Introduction
The use of games has increased at various levels, although this interest is not recent, and many have advocated the use of games to improve the human condition (Nacke and Deterding, Reference Nacke and Deterding2017). In the mid-2000s, the confluence of web technologies, digital models, and location-based online games gave rise to a growing interest in an expanding area (Nacke and Deterding, Reference Nacke and Deterding2017), resulting in an authentic Game Evolution. The evolution of games gave it another dimension — the appearance of Serious Games — designed for the main purpose other than pure entertainment. Despite its frank evolution in recent decades and close association with the idea of electronic games (Tsekleves et al., Reference Tsekleves, Cosmas and Aggoun2016), the term "Serious Games" arose before the digital age. At this level, we can find a variety of games that range from digital games, simulation, to role-play, which can be individual or multiplayer (Wattanasoontorn et al., Reference Wattanasoontorn, Boada and García2013). Games bring together participants with different perspectives and from different fields, such as communication, simulation, and training. Despite these differences, authors seem to agree on the basic components of Serious Games, namely having a “serious” dimension combined with a “game” dimension (Wilkinson, Reference Wilkinson2015).
Today, Serious Games have a strong presence in society, health, and well-being, and we can see their implementation in all these areas, especially health. This has led to recent years being characterized by a growing interest in using these resources to monitor, maintain, and improve human health (Silva et al., Reference Silva, Bermúdez i Badia and Cameirão2021), with increased use in healthcare aimed at a variety of end-users (Sharifzadeh et al., Reference Sharifzadeh, Kharrazi and Nazari2020). This is seen in many systems and applications that take advantage of the benefits of a playful and enjoyable experience to provide a technology-enabled health intervention (Silva et al., Reference Silva, Bermúdez i Badia and Cameirão2021). Serious Games also include simulation in general, for example, training simulations for health professionals, but explicitly emphasize the added pedagogical value of fun and competition (Sharifzadeh et al., Reference Sharifzadeh, Kharrazi and Nazari2020).
Although some authors might consider that not all activities and contexts lend themselves equally to being gamified, it is necessary to extend the use of gamification and systematically study its individual and situational effects in different contexts (Nacke and Deterding, Reference Nacke and Deterding2017), namely in palliative care. Palliative care can improve the quality of life for patients and their families through timely identification of health deterioration, holistic needs assessment, management of pain and other problems, and person-centered care planning (Murray et al., Reference Murray, Kendall and Mitchell2017). In addition, palliative care games can support the promotion of quality care, making it easier to understand the value of accompanying others (Alonso et al., Reference Alonso, Fernández Martínez and Presa2018), offering an innovative approach to overcome reluctance and resistance in discussing uncomfortable topics such as end-of-life care and death (Radhakrishnan et al., Reference Radhakrishnan, Van Scoy and Jillapalli2019).
According to Aldridge et al. (Reference Aldridge, Hasselaar and Garralda2016), it is necessary to overcome barriers to improved education on palliative care, both for health professionals and the public, leading to greater use and earlier improved integration of palliative care services for patients.
In embracing the principles of palliative care in their practice, health professionals must address the multidimensional needs of people with health deterioration more effectively (Murray et al., Reference Murray, Kendall and Mitchell2017). Games can also bring benefits at this level, softening the boundary between people, creating a relaxed environment for patients to disclose important information about themselves, and sharing emotional messages and instructions for professionals and family members (Pon, Reference Pon2010).
Despite the growing popularity of health games, no published reports discuss the use of games in palliative care. Review studies on palliative care were identified at this level, but these were aimed only at training (Pesut et al., Reference Pesut, Sawatzky and Stajduhar2014; Brighton et al., Reference Brighton, Koffman and Hawkins2017; Smith et al., Reference Smith, Macieira and Bumbach2018), and not in line with our view of mapping all types of games. This initiative is the first attempt to provide a historical overview of the use of all types of games involved in palliative care. Therefore, this review aims to identify and map the available evidence on the use of games in palliative care, analyzing how research has been conducted on this topic and identifing knowledge gaps.
