Introduction
A variety of approaches has been recommended for treating posttraumatic stress disorder (PTSD), including pharmacotherapies and psychotherapies. However, previous meta-analyses suggest that psychotherapies are superior to pharmacological treatments in treating people with PTSD (Merz, Schwarzer, & Gerger, Reference Merz, Schwarzer and Gerger2019). Numerous PTSD practice guidelines have been developed either by global or national scale organisations (Card, Reference Card2017; Greenberg, Megnin-Viggars, & Leach, Reference Greenberg, Megnin-Viggars and Leach2019; Phelps et al., Reference Phelps, Lethbridge, Brennan, Bryant, Burns, Cooper and Silove2022). Based on the guidelines, cognitive processing therapy (CPT), cognitive therapy (CT), prolonged exposure (PE), and cognitive behaviour therapy (CBT) were considered as strongly recommended therapies for PTSD while eye movement desensitisation reprocessing (EMDR), narrative exposure therapy (NET), and brief eclectic psychotherapies (BEP) were suggested or conditionally recommended (Courtois et al., Reference Courtois, Brown, Cook, Fairbank, Friedman, Gone and Kurtzman2017).
Although there are previous pairwise meta-analyses that have been conducted to evaluate the efficacy of psychotherapies for PTSD (Chen, Zhang, Hu, & Liang, Reference Chen, Zhang, Hu and Liang2015; Kayrouz et al., Reference Kayrouz, Dear, Kayrouz, Karin, Gandy and Titov2018; Lenz & Hollenbaugh, Reference Lenz and Hollenbaugh2015; Lenz, Haktanir, & Callender, Reference Lenz, Haktanir and Callender2017; Moreno-Alcázar et al., Reference Moreno-Alcázar, Treen, Valiente-Gómez, Sio-Eroles, Perez, Amann and Radua2017; Powers, Halpern, Ferenschak, Gillihan, & Foa, Reference Powers, Halpern, Ferenschak, Gillihan and Foa2010), conventional pairwise meta-analysis can only compare two different treatments or formats on direct effects. Among the numerous therapies used to treat PTSD, exploring and identifying the most effective, reliable, and acceptable treatment would provide better evidence for clinicians in choosing the best intervention in the management of PTSD. Network meta-analysis (NMA), also called mixed treatment comparisons meta-analysis, has been widely used recently to identify and rank the most effective intervention among multiple treatment approaches. Additionally, NMA providing direct and indirect effects simultaneously in a single analysis expands from the conventional pairwise meta-analysis by strengthening the inferences on the relative effects of two treatments (Lu & Ades, Reference Lu and Ades2004). According to the WHO (World Health Organization), the ability of the NMA to make quantitative comparisons of interventions that have not been directly compared in studies is essential for the development of guidelines (Kanters et al., Reference Kanters, Ford, Druyts, Thorlund, Mills and Bansback2016).
Previous NMAs have focused on the comparative effectiveness of PTSD psychotherapies on children and adolescents (Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Stockton, Meiser-Stedman and Pilling2020a) and adults (Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Welton, Stockton and Pilling2020b). However, previous NMA evidence was limited by (1) focusing on children and adolescents and (2) no previous NMA studies explored the short-term and long-term effectiveness in adults with PTSD. Thus, evaluating the long-term effectiveness of psychotherapies for PTSD would provide comprehensive and detailed evidence on the follow-up effects of PTSD psychotherapies. Therefore, this NMA aimed to explore and determine the comparative effectiveness of nine psychotherapies in treating adults diagnosed with PTSD at immediate post-treatment, short-and-long-term follow-up measurements using randomised controlled trials (RCTs) to extend previous evidence. We examined whether outcomes differed by time measurements at (1) immediate post-treatment, (2) short-term (<6-month follow-up) and (3) long-term effects (⩾6-month follow-up). In addition, we also evaluated the proportion of loss of diagnosis as an outcome after successful therapy for comparison of the effectiveness of PTSD psychotherapies.
Methods
Search strategy
The literature was identified in Cochrane library, Embase, Medline-OVID, PubMed, Scopus, and PsycInfo up to January 2021. The search was conducted using medical subject heading terms for all RCTs that focussed on determining the effectiveness of PTSD psychotherapies towards people diagnosed with PTSD without date and language restrictions (online Supplement 1). We also conducted a manual search through Google Scholar and references from previous meta-analyses and/or systematic reviews (Asmundson et al., Reference Asmundson, Thorisdottir, Roden-Foreman, Baird, Witcraft, Stein and Powers2019; Chen et al., Reference Chen, Zhang, Hu and Liang2015; Forman-Hoffman et al., Reference Forman-Hoffman, Middleton, Feltner, Gaynes, Weber, Bann and Green2018; Lely, Smid, Jongedijk, Knipscheer, & Kleber, Reference Lely, Smid, Jongedijk, Knipscheer and Kleber2019; Lenz & Hollenbaugh, Reference Lenz and Hollenbaugh2015; Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Stockton, Meiser-Stedman and Pilling2020a, Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Welton, Stockton and Pilling2020b; Zhou et al., Reference Zhou, Sun, Wang, Wu, Sun, Zhang and Liu2020) to find other potential articles. This study was registered in the international database of prospective registered systematic reviews (PROSPERO) with registration number: CRD42020162143. The reported of this study utilised the PRISMA Extension Statement for NMA (Hutton et al., Reference Hutton, Salanti, Caldwell, Chaimani, Schmid, Cameron and Moher2015).
