Gastrointestinal microbiota
The gastrointestinal (GI) microbiota is a complex and metabolically active ecosystem that plays an important role in health and disease. The microbiota varies in number, diversity, composition and activity depending on the region of the GI tract. The stomach, with its strongly acidic environment and fast transit, harbours relatively small numbers of bacteria (approximately 103/ml), whereas the mildly acidic environment and slower transit in the colon allow for much larger numbers (approximately 1012/g) and greater diversity( Reference Sekirov, Russell and Antunes 1 ).
Historically, our understanding of the composition of the GI microbiota was based upon analytical approaches that relied on the phenotypic characteristics of different strains, such as their ability to grow on selective media or to ferment specific carbohydrates. These techniques are limited as up to 80% of the GI microbiota and have previously not been identified using culturing methods( Reference Eckburg, Bik and Bernstein 2 ). Our understanding of the GI microbiota has rapidly expanded due to the development of genotypic analysis that can accurately characterise its composition. Initially, these techniques utilised oligonucleotide probes (e.g. fluorescent in situ hybridisation) or primers (e.g. quantitative PCR). However, these required the target organisms to be known, isolated and sequenced and for specific probes and primers to be developed and validated. Recently, approaches to sequencing the microbiota have been developed that overcome these problems, allowing the whole GI microbiome to be identified and characterised( Reference Qin, Li and Raes 3 ).
One of the biggest advances thus far has been the comprehensive metagenomic sequencing of the GI microbiota by the MetaHIT Consortium (Metagenomics of the Human Intestinal Tract, http://www.metahit.eu/) ( Reference Qin, Li and Raes 3 ). In a study of 124 individuals, the results demonstrated that any of 1000–1150 different bacterial species could populate the human GI tract, with each individual harbouring approximately 160 different species. Given these large numbers there is great potential for inter-individual diversity in microbiota composition. Despite this, considerable stability was found between individuals for certain species. For example, a core eighteen species were found in all subjects, fifty-seven were found in 90% and seventy-five species were found in 50%( Reference Qin, Li and Raes 3 ).
In a further analysis of the microbiota from across four countries (including those from MetaHIT and the Human Microbiome Project) it was found that bacteria cluster within individuals( Reference Arumugam, Raes and Pelletier 4 ). The GI microbiota sequences were shown to fit into three distinct clusters termed ‘enterotypes’, characterised by the predominance of Bacteroides (enterotype 1), Prevotella (enterotype 2) and Ruminococcus (enterotype 3). The abundance of these main contributors correlated positively or negatively with other genera. For example, human subjects with enterotype 1 had high levels of Bacteroides, the numbers of which were positively correlated with Parabacteroides and Clostridiales but negatively correlated with Lactobacillus( Reference Arumugam, Raes and Pelletier 4 ), indicating a propensity for these to co-exist or avoid other species, respectively. Taken together, these findings describe a microbial ecosystem whose structure is determined, at least in part, by the abundance of species that together contribute to a limited number of preferred compositions. The association between enterotype, optimal health and disease risk is yet to be fully examined.
The composition of the GI microbiota is influenced by a range of factors including ageing and diet. The microbiota in older people has been shown to be considerably different in terms of diversity and abundance when compared with younger adults, with a recent large study showing older people had higher Bacteroides and Clostridia cluster IV (including Faecalibacterium prausnitzii)( Reference Claesson, Cusack and O'Sullivan 5 ). The impact of diet on the GI microbiota in healthy people has been recognised for well over a century, following the description of differences in bifidobacteria between breastfed and formula-fed infants( Reference Tissier 6 ). However, only recently has the impact on the GI microbiota of nutrients and food components been explored in depth. Habitual long-term diet has recently been shown to strongly associate with enterotype, in particular an association between protein/animal fat and Bacteroides (enterotype 1) and between carbohydrate and Prevotella (enterotype 2)( Reference Wu, Chen and Hoffmann 7 ). In terms of dietary alterations, acute feeding studies have identified that altering fat and non-starch polysaccharide intakes has a considerable impact on the microbiota, although they do not result in switching between enterotypes, indicating considerable stability of the latter following dietary change( Reference Wu, Chen and Hoffmann 7 ). Studies in gnotobiotic mice undergoing manipulation of dietary protein, fat and carbohydrate intake have found that dietary changes account for a majority of the alterations occurring in the microbiota( Reference Faith, McNulty and Rey 8 ). Extensive research has demonstrated a role for specific dietary carbohydrates in modifying the microbiota, first described as the prebiotic concept in 1995( Reference Gibson and Roberfroid 9 ).
