CLINICIAN’S CAPSULE
What is known about the topic?
Most ureteral stones pass spontaneously, but intervention is an option. No trials have compared conservative vs. interventional treatment.
What did this study ask?
We compared 60-day outcomes for ED patients with ureteral colic in Calgary and Vancouver.
What did this study find?
Index intervention rate was seven-fold higher in Calgary. Calgary patients had more subsequent ED revisits and hospitalizations. Adverse outcomes were associated with intervention for small stones and with non-intervention for large stones.
Why does this study matter to clinicians?
Conservative management of small stones and early intervention for large stones may improve system utilization and patient outcomes.
INTRODUCTION
Renal colic is a high prevalence disorder that affects 10% of the population.Reference Scales, Smith, Hanley and Saigal 1 It is a recurrent condition that causes extreme pain and has a significant impact on quality of life and health system utilization.Reference Bensalah, Tuncel and Gupta 2 - Reference Bryant, Angell and Tu 4 Guidelines suggest that many patients with an acute stone episode are appropriate for a trial of spontaneous passage that is successful in 60%–90% of cases,Reference Ordon, Andonian and Blew 5 - Reference Teichman 11 but some patients require intervention or hospitalization for control of severe symptoms; however, reported admission rates for acute stone episodes range from 2% to 13%.Reference Brown 12 - Reference Hyams, Korley, Pham and Matlaga 18 A 2005 US study estimated that acute stone events generated total costs of US$5.2 billion per year in the employed population alone, with 3.1 million lost workdays.Reference Saigal, Joyce and Timilsina 3
While the traditional approach is a trial of spontaneous passage, minimally invasive ureteroscopic techniques have made early intervention an option for some patients.Reference Pearle, Nadler and Bercowsky 19 Direct and indirect care costs may be higher with a surgical approach,Reference Saigal, Joyce and Timilsina 3 , Reference Hollingsworth, Norton and Kaufman 20 - Reference Rapoport, Perks and Teichman 22 but early intervention has the potential to terminate an episode of renal colic rapidly, decrease patient disability, and reduce the need for subsequent emergency department (ED) or hospital-based care. To date, no studies have compared the outcomes of patients treated medically v. surgically at their index ED visit for an acute stone, and high inter-institutional practice variability reflects this lack of evidence.
The Calgary Health Region and Vancouver Coastal Health Authority are comparable integrated health systems that have differing approaches to acute renal colic. Vancouver physicians typically prescribe a trial of spontaneous passage for acute stone events, and the Calgary practice favours early surgical intervention for most significant stones.Reference Innes, Lang, McRae and Grafstein 23 These fundamentally different approaches in comparable health systems provide the opportunity to study system-level outcomes associated with interventional v. conservative management. Our main objective was to compare event rates, defined as the need for hospitalization or surgical intervention within 60 days of the index renal colic visit, in these contrasting care systems.
METHODS
Design and setting
We used administrative data supplemented by a structured chart review to study all patients with an ED diagnosis of acute renal colic seen in two Canadian health regions during the calendar year, 2014. Calgary has four adult EDs, and Vancouver has five, serving 1.4 million and 1.1 million people, respectively. 24 , 25 The cities have similar population demographics, health infrastructure, and access to technology. Both have integrated care delivery systems with centralized leadership, regional program structures, operational processes, quality management, data capture, and information systems. Urologists and emergency physicians in both cities have equivalent training and licensing, as well as maintenance of competence requirements. One key difference is that, in Calgary, urological interventions are performed at a single site, which is also the urological referral and intervention centre for Southern Alberta. These regionally coordinated health systems allowed us to conduct a population-based study of all patients who attended an ED with acute renal colic and assured a low likelihood of missing important outcome events in the study cohorts. The study was approved by the University of British Columbia Clinical Research Ethics Board and the University of Calgary Conjoint Health Research Ethics Board in accordance with Canadian Tri-council guidelines and the Declaration of Helsinki.
