Introduction
In 2015, the United Nations General Assembly adopted the sustainable development goals (SDGs) with a target of reducing the maternal mortality ratio to less than 70 per 100000 live births by 2030 (United Nations, 2015). Notwithstanding, worldwide and national interventions to reduce maternal mortality resulting from pregnancy and delivery, maternal mortality rates are still high. According to the World Health Organization (WHO), sub-Saharan Africa contributed about 66% of the global estimated 303,000 maternal death which occur per year (WHO, 2015b). In Uganda, whereas rates have been declining, maternal mortality rate (MMR) is still high standing at about 343 per 100000 live births making it the 36th contributor of all maternal deaths (Central Intelligence Agency, 2018). Most important is that these poor indicators for maternal mortality in developing countries have been largely attributed to inadequate access to antenatal care, postnatal care, emergency obstetric and, family planning services (WHO, 2015b). In the attempt to achieve good health and wellbeing (SDG-3), equity and equality in availability to emergency obstetric care including assisted vaginal delivery, safe Caesarean section is exceedingly indispensable. Caesarean section (C-section) is acknowledged worldwide as a life-saving obstetric procedure that reduces mortality rates of mother and fetus and improves reproductive health (Betran, Torloni, Zhang, Reference Betran, Torloni and Zhang2015). Although vaginal delivery is still an important safe and low-cost method of delivery, C-section is sometimes performed when it is not even required. This creates health challenges for pregnant women and their newborn infants which has become a matter of serious concern for public health experts globally (Abbas et al., Reference Abbas, Amir and Sadiq2018).
There is no consensus on the optimal rate of Caesarean delivery at the population level although values between 5% and 15% of live births have been suggested (Robson & Costa, Reference Robson and Costa2009). At population level, Caesarean section rates higher than 10% are not associated with reductions in maternal and newborn mortality rates (WHO, 2015a). In most countries, the Caesarean section rate has exceeded the level of 10–15% recommended by the World Health Organization (WHO, 2015a). Among high-income countries, C-section rate is 30.3% in the USA, 22% in the United Kingdom, 26% in Canada, 19% in France, 28% in Germany and 30% in Australia. Similarly, in low-income countries, C-section rate is increasing every year (Gibbons et al., Reference Gibbons, Belizán, Lauer, Betrán, Merialdi and Althabe2010). There has been a trend of increasing frequency, acceptance, and popularity of Caesarean sections in Uganda perhaps due to the increasing number of women using in-vitro fertilization or assisted conception. Overall, the C-section rate for live births at facilities was 10%, increasing from 9% in 2012 to 11% in 2016. The overall population-based C-section rate was 5% and increased from 3 to 6% over the same period. Health Centre IV level facilities had the largest annual rate of increase in C-section rate between 2012 and 2016. Overall, Uganda’s facility-based C-section rate was projected to increase by 36% in 2021 while the population-based C-section rate is estimated to have doubled from the baseline in 2016 (Atuheire et al., Reference Atuheire, Opio, Kadobera, Ario, Matovu, Harris, Bulage, Nakiganda, Tumwesigye, Zhu and Kaharuza2019). National referral hospitals such as Mulago hospital are equipped to provide obstetric services including Caesarean sections (Initiative for Social and Economic Rights, 2018). Caesarean section used to be regarded as a last resort and a life-saving measure, but as time went on, it became performed with greater safety and more frequently. In modern times however, there has been a paradigm shift in which C-section is being performed for non-life-threatening indications such as maternal request, especially for women with a higher economic class (Amjad et al., Reference Amjad, Amjad, Zakar, Usman, Zakar and Fischer2018; Manyeh et al., Reference Manyeh, Amu, Akpakli, Williams and Gyapong2018).
