Introduction
Loneliness is surprisingly common in long-term care facilities (LTCF), despite people living physically close to each other (Gardiner et al., Reference Gardiner, Laud, Heaton and Gott2020; Jansson et al., Reference Jansson, Savikko, Kautiainen, Roitto and Pitkälä2020). It is associated with adverse health outcomes (Drageset et al., Reference Drageset, Eide, Kirkevold and Ranhoff2013; Jansson et al., Reference Jansson, Muurinen, Savikko, Soini, Suominen, Kautiainen and Pitkälä2017) and poor satisfaction with care (Kajonius and Kazemi, Reference Kajonius and Kazemi2016). Recent studies have explored older people's experiences of loneliness in LTCF (Victor, Reference Victor2012; Paque et al., Reference Paque, Bastiaens, Van Bogaert and Dilles2018; Barbosa Neves et al., Reference Barbosa Neves, Sanders and Kokanović2019; Jansson et al., Reference Jansson, Karisto and Pitkälä2021a) and how to alleviate them (Quan et al., Reference Quan, Lohman, Resciniti and Friedman2020).
According to Peplau and Perlman (Reference Peplau, Perlman, Peplau and Perlman1982), loneliness is a psychological state, a person's subjective response to a discrepancy between the desired and achieved levels of social contacts. Loneliness derives not only from a person's life experiences, but from various aspects of life in LTCF. It arises from a certain time and place in a person's life to which the context is strongly connected. It is also related to losses and social relationships, in which quality is more important than quantity. In LTCF, loneliness may be experienced in older people's many different realities. Their framework for loneliness may be formed by various times, places, social relations and life contexts (Victor et al., Reference Victor, Scambler and Bond2009; Jansson, Reference Jansson2020) (Figure 1).
Figure 1. Loneliness is related to social relations, place, time and context in long-term care facilities.
Source: Jansson (Reference Jansson2020).
Based on the inherent quality of experiences, previous literature has divided experienced loneliness into three dimensions – social, emotional and existential – originally explored and defined by Weiss (Reference Weiss1973) and Moustakas (Reference Moustakas1961). The difference between social, emotional and existential loneliness manifests itself according to the nature and context in which a person experiences the discrepancy between what is desired and achieved (De Jong Gierveld et al., Reference De Jong Gierveld, Tilburg, Dykstra, Vangelisti and Perlman2018). Emotional loneliness is mostly related to an intimate attachment (Dykstra, Reference Dykstra2009; Victor et al., Reference Victor, Scambler and Bond2009), and the integration of one's meaningful, close relationships, regardless of whether companionship is accessible. It is characterised by intense feelings of emptiness, abandonment and forlornness (De Jong Gierveld et al., Reference De Jong Gierveld, Tilburg, Dykstra, Vangelisti and Perlman2018). Social loneliness derives from a thin circle of friends (Dykstra, Reference Dykstra2009; De Jong Gierveld et al., Reference De Jong Gierveld, Tilburg, Dykstra, Vangelisti and Perlman2018) and is associated with feelings of exclusion from a community (Dykstra, Reference Dykstra2009). Social isolation may or may not lead to social loneliness. Emotional and social loneliness are qualitatively different, although they both involve the same agony and yearning (Weiss, Reference Weiss1973; Dykstra, Reference Dykstra2009). Studies exploring dimensions of loneliness among older residents in LTCF are lacking. However, some studies have explored social and emotional loneliness among community-dwelling older adults. According to Tiikkainen (Reference Tiikkainen2006), emotional and social dimensions are defined by partly the same and partly different factors related to various changes and losses in old age. An older person's emotional loneliness is not related to the quantity of their social contacts. However, loss of a spouse is an exception. Life satisfaction, emotional support and social cohesion are important in emotional loneliness. On the other hand, too few ties or companionships, a lack of instrumental support, low mood and poor functioning may lead to social loneliness. The latter makes it more difficult to stay in touch with other people (Tiikkainen, Reference Tiikkainen2006; Wolfers et al., Reference Wolfers, Stam and Machielse2021).
Existential loneliness has rarely been cited (Victor et al., Reference Victor, Scambler and Bond2009), but in recent years, attempts have been made to analyse it (Larsson et al., Reference Larsson, Edberg, Bolmsjö and Rämgård2018; Bolmsjö et al., Reference Bolmsjö, Tengland and Rämgård2019). Existential loneliness involves awareness of time, space and self, and knowing that a human being is ultimately alone (Moustakas, Reference Moustakas1961; Victor et al., Reference Victor, Scambler and Bond2009). It has been suggested to be related to end-of-life situations (Ettema et al., Reference Ettema, Derksen and van Leeuwen2010) and old age; characterised by meaningless waiting, experiences of exclusion and restricted freedom (Larsson et al., Reference Larsson, Edberg, Bolmsjö and Rämgård2018). Unlike social and emotional loneliness, existential loneliness may also be valued positively despite its negative associations (Moustakas, Reference Moustakas1961; Ettema et al., Reference Ettema, Derksen and van Leeuwen2010; De Jong Gierveld et al., Reference De Jong Gierveld, Tilburg, Dykstra, Vangelisti and Perlman2018). It is considered a pathway for self-growth, creativity and inspiration (De Jong Gierveld et al., Reference De Jong Gierveld, Tilburg, Dykstra, Vangelisti and Perlman2018).