Patients
We identified all patients who attended a Calgary or Vancouver ED during 2014 with an ED diagnosis of renal colic based on the following ICD-10 codesReference Saigal, Joyce and Timilsina 3 , Reference Fwu, Eggers, Kimmel, Kusek and Kirkali 26 : calculus of the kidney (N200), calculus of the ureter (N201), calculus of the kidney with calculus of the ureter (N202), hydronephrosis with renal and ureteral calculous obstruction (N132), unspecified renal colic (N23), and unspecified urinary calculus (N209). We focused on patients who had a well-characterized ureteral stone seen on computed tomography (CT), including the assessment of stone size, location, the degree of hydronephrosis, and stranding. We excluded patients with isolated intra-renal stones because these stones are treated using a different management approach. We also excluded patients who had a prior ED renal colic visit within 30 days because our intent was to study incident cases and to exclude patients who had already failed outpatient management. We excluded patients who were referred for direct urology care because they were thought to represent a selected higher complexity group already deemed to require surgical involvement, and we also excluded patients who had out-of-region postal codes, as their follow-up ED visits and hospitalizations could have occurred at hospitals outside the study areas.
Study procedures
During the study period, there were no renal colic management protocols in place, and the patients were managed at the ED physicians’ discretion in both cities. The usual treatment for acute renal colic in Vancouver is a trial of spontaneous passage, and the treatment for most significant stones in Calgary is admission for early surgical intervention, which may involve stone destruction, stone extraction, ureteral dilation, or stenting. This geographic treatment variability provided a unique opportunity to study comparable cohorts of patients in similar health systems exposed to different management strategies.
Data capture
Patient demographics, arrival mode, presenting complaint, triage category, and index disposition were captured from regional ED clinical databases. ED revisits, hospitalizations, and procedures, as well as ED and inpatient diagnoses, were obtained from the discharge abstract database of the hospitals. To assure inclusion of all relevant Vancouver procedures, the Vancouver Coastal Health Authority (VCHA) regional diagnostic imaging (DI) database was queried to identify outpatient lithotripsy procedures, as well as inpatient or outpatient surgical procedures not coded in the hospital discharge abstracts. All urological procedures and lithotripsy in Southern Alberta occur at a single site; therefore, these were reliably captured in the Calgary zone administrative data and verified by auditing a 20% sample of the electronic patient charts. In Alberta, the provincial health system Data Integration Management and Reporting unit oversees the capture, data management, and data quality of all health system data, and in Vancouver, these functions are performed by the VCHA Decision Support Group. Data were managed in accordance with a provincial data transfer agreement involving both health regions.
Outcomes
Hospital admissions and interventions during the initial ED visit were considered index visit events. Subsequent renal colic-related ED visits, admissions, and rescue interventions that occurred after the index visit discharge, but within 60 day of the index encounter, were considered outcome events. Rescue events occurring after the index visit discharge were considered proxies for patients in severe distress or failure of an intended management strategy.Reference Hollingsworth, Norton and Kaufman 20 , Reference Scales, Saigal and Hanley 27 Our primary outcome was the occurrence of hospitalization or intervention (ureteroscopy, stenting, nephrostomy, or extracorporeal shock wave lithotripsy [ESWL]) during the study period. Secondary outcomes included index visit hospitalization and intervention rates, 60-day ED revisits, hospitalizations, and rescue interventions stratified by city. Many patients had scheduled procedures (i.e., cystoscopy for stent removal) arising from study-related interventions. These were tabulated, but not reported, and were not considered rescue procedures or outcome events.
Sample size
Based on prior data,Reference Innes, Lang, McRae and Grafstein 23 we estimated that 25% of the patients would require readmission or intervention within 60 days. We determined that 1091 patients per group would provide 80% power to detect a difference of 5% in 60-day event rates between cities, at a 95% confidence level. For convenience reasons, and to increase the precision of secondary outcome estimates, we analyzed a full year of data from both cities.
Analysis
Descriptive analyses were performed using means (± standard deviation [SD]), medians (interquartile range [IQR]) or proportions, with estimated differences and 95% confidence intervals (CI) as appropriate. Observed differences in patient characteristics were assessed using t-tests or Wilcoxon rank sum tests. Observed differences in ED revisit rates, admissions, procedures, and other categorical outcomes were assessed using Pearson’s chi-squared test or Fisher’s exact test, as appropriate. Analysis of variance (ANOVA) or Kruskal-Wallis tests were used to evaluate parametric or non-parametric multiple group comparisons. For non-normally distributed data, we used bootstrap methods (resampling with replacement) to recreate sampling distributions and estimate median differences and related CIs. We applied a permutation test to generate the null distribution of hypotheses and compute empirical p values for these comparisons.
