Introduction
Childhood anxiety disorders (CAD) are a significant mental health concern in young children. For example, a recent Australian national survey of mental health of children and adolescents finding 5.7% of 4- to 11-year-olds met criteria for an anxiety disorder and anxiety disorders were the second-most common mental disorder identified in this survey (Lawrence et al., Reference Lawrence, Hafekost, Johnson, Saw, Buckingham, Sawyer and Zubrick2016). Far from remitting during childhood, early CAD is a risk factor for the development of later anxiety disorders and depression as well as a range of other poorer psychosocial outcomes (Bittner et al., Reference Bittner, Egger, Erkanli, Jane Costello, Foley and Angold2007; Kendall et al., Reference Kendall, Safford, Flannery-Schroeder and Webb2004; Mazzone et al., Reference Mazzone, Ducci, Scoto, Passaniti, D’Arrigo and Vitiello2007; Moran, Reference Moran2016). This supports the importance of research that can build an understanding and further elucidate the early predictors and risk factors for CAD.
CAD includes Generalized Anxiety Disorder, Social Phobia, Specific Phobias, Panic Disorders and Separation Anxiety Disorder. In our previous study, we examined a developmental programming hypothesis whereby early life predictors of CAD including maternal depression, history of childhood trauma and antenatal cortisol interacted with parenting stress in the postpartum. We identified that only when there was increasing maternal cortisol in pregnancy together with higher parenting stress reported at 6 months was there an increased risk of CAD in early childhood (Galbally et al., Reference Galbally, Watson, van Rossum, Chen, de Kloet and Lewis2020). Furthermore, both maternal depression and a history of maternal experiences of trauma in childhood were independently associated with CAD. However, in that study we did not examine the quality of the parent–infant relationship and, in particular, infant attachment classification and whether this may moderate these early predictors of CAD.
While there have been many areas of focus in understanding developmental pathways towards the development of CAD, one potentially important area to understand is the role of early infant-parent attachment as potentially a key moderator of risk. According to attachment theory (Bowlby, Reference Bowlby1982), the parent–child relationship plays a central role in the development of children’s emotional regulation capacities, which, in turn, is at the core of children’s emotional well-being and developmental adaptation (for a summary, see DeKlyen & Greenberg, Reference DeKlyen, Greenberg, Cassidy and Shaver2016). Young children rely on their caregivers in regulating negative emotions such as anxiety, sadness, or anger. Securely attached children are thought to develop effective emotion regulation strategies in repeated interactions with a responsive caregiver who is available for support when needed. According to attachment theory, insecurely attached children are hampered in their development of effective dyadic strategies to cope with negative emotions due to inconsistent or less sensitive responsiveness from the parent when the child is distressed. Disorganized attachment is characterized by a (sometimes momentary) breakdown in organized attachment behavioral strategies when the child is distressed and the parent is present, undermining the development of effective emotional regulation. Given that problems with emotional regulation play a key role in many forms of psychopathology (Izard et al., Reference Izard, Youngstrom, Fine, Mostow, Trentacosta, Cicchetti and Cohen2006), in particular internalizing problems such as anxiety, withdrawn behavior and depressive symptoms, there has been a continued research interest in the role that early parent–child attachment may have in the development of internalizing disorders.
Two meta-analyses of attachment classification and security (Groh et al., Reference Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg and Fearon2012; Madigan et al., Reference Madigan, Atkinson, Laurin and Benoit2013) lend some empirical support to the theoretical assumption of a relationship between insecure parent–infant attachment and internalizing psychopathology. The first meta-analysis found a small effect size for the association for attachment insecurity and internalizing symptoms in children measured mostly using the Child Behavior Checklist (CBCL) (d = 0.15, 95% CI [0.06, 0.25]) (Groh et al., Reference Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg and Fearon2012). However, surprisingly, they found no association with disorganized attachment and internalizing symptoms (Groh et al., Reference Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg and Fearon2012). The second meta-analysis of child internalizing symptoms found mid-range small effect sizes for insecure attachment and internalizing symptoms (observed d = 0.37, 95% CI [0.27, 0.46]) and smaller effects for disorganized attachment and internalizing symptoms (d = .20, 95% CI [0.09, 0.31]) (Madigan et al., Reference Madigan, Atkinson, Laurin and Benoit2013).
There are a more limited number of studies that have examined attachment and child anxiety. In one of these few studies, the researchers examined a sample of 155 assessed both in early childhood and then adolescence and found insecure attachment was associated with increased risk of adolescent anxiety symptoms, but not with an increase in earlier childhood anxiety symptoms (Bosquet & Egeland, Reference Bosquet and Egeland2006). The authors postulated that increased vulnerability from insecure attachment in early life to adolescent anxiety might be explained by negative appraisals of peer relationships. A secure attachment may provide the basis for approaching later social and developmental challenges through enhancing the capacity for emotional regulation, social efficacy, and competence and increasing the likelihood of positive peer and teacher interactions (Kerns & Brumariu, Reference Kerns and Brumariu2014). Further, it has been suggested that secure attachment can play a protective role between the effects of maternal prenatal stress and child outcomes beyond the first year of life (Bergman et al., Reference Bergman, Sarkar, Glover and O’Connor2008). Therefore, it remains a plausible hypothesis that the quality of the attachment relationship might, in turn, relate to vulnerability or provide protection for not only anxiety symptoms but also potentially the development of anxiety disorders due to early life exposure to stress. However, few studies have included categorical diagnostic as well as dimensional measures of anxiety in children in relation to attachment.
While previous research has examined maternal depression, salivary basal cortisol secretion and reactivity, infant–parent attachment, and child socio-emotional development including internalizing disorders, studies examining maternal depression, salivary cortisol, and attachment specifically as predictors of childhood anxiety disorders are limited (Luijk et al., Reference Luijk, Saridjan, Tharner, van IJzendoorn, Bakermans-Kranenburg, Jaddoe and Tiemeier2010; Tharner et al., Reference Tharner, Luijk, van IJzendoorn, Bakermans-Kranenburg, Jaddoe, Hofman and Tiemeier2012). However, one study of infant salivary cortisol found that disorganized infants at 14 months of age displayed a flattened diurnal pattern of salivary cortisol and in those with resistant attachment, salivary cortisol reactivity was greater in children with a mother with a lifetime history of depressive disorder (Luijk et al., Reference Luijk, Saridjan, Tharner, van IJzendoorn, Bakermans-Kranenburg, Jaddoe and Tiemeier2010). It is unknown whether, in turn, infant salivary cortisol output or reactivity may mediate risk or resilience for childhood anxiety disorders. Furthermore, it is also unknown how infant salivary cortisol regulation might interact with attachment in the presence of early predictors of CAD.
