Pulmonary artery stenosis is common in patients with CHD, and invasive pulmonary artery procedures may account for up to 20% of all catheter-based interventions in this population. Reference Rothman, Perry, Keane and Lock1,Reference Holzer, Gauvreau and Kreutzer2
Even this type of procedures are apparently safe, the procedure can be quite challenging and could be present with adverse events and some complications, specially related to the techniques of stent implantation, including stent slippage on the balloon during placement, balloon rupture during a stent implant, and stent malposition or embolization. Reference O’Laughlin, Perry, Lock and Mullins3,Reference McMahon, El Said and Vincent4
If the stent is not well centred on the balloon, and the stent can shift either proximally or distally during inflation, resulting in partial dilation of the stent. Typically, either the proximal or the distal edge is dilated more than the opposite end, resulting in a cone shape. In this case, the balloon will have to be deflated and recentered for repeat dilation to fully expand the stent.
In case of balloon ruptures, the balloon must be replaced with a new one. The insertion maneuver of a new balloon could risk distal migration of the stent. A bioptome or snare from a second venous sheath may be required to hold the stent in place during the exchange process.
When a stent has embolised, one may attempt to inflate a balloon inside and reposition the stent back into the stenotic pulmonary branch, but if the stent is already expanded, even partially, it usually cannot be placed back across the stenosis. In fact, there is no information about removal techniques of partial dilated stents after iatrogenic balloon catheter perforation.
Case report
We report the case of an 8-year-old male with history of surgical correction of type II truncus arteriosus when he was 5 years old.
His symptoms began 1 year prior to hospitalisation with significant decrease in his functional class and dyspnoea on slight exertion. On admission, the transthoracic echocardiogram reported severe stenosis of the two pulmonary branches.
Catheterization was performed. We performed an angiography at the Contegra tube visualising severe stenosis in the origin of both pulmonary arteries. We used 12-Fr Mullins-type sheaths and placed them beyond the stenotic portion of the pulmonary branches. Initially, we advanced a Palmaz Genesis 2910-mm stent mounted in a Z-MED 12 × 30 mm balloon to the right pulmonary artery and a Palmaz Genesis 2510-mm stent mounted in a similar balloon into the left pulmonary artery. However, when we tried to advance the PG 2510 mm stent, we could not reach the stenotic region because of the balloon protective covering. So, decision was made to cut and remove the balloon protective covering with a scalpel blade without realising that the balloon catheter had been punctured. Finally, we inflate both balloons observing a correct opening of the right pulmonary branch stent but an only partially open contralateral stent with blood leakage through the syringe, so we could realise that the balloon catheter had been erroneously perforated. We tried to recover the left stent but it was not possible because it was partially open so we decided to use a 10-mm snare which was advanced through the same venous access and across the two lumens of the balloon catheter and then was introduced into the Mullins-type sheath reaching the proximal edge of the stent (partially open site), compressing that part and finally attaching the stent completely to the balloon for pulling back and retrieving both the balloon and stent to the Mullins-type sheath (Fig 1). After that, because we did not have a new stent, we manually repair the used stent (Fig 2) and subsequently mount it on a different 12 × 30 mm balloon and finally advanced it and deploy it correctly into the left pulmonary artery. It is very important to comment that we were aware that there was a risk using the same stent; however, we made sure that the stent was very well fixed.

Figure 1. ( a ) Snare crossing across the lumens of the balloon catheter. The snare is inside a multipurpose catheter. ( b ) Snare before crossing the haemostasis valve (arrow) of the Mullins-type sheath. ( c ) Snare inside the Mullins-type sheath (in the same lumen) of the balloon catheter (arrowhead). ( d ) Fluoroscopy. Snare exiting Mullins-type sheath and across the stiff wire and the balloon catheter (arrow). ( e ) Fluoroscopy. Snare entrapment and compression of the proximal edge of the partial dilated stent (arrowhead). ( f ) Fluoroscopy. Retrieving the stent back into the Mullins-type sheath (asterisk).