Prebiotic carbohydrates
Prebiotics are non-digestible, fermentable food components that result in ‘the selective stimulation of growth and/or activity of one or a limited number of microbial genera/species in the gut microbiota that confer health benefits to the host’( Reference Roberfroid, Gibson and Hoyles 10 ). The most commonly used prebiotics are inulin-type fructans such as inulin, oligofructose, fructo-oligosaccharides and galacto-oligosaccharides (GOS) such as stachyose and raffinose.
The essential characteristics of a prebiotic are their resistance to digestion, fermentability and selectivity in promoting the growth or activity of beneficial bacteria( Reference Roberfroid, Gibson and Hoyles 10 ). Resistance to small- intestinal digestion is the result of human subjects lacking enzymes that hydrolyse the polymer bonds. This allows the prebiotic to reach the colon intact and undergo fermentation, but only by a limited number of genera/species. For example, some bacteria have ‘fructan utilisation locus’ genes that enable them to acquire and ferment inulin-type fructans( Reference Sonnenburg, Zheng and Joglekar 11 ). Recent murine feeding studies have shown that the in vivo functionality of the ‘fructan utilisation locus’ was strongly predictive of the ability of a strain to grow when animals were fed these prebiotics( Reference Sonnenburg, Zheng and Joglekar 11 ). Proliferation of specific genera/species is thought to be driven by competitive selection resulting from the ability of these to access the carbon source of prebiotics.
Many prebiotic carbohydrates are present in the normal diet. For example, inulin-type fructans are found in relatively large amounts in chicory root (35·7–47·6 g/100 g), Jerusalem artichoke (16–20 g/100 g) and garlic (9–16 g/100 g), but they are also present in smaller amounts in cereals such as wheat (1–4 g/100 g)( Reference Van Loo, Coussement and de Leenheer 12 ). However, as wheat is a staple in many western countries, dietary surveys show that it is the major contributor to fructan intake in the United Kingdom (66%)( Reference Dunn, Datta and Kallis 13 ) and the United States (69%)( Reference Moshfegh, Friday and Goldman 14 ). Bread contains only a small amount of fructan (0·61–1·94 g/100 g depending upon the recipe and cereal source)( Reference Whelan, Abrahmsohn and David 15 ), but as the most widely consumed food item in the United Kingdom( Reference Henderson, Gregory and Swan 16 ) it makes a large contribution to inulin intake( Reference Dunn, Datta and Kallis 13 ). Meanwhile, GOS such as stachyose and raffinose are widely contained and consumed within pulses( Reference Biesiekierski, Rosella and Rose 17 ).
In the first key human study to demonstrate the prebiotic effect, eight healthy volunteers consuming a controlled diet were supplemented with 15 g/d oligofructose or inulin, both of which resulted in almost a 1 log10 increase in luminal bifidobacteria, which then returned to baseline following withdrawal of the prebiotic( Reference Gibson, Beatty and Wang 18 ). The prebiotic properties of such supplements have been confirmed in a series of animal and human studies, and have been extensively reviewed elsewhere( Reference Roberfroid, Gibson and Hoyles 10 ). Subsequent research has shown a dose-dependent effect on luminal bifidobacteria of dietary supplementation with oligofructose( Reference Bouhnik, Vahedi and Achour 19 ) and GOS( Reference Davis, Martínez and Walter 20 ). However, interestingly, the effect of prebiotics naturally occurring in foods has received little attention in the literature, and as yet the inulin and oligofructose content of habitual diet has not been shown to correlate with bifidobacteria in healthy people( Reference Whelan, Bartlett and Datta 21 ).