In this paper, we build and extend on these previous findings by investigating the role of infant–parent attachment classification at 12 months of age, assessed using the Strange Situation Procedure (SSP), in our previously identified relationship between antenatal and postnatal predictors of CAD. Furthermore, we also aim to examine the role of child cortisol reactivity at 12 months of age, assessed during the SSP, in the associations between the antenatal and postnatal predictors of CAD. Figure 1 depicts conceptually our study aims. First, we hypothesize that maternal antenatal risk factors related to stress are associated with more CAD symptoms at age 4 and that this association is (at least in part) mediated by children’s physiological stress reactivity (as measured by their salivary cortisol) (Hypothesis 1). We also test attachment quality as a moderator of the pathways to CAD from antenatal and postnatal predictors of CAD. Second, we hypothesize that secure attachment will buffer the negative effects of early life risk factors related to stress (i.e., maternal childhood trauma, depression, prenatal stress as indicated by hair cortisol, and early postpartum parenting stress) on children’s cortisol reactivity (Hypothesis 2a) as well as the negative effect of children’s cortisol reactivity at 12 months of age on CAD at 4 years of age (Hypothesis 2b). Third, regarding disorganized attachment, we hypothesize that disorganization will intensify the negative effects of early life risk factors related to stress (i.e., maternal childhood trauma, depression, prenatal stress as indicated by maternal hair cortisol, and early postpartum parenting stress) on children’s cortisol reactivity (Hypothesis 3a) as well as the negative effect of 12-month-old children’s cortisol reactivity on CAD at 4 years of age (Hypothesis 3b).
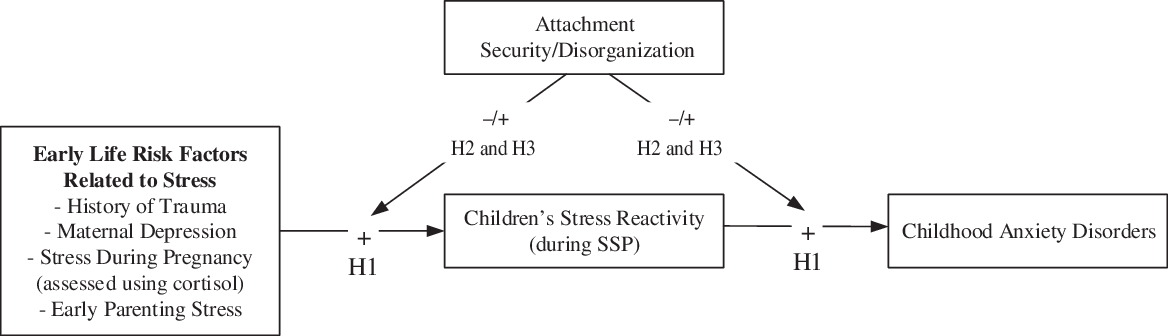
Figure 1. Conceptual model of study hypotheses. H1, Hypothesis 1: children’s cortisol reactivity at 12 months of age as a mediator connecting early life risk factors related to stress (i.e. maternal childhood trauma, depression, prenatal stress as indicated by cortisol, and early postpartum parenting stress) with CAD (Childhood Anxiety Disorders) at 4 years of age; H2, Hypothesis 2: secure attachment will buffer both the deleterious effects of early life risk factors related to stress on children’s cortisol reactivity and, in turn, the deleterious effect of children’s cortisol reactivity on CAD at 4 years of age; H3, Hypothesis 3: disorganised attachment will intensify both the deleterious effects of early life risk factors related to stress on children’s cortisol reactivity and, in turn, the deleterious effect of children’s cortisol reactivity on CAD at 4 years of age. +/- indicate the direction of the hypothesized effects.
Method
This study draws on participants from the Mercy Pregnancy Emotional Wellbeing Study, a prospective, selected cohort pregnancy study, for which women were recruited before 20 weeks of pregnancy and followed up during third trimester, at delivery, and at 6 months, 12 months, and 4 years postpartum. This study utilizes data from a subset of 190 women and children who have completed the SSP at 12 months postpartum and the child psychiatric assessment at 4 years of age. Further details of the study are described in the published study protocol (Galbally et al., Reference Galbally, van IJzendoorn, Permezel, Saffery, Lappas, Ryan and Lewis2017). The Mercy Health Human Research Ethics Committee approved this study, and all participants provided informed, written consent.
Measures
Maternal depression
At recruitment, the Structured Clinical Interview for DSM-IV (SCID-IV) was administered (First et al., Reference First, Spitzer, Gibbon and Williams1997). The Edinburgh Postnatal Depression Scale (EPDS) was also administered in pregnancy, postpartum, and 4 years assessment (Cox et al., Reference Cox, Holden and Sagovsky1987; Spielberger & Gorsuch, Reference Spielberger and Gorsuch1983). The EPDS has 10 items and a response scale of 0 to 3. Summed EPDS can range between 0 and 30 with higher scores indicating more depressive symptoms. Internal consistency (Cronbach’s alpha) of EPDS items across the Waves is good, ranging between .85 and .92.
Maternal childhood trauma
Maternal childhood trauma history was measured using the brief version of the Childhood Trauma Questionnaire (CTQ), which is a 28-item self-report measure (Bernstein & Fink, Reference Bernstein and Fink1998; Bernstein et al., Reference Bernstein, Stein, Newcomb, Walker, Pogge, Ahluvalia and Zule2003). As previously reported, in our sample, the total score CTQ and each of the five subscales (emotional abuse and neglect, physical abuse and neglect, and sexual abuse) demonstrated adequate to strong internal consistency, with Cronbach’s alpha scores ranging .75 to .92 (Galbally et al. , Reference Galbally, Watson, Boyce and Lewis2019). In this study, we used a dichotomized total CTQ score because of the positively skewed reports of CTQ, given higher scores indicate more severe history of trauma and many women reported no history. Responses were dichotomized using severity cut-off scores, provided by the CTQ manual to create binary groups (None-to-Minimal vs. Moderate-to-Severe) (Bernstein & Fink, Reference Bernstein and Fink1998).