The risks and costs associated with Caesarean deliveries are significant (Clark et al., Reference Clark, Belfort, Dildy, Herbst, Meyers and Hankins2008). Caesarean sections when adequately indicated can prevent poor obstetric outcomes and be lifesaving procedures for both the mother and fetus (Souza et al., Reference Souza, Gülmezoglu, Lumbiganon, Laopaiboon, Carroli, Fawole and Ruyan2010). However, C-section rates have been rising globally during the last decades resulting in an overall C-section rate close to 26% in 2010 (Prakash., & Neupane, Reference Prakash and Neupane2014), they differ substantially in different parts of the world, ranging from approximately 1% in some African countries (South Sudan and Niger) to 56 % in some American countries (Brazil and the Dominican Republic) (World Health Organization., 2013). Other studies indicate that Latin America and Caribbean show the highest rate (29.2%) and Africa shows the lowest (3.5%) (Ayano et al., Reference Ayano, Geremew, Beyene and Muleta2015). In developed countries the proportion of Caesarean birth is 21.1% whereas in least developed countries only 2% of deliveries are by cesarean section (Ayano et al., Reference Ayano, Geremew, Beyene and Muleta2015).
Certain obstetric risks such as dystocia, previous Caesarean section, fetal distress, breech births, post-term pregnancy, multiple pregnancy and hypertensive disorder are considered to be justifiable medical reasons for Caesarean deliveries (El–Ardat, Izetbegovic, Mehmedbasic, Reference El–Ardat, Izetbegovic and Mehmedbasic2013; Mishra & Ramanathan, Reference Mishra and Ramanathan2002). Furthermore, demographic, cultural and psychological factors may also influence the increase in C-section rate (Ghosh, Reference Ghosh2010). Maternal demographics such as age, social class, education, occupation and type of residence have been found to be strongly correlated with the type of delivery (Nilsen et al., Reference Nilsen, Østbye, Daltveit, Mmbaga and Sandøy2014). In terms of cultural aspects, studies have shown that the cultural context plays a pivotal role in constructing the patterns of women’s behavior towards pregnancy related issues and mode of delivery (Karlström et al., Reference Karlström, Nystedt and Johansson2011). Additionally, psychological factors which may be due to fear related to prolonged labor and vaginal delivery pain reinforce women’s preferences for Caesarean delivery (Béhague et al., Reference Béhague, Victora and Barros2002). Furthermore, doctors’ decisions and patient demand are contributing factors affecting the escalation of C-section rate across the globe (Agustina et al., Reference Agustina Mazzoni, Liu, Bonotti, Luz Gibbons and Sánchez2012). In developed countries, where patients argiven the option to choose between vaginal and Caesarean delivery, women’s preference for Caesarean delivery has appeared as an important determinant (Ash, Reference Ash2000; Amjad et al., Reference Amjad, Amjad, Zakar, Usman, Zakar and Fischer2018). In developing countries, doctors’ referrals to perform Caesarean surgery appear to be a more significant determinant than the woman’s preference (Lauer et al., Reference Lauer, Betrán, Merialdi and Wojdyla2010).
Although studies have shown an increasing trend in C-section deliveries, besides the medical explanation of saving the mother and the child of obstetric risks, many of the sociodemographic or non-clinical reasons remain unknown (El–Ardat, Izetbegovic, Mehmedbasic, Reference El–Ardat, Izetbegovic and Mehmedbasic2013; Mishra & Ramanathan, Reference Mishra and Ramanathan2002). The ongoing debate between social scientists and medical sociologists on what could be the cause of this trend and preference is still inconclusive. While the medical explanation may be understood in explaining the trend in C-section delivery, what might not be clear about this trend is the parallel argument that the trend could be due to women’s preference, who in most cases, take informed decisions and other non-clinical factors. The current paper therefore, assessed non-clinical factors associated with C-section deliveries among women in Uganda. Results from the study could be useful to policymakers and facility managers in different hospitals in saving cost, improving obstetric practice, and contributing towards the realization of SDG-3.
