence the team.
Other noteworthy situational factors discussed in the interviews are summarized below: (1) the leadership behaviors of the decentralized leaders: when there was a mismatch between the decentralized leader's leadership behaviors and the team members' leadership preferences, it detracted from the leader's ability to influence resource exchanges. Some examples of undesirable leadership behaviors were decentralized leaders being overly critical and too focused on the problems occurring in the team, not sufficiently following through on complaints/issues, and not empowering/trusting team members enough. (2) Team members' characteristics: personality traits such as lacking an openness to change contributed to a greater resistance toward the decentralized leader. (3) The relative workload of the team: more demanding neighborhoods seemed to contribute to work hindrance behaviors occurring more easily due to the added frustrations that arose from feeling overworked, especially in the absence of desirable leadership behaviors. (4) The physical location of the neighborhood: the neighborhood that was furthest away from the others felt isolated and less supported and in turn, faced greater challenges. (5) The use of supplementary programs and trainings (e.g., training on diversity, personality differences, trust, group decision-making, etc.) for both team members and decentralized leaders enhanced the positive effects and acceptance of this position. (6) The newness of the position: participants indicated that there is a learning curve for both the decentralized leader and the team members. They anticipated that with time things would run more smoothly. (7) Confusion regarding changes in reporting structure: the clinical staff members were accustomed to reporting to an RN/LPN, but now they were expected to report to the decentralized leader, which presented unique challenges related to clinical questions.
Discussion
Tannenbaum et al. (Reference Tannenbaum, Mathieu, Salas and Cohen2012) argue that the nature of teams and the environments within which they operate are changing, and that research has not always kept pace with these changes. Our study contribute to this literature by exploring whether and how formal decentralized leadership influences positive (i.e., knowledge sharing) and safeguards against negative (i.e., work hindrance behaviors) resource exchanges within cross-functional healthcare teams. Our results provide evidence for generalized exchanges (Lévi-Strauss, Reference Lévi-Strauss1969), in the form of increased task-specific knowledge sharing, taking place among healthcare workers when they are afforded additional resources and support from a decentralized leader, especially under favorable LMX conditions. These findings coincide with prior work on SET (Homans, Reference Homans1958), leadership, and teams (Omar et al., Reference Omar, Zainal, Omar and Khairudin2009), and are also consistent with research on LMX, which has also found that supportive leadership behaviors foster positive exchanges within teams (Dulebohn et al., Reference Dulebohn, Bommer, Liden, Brouer and Ferris2012). Our results also correspond to the literature on cross-functional (and self-managed) work teams, which has argued that, in order for leaders to be effective, they should act as a resource and offer guidance, coaching, and support for teams, rather than occupying a purely supervisory role as is often the case in more centralized and hierarchical organizational structures (Jones & George, Reference Jones and George2014).
A key contribution of our research is insights on how the effects of decentralized leaders specifically apply to interdisciplinary teams in a long-term care context. We contribute to understanding the dynamics of cross-functional teams in an area of particular relevance in today's society, i.e., the context of shifting/aging demographics (Scheuer & Loughlin, Reference Scheuer and Loughlin2020). Healthcare systems will need to accommodate an ever-increasing number of people living with a greater burden of illness due to multiple complex chronic conditions, as well as dementia. In these more complex patient cases, the ability to ensure that staff have access to the information they need regarding their patients (e.g., via knowledge sharing behaviors) will be vital for effective decision-making and overall service quality (van Beek et al., Reference van Beek, Wagner, Spreeuwenberg, Frijters, Ribbe and Groenewegen2011). Our findings shed light on a new avenue for enabling knowledge sharing among long-term care professionals. Furthermore, pressures on human resources, including nursing shortages, add an additional strain on cross-functional teams who are now required to take on increasing amounts of work (Fox & Abrahamson, Reference Fox and Abrahamson2009; McGilton et al., Reference McGilton, Bowers, Heath, Shannon, Dellefield, Prentice and Boscart2016). The addition of formal decentralized leaders may help to enhance positive resource exchanges, especially under high LMX conditions.