Selection procedure
A systematic screening was independently carried out by two reviewers and any difference in opinion about the eligibility of the study was resolved by discussion with an expert reviewer. A study was selected and included if it met the study PICOS criteria:
Population variable
Participants were adult's ⩾18 with PTSD as the primary diagnosis either defined according to DSM by APA, ICD by WHO, or validated by PTSD assessment tools. Study subjects could also have a comorbid mental disorder or condition as long as PTSD was the primary diagnosis.
Intervention variables
This study focused on determining the clinical importance of included therapies, CPT, CT, EMDR, NET, PE, CBT, present-centred therapy (PCT), BEP, psychodynamic therapy (PDT) or any combination among them. The psychotherapies included in this study were chosen based on the APA and DoD's PTSD guidelines (Courtois et al., Reference Courtois, Brown, Cook, Fairbank, Friedman, Gone and Kurtzman2017) with more details provided in the online Supplement 2. In terms of psychopharmacotherapy, a study was included only if the participant maintained stable medication types and dosages before and during the study.
Comparison variables
Studies that determined psychotherapies' effectiveness were included in the analysis when comparisons used control conditions including waitlist/no treatment (NT), standard care/treatment as usual (TAU), and other guideline-recommended interventions (CPT, CT, EMDR, NET, PE, CBT, PCT, BEP, PDT). Studies were excluded when comparison therapies were beyond the scope of the current NMA.
Outcome variables
The primary outcome for this study was the change of PTSD symptoms score from baseline to immediate post-treatment, short-term (<6-month), and long-term (⩾6-month) follow-up measurements. PTSD symptoms changes from observer-rated measurements were prioritised over self-reported. Intention to treat (ITT) was prioritised over per-protocol (PP) if both were available in a study. Data from the latest observation were preferred if there were more than one observation in short-term or long-term follow-up measurements.
Secondary outcomes were (1) loss of diagnosis, (2) retention rate, (3) anxiety, and (4) depression symptoms. The loss of diagnosis referred to the number of participants that no longer met PTSD diagnosis criteria at post-treatment (Morina, Wicherts, Lobbrecht, & Priebe, Reference Morina, Wicherts, Lobbrecht and Priebe2014). A higher proportion of loss of diagnosis represents more effective psychotherapies to achieve better end-state functioning. Retention rate referred to the percentage of participants who stayed in treatment for its intended dose (Najavits, Reference Najavits2015). The retention rate was calculated using the total number of participants until the last observation time in the studies divided by the total number of participants in the studies. High retention rate represents a successful therapy and research (Dacosta-Sánchez, González-Ponce, Fernández-Calderón, Sánchez-García, & Lozano, Reference Dacosta-Sánchez, González-Ponce, Fernández-Calderón, Sánchez-García and Lozano2022). Based on the availability of data, both proportion of loss of diagnosis and retention rate were analysed at the post-treatment measurement. Both anxiety and depression symptoms were analysed at immediate post-treatment, short-term, and long-term follow-up measurements. Both, anxiety and depression symptoms, refer to the immediate post-treatment, short-term, and long-term follow-up measurements with symptom score changes from observer-rated measurements being prioritised over self-reported. Data based on ITT were prioritised over PP if both were available in a study.
Study design
We included articles with RCTs study design that had been published in peer-reviewed journals without any restriction related to the number of arms, blinding, and the availability of follow-up measurement. RCTs with crossover design were included with the first phase data being used for the analysis.
Data extraction
All eligible studies data were extracted into study identifier (author and year of publication), participant characteristics, therapy characteristics, outcomes, and study characteristics. For each study, the summary of outcomes, including sample size, pre-post mean difference, standard deviations, number of patients with loss of PTSD diagnosis and retained were extracted and documented into a separate excel file. We contacted the corresponding authors if there was missing or unclear data needed. If the s.d. data was unavailable, we calculated it from the sample size, 95% confidence interval, s.e., or using a well-validated method.
Quality assessment
The risk of bias of individual studies was assessed using the risk of bias using Cochrane RoB 2.0 to cover the five domains that are known to affect the results of RCTs and we categorised the articles as low risk, some concern, or high risk of bias. We created a RoB contribution matrix using Confidence in Network Meta-Analysis framework (CINEMA) to describe each pairwise contribution to the NMA risk of bias.