Maternal antenatal cortisol
As previously described for this cohort, a length of maternal hair of approximately 20 g (150 strands) was collected on day 1 post-delivery, which allows to retrospectively provide average cortisol across pregnancy, in addition infant hair was also collected at 12 months postpartum and analyzed for cortisol (Galbally, van Rossum et al., Reference Galbally, van Rossum, Watson, de Kloet and Lewis2019; Manenschijn et al., Reference Manenschijn, Koper, Lamberts and van Rossum2011; Smy et al., Reference Smy, Shaw, Amstutz, Smith, Berger, Carleton and Koren2016). A questionnaire related to factors potentially influencing HCC was administered and as previously reported both bleaching and treating hair during pregnancy and for the infant at 12 months was not associated with differences in hair cortisol concentrations (HCC) (Galbally, van Rossum, et al., Reference Galbally, van Rossum, Watson, de Kloet and Lewis2019). At least 5 mg of the most proximal 3 cm of hair was weighed for each hair sample and samples were collected, processed, and analyzed as previously described (Galbally, van Rossum, et al., Reference Galbally, van Rossum, Watson, de Kloet and Lewis2019; Noppe et al., Reference Noppe, Rijke, Dorst, Akker and van Rossum2015). Hair cortisol was quantified by liquid chromatography – tandem mass spectrometry using a Xevo TQ-S system (Waters, Milford MA) (Galbally, van Rossum, et al., Reference Galbally, van Rossum, Watson, de Kloet and Lewis2019; Noppe et al., Reference Noppe, Rijke, Dorst, Akker and van Rossum2015), where the lower limit of the measuring interval (LLMI) was set at 2.5 pg/ml. Hair cortisol results below LLMI were substituted by a fixed value (0.75*LLMI). Higher concentrations of cortisol indicate higher levels of stress.
Parenting stress
At 6 months postpartum, parenting stress was assessed using the Parenting Stress Index, Short-form (PSI-4-SF) (Abidin, Reference Abidin1990). PSI-4-SF is a 36-item index, which uses a 5-point Likert scale and yields a total score of overall parenting stress and three subscales (Difficult Child, Parent Distress, and Parent-child Dysfunctional Interactions). Raw scale and total scores can be converted to percentile scores for easier comparison across research. Internal consistency of the total score on the PSI and three subscales have been reported as adequate to strong, with Cronbach’s alpha ranging between .75 and .92 (Barroso et al., Reference Barroso, Hungerford, Garcia, Graziano and Bagner2016). Due to strong associations between the Parent Distress subscale and depressive symptoms measured with the EPDS, we used the average of only the Difficult Child and Parent-Child Dysfunctional Interactions subscales percentiles.
Infant cortisol reactivity
As previously reported, at 12 months of age salivary samples from the infant were collected during the Strange Situation Procedure, a laboratory procedure to assess attachment security designed to be mildly stressful for the child by introducing stressors such as an unfamiliar environment, a friendly stranger and two brief separations from the parent (Galbally, van Rossum, et al., Reference Galbally, van Rossum, Watson, de Kloet and Lewis2019). Samples were collected at 3 times: baseline, 10 min after completing the task (+20 min from baseline), and 30 min after completing the task (+40 min from baseline). Salivary samples were collected using a salivette, centrifuged, and stored at −80 °C. Salivary cortisol was measured using a commercially available ELISA assay (Salimetrics, USA), in duplicate according to the manufacturer’s instructions. Salivary cortisol using these assays has been correlated well with matched serum cortisol concentrations (r = .91). Assay sensitivity was 0.003 μg/dl, intraassay variability was 4.4%, and interassay variability was 4.9%. All salivary cortisol levels are expressed in SI units, nmol/L. Average salivary cortisol for each collection is presented in Supplementary Figure 1. A repeated-measures ANOVA found salivary cortisol in the infant was significantly higher in both the +20 min and +40 min collection compared to baseline (p’s < .05), demonstrating cortisol reactivity to the SSP.
Infant cortisol reactivity was expressed using two cortisol response indices, Area Under the Curve relative to ground, or zero (AUCg), and AUC relative to increase (AUCi), using equations outlined in Pruessner et al. (Reference Pruessner, Kirschbaum, Meinlschmid and Hellhammer2003). AUCg and AUCi were introduced to capture a single cortisol response measurement using repeated measurement data and to attempt to standardize the method for reporting change in cortisol so that findings could be easily understood and compared across research (Khoury et al., Reference Khoury, Gonzalez, Levitan, Pruessner, Chopra, Basile and Atkinson2015; Pruessner et al., Reference Pruessner, Kirschbaum, Meinlschmid and Hellhammer2003). In this study, AUCg measures infant cortisol response, that is, an infants’ total cortisol levels during the period prior to commencing and at 30 min after completing the task, whereas AUCi measures cortisol reactivity, that is, infants’ change in cortisol relative to their baseline cortisol level.