Studies exploring the experience of loneliness in LTCF are still scarce. However, linguistic expression could bring out loneliness and make it real (Ettema et al., Reference Ettema, Derksen and van Leeuwen2010). Most studies are based on the prevalence of loneliness, despite its subjective nature (Tiilikainen and Seppänen, Reference Tiilikainen and Seppänen2017). Studies have explored the dimensions of loneliness even less. Pirhonen et al. (Reference Pirhonen, Tiilikainen and Pietilä2018) suggested that residents in LTCF experience social loneliness, which arises from weak bonds both inside and outside the facilities: with co-residents, staff and other people. Emotional loneliness arises in situations in which other residents live physically close but are emotionally distant (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a). Existential loneliness is when residents feel mentally homeless in the facilities (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a). It has also been related to the timeline of life; in old age one is aware of death approaching (Ettema et al., Reference Ettema, Derksen and van Leeuwen2010; Österlind et al., Reference Österlind, Ternestedt, Hansebo and Hellström2017; Hemberg et al., Reference Hemberg, Nyqvist and Näsman2019; Jansson et al., Reference Jansson, Karisto and Pitkälä2021a).
According to Perissinotto et al. (Reference Perissinotto, Holt-Lunstad, Periyakoil and Covinsky2019), social and health-care professionals have not sufficiently acknowledged or recognised older residents’ loneliness, nor have they yet developed a work routine of asking about and documenting related experiences. To be able to alleviate loneliness, professionals need to ‘diagnose’ the resident's experiences: to determine what kind of loneliness a person is experiencing. Only by recognising loneliness can professionals provide tailored care and support and implement interventions accordingly (Pitkälä et al., Reference Pitkälä, Jansson and Savikko2019). To understand the multi-dimensional phenomenon of loneliness, the voices of older people should be heard (Kitzmüller et al., Reference Kitzmüller, Clancy, Vaismoradi, Wegener and Bondas2018). However, the understanding of how experiences of loneliness manifest in the three dimensions of loneliness is limited. This may be due to the scarcity of qualitative studies of loneliness in LTCF (Jylhä and Saarenheimo, Reference Jylhä, Saarenheimo, Dannefer and Phillipson2010).
Aim and methods
Aim
The aim of this study was to explore how the experiences of loneliness of older people in LTCF are manifested and divided into three different dimensions: social, emotional and existential loneliness.
Settings and participants
The present study was part of a larger project examining loneliness, its prevalence, associated factors and prognosis, and how experiences of loneliness are expressed and articulated in LTCF in Helsinki, Finland (Jansson et al., Reference Jansson, Muurinen, Savikko, Soini, Suominen, Kautiainen and Pitkälä2017, Reference Jansson, Savikko and Pitkälä2018, Reference Jansson, Karisto and Pitkälä2021a, Reference Jansson, Karisto and Pitkälä2021b).
The study was conducted in two assisted living facilities (later LTCF): ‘Bright House’ with 90 residents and ‘Long House’ with 150 residents. Both facilities offer residents housekeeping, meals-on-wheels, and 24-hour support and nursing. According to the facilities’ goals, the work orientation of the staff – managers, cleaners, nurses, physiotherapists, occupational therapists and social instructors – is client centred and rehabilitative. The aim is to respect each resident's individuality and uniqueness. In both houses, older people may freely use common spaces such as the sauna, clubrooms, gym, dining room, hobby room and television (TV) lounges. A weekly social programme, including music and singing, instructed gym sessions and facilitated games, is available in both facilities.
We excluded residents with severe dementia, who were unable to provide reliable responses regarding their experiences of loneliness. After the initial information, we approached 16 residents through the staff to recruit them for the study. Of these, 13 experienced loneliness and were recruited. Six lived in Bright House and seven in Long House. In Long House, the participants had no cognitive impairments (Mini-Mental State Examination (MMSE) > 24/30p) and lived in their own apartments. In Bright House, the participants were mildly or moderately cognitively impaired (MMSE 15–24p) and lived in their own rooms in group homes. Perceived loneliness was the main inclusion criterion of the study. This was elicited by a written questionnaire containing a single question: ‘Do you suffer from loneliness?’ (seldom or never/sometimes/often or always). This question has been used in many studies and has proven to be easy for older people to understand and answer (Savikko, Reference Savikko2008; Tilvis et al., Reference Tilvis, Routasalo, Karppinen, Strandberg and Pitkälä2012). It also suits the cultural context in Finland, in which yksinäisyys, loneliness, may also mean solitude to some. Thus ‘feeling lonely’ was not worth eliciting in this study. Residents who experienced loneliness at least sometimes were recruited.
Data collection
The study was conducted and the data collected carefully in accordance with ethical guidelines. After the Helsinki University Hospital ethics committee and the respective committee of Helsinki City approved the study protocol, the management of the houses were contacted, and they granted permission for the study. The staff and residents were informed in detail of the study, with the help of information sheets. After this initial information, we approached individual residents through the staff in order to recruit them. The potential respondents received information on data collection. We emphasised that participation in the study was completely voluntary and that they could withdraw at any time.