The certainty of evidence was analysed using the Grading of Recommendation Assessment Development and Evaluation (GRADE). Five domains, including risk of bias, inconsistency, indirectness, imprecisions, and other considerations (publication bias) were assessed to rate the certainty of evidence. The certainty of evidence was divided into four levels of quality which were (1) high (⨁⨁⨁⨁), (2) moderate (⨁⨁⨁), (3) low (⨁⨁) and (4) very low (⨁). We conducted Cohen Kappa to test differences between raters for GRADE analysis. The results were classified into six categories (1) 0 = no agreement, (2) 0.01–0.20 = slight agreement, (3) 0.21–0.40 = fair agreement, (4) 0.41–0.60 = moderate agreement, (5) 0.61–0.80 = substantial agreement, and (6) 0.81–1.00 = almost perfect agreement (McHugh, Reference McHugh2012).
Statistical analysis
A key feature of the NMA is the indirect treatment comparison technique to compare two treatments indirectly in situations where there is one or more comparator or linking treatments. For example, there is an interest in performing an indirect comparison of treatment A v. B. If trials have separately compared A v. C in trial 1 and compared B v. C in trial 2 then the indirect effect of treatment A v. B can be calculated from trials 1 and 2 through the linking treatment C. In addition, if there's a trial 3 comparing treatment A v. D and trial 4 comparing treatment B v. D, the indirect effect of treatment A v. B can also be calculated from linking treatment D in trials 3 and 4. The NMA also allows for the amount of agreement between results when different linking treatments are used.
The network evidence was calculated based on the frequentist approach adopting the random-effects model using the netmeta package in R (version 4.0.2) (R Core Team, 2020). Q statistics, I 2, and τ 2 were used to report heterogeneity in the NMA. We also assessed the inconsistency between direct and indirect effects using two methods including (1) node splitting and (2) design by treatment interaction model with a p value less than 0.05 considered as significant inconsistency. We estimated the effect size of treatments compared with NT by using standardised mean difference (SMD), 95% confidence intervals (CI), and mean rank. SMD 0.2, 0.5, and 0.8 were considered as small, moderate, and large effect sizes (Cohen, Reference Cohen2013; Faraone, Reference Faraone2008; Lakens, Reference Lakens2013). In addition, we provided 95% prediction intervals (PrI), which gives the range of where the results of similar future studies might lie (Lin, Reference Lin2019). We also calculated the p score to estimate the best to least ranked treatment (Rücker & Schwarzer, Reference Rücker and Schwarzer2015). Regarding publication bias, a comparison-adjusted funnel plot by the order of appearance of the interventions (Salanti, Del Giovane, Chaimani, Caldwell, & Higgins, Reference Salanti, Del Giovane, Chaimani, Caldwell and Higgins2014) was produced by the netmeta package. Publication bias was considered if there were more studies on the outside than inside the comparison-adjusted funnel. Furthermore, Egger's regression test was also conducted to evaluate the existence of publication bias with a p value of less than 0.05 indicating presence of publication bias (online Supplement 3).
Moderator and sensitivity analyses
Moderator and sensitivity analysis were calculated based on random-effects model with the gemtc package using the Bayesian approach. This study used meta-regression models for NMA to determine the efficacy of psychotherapies based on gender, the continent of study, and diagnosis criteria. For gender, we classified studies into two groups as follows: female majority if studies had more than or equal to 50% female participants and vice versa. For continents, we divided studies into five continents as follows, America, Asia, Australia, Africa, and Europe. For the diagnostic criteria, studies were divided into three categories, DSM-III/R, DSM-IV/R/TR, and DSM-5. Risk of bias was classified into three groups which were low, some concern and high. The moderator effect's occurrence was based on a significant change in the deviance information criterion (DIC). DIC is the Bayesian version of the Akaike information criterion (AIC) which is concerned with how replicated data predict the observed data, or how good is the model fit. AIC and DIC estimate the relative amount of information lost by a given model and measures the quality of the model based on how much information it loses. The NMA model with lower scores of DIC suggests a better model fit compared with the other NMA model (Chaimani & Salanti, Reference Chaimani and Salanti2012). A 10-point lower DIC from initial model indicates significant different results or moderator effect (online Supplement 3).
To check the robustness of the study's findings, sensitivity analysis was conducted. We combined treatments, CT, CPT and PE, the specific type of CBT that was developed for a population with a certain problem. The analysis was conducted in three different levels, first we combined CBT and CT, second CBT, CT, and CPT and last CBT, CT, CPT and PE. We then evaluated the significant change of treatment effect size (SMD) of the initial model and compared the DIC (online Supplement 3).