Infant-parent attachment
Infant-Parent Attachment was measured using the Strange Situation Procedure (SSP) at 12 months of age (Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978). The SSP is an observational coded measure of attachment utilizing a standardized protocol of eight 3-min episodes of separation and reunion with the mother. The procedure should act as a mild stressor for the child and is designed to activate attachment behaviors in relation to the caregiver. The separation episodes were curtailed when the infant is overly distressed about the parent’s absence; this was defined as showing physiological signs of distress or prolonged distress and no infant was left distressed for more than 1 min where this was not resolving as recommended (Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978). There are other protocols that recommend curtaining separation after a maximum of 20 s of high infant distress. The SSP is coded for three organized patterns of attachment: secure (B), insecure-avoidant (A), and insecure-ambivalent (C) (Ainsworth et al., Reference Ainsworth, Blehar, Waters and Wall1978). The disorganized/disoriented (D) infant attachment is coded using the Main and Solomon coding system (Main & Solomon, Reference Main and Solomon1990), yielding a 1 (no signs of disorganization) to 9 (strong signs of disorganization) score. Richters continuous security scale (Richters et al., Reference Richters, Waters and Vaughn1988) was also calculated using continuous attachment interactive scales but without infant crying, and respective discriminant functions reported in van IJzendoorn and Kroonenberg (van IJzendoorn & Kroonenberg, 1990). Consistent with van IJzendoorn and Kroonenberg, the derived Richters security score without crying was able to predict Secure vs. non-Secure dyads with 90.5% accuracy in our sample. The SSPs were coded by two certified reliable coders (co-authors AT and ML). Inter-rater reliability (kappa statistic) between these two coders was .64 for the 4-way classification, .75 for the disorganized vs. nondisorganized binary classification, and the ICC was .49 for the Richters security and .61 for the continuous disorganization single measures scores.
Childhood anxiety disorders
CAD were assessed at 4 years of age using the Preschool Age Psychiatric Assessment (Egger et al., Reference Egger, Erkanli, Keeler, Potts, Walter and Angold2006). This is a structured diagnostic interview for 3–8 years of age children was administered to the mothers of the children by trained provisional psychologists. It takes approximately 1 hr to administer and draws on DSM-V based symptoms to use computer algorithms to generate DSM-V diagnoses. Our research team has undertaken training with the authorized trainers of this instrument from Duke University, Developmental Epidemiology (Egger et al., Reference Egger, Erkanli, Keeler, Potts, Walter and Angold2006). Both the test-retest reliability and the inter-rater reliability have been established (Egger et al., Reference Egger, Erkanli, Keeler, Potts, Walter and Angold2006; Luby et al., Reference Luby, Gaffrey, Tillman, April and Belden2014). The CAD assessed by the PAPA are Generalized Anxiety Disorder, Social Phobia, Specific Phobias, Panic Disorders, and Separation Anxiety Disorder. The Child Behavior Checklist for ages 1–5 was also administered at 4 years of age (Achenbach & Rescorla, Reference Achenbach and Rescorla2001). This is a parent report and the anxiety problem scale (t score, higher scores reflecting more anxiety symptoms) was reported in this study. In our data, the anxiety problems t score was significantly positively correlated with CAD from the PAPA (r [190] = .31, p < .001).
Statistical analyses
We first present frequencies of the sample (N = 190) for key demographic and other variables included in this study. We then explore differences between CAD groups (no CAD vs. any CAD) on key maternal and child characteristics and measures, as well as attachment classifications and scores. For categorical variables, chi-square tests of association are used for proportional differences between the attachment groups with Fisher’s exact tests reported when expected cell counts are 5 or fewer, and mean differences on continuous variables are tested using one-way ANOVAs with the robust Welch’s F test reported when variances between groups are significantly different.
To test the study’s hypotheses, which are presented graphically in Figure 1, we present the results of multiple group path modeling conducted using MPlus version 8 (Muthén & Muthen, Reference Muthén and Muthen2017). Prior to the multiple group modeling, we present zero-order bivariate correlations and descriptive statistics for variables included in the modeling. To assess whether children’s cortisol reactivity at 12 months postpartum (i.e., AUCi) mediates the association between early risk factors related to stress and CAD at age four (Hypothesis 1), we estimate individual indirect path coefficients between maternal childhood trauma, depression, prenatal stress as indicated by hair cortisol, and early postpartum parenting stress on CAD through children’s cortisol reactivity measured during the SSP. A significant indirect coefficient would provide support for the hypothesized mediation effects. To assess whether attachment security (Hypotheses 2a and 2b) and, separately, attachment organization (Hypotheses 3a and 3b), moderate the indirect associations between early risk factors related to stress and CAD at age four through children’s cortisol reactivity, we conducted multiple group models on the indirect pathways specified to assess hypothesis 1. For the attachment disorganized multiple groups model, the groups were Non Disorganized and Disorganized; for the attachment security multiple group model, the groups were Securely Attached and Insecurely Attached. For both multiple groups models, we first fit a model constraining all estimated parameters to equality (i.e., no moderating effect of attachment group), which provides a baseline comparison for the final model. Using a stepwise approach, we then fit a series of models allowing one regression path at a time to freely estimate for each group and tested the difference between each group’s regression estimate using a Wald test. Paths that differed significantly according to the Wald test, which indicates a moderating effect of attachment group (support for Hypotheses 2 and 3), were then allowed to freely estimate for the final multiple group model. Fit statistics for the final models were then compared to the baseline model, with support for a better fitting model indicated by lower AIC and BIC fit indices. For the final multiple groups models only, we present the standardized regression coefficients for the continuous AUCi outcome and odds ratios for the binary CAD outcome. Given both linear and nonlinear outcomes are considered concurrently in the multiple group path modelling, attachment groups were considered latent classes using mixture modeling with Monte Carlo numerical integration, which allowed for inferential comparisons of estimated model parameters between the groups. Model parameters were estimated using maximum likelihood with robust standard errors. For each final multiple-group model, the Benjamini–Hochberg procedure to control for the false discovery rate (FDR) at .10 (to account for the exploratory nature of the current study) is applied to significance tests for all estimated parameters in the final multiple groups model (i.e., all freely estimated regression coefficients, covariances, intercepts, residual variances, and thresholds) (Benjamini & Hochberg, Reference Benjamini and Hochberg1995).
We also conduct a series of alternative models to the multiple group models tested, in order to (i) conduct the multiple group models using the continuous CBCL Anxiety Problems raw score; (ii) validate findings from the multiple group models by using continuous attachment disorganization and security scores; and (iii) test the alternative propositions that attachment mediates associations between maternal early risk factors of CAD and the incidence of CAD at 4 years of age. To validate the findings from the multiple group models, attachment disorganization and security were added separately into the path model described above and depicted in Figure 1 at the same level as the children’s cortisol reactivity. Multiplicative interaction terms between maternal childhood trauma, depression, prenatal stress as indicated by hair cortisol, and early postpartum parenting stress with attachment disorganization, and, separately, with attachment security, were added as predictors of CAD at 4 years old.