Theoretical perspectives
A number of theories and research findings have been thought of in trying to explain the rising trend in C-section deliveries however they have all been inconsistent and inconclusive. According to the theory of planned behaviour, one’s decision depends on reasonable investigation and available information (Otogara et al., Reference Otogara2018). In this case, behaviour intention can be predicted by three factors; positive attitude towards that behavior, forces of social pressure (subjective norm), and the perception that it can be done (Ajzen, Reference Ajzen2002). Accordingly, the decision for women to weigh between C-section as opposed to normal delivery as well as the consequences, is one of the construct of the theory. Regarding the subjective norm, a woman’s decision for C-section delivery compared to vaginal is influenced by the views of important others in society. Another construct is the perceived behavioral control which explains whether a pregnant woman is capable of controlling labor pains if she is to deliver normally through the vagina and vice versa. The medicalization theoretical perspective explains how non-clinical problems among pregnant women are defined as medical conditions (Conrad, Reference Conrad2007). In the present context, during pregnancy and childbirth, the theory suggests that the process is no longer taken as a natural process but it is more dependent on the knowledge of physicians; and despite well-known consequences of C-section for the mother and child’s health, the preference for C-section is increasing without convincing medical reasons.
According to body-image theory, delivering through C-section helps to preserve vaginal strength, preserve normal sexual function, and keep anatomical and functional arrangement of the pelvic floor and intrapelvic organs (Hosseini et al., Reference Hosseini, Iran-Pour and Safarinejad2012; Pollack et al., Reference Pollack, Nordenstam, Brismar, Lopez, Altman and Zetterstrom2004; Safarinejad et al., Reference Safarinejad, Kolahi and Hosseini2009). Similarly, others demand C-section due to fear of long labour pains for vaginal delivery (Nazir, Reference Nazir2015). Practically, this might be one of the reasons for promoting the decision of taking up C-section and advancing a positive attitude among women, midwives, and physicians. According to Ghosh’s theory, the increase in C-section delivery in low income countries can be explained by three main aspects: medical or risk factors which influence the doctors decision to perform C-section; socio-economic status, culture and belief of women’s preference (non-clinical); and the institutional concerns of performing C-section (comprising of economic incentives and risk minimizing behavior) (Ghosh, Reference Ghosh2010). A number of medical factors, for example, breech presentation of the unborn child and age of the mother, and size of the unborn at birth, are among the possible risk factors leading to C-section delivery. Non-clinical factors play an important role in influencing a woman’s decision of the mode of delivery.
Based on the argument behind these theories, this paper uses the Ghosh theory by customizing some aspects to explain the influence of non-clinical factors on the variation in intention for C-section delivery among women in Uganda. Five hypotheses were tested: First, older women are more likely to undergo C-section delivery compared to their younger ones. Second, educated women are more likely to have Caesarean deliveries compared to the uneducated. Third, women in urban areas are more likely to deliver by C-section compared to women in rural areas. Fourth, women with higher socio-economic status are more likely to have C-section deliveries compared to those with lower economic status; and five, C-section deliveries are more likely to occur among first-birth order births than sixth-or higher-birth orders.
Methods
This study used data from the 2016 Uganda Demographic and Health Survey (UDHS) to investigate factors associated with Caesarean section delivery in Uganda. The 2016 UDHS is part of the worldwide series of nationally representative cross-sectional household survey programmes. It collects individual- and household-level socio-demographic, health and sexual activity, maternal and child health, mortality, fertility, family planning, domestic violence, and nutrition data. The UDHS is periodically conducted by the Uganda Bureau of Statistics with technical assistance from ICF International and funded by the United States Agency for International Development. At implemementation stage, 20,880 households were selected using a two stage sampling sampling procedure. In the first stage, 162 enumeration areas (EAs) in urban areas and 535 (EAs) in rural areas were selected from the 2014 Uganda National Population and Housing Census. In the second stage, a listing of households was compiled in each of the 697 accessible selected EAs from April to October 2016. All women aged 15-49 found in the household the night before the survey were eligible to be interviewed; and out of the 19088 eligible women, 9929 women were interviewed. Those who had never given birth and those whose responses were noncommittal were excluded from this study. Mothers were asked whether they had a C-section or vaginal delivery during the 5 years preceeding the survey.