An in-depth review has recently been published regarding the physiological effects of prebiotics on GI function, immune function and mineral absorption and their role in the management of paediatric and obesity-related disorders( Reference Roberfroid, Gibson and Hoyles 10 ). However, relatively few studies have addressed the role of prebiotics in digestive disorders( Reference Whelan 22 ), including in patients receiving enteral nutrition (EN) and patients with Crohn's disease and irritable bowel syndrome (IBS).
Enteral nutrition
EN is a common method of artificial nutritional support for patients who are unable to achieve their nutritional requirements through oral diet. Alterations in stool output can occur which result in the diagnosis of diarrhoea, which has a reported prevalence ranging from 2 to 95% of patients. The wide range is the result of differences in the patient groups and the definition of diarrhoea used. There are at least thirty-three different definitions of diarrhoea used in the literature regarding EN( Reference Lebak, Bliss and Savik 23 ). Meanwhile, in clinical practice, doctors, dietitians, nurses and patients vary in the importance they assign to different stool characteristics when defining diarrhoea during EN( Reference Whelan, Judd and Taylor 24 , Reference Majid, Emery and Whelan 25 ), highlighting the importance of standardised, valid and reliable approaches to recording and defining it( Reference Whelan, Judd and Taylor 26 , Reference Whelan, Judd and Preedy 27 ).
Diarrhoea can be a problematic complication of EN, leading to dehydration and a requirement for intravenous fluid support. Despite this, it is not uncommon for some health professionals to reduce or cease EN during episodes of diarrhoea( Reference Majid, Emery and Whelan 25 ), a practice that might in part explain the association between high stool output and poorer delivery of enteral formula( Reference Whelan, Hill and Preedy 28 ). Diarrhoea also increases the risk of faecal incontinence, which patients rate as the most unpleasant aspect of diarrhoea( Reference Majid, Emery and Whelan 25 ), and which of course can contribute to infection of surgical or pressure wounds.
A number of factors implicate a role for the GI microbiota in pathogenesis of diarrhoea during EN, including antibiotic prescription, enteropathogenic colonisation and abnormal colonic responses( Reference Whelan, Judd and Preedy 29 ). The prevalence of diarrhoea during EN is higher in patients prescribed antibiotics( Reference Guenter, Settle and Perlmutter 30 ) which is thought to relate to their effect on the GI microbiota and on the SCFA produced during fermentation( Reference Sullivan, Edlund and Nord 31 ). Clostridium difficile colonisation can occur during EN, with one case–control study demonstrating a 9-fold greater risk of C. difficile-associated diarrhoea in patients receiving EN( Reference Bliss, Johnson and Savik 32 ). During intra-gastric infusion of enteral formula, water is actively secreted into the ascending colon, which might contribute to the pathogenesis of diarrhoea, but this fluid secretion is prevented by caecal infusion of SCFA( Reference Bowling, Raimundo and Grimble 33 ).
Given their potential role in the pathogenesis of diarrhoea during EN, studies have investigated the composition of the GI microbiota in such patients. In a cohort study of twenty patients receiving standard (fibre-free) enteral formula, there was marked instability of the luminal microbiota and those who developed diarrhoea had higher clostridia and lower bifidobacteria( Reference Whelan, Judd and Tuohy 34 ). The origin of these alterations is unclear. Consumption of standard, fibre-free enteral formula by healthy subjects has been shown to result in reduction in total bacteria( Reference Whelan, Judd and Preedy 35 ) and in Faecalibacterium prausnitzii ( Reference Benus, van der Werf and Welling 36 ), a major producer of the SCFA butyrate that stimulates colonic water absorption.