Prior to analyses, we excluded one univariate outlier (z > |3|) from average maternal antenatal HCC and one from infant AUCi, treating these values as missing for the participants. Missing values on all variables (all < 5% missing) were then estimated using Expectation-Maximization imputation models. Following removal of one outlying value, average maternal antenatal HCC remained significantly skewed, with a skew statistic exceeding 3 times its standard error. Also significantly skewed were infant HCC and AUCg both at 12 months postpartum. As such, we applied a natural logarithmic transformation to these skewed variables, which improved normality of each variable’s distribution. There were 42 (22%) recordings of the Strange Situation Procedure that were identified by coders as having technical (i.e., obscured camera angle) or procedural issues (reduced length of separation due to prolonged distress); however, none of these recordings were ruled by the coders as invalid for classification. Despite all cases receiving a valid attachment classification by the coders, we follow-up the presentations of the hypothesized multiple group models by assessing the influence of these 42 cases on the results by adding a binary variable (0 = no issue, 1 = issue) as a predictor of both infant cortisol reactivity during the SSP and childhood anxiety disorders.
Other than the mixture multiple group modeling, all other analyses were conducted using SPSS version 24. It should be stressed that due to limited statistical power, all multivariate analyses should be considered exploratory, requiring replication and/or analytic approaches with improved precision (e.g., using these results to inform model priors for a Bayesian approach). In the multiple group multivariate path models, standardized linear regression coefficients of between .10 and .30 estimated to equality between groups (N = 190) have statistical power ranging between 39.4% and 99.6%. The exponentiated regression coefficients (odds ratio, OR) of between 1.3 and 2.0 estimated to equality between groups (N =190) have statistical power ranging between 49.9% and 99.5%. Although the lower ends of these power ranges reflect an effect size with limited clinical significance, the upper ends are comparable to the relative, mid-range small effect sizes reported in recent meta-analyses (Madigan et al., Reference Madigan, Atkinson, Laurin and Benoit2013).
Results
Table 1 displays maternal sociodemographic and other key characteristics for the sample. Most women were nulliparous (93.2%), married, de facto or in an otherwise committed relationship (93.2%), and of Oceanic/European origin (90%), and two-thirds of the sample were university educated (68.4%). The prevalence of a depression diagnosis in early pregnancy amongst the women was 18.4%, and slightly lower for antidepressant use (17.4%). More than half of offspring were male (56.3%), and the prevalence of CAD at 4 years of age among offspring was 41.1%. The breakdown and reasons for the higher rate of anxiety disorders in this cohort have been previously described and include factors such as this being a selected cohort for maternal depression and higher rates of maternal past history of depression and anxiety (Galbally et al., Reference Galbally, Watson, van Rossum, Chen, de Kloet and Lewis2020). Supplementary Table 1 displays measures of cortisol for mother and infant across the ABCD attachment classification groups. Both maternal antenatal hair cortisol concentrations and infant hair cortisol concentrations at 12 months of age did not differ significantly between ABCD groups. Although the Insecure Ambivalent/Resistant group had higher cortisol reactivity (AUCi) relative to the other 3 attachment classification groups (see Supplementary Table 1), the omnibus groups comparison not significant.
Table 1. Sample characteristics (N = 190)

Note. SCID-IV = structured clinical interview for the DSM-IV.
Attachment and differences in mother and child characteristics across CAD groups
In the sample, 122 women and infants (64.2%) were classified as secure attachment, 24 (12.6%) insecurely avoidant, 13 (6.8%) insecurely ambivalent, and 31 (16.3%) disorganized. The continuous disorganization score was point inflated with 40% (n = 76) of the sample scoring 1 on the 1 to 9 scale (M = 2.99, SD = 1.90, observed range: 1–7.5). When treating the variable as semi-continuous and excluding participants with a score of 1, the continuous part of the distribution was normally distributed (M = 4.31, SD = 1.27). In terms of disorganization across the forced 3-way classification (i.e., ABC) in the whole sample, 10.3% (14/136) of securely attached infants demonstrated disorganization during the SSP, with 23.5% (4/17) disorganized in dyads classified as insecure ambivalent and 35.1% (13/37) in dyads classified as insecure avoidant; these proportions differed significantly (Fisher’s exact χ 2 = 12.82, p = .001). Pairwise comparisons demonstrated that there were significantly more insecure avoidant dyads with disorganized attachment than the securely attached dyads only (p < .05). Richters security score was normally distributed (observed range: −5.94, 6.46) with the sample average (M = 0.83, SD = 2.99) within the Secure attachment region (i.e., scores ≥ 0).
Results of unadjusted group comparisons between those with and without CAD on several key maternal and child characteristics and measures, as well as several classifications and measurements of attachment are presented in Table 2. There were no significant proportional differences between CAD groups on the ABCD classification of attachment, nor were there any differences between CAD groups for secure compared to not secure attachment and disorganized vs. not disorganized. As well, CAD groups did not differ significantly on the continuous Richters security scale or the disorganization scores.
Table 2. Unadjusted differences between key child and maternal variables and attachment classification by childhood anxiety disorder group (N = 190)

Note. AUCi = area under the curve relative to increase; CAD = childhood anxiety disorder; SCID-IV = structured clinical interview for the DSM-IV; HCC = hair cortisol concentrations.
* Log-transformed.
† Welch’s F test result reported due to heterogeneity of variances.
Missing data handled using case-wise deletion.
As a means of comparison with the CAD diagnosed using the PAPA, we used the Anxiety Problems scale from the CBCL to compare children in the borderline and clinical range (i.e., T ≥ 60) to children in the nonclinical range (T < 60) across attachment classification groups. Proportions of children with borderline or clinical range anxiety problems, compared to nonclinical range, were similar to CAD groups across ABCD classifications with no significant proportional differences (nonclinical proportions presented first; A: 8.0% c.f. 13.3%, B: 60.0% c.f. 64.6%, C: 12.0% c.f. 6.3%, D: 20.0% c.f. 15.8%; Fisher’s exact p = .586). Also comparable to proportions of CAD across secure and disorganized binary classifications, there were no significant proportional differences between children in the borderline and clinical range compared to the nonclinical range for secure attachment (70.9% c.f. 70.2%, p = .909) and disorganized attachment (15.8% c.f. 20.0%, p = .600).