The study was inspired by the qualitative longitudinal research approach (Nikander, Reference Nikander2014). Data were collected over a six-month period. The first author of the article (AHJ) entered the everyday lives of the older people in the facilities. The data were collected using a multi-method ethnographic approach that involved individual interviews, group meetings, informal chats and observations. This multi-method approach supports triangulation (Groger and Straker, Reference Groger, Straker, Rowles and Schoenberg2002). In Finland, some ethnographical studies have found experienced loneliness in care settings (Pirhonen, Reference Pirhonen2017; Pirhonen et al., Reference Pirhonen, Tiilikainen and Pietilä2018). Pirhonen's (Reference Pirhonen2017) work particularly inspired our study. He found that assisted living facilities aim to increase residential satisfaction and foster a meaningful and valuable life, but that there may be a gap between these goals and reality in care practices, leading to affiliation ruptures (Pirhonen, Reference Pirhonen2017; Pirhonen et al., Reference Pirhonen, Tiilikainen and Pietilä2018). Therefore, we aimed to deepen our understanding (Gubrium, Reference Gubrium, Henderson and Vesperi1995) of the ‘real-life loneliness’ in the microculture of two LTCF in Helsinki, Finland using an ethnographic method. We explored and wanted to learn how people experienced loneliness in their everyday lives and living surroundings as well as in group meetings with peers. We wanted to look more closely at the experiences of loneliness in these contexts and surroundings, that is, the everyday environment in which this suffering and these emotions take place (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a).
The respondents received our complete attention in the interviews (Heyl, Reference Heyl, Atkinson, Coffey, Delamont, Lofland and Lofland2001) and we listened properly to their stories, carefully and respectfully. The respondents’ right to remain silent was respected, and attention was paid to the situations in which they did not speak. Each participant was individually interviewed twice: at the beginning and at the end of the data collection. The interviews were recorded. The duration of the individual interviews varied from half an hour to one-and-a-half hours. They were informal discussions, in which participants openly shared their experiences. A three-month Circle of Friends group process was offered to the lonely participants between the individual interviews (Jansson et al., Reference Jansson, Savikko and Pitkälä2018): this involved the participants in both houses meeting once a week and each meeting being facilitated by two trained group facilitators. AHJ observed the participants’ experiences and articulations of loneliness, as well as the procedure and contents of the group process at the beginning, middle and end. Free discussions were recorded during the observations and included in the analysis. Focus group interviews of five participants in Bright House and three participants in Long House were conducted and recorded after the three-month group intervention. The duration of the focus groups in both houses was one hour and 40 minutes. AHJ wrote a field diary after the individual and focus group interviews as well as during the Circle of Friends group process.
Data analysis
Data analysis began with the reading and re-reading of the 810 transcribed interview pages (Times New Roman, 12 point, single spacing) and observation field notes of around 50 hand-written pages, to reach a comprehensive understanding of the rich data. With the help of the computer software Atlas.ti (Hwang, Reference Hwang2008), the data blocks (106) of loneliness were first identified from the Finnish words loneliness (yksinäisyys), lonely (yksinäinen) and their derivatives. The participants also used many other words and phrases to describe ‘loneliness’. Manual mapping enabled us to identify the relevant data blocks of idiosyncratic loneliness (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a). Mapping resulted in a total of 546 segments of loneliness to distinguish data blocks describing experiences of loneliness and its associated everyday life situations. Time- and place-dependent experiences of loneliness have also been reported elsewhere, as has another group process for lonely participants (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a, Reference Jansson, Karisto and Pitkälä2021b).
Analysis leant on abductive reasoning (Timmermans and Tavory, Reference Timmermans and Tavory2012; Mirza et al., Reference Mirza, Akhtar-Danesh, Noesgaard, Martin and Staples2014), finding clues from the data as well as from the loneliness literature. Many respondents described their experiences very similarly at different points in the data collection. This confirmed the reliability of the data, but these repeated expressions and duplicates in the statements affected the amount of data. Therefore, we ignored duplicates, but recognised them as background data. Seventy segments were chosen for closer analysis: larger textual blocks and individual sentences. These provided relevant information from the viewpoint of the dimensions of loneliness: social, emotional and existential.
We coded the segments and grouped the codes into categories, inspired by the coding practices typical of the grounded theory (Charmaz and Mitchell, Reference Charmaz, Mitchell, Atkinson, Coffey, Delamont, Lofland and Lofland2001; Timmermans and Tavory, Reference Timmermans and Tavory2012; Foley and Timonen, Reference Foley and Timonen2015). The core categories, social, emotional and existential loneliness, were both the starting and endpoints of the analysis. The starting point was a trichotomy of the dimensions of loneliness found in the literature, and the results were its supplemented picture of how the dimensions appeared in the data. Between these, we made a multi-dimensional journey, stopping at turns in the data and subcategories as well as in the loneliness literature.