Fortifying enteral formulas with prebiotics and fibres has been proposed as a method to increase bifidobacteria to assist in colonisation resistance and to increase SCFA production to stimulate colonic water absorption( Reference Whelan, Gibson and Judd 37 , Reference Whelan 38 ). Indeed, a number of studies have demonstrated that enteral formulas fortified with fibre and prebiotics increase luminal bifidobacteria and SCFA when consumed by healthy people( Reference Whelan, Judd and Preedy 35 , Reference Whelan 38 ). In addition, other benefits such as appetite suppression, which may be important in patients receiving exclusive EN, have also been demonstrated( Reference Whelan, Efthymiou and Judd 39 ).
Despite these promising effects in healthy subjects, application in the clinical setting has yielded disappointing results. Although trials have been limited in design and sample size, some show little impact on bifidobacteria( Reference Schneider, Girard-Pipau and Anty 40 , Reference Majid, Emery and Whelan 41 ) or SCFA concentrations( Reference Sobotka, Brátova and Slemrová 42 ) (Table 1). Two clinical trials in patients receiving long-term EN in the community showed either no impact( Reference Schneider, Girard-Pipau and Anty 40 ) or a trend towards an increase( Reference Wierdsma, van Bodegraven and Uitdehaag 43 ) in bifidobacteria during feeding with formulae supplemented with fibre and prebiotics. Meanwhile, in hospitalised patients, a non-randomised trial found no differences in bifidobacteria between those receiving a standard formula or one supplemented with a mix of fibre, inulin and oligofructose( Reference Majid, Emery and Whelan 41 ). More recently, the results of a randomised controlled trial indicated that compared with normal levels of fibre and prebiotics, additional inulin/oligofructose had no impact on bifidobacteria and actually lowered F. prausnitzii in patients receiving EN on the intensive care unit( Reference Majid, Cole and Sherry 44 ) (Table 1).
Table 1. Clinical trials of prebiotic supplementation in patients receiving enteral nutrition

EN, enteral nutrition; ICU, intensive care unit.
Given the disappointing results for use of prebiotics in patients receiving EN, a contrasting approach is the use of probiotics, some strains of which are efficacious in the prevention of C. difficile-associated diarrhoea( Reference Hickson, D'Souza and Muthu 45 , Reference Parkes, Sanderson and Whelan 46 ). At least six randomised controlled trials of probiotics in prevention or treatment of diarrhoea in EN have been undertaken( Reference Whelan and Schneider 47 ), but only two have shown a beneficial effect in preventing diarrhoea, for Saccharomyces boulardii ( Reference Bleichner, Blehaut and Mentec 48 ) and VSL#3( Reference Frohmader, Chaboyer and Robertson 49 ) both in the intensive care setting. Some researchers and clinicians have raised concerns about the safety of probiotics in such patient groups. However, despite a systematic review identifying case reports of adverse events in thirty-two patients receiving EN and probiotics, the vast majority of trials showed either no effect, or a positive effect, on outcomes related to safety (e.g. mortality and infections)( Reference Whelan and Myers 50 ).
Crohn's disease
Crohn's disease is a chronic relapsing and remitting inflammatory bowel disease characterised by discontinuous transmural inflammation, ulceration and stricturing anywhere in the GI tract. In Europe, the incidence ranges from 0·7 to 9·8 cases per 100 000 person-years( Reference Loftus 51 ). Symptoms include diarrhoea, faecal urgency, severe abdominal pain and rectal bleeding and complications such as fistula may occur. These symptoms can have a profound impact, with evidence of impairments in nutritional status( Reference Gerasimidis, McGrogan and Edwards 52 ), body weight, social functioning( Reference Prince, Whelan and Moosa 53 ) and quality of life( Reference Irvine 54 ).
The primary treatment approach in Crohn's disease is usually drug therapy, including steroids (e.g. prednisolone), immunosuppressants (e.g. azathioprine) and biological drugs such as monoclonal antibodies (e.g. infliximab)( Reference Dignass, Van Assche and Lindsay 55 ). Nutritional approaches to treat Crohn's disease are available, the most notable being exclusive EN, which in clinical trials induces remission in 60–85% of patients( Reference Zachos, Tondeur and Griffiths 56 ). However, there are some drawbacks. Studies show that EN is less effective a treatment for Crohn's disease than steroids( Reference Zachos, Tondeur and Griffiths 56 ), while in clinical practice, palatability and poor compliance can be problematic( Reference Lomer, Gourgey and Whelan 57 ) and as a result it is mostly commonly used as a steroid-sparing treatment in children. There is considerable evidence that the GI microbiota are directly involved in the pathogenesis of Crohn's disease, and therefore nutritional treatments such as prebiotics which might be a safe and effective treatment strategy, are an attractive option.