Methods
Review design
This scoping review study was designed according to the steps provided by Joanna Briggs Institute (Peters et al., Reference Peters, Godfrey and Khalil2017):
• define the research objective and question;
• define inclusion and exclusion criteria;
• describe research planning;
• select, extract, and map evidence;
• search, select, extract, and map evidence; and
• finally, summarize, and analyze the evidence in relation to the research objective and question.
This review was guided by the research question: Which studies refer to the use of gamification in palliative care?
Criteria for study inclusion and exclusion
All articles that met the following inclusion criteria were selected: articles exploring the use of games, namely Serious Games, board games, card games, simulation games, and role-play games, regardless of their objective, and applied in palliative care. All types of publication, regardless of design, in English, Portuguese, French, and Spanish were included. No limits were applied regarding publication date, integrating adults aged 18 or over. Articles referring to the use of games with children were excluded.
Search strategy
The search was conducted in February 2021, using the following databases of specific subjects: CINAHL® and PUBMED®, which includes MEDLINE®, PsycINFO®, SCOPUS®, and SciELO®. Special attention was paid to keywords during navigation to ensure the consistency of searches in each of the databases, constructing the appropriate phrases for each of them. In addition, the truncation and Boolean logic used in all the databases allowed the research to be enhanced by creating new variations of the same word. The respective phrases are presented in Supplementary Appendix 1. The search for additional studies was also carried out in the reference lists of all publications included in the review (“Backward citation searching”).
Study selection and data extraction
The data selection was carried out by two authors independently, and disagreements were resolved by consensus with a third author to confirm the publications’ eligibility. The Rayyan QCRI® platform (Web Systematic Reviews) was used in the first stages of data selection to facilitate this process. Data extraction is presented in Tables 1–3. Data extraction was completed by two of the authors and verified by the third author. Differences of opinion between the two authors regarding the inclusion or exclusion of articles were resolved through a discussion with the third author, revisiting the inclusion and exclusion criteria for the selection of studies.
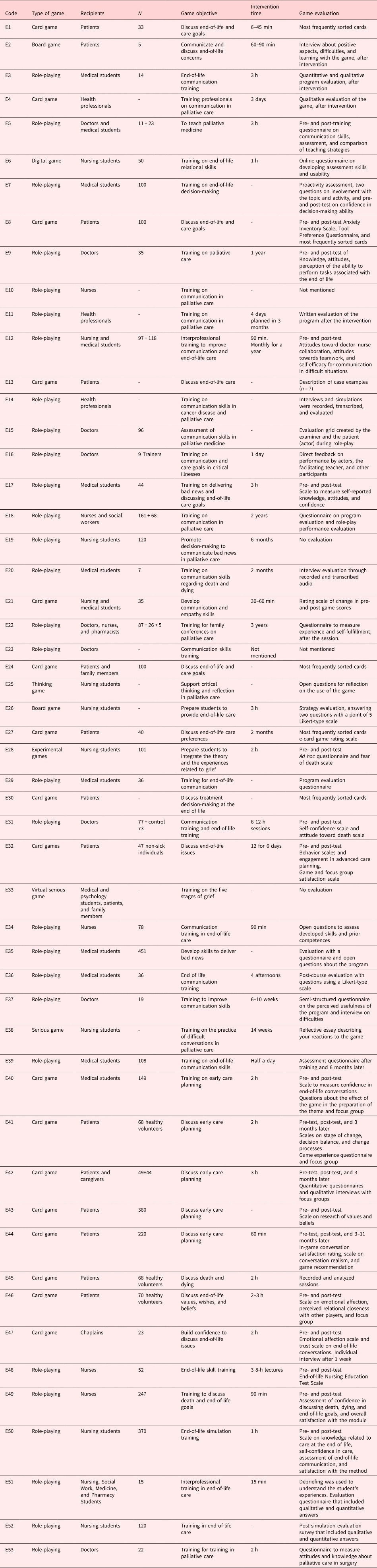
Table 1. Characteristics of studies in the scoping review (n = 53)

Table 2. Quality appraisal result

X: no, √: yes, 0: unclear, studies without evaluation: 10, 19, 23, 33.