We evaluated our primary outcome and the need for hospital admission or intervention during the study period, using a time to event analysis. Events were plotted on Kaplan-Meier curves, and hazard ratios (95% CI) were generated using the Vancouver cohort as the reference group. Patients who did not have an outcome event during the 60-day follow-up were censored at that time. We used Cox proportional hazards models to adjust for differences in key covariates including patient age, sex, city, stone size, stone location, the degree of hydronephrosis, triage acuity level, index visit length of stay, and interactions between stone size and location. Statistical analyses were conducted using the R statistical package (the R Foundation for Statistical Computing; http://www.R-project.org/).
RESULTS
During the study year, 4902 in-region patients were seen with an index ED diagnosis of renal colic (Figure 1). Of these, 3105 (63.3%) had a CT at their index visit, and 213 (4.3%) had a CT within 30 days of their stone episode. Five hundred forty-five (11.1%) had an ultrasound (US) during their index visit, and 49 (1.0%) had a US within 30 days of their stone episode. Overall, 3518 (71.8%) had a US or CT imaging during their index visit, and 3775 (77.0%) had imaging within 30 days of the index visit and during their stone episode. The number of studies did not equal the number of patients because some patients had two studies during the index visit or study period. Based on a lack of imaging, 1127 patients were excluded. Another 411 patients were excluded because imaging confirmed only isolated intra-renal stones. There were 3283 patients with well-characterized ureteral stones on CT (Table 1). The mean age of the study group was 50.6 years, and slightly more than two-thirds were male. The stone incidence was higher in Calgary, but the age and sex distribution, EMS arrival rates, day and time of arrival, triage acuity level, vital signs, white blood cell counts, and serum creatinine levels were similar. Table 1 shows that the stone length was slightly larger in Calgary, although the width (transverse diameter) was the same. The stone location was similar between cities, with no difference in the proportions of the proximal, middle, or distal ureteral stones. Concerning the subjective stone parameters, Calgary had higher proportions of patients with moderate or severe hydronephrosis (38.0% v. 32.7%, respectively), and Vancouver had more patients with peri-renal stranding (61.1% v. 55.7%, respectively).
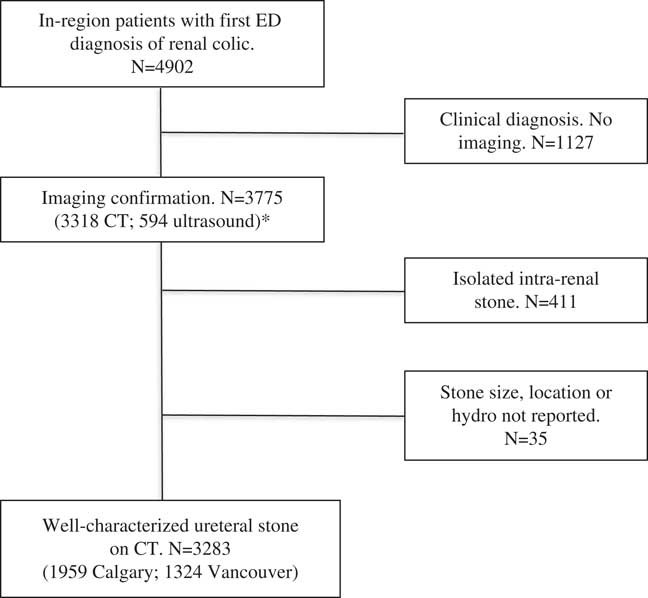
Figure 1 Study Flow Sheet.
*Note: Number of imaging studies does not equal number of patients because some patients underwent two or more studies during the index visit or during the study period.
Table 1 Patient and stone characteristics

BP=blood pressure; CTAS=Canadian Triage and Acuity Scale; Diff=difference; IQR=interquartile range; EMS=emergency medical service; SD=standard deviation; WBC=white blood cell count.
* CTAS 2–3 are the high acuity emergent (2) and urgent (3) categories.