Insights from our research about the effects of decentralized leadership on negative resource exchanges (i.e., work hindrance behaviors) also contribute to the literature. Prior work has mainly focused on the role of leaders in influencing ‘positive’ resource exchanges (Rangus & Slavec, Reference Rangus and Slavec2017). However, it is also important to understand the unique challenges associated with negative resource exchanges, especially in the healthcare context where teamwork has been found to be challenging (Atwal & Caldwell, Reference Atwal and Caldwell2005; Caldwell & Atwal, Reference Caldwell and Atwal2003). Interestingly, our findings suggest that the presence of a decentralized leader could actually do more harm than good when attempting to influence work hindrance behaviors in the absence of a high-quality LMX relationship. These negative effects can be explained by the unique hierarchical structure and rigid professional boundaries based on expert knowledge and clinical skills that are characteristic of the healthcare context. Contingency models of leadership and the leader substitutes model in particular, suggest that under certain conditions employees can perform at a high level without a formal leader exerting influence over them (Kerr & Jermier, Reference Kerr and Jermier1978; Podsakoff, Niehoff, MacKenzie, & Williams, Reference Podsakoff, Niehoff, MacKenzie and Williams1993). In these cases, a characteristic of a subordinate and/or of a situation or context can act in place of the influence of a leader and subsequently make leadership unnecessary and even a hindrance (Jones & George, Reference Jones and George2014). In one of the earliest studies in cross-functional long-term care teams, Cott (Reference Cott1997) analyzed social networks across different professional disciplines and units and found that decision-making was hierarchical in terms of staff in higher status professions (e.g., nurses) making decisions, whereas lower status staff were carrying out daily care. The study found that although cross-functional teams engage in teamwork the nursing team has a primarily mechanistic structure. In our study, it is possible that leadership may have been ‘substituted’ already by certain ‘higher status’ staff members, such as RNs. The presence of the decentralized leader may have fostered discontent among these staff members by disrupting the ‘natural’ work processes and power dynamics that were previously occurring in these neighborhoods, thereby contributing to more negative exchanges (i.e., work hindrance behaviors). The comments from the interview participants regarding the negative effects of status hierarchies, the desire for the decentralized leader to be more empowering and trusting in team members' abilities, and the stated confusion among the RNs/LPNs with respect to the new reporting structure offer additional support for this claim. However, it is important to note that when the decentralized leader fostered a high-quality LMX relationship with his/her team members the negative effects of decentralized leadership on work hindrance behaviors seemed to be augmented most likely because the decentralized leader was able to gain the respect of these high status team members. This is a particularly interesting finding as it highlights contextual contingencies to the effects of formal decentralized leadership in a healthcare setting, something that has mostly been overlooked in prior research.
A final contribution of our study stems from our choice of methodology. As Gigerenzer (Reference Gigerenzer1991) argues, ‘scientists’ tools are not neutral’ (p. 264) – methods impact theory construction and ultimately our understanding of a given phenomenon. By gathering ‘network’ data along with capturing decentralized leadership via a naturally occurring ‘empowerment initiative’ at our research site (rather than asking team members to share their perceptions of team behaviors and/or decentralized leadership as most prior studies have done) our study offers a more complex and arguably also a more realistic understanding of the role of decentralized leaders in cross-functional healthcare teams.
Implications for healthcare practice
The current study sheds light on how healthcare organizations should approach designing their organizational structures. Our results suggest that hiring and/or retaining decentralized leaders may be a worthwhile endeavor, but only under certain circumstances. Given the findings on the moderating effects of LMX, organizations should ensure that they are training their decentralized team leaders on how to foster high-quality relationships with their team members and/or should hire individuals that are naturally inclined to enact these supportive leadership behaviors. In addition, before healthcare organizations incorporate decentralized leaders into their teams, they should become educated on existing status-based hierarchies, the personalities and leadership preferences of their team members, and other situational factors that arose as important in our interviews in order to ensure that this individual does not act as a hindrance rather than as a benefit to the team. It would also be helpful for decentralized leaders to have the clinical expertise necessary to support their teams effectively.
Our study is also informative in light of the trend toward delayering and the elimination of middle managers (Jones & George, Reference Jones and George2014). According to Engle et al. (Reference Engle, Lopez, Gormley, Chan, Charns and Lukas2017), middle managers play a key role in implementing new, innovative practices in the current environment of burgeoning healthcare budgets and fiscal restraint. They argue that research has been limited to senior managers and that a gap exists in understanding how middle managers can impact decision-making and influence organizational performance. Other researchers share in this sentiment (Birken et al., Reference Birken, Clary, Alishahi Tabriz, Turner, Meza, Zizzi and Charns2018; Institute of Medicine, 2001). Our study suggests that middle managers in the form of decentralized formal leaders could indeed add value to healthcare organizations, but only in certain situations (e.g., where LMX is high). Our results also demonstrate that self-managed healthcare teams (without the added support of a decentralized leader) might find themselves overwhelmed and in turn their teamwork (e.g., knowledge sharing and work hindrance behaviors) is likely to be hindered. Such findings speak to the importance of organizations ensuring that they are not ‘cutting corners’ when empowering their work units, e.g., by failing to provide team members with the proper resources, support, and coaching needed in order to be successful in their empowered roles (De Janasz, Dowd, & Schneider, Reference De Janasz, Dowd and Schneider2018).
This is especially relevant for smaller nursing homes in rural/sub urban areas. Physicians/nurses who head/own many of these private nursing homes invariably have their prior work experience based in large and medium sized hospitals in urban communities and hence may have an inherent bias toward replicating the bureaucratic structure and culture that they have experienced earlier. Our study suggests that smaller nursing homes such as the one investigated in our study may find value in allowing decentralized leadership in their units as an extra support to their teams.