Crohn's disease results from a heightened mucosal immune response to the GI microbiota in genetically susceptible individuals. Broadly speaking, this results from alterations in the balance of pro-inflammatory (e.g. IL-1, IL-6, IL-12 and interferon-γ) and immuno-regulatory (e.g. IL-10, IL-4 and transforming growth factor-β) cytokines released by activated T helper1, T helper17 or regulatory lymphocytes. There is convincing evidence that this inflammatory cascade is driven by the GI microbiota. For example, animal models of inflammatory bowel disease reared in germ-free conditions do not develop GI inflammation until they are transferred to non-sterile conditions or until they are artificially colonised with bacteria( Reference Sellon, Tonkonogy and Schultz 58 ). Similar observations have been described in human subjects, where surgical diversion of the faecal stream away from the site of inflammation results in disease remission in the majority of patients( Reference Fasoli, Kettlewell and Mortensen 59 ). More recently, the identification of Crohn's disease susceptibility loci/genes also implicate the GI microbiota in its pathogenesis. For example, mutations in the caspase activating recruitment domain 15 gene, which is involved in bacterial recognition, increase the risk of developing Crohn's disease 38-fold( Reference Hugot, Chamaillard and Zouali 60 ), while mutations in genes responsible for the processing of intracellular bacteria through autophagy have also been implicated( Reference Lees, Barrett and Parkes 61 ).
Numerous studies have demonstrated alterations in many genera/species of the GI microbiota in Crohn's disease compared with healthy controls. This ‘dysbiosis’ has been linked with some aspects of disease behaviour, including the presence of ileal disease( Reference Willing, Dicksved and Halfvarson 62 ) and fistulating disease( Reference Tozer, Whelan and Phillips 63 ). Meanwhile, in a study of over 100 patients, smoking, an environmental risk factor for developing Crohn's disease and for the severity of disease course, was associated with higher bacteroides( Reference Benjamin, Hedin and Koutsoumpas 64 ). Clinically relevant aspects of the ‘dysbiosis’ include lower luminal bifidobacteria( Reference Seksik, Rigottier-Gois and Gramet 65 , Reference Sokol, Seksik and Furet 66 ), where some species have been shown to stimulate dendritic cell IL-10 production in vitro ( Reference Hart, Lammers and Brigidi 67 ), where greater numbers are associated with higher mucosal IL-10+ dendritic cells in patients with Crohn's disease( Reference Ng, Benjamin and McCarthy 68 ), indicating that dendritic cell function might be influenced by composition of the commensal microbiota. Furthermore, lower concentrations of F. prausnitzii have also been reported in Crohn's disease which is relevant as higher numbers of this species are associated with longer post-operative disease maintenance, thought to be due to its immuno-regulatory capacity in reducing IL-12 and interferon-γ and stimulating IL-10 secretion( Reference Sokol, Pigneur and Watterlot 69 ).
Prebiotics have been shown to stimulate faecal and mucosal bifidobacteria( Reference Roberfroid, Gibson and Hoyles 10 ) and F. prausnitzii ( Reference Ramirez-Farias, Slezak and Fuller 70 ) in healthy people, while acetate and propionate increase immuno-regulatory IL-10 production( Reference Cavaglieri, Nishiyama and Fernandes 71 ). Consequently, prebiotics have been investigated as a potential therapeutic target for Crohn's disease( Reference Hedin, Whelan and Lindsay 72 ). Many animal studies have demonstrated the effectiveness of prebiotics in preventing and treating models of inflammatory bowel disease, although these results often differ depending upon the compound used (e.g. inulin and fructo-oligosaccharide)( Reference Koleva, Valcheva and Sun 73 ). In human subjects, a number of studies have investigated the combined use of probiotic and prebiotic combinations( Reference Hedin, Whelan and Lindsay 72 ), but few have investigated the effect of prebiotics alone (Table 2).