Results
Studies and treatments
After the removal of duplicate studies, 18 987 studies were found in databases and manual searches. About 17 128 studies were excluded based on title and abstract, and 506 full-text articles were retrieved for further consideration. Finally, 98 RCT's published from 1990 to 2020 involving 5567 participants with nine therapies including (1) CPT, (2) CT, (3) EMDR, (4) NET, (5) PE, (6) CBT, (7) PCT, (8) BEP, (9) PDT, and two types of control NT and TAU were included in this NMA (Fig. 1). One non-English language publication could not be used because the authors did not reply to email requests. Detailed characteristics of the included studies in the analysis have been provided in online Supplement 4 and the reference list in online Supplement 5.
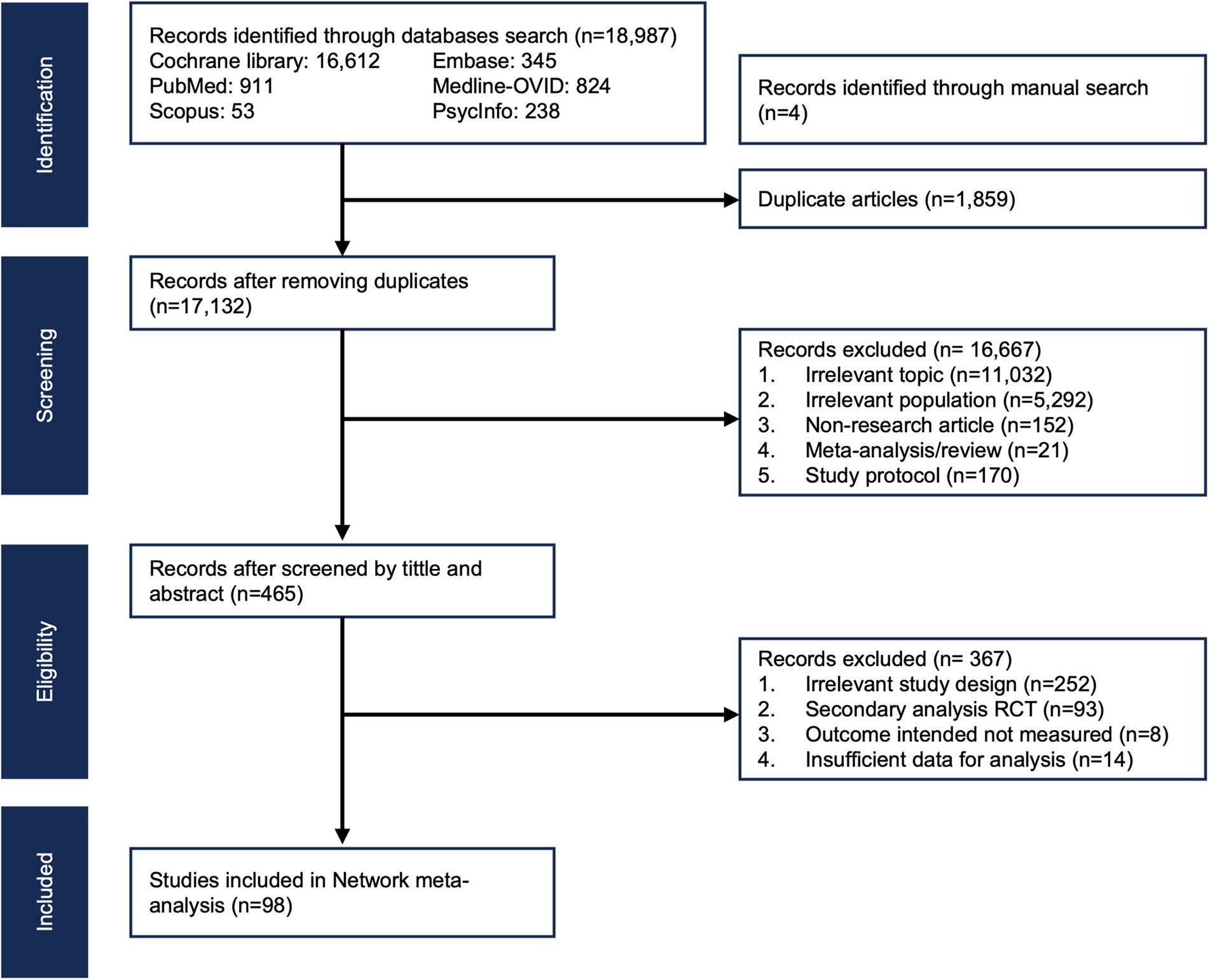
Fig. 1. PRISMA flowchart. This figure illustrating identification and screening process of eligible studies to be included in this network meta-analysis of psychotherapies for PTSD. Study size (n); RCT, Randomised control trials; CBT, Cognitive behaviour therapy; CPT, Cognitive processing therapy; CT, Cognitive therapy; EMDR, Eye movement desensitisation and reprocessing; NET, Narrative exposure therapy; PCT, Present centred therapy; PDT, Psychodynamic therapy; PE, Prolonged exposure; BEP, Brief eclectic psychotherapy; TAU, Therapy as usual; NT, No treatment; Figures was created by the authors.