Measures of outcome variable
The outcome variable was created from a general question regarding the most recent birth, ‘Was (NAME) delivered by Caesarean (did they cut your belly open to take the baby out) or normal vaginal delivery?’ Based on this question, a dummy variable was created indicating whether the woman respondent had the most recent birth by Caesarean section mode of delivery or not. In this study, whoever delivered by Caesarean section was coded as 1 (Yes) and as 0 (otherwise); and women who had never given birth were dropped from the dataset.
Measures of explanatory variables
The independent variables included maternal age, size of the baby, birth order, children everborn, education level, type of place of residence, wealth quintile, employment status and marital status. These variables were selected based on earlier studies (Amjad et al., Reference Amjad, Amjad, Zakar, Usman, Zakar and Fischer2018; Abebe et al., Reference Abebe, Gebeyehu, Kidane and Eyassu2016). Maternal age is a key variable to this study and during data collection, it was captured as a continuous variable. During analysis, it was grouped as 15-19, 20-24, 25-29, 30-34, 35-39, 40-44, 45-49. During data collection, birth weight was obtained from either the written record or, in absence of the record, the mother’s recall. It is from this, that the variable size of the baby was constructed and categorized as very large, larger than average, average, smaller than average, very small. Mothers who responded that they “don’t know” were dropped from thhe sub-sample since they were noncommittal. Birth order was categorized as first, second and third or higher, children everborn coded as 1-3 children and 4 or more births, four being Uganda’s wanted fertility.
During data collection, the level of education of the mother was captured as no education, primary, secondary, tertiary. In modelling using complementary log log (cloglog), post-secondary was labelled as “tertiary. Thus, the categories were collapsed into four as, no education, primary, secondary and tertiary; type of place of residence was grouped as urban and rural. Wealth index grouped into quintiles, categorized as poorest, poorer, middle, richer, richest, a woman’s employment status shapes her social life in a way that working women tend to have more control of their lives unlike those who do not work as they can afford the costs of living. In modeling, woman’s employment was grouped as working and not working. Timing of antenatal Care (ANC) visit was coded as first trimester, second trimester and third trimester. Because partners usually influence one’s decision making process, in modeling marital status, it was categorized as married or living together, widowed or separated, never in union and divorced.
Statistical analyses
Data were weighted to mitigate the effect of sampling imbalances, complex survey design, and nonresponse. Frequency distributions were computed to summarise the characteristics of women considered in the sample. The relationship between the dependent variables as to whether the woman respondent delivered through C-section or vaginal delivery and the independent variables were established at bi-variate level and tested using chi-square test, set at p<0.05. In the data, about 7% of the women reported to have delivered using C-section, indicating that this is a rare event and a possibility of biases resulting from perfect separation and maximum likelihood estimation method (Rahman & Sultana, Reference Rahman and Sultana2017). Perfect separation often occurs when the outcome variable separates the predictor variable and when the distribution is somewhat extreme. For these two reasons, the complementary log log (cloglog) was used at multivariate level to determine the net effect of independent factors on the dependent variable (mode of delivery) (Firth, Reference Firth1995). The covariates included in the final model were based on statistical significance p<0.05 at bivariate level as well as those found to be significant elsewhere from other studies. The results of the cloglog model are presented in form of odds ratios (OR) with their corresponding 95% confidence interval. The fitted model was subjected to the link-test to examine whether the independent variables were specified correctly and also assess the goodness of fit of the model (Kohler & Kreuter, Reference Kohler and Kreuter2005). The test uses the hat and _hatsq statistic. When the model describes the data correctly, the hatsq should not be significant (_hatsq, p>0.05), which implies that the observed data mirror the expected. Before fitting the model, the independent variables were tested for multicollinearity (results not presented). The variable ‘children ever born’ and ‘birth order, though significant at bivariate level, had a positive correlation (r=0.6761). However, after some diagnostic analysis, it was found that both have a separate effect on the risk of Caesarean section, so both were retained in the model. Missing data were assumed to be missing completely at random (Abonazel & Ghallab, Reference Abonazel and Ghallab2018).