Attachment as a moderator of early risks for CAD and children’s cortisol reactivity
In the full sample, descriptive statistics and zero-order bivariate Spearman’s rho correlations for all variables used to test hypotheses and considered for modeling are presented in Supplementary Table 2. Table 3 and Supplementary Table 3 display these descriptive statistics and zero-order bivariate Spearman’s rho correlations for the disorganized attachment multiple group mixture model and the attachment security multiple group mixture model, respectively. In Table 3, bivariate correlations are reported for the disorganized/insecure group above the diagonal divide within the table and below the divide for those within the not disorganized/secure group.
Table 3. Zero-order bivariate correlations between sociodemographic characteristics and mental health with childhood anxiety disorders diagnosed at 4 years of age and univariate descriptive statistics by disorganized attachment above the diagonal (n = 31) and not disorganized attachment below the diagonal (n = 159)

Note. AUCg = area under the curve relative to ground, or zero; AUCi = area under the curve relative to increase; HCC = hair cortisol concentrations; M = mean; SD = standard deviation.
* p < .05
† Log-transformed variable.
** p < .01.
*** p < .001
Correlations between binary and continuous variables represent point-biserial coefficients, and between binary and binary variables represent Phi coefficients.
In both multiple group models, maternal moderate-to-severe childhood trauma, depression, antenatal HCC, and early postpartum parenting stress were not significant predictors of AUCi, and there were also no significant differences in these direct pathways between attachment disorganization and attachment security groups. Further, there was no significant direct effect between AUCi and CAD, which also did not differ significantly between attachment disorganization and security groups. As such, there was no support for the mediational hypothesis between antenatal and postnatal predictors of CAD via children’s cortisol reactivity (Hypothesis 1), and no support for either attachment security or attachment disorganization as moderators of these mediational pathways (Hypotheses 2 and 3). However, in the disorganized attachment multiple groups model only, pairwise parameter testing identified significant differences for direct associations between maternal depression and CAD and between maternal average antenatal HCC and CAD (Wald p’s < .05).
Disorganized compared to nondisorganized attachment
The final attachment disorganization multiple group model (AIC = 2644.06, BIC = 2704.93), which is shown in Figure 2, was a better fit compared to the fully constrained, baseline model (AIC = 2656.19, BIC = 2710.66). Further, the omnibus Wald test for relaxing the equality constraints for the direct paths between maternal depression and CAD and maternal average antenatal HCC and CAD was also significant (χ 2 [df = 2] = 15.13, p = .005). Together, these fit statistics suggest that the specification of individual group estimates for the two direct associations was a better fit to the data than constraining the associations to equality between groups, and the results indicate that disorganized attachment moderates the associations between maternal depression and CAD and maternal average antenatal HCC and CAD. It should be noted that all estimated parameters that were significant using p < .05 were also significant after adjusting for the FDR using the Benjamini–Hochberg q < .10, suggesting that the substantive findings for the multiple group model cannot be dismissed after accounting for multiple significance tests.

Figure 2. Results of the final mixture path model with multiple-group comparison of estimates. Where estimated path parameter estimates differ significantly using a Wald test (p <.05), the Not Disorganized Attachment group is presented first, and Disorganized Attachment group estimate is presented second in parenthesis. Although not included in the figure, infant sex was included as a covariate of AUCi, and gestational age at birth was included as a covariate of CAD at 4 year of age. The model was estimated using Maximum Likelihood with Robust standard errors. Note. Grayed-out paths and estimates are not significant. Pathway estimates predicting AUCi are standardised regression coefficients; pathway estimates predicting Childhood Anxiety Disorders at 4 years of age are Odds Ratios (OR). AUCi, Area Under the Curve relative to increase, HCC, Hair Cortisol Concentrations, M, mean, SD, standard deviation. *p < .05, **p < .01.
In Figure 2, the estimate for the nondisorganized group is presented first, followed by the estimate for the disorganized group in parenthesis. Higher average maternal antenatal HCC (OR = .30, p = .008) and depression in early pregnancy (OR = .08, p = .039) were each independently associated with significantly lower odds of CAD for the children in the disorganized group, which was the opposite direction of what was expected. For children in the nondisorganized group, the opposite associations were found such that higher average maternal antenatal HCC (OR = 1.45, p = .041) and maternal depression in early pregnancy (OR = 3.23, p = .010) were each independently associated with significantly higher odds of CAD at 4 years old. Although not different between the groups, moderate-to-severe maternal childhood trauma was also independently associated with significantly higher odds of CAD for all children in the sample (OR = 2.45, p = .013).
Taken together, the results from the exploratory modeling suggest disorganized attachment (c.f. nondisorganized) between mother and her child observed at 12 months during the SSP can differentiate between the strength and direction of direct associations such as between early risk factors of CAD and CAD at 4 years of age, whereas secure attachment (c.f. insecure attachment) does not differentiate between the strength and directions of the direct associations. When adjusting for the effect in the hypothesized multiple group models of technical and procedural recording issues identified by the coders, these 42 cases (22%) did not alter the pattern of reported effects or the conclusions of the hypothesis testing.
Alternative models
When conducting the multiple group models presented above but using the CBCL Anxiety Problems raw scale, there was again no support for the mediational hypothesis between antenatal and postnatal predictors of CBCL Anxiety Problems via cortisol reactivity during the SSP at 12 months. Furthermore, neither attachment security nor attachment disorganization moderated this indirect path. Similar to the attachment security multiple group model predicting CAD, there were no significant differences between the regression parameters for the two groups. There were, however, significant differences between three of the attachment disorganization groups’ regression coefficients in the multiple groups model predicting CBCL Anxiety Problems. For the disorganized group, compared to the nondisorganized group, maternal major depression (β = −.30, p = .009 c.f. β = .03, p = .735), and maternal childhood trauma (β = −.28, p = .010 c.f. β = −.07, p = .309) were both significant predictors of child cortisol reactivity at 12 months. For the not disorganized group, compared to the disorganized group, maternal major depression was a significant predictor of Anxiety Problems (β = .18, p = .043 c.f. β = −.06, p = .726). In the full sample, maternal childhood trauma (β = .13, p = .070) and average maternal antenatal HCC (β = −.08, p = .163) were not significant predictors of anxiety problems.