Table 3. Games characteristics
Data analysis
In the first phase, the studies were selected for relevance by reading the title and summary, followed by the full reading of the studies identified, with subsequent integration of the final sample. To translate the respective stages of the identification and inclusion process of the articles, the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist was used (Figure 1). All articles that met the inclusion and exclusion criteria, or had abstracts with insufficient information available to determine if they met inclusion criteria, were moved to the full-text eligibility review phase. In this step, two of the reviewers separately evaluated 84 articles. A third reviewer resolved all discrepancies between the two reviewers in this phase. In total, 53 articles met the eligibility criteria. In order to systematize the information and facilitate the reading of the results, these were compiled in descriptive tables previously prepared by the researchers and coded as shown in Tables 1–3.

Fig. 1. Process of identification and inclusion of articles — PRISMA Flow Diagram
The methodological evaluation of the studies was carried out by two authors independently, using the different standardized assessment tools of the Joanna Brigg's Institute (JBI, 2020) for each type of study (Table 2). However, it was not the aim of the authors to eliminate studies based on these results. The rating level of each article is reported by study type; however, given the purpose of the review, none of the studies were eliminated based on this assessment.
Results
After duplicates were removed, the search resulted in 685 articles (Figure 1). Based on title and summary, 601 articles were excluded because they did not meet the objectives of this scoping review. The full text was read to assess eligibility for 84 articles, and 53 were included for the final analysis.
Table 1 summarizes the characteristics of the 53 studies included in the review, with regard to the authors, year, country, objectives, and study design.
Overview
As shown in Figure 2, most studies were conducted in the USA (n = 35), followed by England with five studies, Germany, France, Australia, and China with two studies each, and Spain, Switzerland, Japan, New Zealand, and Italy with one study each. The first publication was in 1993, with the largest increase in publications during the last decade. As for methodology, the studies present different methodologies, with the most frequent being quantitative studies of the descriptive type or mixed-methods studies. Table 2 presents the methodological evaluation scores of each study, according to the respective scales, with the exception of studies E10, E19, E23, and E33, which did not present results in the articles.

Fig. 2. Study characteristics
As previously mentioned, given the purpose of this review, none of the studies were excluded based on this assessment. However, we can observe that most studies have low scores, with none receiving scores for all items. Of the 53 studies, only 6 were randomized controlled trials (E7, E8, E18, E24, E31, E48), but with limitations due to the adequacy of baseline similarity of the groups and blinding of participants, evaluators, and results.
Table 3 summarizes studies presenting game type, recipients, game objective, intervention time, and game evaluation. The most frequent game type used was role-playing (n = 29), followed by card games (n = 17). The games were principally aimed at patients (n = 14), and in some cases extended to families (E24) or caregivers (E42), as well as medical students (n = 10) and nurses (n = 8). The sample sizes ranged from 5 to 451, with a total of 4,324 participants. Some studies did not reference sample size. Concerning the games’ objectives, most focused on training (N = 40). The intervention time ranged from 15 min to 1 year, and some studies did not specify this. The methodologies used to assess the games were very diverse, and in some studies were even absent (E10, E19, E23, E33). Nonetheless, the majority used pre- and post-test mechanisms (n = 19). Regarding the evaluation of the results in the studies, all refer to advantages with the application of different strategies. Only study E48 reported that no significant differences were found between the groups, despite the positive appreciation of the program. On the other hand, some studies mention participants’ discomfort with the use of role-play representation (E11, E17, E20, E35, E37), despite the positive impact of the intervention.