Results
Distribution of respondents by non-clinical characteristics
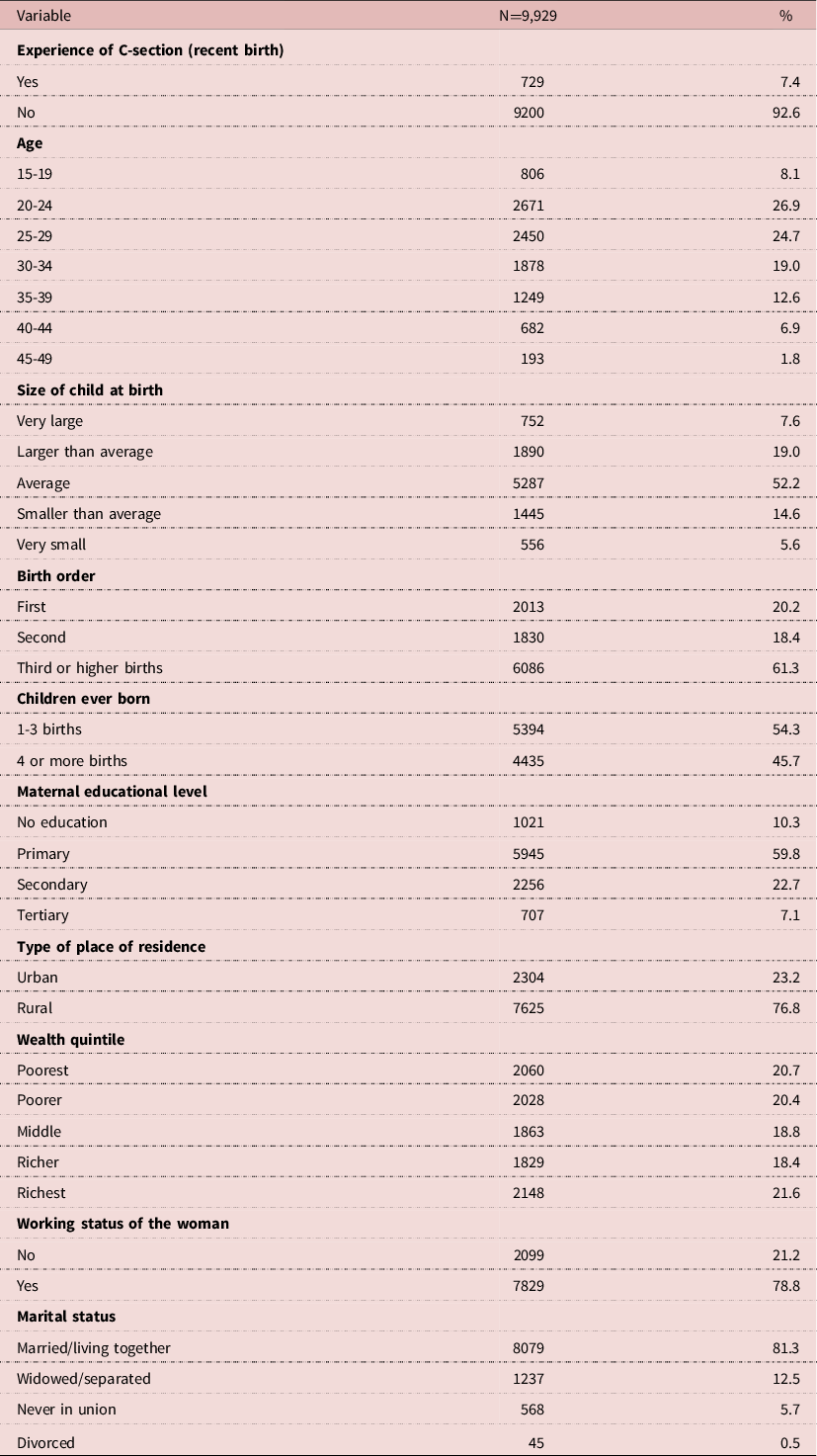
Table 1 presents the distribution of respondents by selected non-clinical characteristics. It shows that overall the proportion of women who had their last birth by Caesarean section was about 7%. The majority of the respondents (61%) said their most recent child was the third born or higher. Concerning the weight of the recent birth, 52% were of average. About 30% of the women had at least secondary education. Regarding type of residence, majority of the women (77%) were from rural areas. The majority of respondents (79%) were currently employed in gainful employment. About 81% of the respondents were married or living together with their partners. With regard to age, approximately 8%, 27%, 25%, 19%, 13%, 7%, and 2% were in the age range 15-19, 20-24, 25-29, 30-34, 35-39, 40-44, and 45-49 years respectively. Majority of the women (54%) had given birth to not more than 3 births and 46% of the women had given birth to 4 or more children. Regarding the timing of the first ANC visit, results show that the mean time to the first ANC visit was 4.3 months with a standard deviation of 1.47 months.