NMA model fit
The network plot of the post-treatment meta-analysis showed the nodes along with direct and indirect effects of interventions and comparisons. The width of the lines was proportional to the number of trials involved in each comparison. CBT had the majority of studies compared to other therapies. Pairwise meta-analysis conducted on 109 direct and indirect comparisons in post-treatment showed that all interventions but PDT were superior compared to NT. In the analysis between psychotherapies, direct comparisons were relatively few and not strongly attached to the network, as was the combination among them. Both inconsistency checks using loop and design by treatment interaction model showed that there was no inconsistency between direct and indirect effect with p values more than 0.05. This result showed that the NMA model had a good model fit.
Primary outcome: PTSD symptoms
Baseline to endpoint
Evidence from 89 studies was retrieved for analysis of PTSD symptoms at immediate post-treatment. CPT, CT, NET, EMDR, PE, CBT, and PCT had statistically significant effect on improving PTSD symptoms with moderate to large effect size (SMD range −1.53 to −0.75), while BEP and TAU showed no significant effect and PDT had a positive direction with high heterogeneity (I 2 = 76.9%; τ 2 = 0.266). Rank analysis found CPT, EMDR, and CT as the most effective therapies (upper quartile) with respect to NET and PE (second quartile) and CBT and PCT (third quartile) (Table 1).
Table 1. Estimates of effect, certainty, and rank for psychotherapies effectiveness in PTSD symptoms at immediate posttreatment and loss of PTSD diagnosis

PTSD, Posttraumatic stress disorder; CI, Confidence interval; CPT, Cognitive processing therapy; EMDR, Eye movement desensitisation and reprocessing; CT, Cognitive therapy; NET, Narrative exposure therapy; PE, Prolonged exposure; CBT, Cognitive behaviour therapy; PCT, Present centred therapy; BEP, Brief eclectic psychotherapy; TAU, Treatment as usual; PDT, Psychodynamic therapy
Explanatory footnotes
1 major concern heterogeneity
2 major concern imprecisions since the 95% CI crosses unity
Effect size, 0.2 (small); 0.3 (medium); 0.8 (large);
1.3 (very large) (Cohen's d).
Baseline to longitudinal follow-up
In the short-term follow-up, 30 studies were included in the analysis. The results revealed that EMDR, CPT, CT, CBT, PE, and NET showed statistically significant effect on improving PTSD symptoms with moderate to large effect size (SMD range −1.02 to −0.39) with moderate heterogeneity (I 2 = 55.9%; τ 2 = 0.072), while PCT and TAU showed no significant effect. According to the rank analysis, EMDR and CPT were the most effective therapies (upper quartile) followed by CT and CBT (second quartile) then PE and PCT (third quartile) (Table 2).
Table 2. Estimates of effect, certainty, and rank for psychotherapies effectiveness in PTSD symptoms at short-term and long-term follow-ups

PTSD, Posttraumatic stress disorder; CI, Confidence interval; CPT, Cognitive processing therapy; EMDR, Eye movement desensitisation and reprocessing; CT, Cognitive therapy; NET, Narrative exposure therapy; PE, Prolonged exposure; CBT, Cognitive behaviour therapy; PCT, Present centred therapy; BEP, Brief eclectic psychotherapy; TAU, Treatment as usual; PDT, Psychodynamic therapy
Explanatory footnotes
Effect size, 0.2 (small); 0.3 (medium); 0.8 (large);
1.3 (very large) (Cohen's d).
In the long-term follow-up, 19 studies were included in the analysis. The results found that CPT and EMDR showed statistically significantly effect on improving PTSD symptoms with moderate to large effect size (SMD range −0.85 to −0.64) with moderate heterogeneity (I 2 = 68.9%; τ 2 = 0.111). While PE, CBT, PCT, CT, BEP, and PDT showed no significant effect. Rank analysis found both CPT and EMDR as the most effective therapy for PTSD symptoms (upper quartile) (Table 2).
Secondary outcomes
Loss of PTSD diagnosis
In terms of loss of diagnosis, 46 studies were included in the analysis. According to Table 1, NET, CPT, EMDR, CBT, PE, BEP, CT, and PCT showed significant proportion of loss of PTSD diagnosis (RR range 5.51 to 1.70) compared to NT with high heterogeneity (I 2 = 77.6%; τ 2 = 0.037). Our rank analysis found that NET, CPT, and EMDR (upper quartile) were the therapy with highest proportion of loss of diagnosis with regards to CBT and PE (second quartile), BEP and CT (third quartile), and PCT (fourth quartile) (Table 1).
Retention rate
Evidence from 78 studies found a lower different retention rate. CT, NET, EMDR, PCT, PDT, CPT, and BEP were not significantly different compared to NT (RR range 1.00 to 0.79) with moderate heterogeneity (I 2 = 62.8%; τ 2 = 0.011), while CBT and PE were statistically significant. Rank analysis found that only CT (upper quartile) as most effective therapies in retained participants of studies followed by NET and EMDR (second quartile), PCT and PDT (third quartile), and PE and BEP (lower quartile) (online Supplement 6).