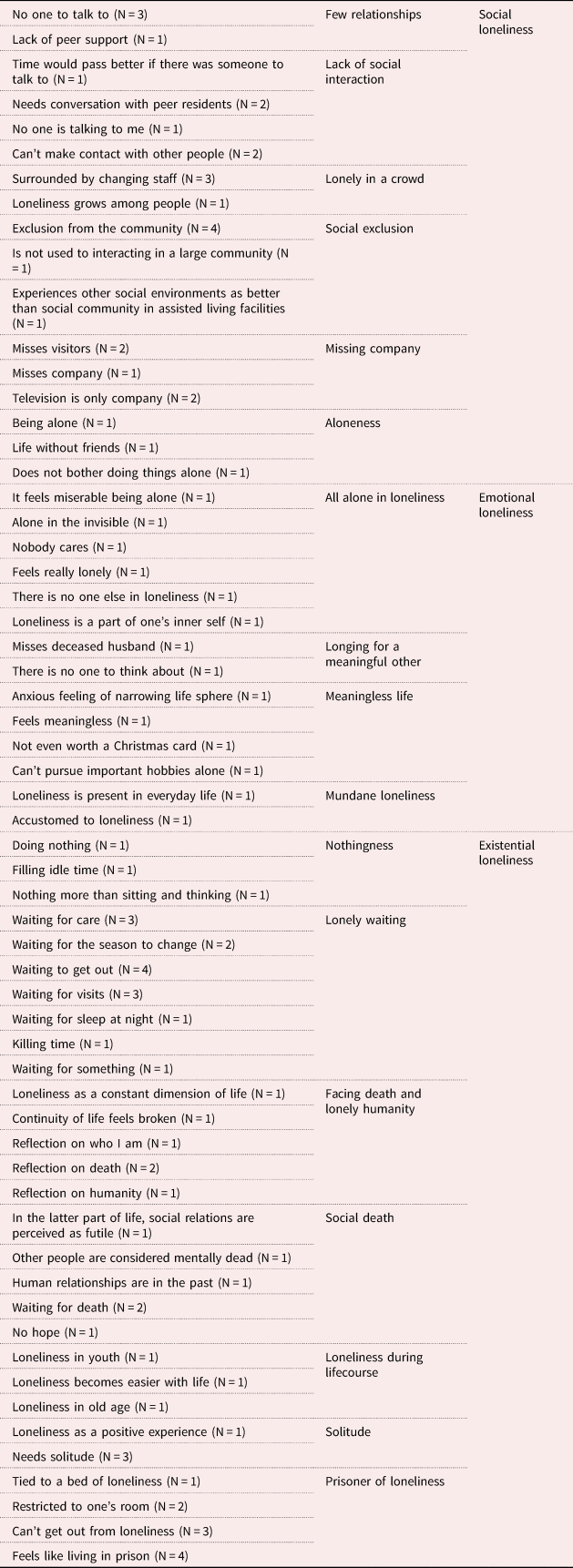
The categories were thus constructed from numerous experiences of loneliness and clues from the literature. For example, ‘no hope’, ‘human relations are in the past’, ‘other people are perceived as mentally dead’ and ‘social relations are perceived as futile’ produced a further ‘social death’ category. Along with the other categories – ‘prisoner of loneliness’, ‘solitude’, lonely humanity’, ‘lonely waiting’ and ‘nothingness’ – this new category was related to the core category of existential loneliness (Table 1).
Table 1. Categories formed from a rich variety of experiences
Results
The material was abundant and varied in its descriptions of loneliness. Half of the respondents from both houses described loneliness in their first individual interview in notably general terms, not explicitly – even trying to avoid the painful topic while speaking of their experiences. As data collection progressed, people became more familiar with and more open about the topic. In the group meetings and focus groups, the facilitators and group participants encouraged each other to express their experiences of loneliness.
Experiences of loneliness were richly manifested in the dimensions. The respondents had many experiences of few relationships and a lack of social interaction, and they felt socially excluded and lonely in a crowd. They also missed company and felt alone, although they lived side by side in LTCF. These categories came under social loneliness. In emotional loneliness, however, the respondents felt all alone in loneliness. They longed for a meaningful other and a meaningful life. Loneliness seemed to be even mundane to them. Nothingness and lonely waiting were part of existential loneliness, of which some felt they were prisoners. They had experienced social death in their lives. Existential loneliness was reflected during the lifecourse and was experienced as facing death and lonely humanity. As typical in existential loneliness, in LTCF it was related to solitude. These experiences and manifestations of dimension were by no means formed in a vacuum. Their roots were in the time, place and context in which the residents lived and the social relationships around them (Figure 2). Next, we describe the experiences in more detail, focusing on the voice of the older people.