Table 1: Percentage distribution of selected characteristics of respondents
Differentials in C-section deliveries of the most recent birth by non-clinical characteristics
Table 2 presents differentials in C-section deliveries during the most recent birth by socio-ecnomic characteristics. C-section deliveries varied significantly with age of the mother (χ2=13, p=0.045), education level (χ2=364, p=0.000), residence (χ2=166, p=0.000), wealth quintile (χ2=346, p=0.000), employment status (χ2=5, p=0.027), marital status (χ2=13, p=0.004), number of children everborn (χ2=101, p=0.000) and birth order (χ2=128, p=0.000). Differentials by birth weight however did not show significant variation with C-section (χ2=7, p=0.112).
Table 2: Differentials in respondents’ utilization of Caesarean section for the most recent birth in Uganda by selected characteristics

Multivariate results
In identifying the net effect of each independent factor on the dependent, a final model was built based on the variables identified by the bivariate analysis. These include maternal age, birth order, children everborn, maternal education level, type of place of residence, wealth quintile of mother, timing of first ANC and marital status. The results in Table 3 show that odds of utilizing C-section mode of delivery increased for women aged between 30-34 (OR=1.80; 95% CI = 1.15-2.84, p= 0.011), aged 35-39 (OR=1.97; 95% CI = 1.17-3.30, p= .011); and aged 40-44 (OR=1.88; 95% CI = 1.04-3.42, p= .037) compared with those aged 15-19. Furthermore, women were 30% less likely to have their second (OR=0.70; 95% CI = 0.55-0.90, p= 0.005) and 53% less likely to have the third or higher births (OR=0.47; 95% CI=0.34-0.64, p= 0.000) through Caesarean section compared to the first birth. Relatedly, women with 4 or more births were 33% less likely to have a Caesarean section compared to those with atmost three (OR=0.67; 95%CI=0.49-0.93, p=0.016).
Table 3: Odds ratio estimates for utilizing Caesarean section for the most recent birth for women in Uganda

Ref.=Reference Category; CI=Confidence Interval.
Women with tertiary level of education were found to be 2 times more likely to have given birth to their most recent child through Caesarean section compared to those with no formal education (OR=2.25; 95% CI = 1.42-3.56, p= 0.001). In addition, the table shows that the odds of women from the middle wealth quintile using C-section for the most recent birth were 1.67 times higher (95% CI=1.21-2.29, p= .002); 1.76 times higher for women in the richer wealth quintile (95% CI=1.24-2.49, p= .002); and 3.05 times significantly higher for women in the richest wealth quintile (95% CI = 2.12-4.38, p= .000) relative to women in the poorest category. A one-month increase in the timing of ANC visit is associated with a reduction of 8% (OR=0.92) in the odds of a Caesarean section (95% CI = 0.86-0.98, p= .018). Working status, type of place of residence, and marital status were not associated with using Caesarean section as a form of delivery in Uganda. Regarding the diagnostic test of the model, results show that the final model was correctly specified. In this case, data suggests that the observed data mirror the expected data (hat:p=0.000; _hatsq:p= 0.557).