Table 2. Clinical trials of prebiotic supplementation in patients with Crohn's disease

TLR-2, Toll-like receptor-2.
The first was a pilot study of just ten patients with active Crohn's disease consuming 15 g/d oligofructose/inulin that appeared to improve disease activity alongside increasing luminal bifidobacteria and stimulating IL-10+ dendritic cells and Toll-like receptor-2 expression( Reference Lindsay, Whelan and Stagg 74 ). Since these promising, but preliminary findings, two large randomised controlled trials have been published( Reference Benjamin, Hedin and Koutsoumpas 75 , Reference Joossens, De Preter and Ballet 76 ). Neither demonstrated an impact of oligofructose/inulin at doses of 15 g/d( Reference Benjamin, Hedin and Koutsoumpas 75 ) or 20 g/d( Reference Joossens, De Preter and Ballet 76 ) on Crohn's disease activity; indeed both studies showed greater withdrawal in the prebiotic groups. Furthermore, neither of them resulted in higher bifidobacteria or F. prausnitzii in the prebiotic groups compared with placebo. Interestingly, one study showed that those patients who did experience an increase in bifidobacteria during prebiotic consumption had less severe disease, as evidenced by lower Crohn's disease activity index and lower faecal calprotectin( Reference Benjamin, Hedin and Koutsoumpas 75 ). This perhaps suggests that the prebiotic effect may be most pronounced at lower levels of inflammation, highlighting a need for studies investigating the role of prebiotics in disease maintenance. Preliminary studies are also underway to investigate the role of prebiotics in the prevention of Crohn's disease in those at elevated genetic risk( Reference Hedin, Stagg and Whelan 77 ).
Given the lack of success of prebiotics in treating active Crohn's disease, alternative approaches to successfully modifying the microbiota have been investigated. Few patients with Crohn's disease (<5%) have ever used prebiotics to manage their disease, whereas many (>40%) have trialled probiotics( Reference Hedin, Mullard and Sharratt 78 ). A small number of clinical trials of probiotics have been undertaken, but a recent meta-analysis has shown no effects for the use of Lactobacillus rhamnosus GG or L. johnsonii for preventing endoscopic recurrence in inactive Crohn's disease( Reference Jonkers, Penders and Masclee 79 ). There is increasing interest in the use of faecal microbiota transplantation, which has been undertaken by a small number of institutions for many years, despite little robust research evidence. A recent systematic review failed to identify any controlled trials of faecal microbiota transplantation in Crohn's disease( Reference Anderson, Edney and Whelan 80 ). However, case series/case reports of at least six patients receiving faecal microbiota transplantation for the management of Crohn's disease were identified in which the majority experienced considerable disease response (although outcome data for Crohn's disease and ulcerative colitis were combined)( Reference Anderson, Edney and Whelan 80 ). Controlled trials of faecal microbiota transplantation in management of active Crohn's disease are warranted.
Irritable bowel syndrome
IBS is a functional GI disorder characterised by abdominal pain and altered stool output in the absence of an organic cause. It is defined using the Rome III criteria as recurrent abdominal pain or discomfort at least three days per month in the last three months associated with at least two of the following (a) improvement with defecation; (b) onset associated with a change in frequency of stool; or (c) onset associated with a change in stool form. With a prevalence of 10–20% in developed countries, IBS is a problematic disorder resulting in impaired quality of life and high healthcare utilisation( Reference Agarwal and Spiegel 81 ).