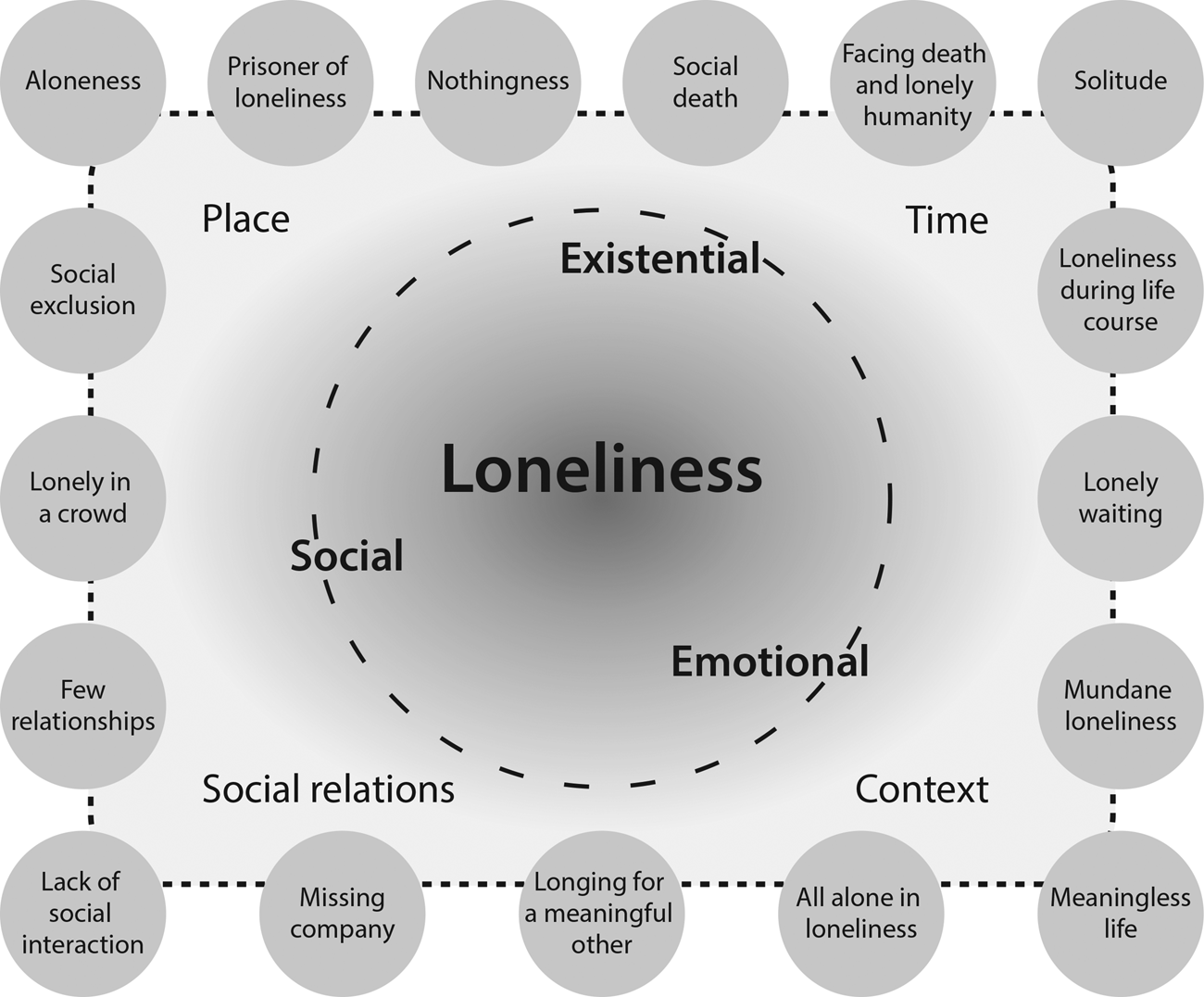
Figure 2. Multi-dimensional phenomenon of loneliness according to experiences of older people in long-term care facilities: social, emotional and existential aspects.
Social loneliness
Many lonely respondents felt that they had too few relationships, had no one to talk to and that they spent much of their time alone. In loneliness, they suffered from a lack of social interaction or a lack of peer support. Eleonora, in the first individual interview in Long House, asked, ‘When loneliness strikes, where can I go? Nowhere. There should be some kind of space where you can sit with others at an agreed time.’ Many expressed having only a few conversations with peer residents in their daily lives, like Eleonora: ‘I feel lonely when I have no one to talk to.’ The lack of conversation was mutual; she did not talk to others and simultaneously wondered ‘why is no one talking to me?’ The difficulty of making contact was justified by, for example, language problems, or being shy or reserved. In her individual interview before participating in the group, Sophie pondered, ‘Maybe I'm a little bit shy, I don't really dare participate. I don't think I know the right things to do in the group.’ Many of the expressions of social loneliness were metaphorical, such as ‘I never get over the fence that prevents me from being in contact with others.’ This comment from a cognitively impaired Silvia referred to situations in which other residents passed her in the hallways, but the respondent believed she was unable to initiate a conversation with them.
They missed company: visitors, friends, children and grandchildren: ‘Saturday and Sunday are the lonely days, other people get visitors, but I don't.’ Several respondents pointed out that TV was their only regular company: ‘But television is okay. Without television, I'd have a hard time’, Keith from Bright House said in his individual interview. An excerpt from the focus group discussion in Long House demonstrates how the concept of loneliness is constructed and shared among the participants:
Sophie: I often miss my loved ones.
Sissy: No one came to visit me over the weekend.
Sophie: The weekend is often a bad time for me too.
Sissy: Oh, it is.
Birgit: When I'm alone in my room (pause). I have a daughter who lives with her family nearby. But they don't have time to visit. They have their own time pressures. And I don't demand that they come. They very recently went on vacation as well. Let them go.
Sissy: You miss them, don't you?
Sophie: That's somehow how it is. And there's absolutely nothing to watch on TV on the weekends. There should be at least old movies on offer.
Sissy: They're all reruns.
Birgit: And they lie that the reruns are at the request of the public.
Feeling lonely in a crowd was a very common feeling. In Bright House, Silvia said in her individual interview: ‘When some interesting programme is on the TV, we all gather in the chairs around it. But it doesn't take long until some people are snoring. It bothers me.’ The respondents felt that loneliness emerged when they were with other people who were not mentally accessible. ‘It was so shocking how demented the people here were. I started to whine about having no one to talk to’, Rose said. Loneliness was also very common when ‘someone just visits, does something and rushes away. That causes loneliness’. Members of the staff came and went, and the staff caring for the resident changed frequently.