Discussion
The main objective of the study was to examine the influence of non-clinical factors on Caesarean deliveries in Uganda. As a result, five hypotheses were tested: ‘Older women are more likely to use Caesarean section as a mode of delivery than young ones’; ‘Educated women are more likely to have an increased chance of using Caesarean section than the less educated’; ‘Women residing in urban areas are expected to utilize Caesarean section as a mode of child delivery than those in rural areas’; ‘socio-economic status was likely to have a positive effect towards Caesarean section utilization; Caesarean deliveries were likely to be higher among first-order births. The C-section risk was increased with increase in the age of the mother and the risk was doubled for women aged 40 and over compared to younger mothers. These results are similar with those of Ababa and Thupayagale (Reference Ababa and Thupayagale-2010) in Ethiopia who found women aged 30 and over to have an increased likelihood of Caesarean deliveries compared to younger ones which is in agreement with Ghosh’s theory (Ghosh, Reference Ghosh2010). Similar results were observed in India and Vietnam (de Loenzien et al., Reference de Loenzien, Schantz, Luu and Dumont2019) and in Bangladesh by Rahman et al., (Reference Rahman, Haider, Rahman, Ahmed and Khan2018). However, results are contrary to the findings of (Mulongo et al., Reference Mulongo, Mwamini, Mukanire and Kyambikwa2017) who found no association between maternal age and C-section deliveries and Yassin and Saida, (Reference Yassin and Saida2012) who in their study in Egypt found women less than 30 years more likely to use C-section.
The positive association between advanced maternal age and C-section deliveries may be understood from five arguments. The first is the increasing pregnancy rate at advanced ages which seem to be occurring at the same rate with Caesarean deliveries. The natural physiological and anatomical changes which comes with aging exposes such mothers at advanced age to an elevated risk of maternity complications (Ghosh, Reference Ghosh2010). Consequently, older women may consider C-section to be safe with regard to protecting the unborn baby after a long period of conception difficulty. It could also be due to fear of labour pains and losing the baby. The second is that advanced maternal age is associated with adverse pregnancy outcomes and complications (for instance, high blood pressure or preeclampsia) that may lead to Caesarean deliveries (Lin, Sheen, & Tang, Reference Lin, Sheen and Tang2004; Souza et al., Reference Souza, Gülmezoglu, Lumbiganon, Laopaiboon, Carroli, Fawole and Ruyan2010). The third is that of accumulated experience in using health services which gives older women more confidence in decision-making towards their healthcare including pregnancy and child birth. The fourth is that, at advanced maternal age, women who may not want to have more children might prefer to undergo through bilateral tubal ligation (BTL) to guard themselves against ovarian cancer. Because BTL is a surgical process, they prefer to do it during Caesarean delivery. Fifth, young mothers may be reluctant to go for C-section possibly because of the discomfort, fear and risk accompanying C-section delivery, the risk of repeated C-section birth, and the limited number of C-section deliveries allowed in the developing world.
A decrease in Caesarean delivery likelihood was found to be associated with higher birth orders which is consistent with the findings of the study done in Bangladesh by Rahman and colleagues (Rahman et al., Reference Rahman, Haider, Rahman, Ahmed and Khan2018). The odds ratios of the second and third born and higher decrease by 30% and 53% respectively. These results might be explained by two perspectives. The first is that birth order is one factor that accounts for the most demographic changes given that there is a high primary C-section rate for first birth to women aged 30 and over. In the case of Uganda, majority of women give birth to their first birth before 30 years. This might be used to explain the inverse relationship between Caesarean delivery and higher birth orders. Second, it could be explained by women of advanced age with low birth order but with a higher likelihood of C-section delivery.
Some characteristics of women might increase the risk of C-section delivery. Results from the study show that women with tertiary level of education were found to be 2 times more likely to have C-section delivery compared to women with no education. This finding concur with that of Strom and Painter who argued that women in El Salvador with 10 or more years of education were found to be at least 4 times more likely to deliver by Caesarean section compared to those with no formal education (Strom & Painter, Reference Strom and Painter2013). Also, it is inline with the body-image theory where such women may want to prevent the pelvic floor disorders often associated with vaginal birth (Menon & Handa, Reference Menon and Handa2013). Relatedly, Manyeh et al., (Reference Manyeh, Amu, Akpakli, Williams and Gyapong2018) and (Banchani & Tenkorang, Reference Banchani and Tenkorang2020) found similar results in Ghana. Two perspectives are advanced to explain this finding. First, the increasing trend among women pursuing tertiary education and orienting themselves towards career and financial goals. The implication is that such women end-up postponing their childbearing to have their first births when aged 30 and over thus increasing their likelihood of undergoing through C-section delivery. As a result, this may conceivably be a factor in what is seen as an increasing trend in C-section. Second, educated women can afford the cost of C-section delivey and fees especially in private or private-not-for-profit hosipitals.