Given the continuous attachment disorganization score was point-inflated, we treated the disorganization score as a set of semi-continuous variables: a binary semi-continuous disorganization variable comprising a group with a score of 1 (n = 79) compared with a group with scores ranging 2 through 7.5 (n = 111); and, a continuous disorganization variable restricted to only scores ranging 2 through 7.5 (n = 111), with scores of 1 handled as missing data. We argue that this approach acknowledges both the conceptual distinction in the continuous D score between a score of 1 (no signs of disorganization) and scores between 2 through 9 (the degree of observed patterns of disorganization), and the empirical point-inflated distribution observed in our sample. Due to difficulties including multiplicative interaction terms derived from the semi-partial variables in two-part modeling approaches, a model was conducted for the interaction between the semi-continuous binary disorganization score and then separately for the restricted continuous disorganization score. Using the binary semi-continuous disorganization variable, none of the multiplicative interaction terms were significant predictors of CAD. Further, scores ranging 2 through 7.5 on the disorganization score, compared to a score of 1, were not significantly associated with CAD at 4 years old.
In the restricted continuous model, only the multiplicative interaction term between maternal antenatal HCC and the disorganization score was a significant predictor of CAD at 4 years old (β = −.52, SE = .19, p = .007). In probing this significant interaction, analysis of simple slopes demonstrated that for restricted disorganization scores below the restricted average (M = 4.39), higher maternal antenatal HCC was associated with significantly higher logits of CAD (β mean-2 SD = 1.60, SE = .58, p = .006; β mean-1 SD = .92, SE = .37, p = .012), and for very high scores for restricted disorganization (2 standard deviations above the mean), higher maternal antenatal HCC was associated with significantly lower logits of CAD (β mean+2 SD = −1.13, SE = .55, p = .041). For average disorganization and one standard deviation above the average (approximately 6.00), maternal antenatal HCC was not a significant predictor of CAD at 4 years of age (β mean = .24, SE = .25, p = .346; β mean+1 SD = −.45, SE = .35, p = .196). Although the interaction pattern for the restricted semi-partial continuous component of attachment disorganization is consistent with the multiple group model for attachment disorganization, the estimated simple slopes at ± 2 SD from the mean represent associations between HCC and CAD for the extremes of the distribution of restricted attachment disorganization scores (i.e., −2 SD ∼ 2 and +2 SD ∼ 7). Inconsistent with this multigroup model, the restricted disorganization score did not significantly moderate the association between maternal antenatal depression and CAD (β = −.74, SE = .51, p = .152). Consistent with the secure multiple groups model, Richters attachment security score did not moderate any of the indirect and direct associations between early risk factors for CAD risks and CAD at 4 years age.
In the alternative models above, we also tested the indirect effects through attachment security and, separately, attachment disorganization between maternal childhood trauma, and depression and antenatal cortisol, to CAD at 4 years of age (i.e., Hypothesis 1). To test for mediation in the disorganization model, we entered the semi-continuous variable set simultaneously using a two-part path modeling approach. In both the two-part attachment disorganization model and the attachment security model, there were no significant indirect pathways between the early CAD risk factors and CAD at 4 years old both via the binary and semi-continuous disorganization variables, and via the security score.
Discussion
This study examined early stress-related risk factors for Childhood Anxiety Disorders at age 4, as well as the potential mediating role of children’s cortisol reactivity at 12 months of age and the moderating role of attachment security and disorganization in a sample of 190 mothers and children who were followed from pregnancy to 4 years of age. First, we found that, maternal antenatal HCC, depressive symptoms and a history of moderate to severe trauma directly predicted CAD at age 4. However, these associations were not mediated by the infant’s cortisol reactivity at 12 months of age. These findings were also independent of attachment security vs. insecurity, which did not moderate these associations. In addition, none of the attachment classifications in themselves, or when examined as insecure vs. secure attachment, were associated with an increased risk for Childhood Anxiety Disorders (CAD). As such neither hypothesis one or two were fully supported. For hypothesis three, we found when comparing disorganized vs. non disorganized dyads, both higher average maternal antenatal HCC and maternal depression in early pregnancy were each independently associated with significantly higher odds of CAD only in dyads who were not disorganized. Therefore, disorganized attachment did not increase the vulnerability from early life stress (maternal depression, early life trauma and antenatal cortisol) and/or from infant cortisol reactivity in developing CAD at 4 years of age and as such hypothesis 3 was not supported.
Our main finding suggests there may be different pathways from early predictors to CAD depending on the attachment organization. In children with organized attachment relationships, an increased risk for CAD was found in those whose mothers had antenatal depressive disorder and higher antenatal cortisol concentrations, whereas the converse was true for disorganized attachment. These suggest a possibility that there may be different pathways by which early life risk factors for CAD are moderated by attachment organization. In prior studies, disorganized attachment has been most strongly associated with poorer long-term outcomes for children including psychopathology, although effect sizes are mostly small to moderate (Granqvist et al., Reference Granqvist, Sroufe, Dozier, Hesse, Steele, van IJzendoorn and Duschinsky2017). Predictors of disorganized attachment have included parental risk factors such as unresolved past trauma, previous loss of a child, stress associated with low socio-economic status, depression, and teenage motherhood (Cyr et al., Reference Cyr, Euser, Bakermans-Kranenburg and van IJzendoorn2010; Flowers et al., Reference Flowers, McGillivray, Galbally and Lewis2018; McIntosh et al., Reference McIntosh, Schnabel, Youssef and Olsson2020). Our findings suggest early life stress including maternal depression and antenatal cortisol did not increase the risk of Childhood Anxiety Disorders in those with disorganized attachment.