Limitations
Although the results of our study provide insight into the impact of decentralized leaders on cross-functional healthcare teams' resource exchanges, a limitation of our study is that it did not specifically evaluate team performance. However, the resource exchanges investigated in our study have been associated with a variety of performance outcomes in the literature (Mehra et al., Reference Mehra, Smith, Dixon and Robertson2006; Sparrowe et al., Reference Sparrowe, Liden, Wayne and Kraimer2001). Prior studies have also demonstrated indirect relationships between performance and high-quality LMX relationships (Gully, Incalcaterra, Joshi, & Beaubien, Reference Gully, Incalcaterra, Joshi and Beaubien2002). Therefore, we can assume that decentralized leaders also would have positively influenced team performance. This assumption is further supported by the results of a resident satisfaction survey showing improvements in perceived service quality. The survey was administered to the residents by the facility both prior to, and after the introduction of, the decentralized leaders.
A second limitation of our study was the relatively small sample drawn from a single healthcare facility. Although small sample studies are common in healthcare research due to privacy issues, we acknowledge that our sample size may have limited the effects we were able to detect and therefore we advise readers to interpret our results with extreme caution. Furthermore, although sampling participants from one site was beneficial in that we were able to study the factors of interest in a controlled quasi-experimental design by comparing neighborhoods with and without a decentralized leader, we also caution readers to refrain from generalizing our findings beyond our immediate context.
Future research
Additional research directly linking the performance (e.g., service quality) of cross-functional teams and decentralized leadership would be worthwhile in understanding how best to position decentralized leaders in order to address the demands of modern organizations. Investigating the role of other moderating variables (such as status perceptions, perceptions of leadership behaviors, leader or team member traits, or other situational factors identified in our interviews) would be useful areas for future research also. Cross-sector studies, in which the effects of decentralized leadership are compared across different industries or in different sized organizations, could help in identifying additional contextual factors influencing these effects. The use of a longitudinal rather than a cross-sectional design would also be a valuable extension because it would account for the time needed for a ‘new’ leader to begin having a noticeable effect on his/her team. In addition, it could help to determine whether there becomes a point at which team members no longer need the added support of a decentralized leader.
As more professions are included as part of team-based healthcare delivery, additional research is also needed to aid in our understanding of the implications of status-based hierarchies in healthcare teams. Although our study highlighted resource exchanges in a facility that centered on the RN/LPN dyad, in hospital as well as community-based healthcare teams, physicians and increasingly, nurse practitioners play significant roles, where traditionally the former have dominated healthcare environments. Therefore, further research specifically investigating status hierarchies associated with nurse practitioners and the resulting impact on decentralized leadership would be informative.
Conclusion
Collectively, our mixed method study highlights the potential contributions of formal decentralized leadership to cross-functional healthcare teams. Specifically, the findings suggest that decentralized leaders may enable knowledge sharing and safeguard against work hindrance behaviors, but that the effects are contingent upon the situation (e.g., LMX quality and status-based hierarchies). As management scholars develop a deeper understanding of the role of decentralized leaders, e.g., by engaging in the suggested avenues for future research recommendations, the demands on modern, complex health organizations and their teams will be better served.
Acknowledgements
We would like to thank Dr. James O'Brien, Associate Professor of Management, Saint Mary's University, Canada, for your guidance during the initial development of this research project and the early drafts of this paper. We would also like to thank Dr. Kay Keels, Professor of Management and Decision Sciences, Coastal Carolina University, for your assistance with copyediting our paper.
Appendix A: Interview guide
(1) Can you tell me how you generally feel about the Decentralized Neighborhood Leader (NBL) position?
(2) Can you discuss the impact that the NBL is having in your neighborhood?
(a) Can you discuss if and how the NBL is influencing knowing sharing among employees in your neighborhood (i.e., the sharing of work related information, skills, and expertise)?
(b) Can you discuss if and how the NBL is contributing to a more cooperative and less disruptive work environment?
(3) What would you change about the NBL position so that it would have a greater positive impact on the neighborhood?
(4) In your opinion, would you keep the NBL position? Why or why not?
(5) Is there anything else you would like to share about the NBL position?
Cara-Lynn Scheuer is an Assistant Professor of Management at Coastal Carolina University. She holds a PhD in Business (Management) from Saint Mary's University (Canada). Her research interests include workplace diversity, leadership, and teams with a particular focus on the plight of the young professional.
Annika Voltan is the Executive Director of the Nova Scotia Community Sector Council in Canada. She holds a PhD in Business (Management) from Saint Mary's University (Canada). Her research interests focus on social entrepreneurship and social innovation, and the role of networks in these contexts.
Kothai Kumanan is a Senior Strategist with the Nova Scotia Department of Health and Wellness. She holds a Master's in Health Administration (Dalhousie University, Canada). Her research interests include primary health care reform and health services delivery; health human resource planning; policy and implementation of palliative care services, with a particular focus on the early integration of the palliative approach in primary care and oncology settings.
Subhajit Chakraborty is an Assistant Professor of Management and Decision Sciences at Coastal Carolina University. He holds a PhD in Business Administration with a focus on operations management from The University of Texas Rio Grande Valley. His research interests include service quality, services design, outsourcing, and lean healthcare operations.






