Ectopic atrial tachycardia is an uncommon cause of supraventricular tachycardia in children, which occurs because of an abnormal, nonsinus, atrial focus with enhanced automaticity. Reference Gillette1 The crista terminalis, atrial appendages, and pulmonary veins are the most common anatomical locations. Reference Koike, Hesslein, Finlay, Williams, Izukawa and Freedom2
Ectopic atrial tachycardia is managed successfully in most children with antiarrhythmic medications. Catheter ablation is an effective alternative therapy in the case of resistance to medical therapy and/or left ventricular dysfunction, but with a high risk of morbidity and mortality especially in infants.
Ivabradine selectively inhibits If (funny) channels in a concentration-dependent manner reducing heart rate, without affecting cardiac inotropy or systemic vascular resistance. Ivabradine is indicated for heart failure with reduced ejection fraction by the most recent Heart Failure Guidelines in adults. Reference January, Wann and Calkins3 In addition, there are reports of the efficacy of ivabradine in controlling ectopic atrial tachycardia in adult patients and older children and adolescents. Reference Banavalikar, Shenthar and Padmanabhan4 However, there are insufficient data on its use in younger children. Recently, ivabradine has been successfully used as an adjunctive therapy in infants with junctional ectopic tachycardia and ectopic atrial tachycardia, resistant to a number of drugs. Reference Dieks, Klehs, Müller, Paul and Krause5,Reference Ergul, Ozturk, Ozgur, Ozyurt, Cilsal and Guzeltas6
Case presentation
A seven-month-old male infant was admitted to a paediatric cardiology clinic due to weakness and loss of appetite. Upper respiratory tract infection and supraventricular tachycardia were diagnosed. A narrow QRS long RP tachycardia (ectopic atrial tachycardia) with a fast ventricular rate of 220–230 bpm was detected on electrocardiogram, and the patient was hospitalised for multidrug therapy with propranolol, amiodoron, and flecainide. He was discharged when his heart rhythm was restored to the sinus. Thanafter, he was followed up for about 3 months without any problem. When he was admitted again with an ectopic atrial tachycardia of 240 bpm heart rate, he was hospitalised and the therapy was changed to sotalol, flecainid, and digoxin. But the tachycardia could not be controlled, so he was transferred to our centre for catheter ablation.
The patient was 11 months old and weighing 10 kg when admitted to our centre. Physical examination was normal except for tachycardia. Echocardiography showed normal anatomy and left ventricular functions. Laboratory studies including blood count, inflammatory biomarkers, and cardiac troponin were normal. The 12-lead electrocardiogram showed a regular narrow QRS tachycardia with a rapid ventricular rate of 260 bpm and a long RP interval (Fig 1a). The tachycardia had a wide range of rate between 190 and 290 bpm in reponse to patients crying and agitations, and during the relative slow phases, the p morphology was similar to sinus p wave. The tachycardia was stopped with an QRS complex when 0.2 mg İV adenosin was given as rapid bolus, and sinuse rhythm with 168 bpm was restored for a short time (Fig 1b). Later on the tachycardia started rapidly with a heart rate up to 260 bpm. All these characteristics together ruled out diagnosis of sinus tachycardia, inappropriate sinus tachycardia, permanent junctional tachycardia, and the other reentrant short RP tachycardias. A microreentrant focal atrial tachycardia responsive to adenosine was considered.
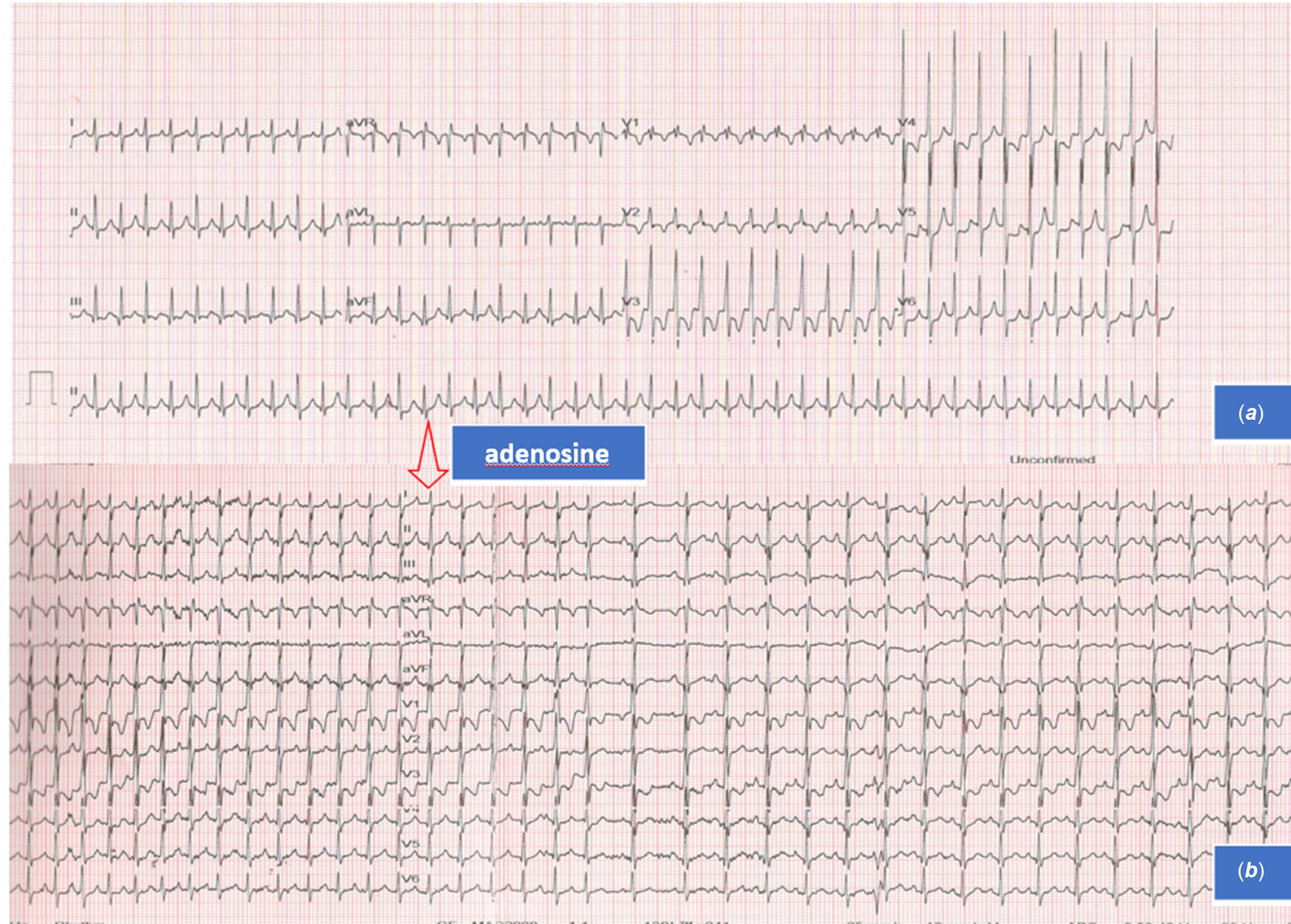
Fig. 1 a) The 12-lead ECG at admission showing narrow QRS long RP tachycardia at a heart rate of 260 bpm. b) Response of the tacycardia to a rapid IV bolus of 0,2 mg adenozin, showing termination of the tacycardia ending with QRS, and starting again in a short time.