The pathogenesis of IBS is complex and multifactorial and includes physiological, emotional, cognitive and behavioural pathways, a number of which implicate a role for the GI microbiota( Reference Parkes, Brostoff and Whelan 82 ). Firstly, numerous studies report an increased risk of IBS following gastroenteritis, demonstrated in particular by data from the Walkerton Health Study, which monitored the clinical sequelae of an outbreak of acute gastroenteritis (Escherichia coli and Campylobacter jejuni) following municipal water contamination in Walkerton, Ontario, Canada. This cohort study has shown that acute gastroenteritis resulted in an increased odds of developing IBS at both 2 years (OR 4·8)( Reference Marshall, Thabane and Garg 83 ) and 8 years (OR 3·1)( Reference Marshall, Thabane and Garg 84 ). Secondly, alterations in the GI microbiota have also been reported in patients with IBS. Patients with diarrhoea-predominant IBS have been shown to have lower bifidobacteria( Reference Kassinen, Krogius-Kurikka and Mäkivuokko 85 ), the genera frequently responsive to prebiotic supplementation. Despite the traditional view of IBS as a luminal disorder, more studies are now investigating the mucosal microbiota, with a recent case–control study also reporting lower bifidobacteria in the GI mucosa of patients with diarrhoea-predominant IBS compared with controls( Reference Parkes, Rayment and Hudspith 86 ). Interestingly, a negative correlation between the frequency of pain or discomfort and the numbers of mucosal bifidobacteria was also reported( Reference Parkes, Rayment and Hudspith 86 ). Metagenomic sequencing to determine whether distinct microbial enterotypes are associated with IBS is yet to be undertaken. However, as with all observational studies of the human GI microbiota, identifying whether dysbiosis is a primary event that drives the development of disease or is merely a secondary effect of the disease is difficult to determine. Thirdly, there is evidence of elevated luminal gas production in IBS, with a recent meta-analysis reporting a greater than fourfold odds of an abnormal breath test in patients with IBS compared with controls (OR 4·46)( Reference Shah, Basseri and Chong 87 ).
The potential role of the GI microbiota in pathogenesis of IBS, and in particular the relative lower numbers of bifidobacteria in diarrhoea-predominant IBS, has led to a small number of studies investigating prebiotics in its management( Reference Whelan 88 ). The four major studies have used a variety of prebiotics (oligofructose, fructo-oligosaccharide and GOS), in varying doses (3·5–20 g/d) and for varying durations (4–12 weeks)( Reference Hunter, Tuffnell and Lee 89 – Reference Silk, Davis and Vulevic 92 )(Table 3). Two trials, one using oligofructose (6 g/d)( Reference Hunter, Tuffnell and Lee 89 ) and one using fructo-oligosaccharide (20 g/d)( Reference Olesen and Gudmand-Hoyer 90 )found no significant impact on symptoms at the study endpoints, although in the latter high dose study, prebiotics actually worsened symptoms at the study mid-point( Reference Olesen and Gudmand-Hoyer 90 ). Two studies have demonstrated symptom improvement, with fructo-oligosaccharide (5 g/d) lowering composite symptom score( Reference Paineau, Payen and Panserieu 91 ) and trans-GOS (3·5 g/d) lowering flatulence and bloating and improving global symptom relief( Reference Silk, Davis and Vulevic 92 ). However, in the latter study patients randomised to a higher dose of trans-GOS (7 g/d) reported higher composite symptom scores( Reference Silk, Davis and Vulevic 92 ) (Table 3).
Table 3. Clinical trials of prebiotic supplementation in patients with IBS
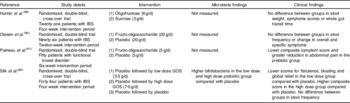
IBS, irritable bowel syndrome; GOS, galacto-oligosaccharides.
These data would suggest that both the type and dose of prebiotic is important in determining any clinical benefit in IBS, with some evidence that higher doses may have a negative impact on symptoms. High doses of fermentable carbohydrates can stimulate colonic gas production, which might increase flatulence and which in the context of visceral hypersensitivity might also induce abdominal discomfort and pain. In a recent study, a diet high in fermentable carbohydrates was shown to increase breath hydrogen in both fifteen patients with IBS and fifteen healthy controls( Reference Ong, Mitchell and Barrett 93 ). This was associated with an increase in abdominal pain, bloating and flatulence in patients with IBS, but only in flatulence in the healthy controls( Reference Ong, Mitchell and Barrett 93 ). A study in ileostomists has shown that diets high in fermentable carbohydrates can increase water delivery into the ileum, thus potentially contributing to the generation of diarrhoea( Reference Barrett, Gearry and Muir 94 ).