Games characteristics
The analysis of the games included in this review resulted in two major themes: the use of role-playing for training in palliative care and the use of card games to discuss end-of-life care. Although some authors used other games [e.g., board games (E2, E26), Serious Games, and digital games (E6, E25, E28, E33, E38)], these had less expression.
Of the 53 articles, 29 used role-plays, mostly to develop communication skills and for planning end-of-life care. In this context, the use of role-play mainly was addressed to health professionals (n = 19), namely physicians (E9, E15, E16, E23, E31, E37, E53), nurses (E10, E34, E48, E49), or several other professions (E11, E14, E22). Some were also aimed at students in their training processes (n = 10): in medicine (E3, E5, E7, E17, E20, E29, E35, E36, E39), in nursing (E19, E50, E52), or other (E12, E51). However, in the context of palliative care, its objective was mostly to develop communication skills at the end of life (E3, E10, E11, E12, E14, E15, E16, E18, E20, E23, E29, E31, E34, E36, E37, E39). Other objectives included training in palliative care (E5, E9, E48, E53), training in decision-making at the end of life (E7, E19, E31; E34, E49, E50, E51, E52), care goals (E16, E17), training on how to break bad news (E17, E35), and training for family conferences on palliative care (E22).
Card games were used in 17 of the 53 articles and were mostly used to discuss care. Card games were mostly addressed to patients (n = 13), or in some cases extended to the family (E24) or caregiver (E42). In some cases, even though the ultimate goal was the use with patients, it was used to train health professionals [health professionals (E4), nursing and medical students (E21) and medical students (E40), and chaplains (E47)] for its use. The card games used were the “Go Wish®” card game (E1, E8, E13, E24) and the “My Gift Grace®” card game (E33, E41, E45, E47).
Discussion
Principal findings
The objective of this scoping-type review was to identify and map the available evidence on the use of games in palliative care, analyzing how research has been conducted on this topic, and identifying knowledge gaps. From a total of 685 articles initially identified, 53 articles were included in this review. The observation of the articles in this review shows an increase in their use, with the first study identified in 1993. However, the methodological analysis of the studies, and the types of method used, identified gaps for the validation of results obtained. Randomized studies with a control group that could prove the effectiveness and impact of the game should be favored. Similar results are reported by other authors who report that the impact assessment of games with single-arm studies has a great potential for bias, where results are usually measured before and after the intervention or only after the intervention (Wang et al., Reference Wang, DeMaria and Goldberg2016; Gauthier et al., Reference Gauthier, Kato and Bul2019). In addition, the heterogeneity of measures used and the behavior measures used are particularly vulnerable to biases because they can be associated with social or behavioral stigmas (Gauthier et al., Reference Gauthier, Kato and Bul2019) (better communication, ethical behavior, etc.). Therefore, to correctly analyze the functioning of these games, control groups should be included, and this requirement is even more necessary in educational interventions (Wang et al., Reference Wang, DeMaria and Goldberg2016). Another interesting finding that emerged from our review is the imbalance in the methodological aspects of using games. In Table 3, we can observe that the authors’ strategies to assess the use of games in their interventions are highly variable and sometimes non-existent. Most studies evaluated the impact and effectiveness of the game on the result of training and not the game itself. This may be related to what Berger et al. (Reference Berger, Fenies and Pizot2014) wrote, noting that end-of-training evaluations show the difficulty in differentiating the game's impact from the program content.
Finally, two major themes resulted for the type of game used: role-playing for training in palliative care and card games to discuss end-of-life care.