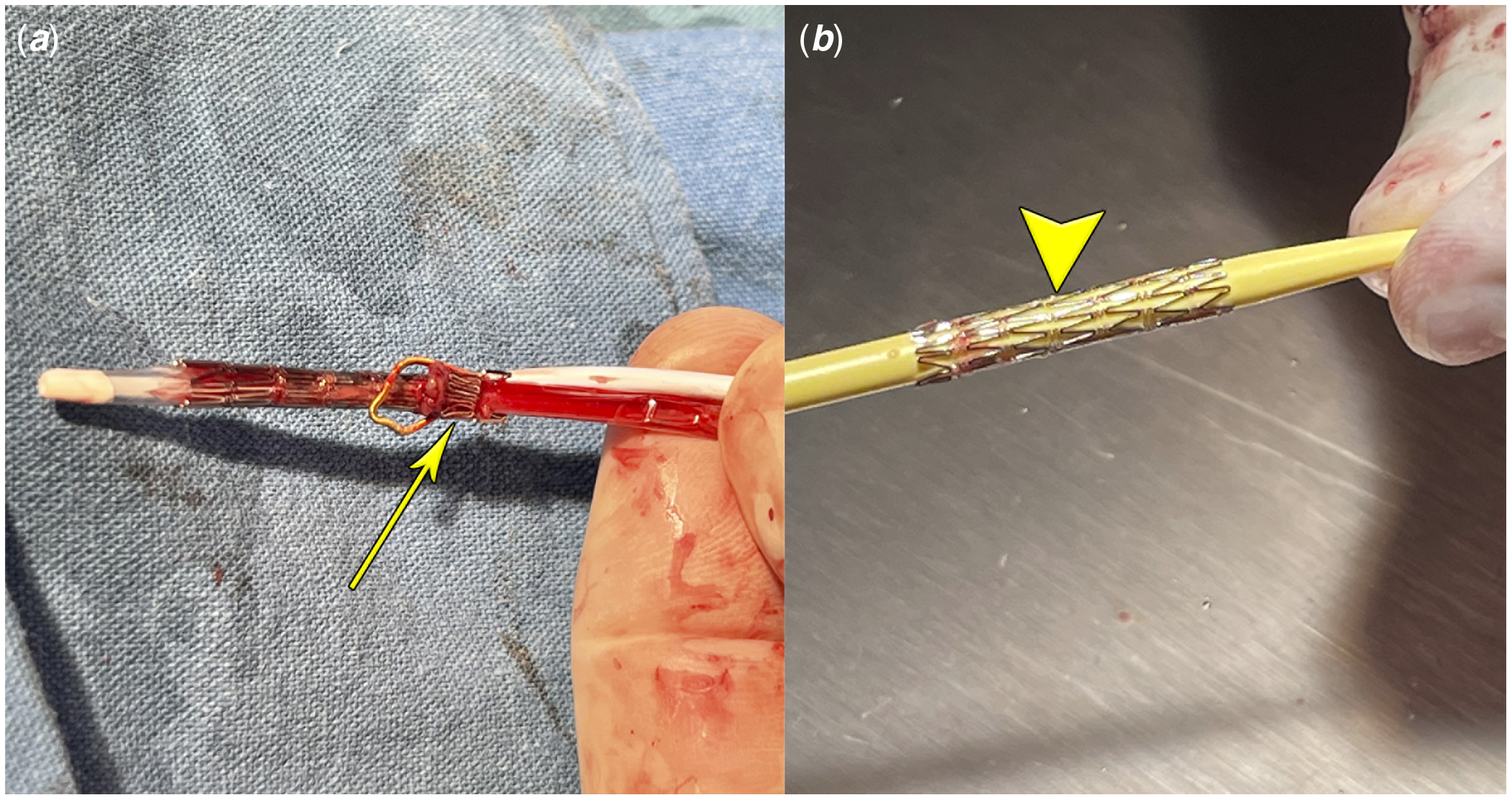
Figure 2. ( a ) Stent after removal using a snare. The stent is deformed in its proximal edge (arrow). ( b ) Stent after manual repair (arrowhead).
The patient showed improvement after the intervention and was discharged 4 days after the procedure with no complications. One month after the intervention, the patient showed improvement in his functional class with excellent clinical outcome. The stent is seen in excellent shape on echocardiogram.
Discussion
Over the past several decades, technological advances and innovative approaches have expanded therapeutic options for transcatheter rehabilitation of branch pulmonary artery stenosis. Reference Trant, O’Laughlin, Ungerleider and Garson5 Complications during this procedure can occur. A study from Children’s Hospital of San Diego showed that balloon rupture during stent implantation occurred in 22.4%. Reference Ing6 Other study published in 2016 reported complication rate of 14%, with 9% of patients experiencing death or major adverse events. Reference Lewis, Kennedy and Ginns7
In a multicenter study from the United States of America (Texas Children’s Hospital, Children’s Hospital of Michigan, and the Mayo Clinic), there were 10 complications overall. Major complications included stent migration, dissection, transient hypotension, thrombosis, reperfusion injury, and recurrent laryngeal nerve palsy. Minor complications included stent malposition, minor dissection, and aneurysm not requiring treatment. Of the two stent migrations, one was repositioned and restented successfully. The other underwent surgical repair. Reference Ing, Khan and Kobayashi8 We describe the perforation of a balloon catheter while trying to advance it to the stenotic pulmonary branch, which was caused while cutting the balloon protective covering with a scalpel blade causing an iatrogenic complication and how this prevented the correct expansion of the stent and therefore the impossibility of deployed it or retrieve it into the Mullins sheath.
In the literature, there are no previously cases reported using similar retrieval techniques. Our case is the first describing a different technique (Mij-Her technique) for percutaneous retrieval of a partial dilated stent after an inadvertent iatrogenic perforation of a balloon catheter during an attempted pulmonary artery stent angioplasty. There are a variety of techniques for stent removal in case of a fully expanded stent. Reference Hoyer9 However, no information exist in the literature about the specific complication that we show in our case.
Conclusion
Pulmonary artery stenosis, whether congenital or acquired, is a challenging problem. So, during pulmonary branch stenting procedures, a full armamentarium of interventional supplies and retrieval devices should be available in the catheterisation lab. Percutaneous snare capture and compression of a partial dilated stent for achieving a safe introduction into a long sheath is a safe and a novel technique in case of a iatrogenic catheter balloon perforation during pulmonary artery stenting
Acknowledgements
The authors thank all the cath team for the participation during this very challenger case.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.