In the first day of hospitalisation, the medications he was taking were continued as sotalol (95 mg/m2), flekainide (120 mg/m2), and digoxin in maintenance dose, and a 24-hour ambulatory ECG (Holter) was obtained, revealing incessant long RP tachycardia with heart rates of maximal: 292 minimal: 189 and mean: 230 bpm. Before an electrophysiologic study and ablation attempt, we decided to to see ivabradin response of the tachycardia and we stopped all the other medications. After a single dose of ivabradin (0.15 mg/kg/day), heart rhythm was restored to sinus 2 hours later (Fig 2a). Ivabradin was continued as 0.2 mg/kg/day in two doses, and catheter ablation was abandoned. The control holter before discharge revealed normal sinus ryhthm with a regular diurnal pattern and normal rate limits (Fig 2b) and normal 12-lead ECG (Fig 2c). No side effects attributable to ivabradine were recorded during follow-up.

Fig. 2 a) Heart rate trend in the second ambulatory ECG of the patient, after the antiarrhythmic therapy with sotalol, flecainid and digoxin was stopped and ivabradin was given, showing an gradual decrease in heart rate after 2 hours of administration. b) Heart rate trend in the last ambulatory ECG of the patient before discharge, showing normal heart rate variability and limits according to age. c) Normal sinus ryhthm on 12-lead ECG before discharge.
Discussion and conclusion
Ectopic atrial tachycardia is an uncommon cause of supraventricular tachycardia in children. Reference Gillette1,Reference Koike, Hesslein, Finlay, Williams, Izukawa and Freedom2 Incessant ectopic atrial tachycardia can lead to tachycardia-induced cardiomyopathy. Reference Kang, Etheridge and Kantoch7 The cause is usually idiopathic but identified risk factors include viral infections, atrial tumours, and surgery for congenital heart disease.
Studies shows that 74% of children with FAT diagnosed in the first year of life achieve spontaneous resolution, suggesting that these children, in particular, may benefit from an initial trial of medical therapy. Reference Kang, Etheridge and Kantoch7 Vagal manoeuvers, adenosine, and DC cardioversion are ineffective. Betablockers and class Ic antiarrhythmic drugs are most commonly used for the management of ectopic atrial tachycardia. Betablockers used as first-line treatment alone or in combination with other medications, including amiodarone, digoxin, flecainide, and sotalol. However, the use of ivabradine has recently been reported in multidrug-resistant cases and sometimes as first-line therapy. Reference Kang, Etheridge and Kantoch7
Holger M. et al. reported the successful use of ivabradine (0.05 mg/kg/day) in combination with a betablocker (esmolol and metoprolol) for the therapy of ectopic atrial tachycardia in an 1-year-old girl. Amiodoron was used as the initial treatment for the patient. Reference Michel, Heißenhuber, Wellmann, Melter and Gerling8
Balaganesh K. et al. reported two cases of tachycardia-induced cardiomyopathy secondary to incessant ectopic atrial tachycardia in an infant presenting with severe left ventricular dysfunction and haemodynamic instability. They reported that after the initiation of enteral ivabradine (0.15 mg/kg), sinus rhythm was restored within 12 hours in the first case and within 4 hours in the second case and that left ventricular functions improved in the follow-up. Reference Karmegaraj, Balaji and Raju9
Janson et al reported that an 11-year-old, previously healthy ectopic atrial tachycardia patient was restored to sinus rhythm in 90 minutes with a single dose of ivabradine (0.05 mg/kg/day). Esmolol was used as the initial treatment for the patient. Reference Janson, Tan, Iyer, Vogel, Vetter and Shah10
In infants, the risk of complications due to catheter ablation is higher due to low body weight. Since spontaneous resolution of tachycardia is more likely in this age group, it is wiser to initially opt for medical treatment. Therefore, we think that ivabradine can be used successfully in the treatment of ectopic atrial tachycardia as an alternative treatment before catheter ablation in this age group.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical standards
Informed consent from the parents of the case was obtained for publication.