Role-playing for training in palliative care
The purpose of role-play is to portray situations rather than simply describe them. That is, participants assume the role of the other, allowing them to develop understanding and empathy for the other's point of view (Baile et al., Reference Baile, De Panfilis and Tanzi2012). In role-play, participants play the role of another, in a “role training” that focuses on preparing individuals for their professional responsibilities (Tanzi et al., Reference Tanzi, De Panfilis and Costantini2020). Most studies reviewed used role-play to educate health professionals, mostly doctors and nurses. Similar results were found in a review study on the use of simulation to teach nursing students and physicians in palliative care, in which the majority used role-play using roles played by other people, including actors (Smith et al., Reference Smith, Macieira and Bumbach2018). As well as, in the review study developed by Brighton et al. (Reference Brighton, Koffman and Hawkins2017) on communication and end-of-life skills training, and in the study by Pesut et al. (Reference Pesut, Sawatzky and Stajduhar2014) on training nurses in palliative care. Research suggests that game-based education, notably using role-play, encourages motivation and drives academic progress, integrating challenge, narrative, and collaboration within the overarching theme of character and player development.
Role-play allows participants to explore attitudes and feelings as part of professional development. The objective is to rehearse situations to improve the participant's abilities to face similar situations in clinical practice (Rønning and Bjørkly, Reference Rønning and Bjørkly2019). Despite the listed advantages, some authors noted some difficulties, considering them stressful (Hawkins and Tredgett, Reference Hawkins and Tredgett2016), with participants feeling embarrassed at being observed (Baile et al., Reference Baile, De Panfilis and Tanzi2012), or referring to being unrealistic (Tanzi et al., Reference Tanzi, De Panfilis and Costantini2020). The majority (n = 16) focused on developing communication skills, an essential skill in palliative care. Indeed, effective communication about death and dying is a crucial skill for health professionals and a significant aspect of quality care in the field of palliative care (Hamilton et al., Reference Hamilton, Ortega and Hochstetler2014). According to Leeson and Gibbs (Reference Leeson and Gibbs2019), role-play games are being used to develop collaboration and communication skills, and their educational potential increases when combined with a final debriefing period. These aspects can overcome the barriers of communication difficulties with patients and their families and find the best method to teach palliative care (Aldridge et al., Reference Aldridge, Hasselaar and Garralda2016).
Card games to discuss end-of-life care
Card games were used in 17 of the identified studies. These card games consisted of question cards that prompt players to discuss their views on death and end-of-life planning issues (Van Scoy et al., Reference Van Scoy, Reading and Scott2016b). Card games allow patients to consider the importance of debating common end-of-life problems in a non-confrontational environment, ranking their values, and facilitating a focused conversation about end-of-life care (Lankarani-Fard et al., Reference Lankarani-Fard, Knapp and Lorenz2010). These games offer an innovative approach to overcoming reluctance and resistance to discussing uncomfortable topics about end-of-life care, death, and dying (Radhakrishnan et al., Reference Radhakrishnan, Van Scoy and Jillapalli2019).
The games used were mainly the “Go Wish®” card game (E1, E8, E13, E24), which consists of a set of 35 cards where patients are asked to place each card in one of the three importance categories (“very important,” “something important,” or “not at all important”) according to their preference (Lankarani-Fard et al., Reference Lankarani-Fard, Knapp and Lorenz2010). The results serve as the basis for a discussion focused on end-of-life care goals (Kaplan, Reference Kaplan2016). This game is an advanced care planning tool designed to help people have conversations about end-of-life care, giving voice to patients’ needs and concerns and providing a means to share those ideas (Menkin, Reference Menkin2007).
Another game mentioned in several studies was the card game “My Gift Grace®” (E33, E41, E45, E47), which consists of 47 cards with questions that encourage players (groups of 4–6) to discuss topics related to quality of life, end-of-life planning, values and preferences about medical care, spirituality, among others (Van Scoy et al., Reference Van Scoy, Watson-Martin and Bohr2018). The game is played by taking turns reading the cards aloud, the players writing their answers, and then sharing them with the group. Players can skip any questions if they wish (Van Scoy et al., Reference Van Scoy, Reading and Scott2016a). The game “My Gift Grace®” is a tool to facilitate meetings with discussions related to advanced care planning (Radhakrishnan et al., Reference Radhakrishnan, Van Scoy and Jillapalli2019).