Indeed, recent research has actually focused on restricting fermentable carbohydrates (fermentable oligo-, di, mono-saccharides and polyols) in IBS. There is now evidence for the use of the so-called ‘Low FODMAP diet’ from both non-randomised( Reference Staudacher, Whelan and Irving 95 ) and randomised trials( Reference Staudacher, Lomer and Anderson 96 ). In the latter study of forty-one patients with IBS, those following a fermentable carbohydrate restricted diet were more likely to report adequate control of symptoms compared with controls (68% v. 23%; P = 0·005). However, this diet also reduced luminal bifidobacteria, which is hypothesised to be the result of restricting dietary prebiotic intake( Reference Staudacher, Lomer and Anderson 96 ).
In contrast with both prebiotics and the low FODMAP diet, there are many clinical trials investigating the use of probiotics in the management of IBS. A recent Rome Foundation group report identified thirty-two randomised controlled trials of probiotics in IBS( Reference Simren, Barbara and Flint 97 ). At least six systematic reviews have been published on probiotics in IBS, and these have been summarised elsewhere( Reference Whelan 88 ). Most of the meta-analyses indicate a beneficial impact of probiotics on global symptoms, abdominal pain and flatulence, whereas the impact on bloating is equivocal. Based upon the evidence described here, recent guidelines have recommended the use of specific strains of probiotics, and the use of the low FODMAP diet in the management of IBS( Reference McKenzie, Alder and Anderson 98 ). The use of prebiotics in IBS should therefore be restricted to only those compounds and doses for which there is supporting evidence.
Conclusion
The interaction between dietary intake and the microbiota in healthy people has been recognised for many years. However, evidence of the interaction between prebiotics, the GI microbiota and digestive disorders is now emerging, in part due to the development of more robust approaches to examine dietary intake, complex microbial ecosystems and disease outcomes. Unlike healthy human subjects, patients experience a number of issues that may alter their microbiota (disease, antibiotics and inflammation) and the use of microbiota modifying therapies, such as prebiotics, may not elicit the same effects in patients as they do in healthy people. The interaction between dietary intake, the microbiota and GI disease is emerging as an exciting area requiring research and application through multidisciplinary collaboration between experts in dietetics, microbiology and gastroenterology.
Acknowledgements
Many expert researchers and clinicians contributed to the research reviewed in this manuscript, whose collaboration is gratefully acknowledged. Particular thanks go to Professor Pat Judd (University of Central Lancashire), Dr Moira Taylor (University of Nottingham), Professor Victor Preedy, Professor Peter Emery, Dr Charlotte Hedin, Dr Gareth Parkes, Dr Jane Benjamin (King's College London), Dr Hazreen Abdul Majid (University of Malaya), Dr James Lindsay (Barts Health NHS Trust), Dr Andrew Stagg (Queen Mary, University of London), Professor Alastair Forbes (University College London), Dr Ailsa Hart (St Marks Hospital), Dr Jeremy Sanderson, Dr Miranda Lomer, Heidi Staudacher and Dr Peter Irving (Guy's and St Thomas' NHS Foundation Trust and King's College London).
K. W. has previously or currently received research funding, speaker's honoraria or consulting fees from a range of research and charitable bodies, including the Broad Medical Research Program, British Dietetic Association, Core, Crohn's and Colitis UK, Healthcare Quality Improvement Partnership and National Institute of Health Research, as well as industry bodies including the Californian Dried Prune Board, Danone, Dr Schar, Nestle, Nutricia, Novartis and Yakult. None of these funding bodies contributed to the writing of this manuscript.