One of the main things related to social loneliness in the houses was the feeling of social exclusion. The respondents felt excluded from the community and groups inside the houses, ‘When I went to a new group that already existed, it wasn't easy to get in’, Emma in Long House explained in her individual interview before the group intervention. One person isolated himself from the others because he was not accustomed to large groups. The respondents in the houses also perceived themselves as separate from surrounding society and nature, which the residents could not often reach, but which seemed important to them. Sissy in Long House discussed in her second individual interview:
If I get out, I'm not lonely anymore. I take a taxi and go to the mall to do some window shopping and drink tea. I spend a few hours there and take a taxi back. Once again the day is saved.
She had found a way to cope with her loneliness.
Emotional loneliness
The respondents expressed the feeling that they were all alone in their loneliness: ‘It feels miserable being alone all the time.’ In the group discussion, this issue was linked to being alone in the room: ‘I feel more pain when I'm alone in my room. In this group I can forget my pain.’ Many of the respondents expressed that there was no one else with whom to share their feelings. Violet in Long House claimed that she lived in invisibility in her loneliness, despite several activities in the house: ‘When no one pays attention to me, I disappear.’ This was related to the feeling that nobody cared, nobody paid attention. Experiences of loneliness triggered anxiety and feelings of being very lonely. Many times, when talking about loneliness, these feelings were also shown on a person's face and in their gestures. These observations were recorded in the field notes, as in the following example:
When asked about loneliness the interviewee became tearful, whereupon the interviewer was also sensitised. After a silent moment, the interviewee started talking about her loneliness using few, but strong, emotional words.
The respondents longed for meaningful others and felt they had a meaningless life: ‘I miss my husband. We were married for 60 years.’ Many of the respondents felt completely meaningless and useless, ‘I'm not even worth a Christmas card.’ The experience of loneliness had become mundane and trivial for some older people, because they felt loneliness in their everyday lives. Lars in Bright House speculated that ‘I've been so engaged with loneliness that I'm used to it’. The feelings related to loneliness had also become milder, ‘I was told that time heals, but I wasn't sure it would. But it seems to have worked!’ Experiences of loneliness seemed to change both during the lifecourse and over a shorter period of time.
Existential loneliness
Lonely waiting was part of almost every respondent's life: ‘This life has become just lonely waiting. I'm just constantly waiting for something.’ They waited for their care, for the season to change, to get out, for company, for sleep at night. Lonely waiting manifested when, for example, Violet living in Long House sat at a set coffee table and revealed in her individual interview: ‘I'm waiting for the priest. The priest visits me once a week. She won't be here tonight, but I still set the table and got the coffee cups ready.’ She knew that the priest would be on vacation until the following week. Many times, waiting had no target. Killing time was a daily task, and TV was a very important tool for this. Some of the respondents reported that they just sat and did nothing. In their loneliness, they felt they were ‘living in nothingness’.
Loneliness was a constant dimension of life for many respondents. At the same time, it was perceived as a part of lonely humanity, and expressed in a harsh way. ‘We are put into boxes. And fed through a hatch’, Sissy summed up the lively discussion in the group intervention at Long House. Emma described in her individual interview and in the group discussions how she felt she was part of a broken chain of generations: ‘I'm the last in my family. All the traces have been scraped on to me, but after me there'll be nothing. It feels strange that there are no descendants.’ In existential loneliness, the respondents truly reflected on the fundamental issues of humanity: ‘I don't know if it's loneliness or what. Or is it about who or what I really am.’ Existential loneliness seemed to refer to the variable emotional landscape along the lifecourse. It was present in lonely life, and lonely death.
Some of the respondents thought that human relationships were a thing of the past. Violet in Long House was not satisfied with her peers or support in the group intervention: ‘I feel I have nothing to tell the group and there's no one to make friends with.’ Violet and Rose in Long House were waiting for death, and Violet believed there was no longer any hope: ‘After all, you can't plan a future here. And hope is completely gone.’ These respondents with thoughts of social death seemed to consider social relationships at the end of life as quite futile. ‘We're all near death and we don't need to be here very long, so why should we invest in life anymore?’, Rose speculated. Respondents also reminisced about their deceased friends and in this way kept their memories alive.
Feeling like a prisoner in one's loneliness is a strong description of the experience of loneliness, but the respondents used this metaphor. Many of them were restricted to their rooms, and could not get away from their loneliness. In the group conversation, four participants with no cognitive impairment ironically discussed how they felt that they were living in a prison:
Sophie: Do you think this is a prison?
Birgit: Yes, I do.
Sissy: But prisoners are able to shower twice a week and get outdoors every day.
Rose: You can't leave. In prison you can at least get a holiday.
Some respondents compared themselves to other residents: ‘Of course, those in a wheelchair or tied to a bed. They may suffer even more from loneliness.’ They believed some of the residents were even worse off. At the same time, these explanations seemed to be attempts to explain and justify one's own experiences to oneself.
However, some expressions related to loneliness were also positive. The respondents in both houses described significant artefacts and cherished objects that aroused feelings of solitude. Violet, who had been waiting for a priest for many days in Long House, explained how ‘ticking makes the room cosy and alive. I have six clocks ticking in here’. The respondents emphasised how they missed solitude, especially in the midst of changing, busy staff: ‘For heaven's sake, can't I get any privacy or peace here at all?’ and ‘My temperament needs aloneness from time to time.’ While they experienced loneliness, they also perceived aloneness, solitude and privacy as something they needed.