Anxiety
Forty-eight studies were included in the analysis to measure the effectiveness of treatments toward anxiety at immediate post-treatment. The analysis found NET, CT, CBT, EMDR, and PE had significant effect with moderate to large effect size (SMD range −1.25 to −0.52) with high heterogeneity (I 2 = 92.9%; τ 2 = 5.66) (online Supplement 6). Meanwhile, only EMDR, CBT, and CT showed significant effect on anxiety in the short-term and long-term follow-ups accordingly.
Depression
Evidence from 68 studies found that CPT, CT, EMDR, NET, PE, and CBT had significant effect compared to NT with moderate to large effect size (SMD range −1.46 to −0.70) with high heterogeneity (I 2 = 80.7%; τ 2 = 3.929) (online Supplement 6). In longitudinal data analysis, CPT, EMDR, and CBT showed significant effect on depression in short-term follow-up while only CPT was found as a significant therapy in the long-term follow up.
Quality assessment
Overall results showed that 24.7%, 41.6%, and 33.7% of studies had low, some concern, and high risk of bias, respectively. Twenty-five comparisons were performed to evaluate certainty based on contribution matrix risk of bias, inconsistency, indirectness, imprecisions, and publication bias of each comparison. GRADE NMA analysis from direct, indirect, and network evidence revealed that 4, 1, 3, and 2 therapies showed high, moderate, low, and very low certainty (Table 1). Cohen kappa test of GRADE analysis for all domains showed 92.6% agreement among ratters.
Publication bias
Publication bias assessment was conducted on post-treatment measurement of PTSD by adjusting the covariates. Therapies were arranged based on APA recommendation order prior by CBT, CPT, CT, PE, BEP, EMDR, NET, PCT, PDT, TAU and NT. Although the distribution of included studies was equal in both sides of the funnel, yet the results from Egger regression analysis showed significant publication bias with p value = 0.0009 (online Supplement 7).
Moderator and sensitivity analyses
Our study utilised four different models for moderator analysis that included gender, RoB, continent of study, and diagnostic criteria. Among all models of moderator analysis, none of the adjusted models showed significant increasing or decreasing DIC score (Table 3).
Table 3. Model fits of moderator analyses

CPT, Cognitive processing therapy; CT, Cognitive therapy; CBT, Cognitive behaviour therapy; EMDR, Eye movement desensitisation and reprocessing; NET, Narrative exposure therapy; PCT, Present centred therapy; PDT, Psychodynamic therapy; PE, Prolonged exposure; BEP, Brief eclectic psychotherapy; TAU, Therapy as usual; NT, No treatment; MD, Mean different; DIC, Deviance information criterion; MD, Mean different; CI, Confidence interval; β, Beta coefficients.
Note: β represent the effect of moderator in the NMA result from meta-regression using Bayesian approach of NMA. Unadjusted value was obtained using Bayesian NMA without adjusting for specific risk factors. Adjusted value was obtained after adjusting for different risk factors. We choose the adjusted model if there was DIC value difference more than 10 points between adjusted and unadjusted model. Model A using percentage of gender (male & female) as moderator; Model B using risk of bias (low, some concern, & high) each study as moderator variable; Model C using five different type of continent as moderator variable (African, American, Asian, Australian, & European); Model D using diagnostic criteria (DSM-III/R/TR, DSM-IV-R/TR, & DSM-5).
A series of sensitivity analyses based on CBT combinations were performed to evaluate the robustness of study results. The analysis found no significant moderator for psychotherapies effectiveness after adjusted by participant's gender, studies' risk of bias, continent, and diagnostic criteria (DIC<10). Sensitivity analysis based on treatment combinations were also performed in four different formats. According to the change of DIC score from initial model (DIC = 360.04), only combination of CBT + CT (DIC = 363.29) and CBT + CT + PE (DIC = 346.44) were significant statistically (Table 4).
Table 4. Models fits of sensitivity analysis

CPT, Cognitive processing therapy; CT, Cognitive therapy; CBT, Cognitive behaviour therapy; EMDR, Eye movement desensitisation and reprocessing; NET, Narrative exposure therapy; PCT, Present centred therapy; PDT, Psychodynamic therapy; PE, Prolonged exposure; BEP, Brief eclectic psychotherapy; TAU, Therapy as usual; NT, No treatment; DIC, Deviance information criterion; ES, Effect size; SMD, Standardized mean different; CI, Confidence interval.