It is not surprising to find a positive association between C-section delivery and wealth. Results show that the likelihood of C-section delivery is increasing with better wealth with women in the middle quintile being 67% more likely; women in the richer quintile being 76% more likely and; women in the richest quintile being about 3 times more likely compared to women in the poorest quintile. These results concur with the overall literature in general and with similar studies in Pakistan (Amjad et al., Reference Amjad, Amjad, Zakar, Usman, Zakar and Fischer2018) and in Bangladesh (Rahman et al., Reference Rahman, Haider, Rahman, Ahmed and Khan2018) which reported a higher likelihood of C-section deliveries among affluent mothers relative to the poorest. The significant likelihood in use of C-section among the affluent mothers could be due to costs associated with Caesarean birth. While C-section delivery is free in public hospitals, there are indirect costs and other unofficial fees from health professionals which are not covered by Uganda’s health policy. Ugandan women also prefer to go to private and private-not-for profit or faith based hospitals where services seems to be better but with high direct and professional costs. On the one hand, this implies that these costs may deter poor women from accessing C-section services at hospitals; and on the other hand, it implies that women from affluent households, may be more likely to go for C-section delivery because of the perceived lower risk. The lower likelihood of opting for Caesarean delivery among multiparous women (those with four or more children) is not surprising and might be explained by previous delivery type. It is a common perception among women with vaginal delivery experience to reject Caesarean delivery even when it is recommended by medical professionals. This is because of the guilt of not delivering normally and the risk associated with future C-section deliverie s.
In summary, the study used the 2016 Uganda Demographic and Health Survey to examine the influence of non-clinical factors associated with Caesarean deliveries in Uganda. Accordingly, five hypotheses were tested, ‘older women are more likely to use Caesarean section as a mode of delivery than young ones’; ‘Educated women are more likely to have an increased chance of using Caesarean section than the less educated’; ‘Women residing in urban areas are expected to utilize Caesarean section as a mode of child delivery than those in rural areas’; ‘socio-economic status is likely to have a positive effect towards Caesarean section utilization; and Caesarean deliveries were likely to be higher among first-order births. The discussion in the above seems to be in line with some of the arguments behind Ghosh’s theory where the risk increases with increase in age; and body image theory in which the more educated would like to keep anatomical and functional arrangement of the pelvic floor and intrapelvic organs. These results are expected to be useful in informing policy dialogue and formulation, given the increasing trend in Caesarean deliveries. In future, more data should be collected to explore further the linkage between C-section delivery, type of place of residence, work status of women, marital status and the timing of antenatal care services.
There are some limitations which can be addressed for future studies. First, social desirability which could arise from self-repoted data on maternal age and recall bias regarding C-section birth. However, Caesarean section delivery was restricted to the recent birth within a 5 year period to limit this type of bias. Finally, Uganda Demographic Healthy Survey data is cross-sectional and thus what is reported by the study are factors associated with, which do not imply a causative relationship. In conclusion, the study found maternal age, education level and wealth quintile as non-clinical factors found to positively influencing Caesarean deliveries.This evidence directs public policy to go beyond using aggregate indicators when planning.
Acknowledgements
The authors extend their appreciation to ICF International for allowing them to access the 2016 Uganda Demographic and Heathy Survey data.
Funding
This study received no specific grant from any funding agency, commercial entity or not-for-profit organization. However, the corresponding author is grateful to the College of Business and Management Sciences (CoBAMS), Makerere University, for the institutional grant, as research facilitation support, for staff.
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
This study used secondary data and the authors affirm that all procedures contributing to this work conform with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.