As well as psychosocial stress, physiological measures of stress in the mother and child have been examined in relation to attachment classification; this has included infant cortisol reactivity, diurnal variation and mother–infant cortisol attunement (Ludmer Nofech-Mozes et al., Reference Ludmer Nofech-Mozes, Jamieson, Gonzalez and Atkinson2020; Luijk et al., Reference Luijk, Saridjan, Tharner, van IJzendoorn, Bakermans-Kranenburg, Jaddoe and Tiemeier2010). Disorganized attachment has been found to be associated with lower infant salivary cortisol and mother–infant cortisol mis-attunement; however, findings across studies are far from consistent and measurement of cortisol varies considerably (Ludmer Nofech-Mozes et al., Reference Ludmer Nofech-Mozes, Jamieson, Gonzalez and Atkinson2020; Luijk et al., Reference Luijk, Saridjan, Tharner, van IJzendoorn, Bakermans-Kranenburg, Jaddoe and Tiemeier2010). Furthermore, in a previous study, insecure attachment was found to moderate the relationship between exposure to higher amniotic fluid cortisol levels and infant cognition measured using the Bayley Scales of Infant Development at 17 months of age (Bergman et al., Reference Bergman, Sarkar, Glover and O’Connor2010). However, disorganization and also child mental health outcomes were not examined within this previous study (Bergman et al., Reference Bergman, Sarkar, Glover and O’Connor2010). What continues to be unclear is whether women with infants with disorganized attachment may have a range of different risk factors, unrelated to measures of maternal and infant physiological stress such as cortisol for a child to develop CAD compared to women with organized attachment. Overall, these findings of differential risk from organized compared to disorganized attachment can also only be regarded as preliminary because of the rather modest (intercoder) reliability of disorganized attachment assessments. Finally, these findings may also be explained in relation to the structure of the data, namely that a greater error variance in measures of disorganized attachment may lead to false positives. This will increase in smaller and also in higher risk compared to community samples. Therefore, independent replication of these findings is critical.
Another aspect of our findings is the use of a diagnostic measure of childhood anxiety disorders rather than relying on broader dimensional measures such as internalizing symptoms as measured using an instrument such as the Child Behavior Checklist (CBCL) or emotional symptoms on the Strengths and Difficulties Questionnaire. Both internalizing and emotional symptom scales, measured using these instruments, include symptoms across potentially a range of anxiety disorders and depressive disorders and not always reaching a clinical threshold. The majority of research examining attachment as a predictor of child mental health has relied on these dimensional scales within samples that typically have low numbers of children with mental health disorders. Interventions designed around anxiety in children also commonly rely on dimensional outcomes and are often designed for use across anxiety disorders rather than a specific condition (Lenz, Reference Lenz2015; Rooney et al., Reference Rooney, Morrison, Hassan, Kane, Roberts and Mancini2013). In considering attachment theory, it may be in that there are only specific childhood mental disorders that are predicted by attachment rather than the broad range of depressive and anxiety symptoms and disorders (Bretherton, Reference Bretherton1992; Cassidy, Reference Cassidy1994). For instance, as reported in our supplementary data, we did find a trend toward higher rates of ambivalent attachment in those specifically with separation anxiety disorder. Whereas those with secure, avoidant, or disorganized attachment were not strongly associated with any of the specific anxiety disorders. This can only be regarded as exploratory, as we were not powered to examine specific anxiety disorders in this study; however, this may also provide guidance in the design of future studies on anxiety disorders and attachment. While there have been a number of studies that have examined specific anxiety symptoms and attachment across infancy and childhood with mixed findings, there are few that have used diagnostic measures and most draw from lower risk populations for mental health disorders, where few children would meet a clinical threshold (Bar-Haim et al., Reference Bar-Haim, Dan, Eshel and Sagi-Schwartz2007; Brumariu & Kerns, Reference Brumariu and Kerns2010, Reference Brumariu and Kerns2013; Dallaire & Weinraub, Reference Dallaire and Weinraub2005; Kerns & Brumariu, Reference Kerns and Brumariu2014). The next step in future research could be to examine specific anxiety disorders in childhood. As it seems future research examining specific anxiety disorders and attachment in clinical samples are warranted in order to further explore the relationship between infant attachment and later vulnerability to anxiety disorders. This also has the potential inform interventions where specific attachment patterns may be an early risk for specific disorders and hence early interventions may be designed to target this early vulnerability to later specific anxiety disorders.
Limitations
The strengths of this study include the longitudinal design from early pregnancy to 4 years of age, multimethods for examining maternal depression including symptom and diagnostic measures as well as long-term (hair) and short-term (saliva) measurements of cortisol in pregnancy and in infants and also including robust measures of both attachment and of childhood anxiety disorders. However, there are several limitations. These include within this study a higher rate of childhood anxiety disorders, with 41.1% meeting diagnostic criteria, than would be anticipated. As previously reported this is likely due to the overrepresentation of women with not only current but also a lifetime history of depression and this has been previously noted (Galbally et al., Reference Galbally, Watson, van Rossum, Chen, de Kloet and Lewis2020). While this study focused on anxiety disorders, future studies on childhood depression are equally warranted. Further limitations include the sample size within each of the attachment classifications, the absence of father–infant attachment in understanding CAD, and the sample size precluded the examination of individual anxiety disorders. Furthermore, there was more limited inter-rater reliability for the continuous measure of attachment.
Conclusion
While the findings from this study suggest that attachment classification does not appear to be a strong influence on the development of childhood anxiety disorders as a single entity; nevertheless, this study did demonstrate that for organized compared to disorganized children there were different pathways from early life stress predictors to developing childhood anxiety disorders. Furthermore, this study highlights the importance of understanding early life stress including biological pathways in mother and infant for later childhood mental health outcomes and supports future research examining specific anxiety disorders.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579421001206
Acknowledgments
The authors would like to thank those who have supported the development of MPEWS including Michael Permezel. Sjoerd van den Berg for his advice and expertise in clinical chemistry particularly for the LC-MS aspects of hair analysis and also Yolanda de Rijke for her assistance with the hair analysis. The authors also thank staff, students, and volunteers on the MPEWS study as well as study co-ordinators Tina Vaiano and Jacinta Holland for their contributions to MPEWS. We are also sincerely grateful to the study participants who have contributed a substantial amount of time to participating in this study.
Funding statement
This study is supported through the 2012 National Priority Funding Round of Beyond blue in a three-year research grant (ID 519240) and a 2015 National Health and Medical Research Council (NHMRC) project grant for 5 years (APP1106823).
Conflicts of interest
None.