Note: Different types of CBT therapies (CT, CPT, and PE) were combined as CBT in each model to evaluate its effectiveness. Unadjusted SMD and DIC value were obtained using Bayesian NMA without adjusting for specific risk factors. Adjusted SMD and DIC value were obtained after adjusting for different risk factors. We choose the adjusted model if there was DIC value difference more than 10 points between adjusted and unadjusted model. β coefficient represent the effect of moderator in the NMA result. Example: at the second model analysis, the DIC at initial model was 360.04, While after CBT and CT was combined together, the DIC change into 363.29. There was a significant different between initial and after combined since the different was more than 10 points.
Discussion
Our NMA examined the comparative effectiveness of psychotherapies on PTSD symptoms, loss of diagnosis, retention rate, anxiety, and depression at post-treatment, short and long-term follow-ups. We also performed sensitivity and moderator analyses to understand the effects of PTSD psychotherapies better.
Principal findings
The psychotherapies listed in the current meta-analysis differ in the intervention, number of sessions, duration, and format but commonly facilitate people with PTSD to ‘process’ their traumatic memories. Of the recommended therapeutic approaches, CPT, CT, CBT, brief eclectic psychotherapy (BEP), PCT, and PDT mostly focus on cognitive restructuring skills by challenging the maladaptive cognitions with cognitive restructuring techniques. After undergoing these therapeutic approaches, patients will improve their understanding about their negative patterns in thoughts and feelings in order to have more ideas that are realistic and behavioural patterns (Adams, Reference Adams2018). On the other hand, PE and NET use gradual exposure of stimuli using writing, imagery, or direct contact with the related place through a hierarchical of fearful events, one at a time (McLean & Foa, Reference McLean and Foa2011). Through repeated exposures, people with PTSD may be able to face challenging situations without feeling traumatised and anxious. Meanwhile, Eye Movement Desensitisation and Reprocessing (EMDR) works by extracting all the anxious feelings leading to a decrease in vividness and emotionality in regards to memory. EMDR reconstructs patients' cognitive thinking, along with their emotional status, which in turn helps the patient to process their memory and emotions correctly (Shapiro, Reference Shapiro2001).
Our analyses showed that CPT and EMDR were consistently in the upper quartile as the most effective therapies for improving PTSD symptoms at immediate post-treatment, short-term and long-term follow-up. However, in terms of loss of PTSD diagnosis, NET, CPT, and EMDR were the most effective therapies. In addition, CPT, CT, EMDR, and NET switched interchangeably as the most effective therapies in decreasing anxiety and depression symptoms. In consideration of the comparative effectiveness of PTSD psychotherapies on improving the primary and secondary outcomes in the current NMA, we suggest CPT, CT, EMDR, and NET as the four most recommended therapeutic approaches.
As noted above, CPT, EMDR, and CT all showed very good efficacy in the current analysis. CPT and CT aim to improve a person's ability to accommodate and decrease rumination by targeting specific thoughts and beliefs, NET aims to develop a coherent narrative of the trauma autobiographical memory. On the other hand, EMDR applies bilateral stimulation as the patients recall specific events from the trauma. Despite the seemingly different nature of these approaches, one notable commonality is that CPT, EMDR, and CT all require some form of re-exposure and reprocessing of the traumatic memory. Therefore, re-exposure and more importantly subsequent reprocessing may be crucial elements to ensuring effective PTSD treatment. Indeed, these elements are also present in most psychotherapies in the top two quartiles in the primary outcome, though CBT is one notable and perhaps surprising exception. We take this variability to suggest a slightly more nuanced view: perhaps re-exposure and reprocessing of traumatic events are necessary, though not sufficient in and of themselves, components to effective psychotherapy. As of now, it does seem that all forms of treatments are capable of reducing anxiety and depression but PDT.
Comparison to other studies
Previous NMA conducted for adults with PTSD showed slightly different results where EMDR, CT, TF-CBT, and self-help with support were the most effective therapies (Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Welton, Stockton and Pilling2020b). While our current study found CPT, CT, EMDR, and NET as the most recommended therapies. Our results were slightly different when compared to some previous meta-analyses, which found no significant differences among psychotherapy comparisons (Bisson, Roberts, Andrew, Cooper, & Lewis, Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Power et al., Reference Power, McGoldrick, Brown, Buchanan, Sharp, Swanson and Karatzias2002). Different meta-analyses also had different categorisations for grouping interventions; for example, Chen et al. (Reference Chen, Zhang, Hu and Liang2015) grouped BEP and PE into CBT and found that EMDR was slightly better than the grouped CBT category. However, when interventions were analysed separately and not grouped into CBT, CPT also showed significant effect size (SMD −1.40 95% CI −1.95 to −0.85) in Cusack et al.' meta-analysis (Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016) of psychological treatments for adults with PTSD. Our sensitivity analysis of grouping different interventions into CBT, has different results than Gerger et al.'s NMA (Gerger et al., Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Jüni and Barth2014). Different formats of CBT therapies (CT, CPT, and PE) were put into the CBT group, our study found that the difference of the DIC was higher than 10 in the combination model from the original one, there needs to be further research for how best to approach grouping different interventions in categories of comparison in meta-analysis and NMA.