The use of the card game in palliative care is referred to as a facilitator for expressing feelings and emotions (Pazart et al., Reference Pazart, Vidal and Chalon2011; Delgado-Guay et al., Reference Delgado-Guay, Rodriguez-Nunez and la Cruz2016). The authors in some studies noted that the use of card games to discuss sensitive topics does not increase anxiety (DeVita et al., Reference DeVita, Arnold and Barnard2003; Van Scoy et al., Reference Van Scoy, Reading and Scott2016a) and has no negative effects on the emotional state of participants after the game (Van Scoy et al., Reference Van Scoy, Reading and Scott2016a).
Implications for palliative care
Games can facilitate improvements in palliative care provided to people, both in its training component and integrated to meet the real needs of people and families.
Role-play works as a facilitating agent, helping students understand and articulate the hidden feelings of fear and loss behind the person's and family's emotional reactions (Baile and Walters, Reference Baile and Walters2013). Grudzen et al. (Reference Grudzen, Emlet and Kuntz2016) highlight many other advantages, including role-modeling and the practice of skills, the improvement of care provided to people in palliative care, the increase of self-efficacy of health professionals, the development of effective strategies to communicate bad news, and conduct care planning, as well as avoiding situations to escape from confronting the family and clarifying doubts. These strategies can enhance health professionals’ communication skills. Moreover, by developing effective communication skills, they improve the experiences of patients and families (Hawkins and Tredgett, Reference Hawkins and Tredgett2016).
The use of card games to discuss care allows the patient and family to find their own answers. It is seen as a simple tool to initiate discussions about people's end-of-life wishes (Delgado-Guay et al., Reference Delgado-Guay, Rodriguez-Nunez and la Cruz2016), proving to be a pleasant and positive experience (Van Scoy et al., Reference Van Scoy, Reading and Scott2016a) without increasing anxiety (Van Scoy et al., Reference Van Scoy, Watson-Martin and Bohr2018). Topics likely to be discussed during the game are substantive and address important issues in early care planning (Van Scoy et al., Reference Van Scoy, Reading and Scott2016b).
Given these data, further studies are needed to assess the effectiveness of these interventions in the quality of care.
Study strengths and limitations
A strong point of this review is that it was carried out without time limits, and the first article was published in 1993. To the best of our knowledge, this is the first initiative that provides a historical overview of the use of all types of games involved in palliative care, namely, Serious Games, board games, card games, simulation games, RPG games, among others. This allowed us to list a variety of studies.
Limitations of our study include the methodological variability of the studies and the lack of prioritization of the quality assessment of the included studies. This aspect was related to the review's objective, which was to cover all studies that used games in palliative care to ensure comprehensive coverage. As mentioned above, we can observe that most studies have low scores for the assessment of methodological quality. Of the 53 studies, only six were randomized clinical trials, highlighting that more randomized clinical trials reporting results from the use of games are needed. Another relevant aspect to consider in future studies is that the methodologies used to assess the games and their impact were very diverse, even absent in some studies.
According to Calderón and Ruiz (Reference Calderón and Ruiz2015), all the following items should be evaluated in game interventions: user interface, game design, user's satisfaction, usability, usefulness understandability, motivation, performance, playability, pedagogical aspects, learning outcomes, engagement, user's experience, efficacy, social impact, cognitive behavior, enjoyment, and acceptance.
Conclusion
The use of games in palliative care has been recognized, especially in the last decade, due to their potential for training and meeting the needs of patients and families. This review identified two major themes for games: role-playing for training in palliative care and card games to discuss end-of-life care. Our analysis suggests that more of these resources adapted to the needs of individuals and families can still be developed and applied. However, a more rigorous methodology for game evaluation must be considered, as some studies did not provide in-depth evaluation, and large variability of instruments was used in literature making it difficult to assess their effectiveness.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951521001929.
Funding
The authors received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors for this research.
Conflict of interest
There were no conflicts of interest related to the study.