An excerpt from the focus group discussion in Bright House demonstrates experiences of solitude and privacy:
May: I enjoy being alone.
Alea: So do I.
May: When it's often loud and noisy here, you get tired of it.
Alea: Yes.
May: Loud people shout in the hallways.
Keith: Yes, privacy should be respected.
Lars: Different people perceive loneliness differently. Someone can be lonely all the time, no matter how many groups they participate in.
Keith: However, (five-second pause) every person needs to be alone. When being alone goes to extremes, then it's a difficult thing. These are the big questions of life.
The excerpt is a practical example of how the experiences were constructed and shared among cognitively impaired participants in the LTFC.
Discussion
This study, conducted in two assisted living facilities in Helsinki, Finland, examined 13 older people who experienced loneliness at least sometimes. The results showed all three dimensions of loneliness – social, emotional and existential – and that they related to a variety of experiences. Social loneliness meant that the respondents felt they had no one to talk to and lacked peer support. They missed company but were also lonely in a crowd. Even when they were among other people, they felt socially excluded. Emotional loneliness made them feel miserable, and they were unable to share their feelings with anyone. This loneliness was related to a meaningless life and a lack of meaningful others. Existential loneliness was related to solitude, but also filled with lonely waiting and emptiness. It emerged from some of life's most difficult issues such as involuntary childlessness, the feeling of breaking the chain of generations and approaching death. At the same time, the respondents reflected on fundamental issues of humanity. Many of their experiences consisted of feelings related to social death and expressions of prison.
The present study is one of the first to explore the dimensions of the experiences of loneliness among older people in institutional settings. One of its main strengths is that it targeted frail older people, half of whom were cognitively impaired. Previous qualitative studies have rarely addressed the experiences of this target group (Paque et al., Reference Paque, Bastiaens, Van Bogaert and Dilles2018). The results of this study encourage researchers to include cognitively impaired older people in studies that explore loneliness. Those with and without cognitive impairment described their loneliness in both similar and different ways. Both used rich metaphors when speaking about loneliness. However, unlike people without cognitive impairment, many of the respondents with cognitive impairment described their experiences using similar expressions at different time points of the research process. Another strength is that the study had a clear focus: all the participants experienced loneliness at least sometimes.
A limitation of this study is the way in which it measured loneliness. We asked, ‘Do you suffer from loneliness?’, but this question does not really capture the dimensions of loneliness, as does, for example, the De Jong Gierveld Loneliness Scale (De Jong Gierveld and Van Tilburg, Reference De Jong Gierveld and Van Tilburg2006). A second limitation is that Finnish cultural aspects were not taken into account in the analysis. Older residents’ experiences of loneliness may be affected by certain aspects of Finnish culture and the staff's work orientation in Finnish assisted living facilities. Thirdly, the experiences of the respondents may not be comparable to those of other residents, and thus transferability to other contexts or facilities is not guaranteed (Kylmä and Juvakka, Reference Kylmä and Juvakka2007). In other facilities, experiences may be formed differently, with different times, places, contexts and respondents. Furthermore, the results are not at all applicable to older people who are not lonely in LTCF.
The findings of this study related to social loneliness are in line with the those in the previous literature (Weiss, Reference Weiss1973: 18–19; De Jong Gierveld et al., Reference De Jong Gierveld, Tilburg, Dykstra, Vangelisti and Perlman2018). They derive from feelings of exclusion and a dissatisfactory social network. Also in line with previous studies, losses, unfulfilled contacts and a narrowed social network formed the basis of the respondents’ loneliness (Kirkevold et al., Reference Kirkevold, Moyle, Wilkinson, Meyer and Hauge2013; Taube et al., Reference Taube, Jakobsson, Midlöv and Kristensson2016; Österlind et al., Reference Österlind, Ternestedt, Hansebo and Hellström2017; Tiilikainen and Seppänen, Reference Tiilikainen and Seppänen2017). Thus, the loneliness of older people in LTCF derive from similar experiences to those of community-dwelling older people (Tiikkainen, Reference Tiikkainen2006). However, loneliness also emerged in the company of other people: some residents felt lonely even when in a crowd (Newall and Menec, Reference Newall and Menec2019). According to Jakobsson and Hallberg (Reference Jakobsson and Hallberg2005), this may be considered a paradox. Those who live by themselves should be expected to feel lonely, and those who live in long-term care settings should ‘meet and greet’ other residents and personnel. The results of this study are important from the perspective of loneliness research and reinforce the premise of loneliness: it is essential that social relationships meet older people's own expectations (Derlega and Margulis, Reference Derlega, Margulis, Peplau and Perlman1982; Savikko, Reference Savikko2008: 67).
Older people who view their social surroundings as negative may distance themselves from others. This may result in greater levels of loneliness (Ayalon, Reference Ayalon2018). The community may also exclude an individual, even if inclusion is the common goal of the facilities’ social and health-care professionals. Therefore, not everyone gets involved in communities and groups – on the contrary – they may be rejected, which can lead to social exclusion and loneliness (Okulov, Reference Okulov2008: 93). In addition to social loneliness (Weiss, Reference Weiss1973: 18–19), social exclusion may also lead to existential loneliness. According to Edberg and Bolmsjö (Reference Edberg and Bolmsjö2019), existential loneliness may be an experience of being separated from others and the world even when one has social relationships.