In the context of APA and VA/DOD guidelines
Recently, there have been growing concerns regarding Courtois et al. (Reference Courtois, Brown, Cook, Fairbank, Friedman, Gone and Kurtzman2017) and Card (Reference Card2017) guidelines on PTSD treatment. Based on RCTs data, APA's PTSD guideline strongly recommends CBT, CPT, CT, and PE as psychotherapies for treating people with PTSD while BEP, EMDR, and NET were suggested psychotherapies (Courtois et al., Reference Courtois, Brown, Cook, Fairbank, Friedman, Gone and Kurtzman2017). The Veteran Affairs/DoD clinical practice guidelines recommended PE, CPT, EMDR, BEP, and NET as trauma-focused psychotherapies for full PTSD treatment. Putting our results in the context of these guidelines, our results help to refine the list to just CPT, CT, EMDR, and NET. This appears rather surprising at first, as one would expect that the inclusion of more studies should yield a more diverse line-up of psychotherapies. However, it is important to note that all therapeutic approaches in our NMA showed efficacy over the control or waitlist groups. Therefore, by focusing on the top quartiles, a shorter recommended list in the present study merely means that CPT, CT, EMDR, and NET seem to be most effective in a list of psychotherapies that have all proven to be effective. Though, of course, meta-analyses are by nature biased towards therapies that enjoy more clinical data and studies, which are often the case in RCTs. Thus, we also recommend caution when interpreting the present results because the numbers here simply cannot replace the therapists' insights of a client/patient gained through mutual understanding and long-term rapport.
Our point above is similar to the concern raised by Norcross and Wampold (Reference Norcross and Wampold2019), who pointed out that the importance of therapist-client relationship seems to be missing in the current versions of the guidelines. We respectfully agree with this point, as our findings in the current NMA also suggest and show that not all therapies are equal. Therefore, perhaps a middle ground for this issue is that the guidelines and the concerns raised are not mutually exclusive; rather, by combining therapist-client relationship with the most efficacious psychotherapies such as CPT, EMDR, and NET, treatment efficacy can likely be maximised. As such, we anticipate that as more studies and data on the catalytic and therapeutic effects of therapist-client relationships become available, these data should be able to help better strengthen and expand the scope of American Psychological Association (2017) and VA/DOD guidelines.
Strengths and limitations of the study
This review provides an overview of the current state of knowledge concerning the PTSD psychotherapies recommended in clinical guidelines. Firstly, this study was conducted with rigour and followed the Cochrane NMA guidelines and GRADE analysis guidelines. Secondly, it examined 141 studies from across the world in a wide age range. Thirdly, long-term follow-up measurements were analysed with available data. Finally, moderator and sensitivity analyses were also conducted to check for the robustness of the results. Although the study's results can be helpful for making treatment decisions, there are limitations that should be noted when interpreting the study's results. First, limited studies provide complete demographic information including socioeconomic data that might be useful in determining the moderating effect of demographic variables in the final analysis. Second, small number of studies in some of the included psychotherapies might have led to over-estimation or under-estimation of the treatment effects leading to misleading results in the final analysis. Finally, in NMAs it is important to detect inconsistency due to the inherent assumptions for indirect comparison. Although in the local inconsistency coefficient of difference analysis showed the value of p > 0.05, yet the node-splitting model found some intervention comparisons were not in agreement. Overall, our analysis showed no significant global and local inconsistency meaning that our results are statistically reliable.
Conclusion
In summary, CPT, EMDR, CT, NET, PE, CBT, and PCT showed as the most effective therapies on improving PTSD symptoms with large to moderate effect at post-treatment measurement. The proportion of loss of diagnosis showed that all specific psychological treatments tended to decrease the number of people who meet PTSD diagnosis at post-treatment. Thus, future studies should consider exploring the combination and long-term effectiveness of PTSD psychotherapies. We also recommend that therapists' insights of a client/patient gained through mutual understanding and long-term rapport should be taken into consideration when delivering PTSD psychotherapies.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291722003737.
Acknowledgements
The findings and conclusions in this document are those of the authors, who are responsible for its contents
Author contributions
Ninik Yunitri: conceptualisation, acquisition, format analysis, interpretation of the data, & writing original draft, visualisation Hsin Chu: visualisation Xiao Linda Kang: acquisition, validation, investigating, analysis, writing-review and editing, visualisation Bayu Satria Wiratama: analysis, interpretation of the data writing-review & editing Doresses Liu: writing-review & editing, Christina Yeni Kustanti: investigating & visualisation Kai-Jo Chiang: investigating & visualisation Ruey Chen: investigation & visualisation Philip Tseng: investigation, writing-review & editing Kuei-Ru Chou: supervision, conceptualisation, final approval, agreement.
Financial support
None to be declared.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical standards
As this study is a NMA of previous published data.