In previous studies, losses and longing for meaningful and close relationships have been expressed through grief, meaninglessness and uselessness (Weiss, Reference Weiss1973: 20–21; Kirkevold et al., Reference Kirkevold, Moyle, Wilkinson, Meyer and Hauge2013; Tiilikainen and Seppänen, Reference Tiilikainen and Seppänen2017). The respondents in this study had too few meaningful others or meaningful activities. Involuntary childlessness was related to a deep feeling of life being meaningless. Tiilikainen and Seppänen (Reference Tiilikainen and Seppänen2017) considered childlessness to be behind emotional loneliness. In this study, childlessness was also related to a part of human continuity as well as ‘something greater’ and was thus anchored more closely to existential loneliness.
In many cases, the expressions indicated existential loneliness. These experiences were related to time, space and self, and included a few positive aspects (Moustakas, Reference Moustakas1961; Ettema et al., Reference Ettema, Derksen and van Leeuwen2010). Taube et al. (Reference Taube, Jakobsson, Midlöv and Kristensson2016) describe how loneliness may be seen as a bubble, the walls of which are formed by physical, psychological and social barriers. Kitzmüller et al. (Reference Kitzmüller, Clancy, Vaismoradi, Wegener and Bondas2018), in turn, describe existential loneliness using a metaphor of being ‘trapped in an empty waiting room’. This study used the metaphor of prison, with quite similar meanings to those of the bubble or waiting room. Inside the walls of the prison, some of the respondents had almost constant negative emotions of loneliness, with empty waiting and nothingness. However, in contrast, some experiences, such as solitude, were positive; some residents actually enjoyed being alone (Ettema et al., Reference Ettema, Derksen and van Leeuwen2010; Taube et al., Reference Taube, Jakobsson, Midlöv and Kristensson2016; Kitzmüller et al., Reference Kitzmüller, Clancy, Vaismoradi, Wegener and Bondas2018; Larsson et al., Reference Larsson, Edberg, Bolmsjö and Rämgård2018).
Experiences of loneliness manifested themselves through dimensions, but at the same they were also attached to time, place and social relationships. The respondents’ loneliness often struck in the evenings, at weekends and in the wintertime, as demonstrated in our previous article (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a). The experiences were also anchored in life's three time horizons: the past, the present and the future (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a). However, the study was conducted from winter to summer, towards increasing light. The results may have been different if the study had been conducted in the autumn, moving towards the Finnish polar nights. Experiences of loneliness were even more place-dependent in Long House (Jansson et al., Reference Jansson, Karisto and Pitkälä2021a). Older residents there used a coarse prison comparison when describing their living surroundings. In both houses, the respondents suffered from a lack of meaningful others, but at the same time needed more privacy. Poor mastery of life was evident in both houses. Lonely older adults living in an assisted living facility perceived themselves as bystanders in their own daily lives. As in a previous study by Pirhonen (Reference Pirhonen2017), they felt invisible and not recognised as persons.
Death was closely related to existential loneliness. Social death (Borgstrom, Reference Borgstrom2016) was when the respondents felt they were losing their social identity and social connectedness. It was also felt when other respondents with dementia were perceived as socially dead, and not worth interacting with. Some of the respondents reminisced about their deceased friends, whose memories they cherished. According to Borgstrom (Reference Borgstrom2016), social death may not occur until someone is forgotten. Some of the lonely respondents were waiting for death, one of the most intimate and difficult times of one's life (Routasalo and Pitkälä, Reference Routasalo and Pitkälä2003; Österlind et al., Reference Österlind, Ternestedt, Hansebo and Hellström2017). However, this had not only negative associations; it was also considered a relief.
Conclusions
Older people's loneliness in LTCF is a multi-dimensional, complex phenomenon. The experiences of the respondents varied, were heavy and needed to be heard. Their voices told of how loneliness has many social, emotional and existential aspects, which brings measuring and screening loneliness into a new light. In addition to asking about loneliness, it is important to discuss loneliness in LTCF in a varied and regular manner. Peer discussions are important: even very frail people with mild or moderate cognitive impairment were able to reflect on their experiences in group discussions. Finally, in the light of this study, it is worth critically examining the well-intentioned goal of increasing clubs and activities for the residents to alleviate loneliness. The core of loneliness does not always lie in insufficient activities or social relationships. Existential loneliness, for example, was associated with the presence of approaching death and needs to be addressed by other means. Among older people in LTCF, two life events are really close in the past and in the future of their lifecourses: moving from a ‘real’ home to assisted living and approaching death there. It is obvious that the time between should be made as enjoyable as possible. Not by just any means, but via well-designed, meaningful approaches that address loneliness from the necessary perspectives.
Financial support
This work was supported by Helsinki City; a Helsinki University Hospital; the Olvi Foundation (grant number 201810048); the Signe and Ane Gyllenberg Foundation; the Miina Sillanpää Foundation; and the Orion Research Foundation sr (grant number 180044).
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
This research was approved by the Helsinki University Hospital ethics committee (1150/2016) and respective committee of Helsinki City (2016-014058).