Table 2 shows that the median wait time to see a physician was shorter in Vancouver than Calgary (34 v. 70 min, respectively), as was the ED length of stay (4.0 v. 5.5 hours, respectively). The latter finding was related to higher admission rates in Calgary. Patients in Calgary were more likely to be hospitalized than patients in Vancouver (55.6% v. 10.3%, respectively) and to undergo urological intervention (52.1% v. 7.5%, respectively) during their index visit. Of the 1089 patients admitted in Calgary, 1021 (93.8%) had an immediate ureteroscopic procedure. Of the 160 patients admitted in Vancouver, 99 (61.9%) underwent an immediate intervention, with 87 ureteroscopic procedures and 12 shock wave lithotripsies.
Table 2 Treatment stratified by city
CI=confidence interval; Diff=difference; ED=emergency department; IQR=interquartile range; LOS=length of stay.
* Index visit interventions occurred during the index visit encounter.
The primary outcome, hospitalization or intervention during the study period, occurred for 1194 patients in Calgary and 414 patients in Vancouver (60.9% v. 31.3%, respectively; p<0.001). Table 3 summarizes the adjusted hazard ratios for the determinants of the primary outcome. The strongest predictor (adjusted hazard ratio) was a Calgary visit site (3.31), followed by proximal stone location (2.95), severe hydronephrosis (2.67), moderate hydronephrosis (2.25), mild hydronephrosis (1.43), ED length of stay (LOS) (1.23 per hour), and stone size (1.11 per mm of width). Age, sex, EMS arrival, triage acuity level, and peri-renal stranding were not associated with the occurrence of hospitalization or intervention.
Table 3 Determinants of the primary outcome (admission or intervention)
CTAS=Canadian Triage and Acuity Scale; ED=emergency department; LOS=length of stay.
* The primary outcome is a composite of hospitalization or stone intervention during the index visit encounter or within 60 days.
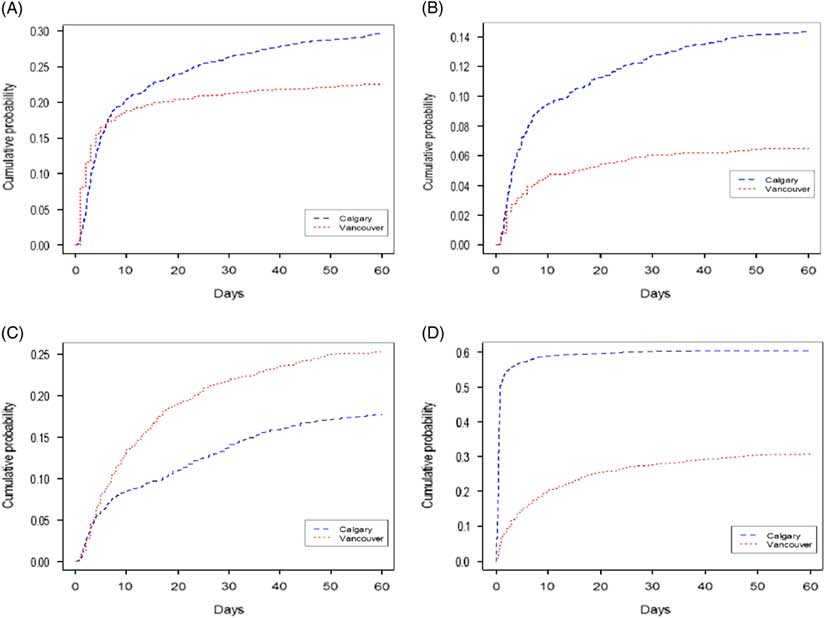
Table 4 shows that patients in Calgary were more likely to have ED revisits and hospital readmissions during the 60-day follow-up period, despite higher index admission and intervention rates (Figure 2A–B). Figure 2C shows that patients in Vancouver were more likely to undergo a rescue intervention at all time intervals after the index encounter than patients in Calgary (cumulatively, 25.3% v. 17.8%, respectively). By 60 days, 1183 patients in Calgary (60.4%) and 408 patients in Vancouver (30.8%) had undergone a stone intervention. Figure 2D shows that the total number of interventions occurring during the study period was substantially higher in Calgary, inclusive of index interventions.
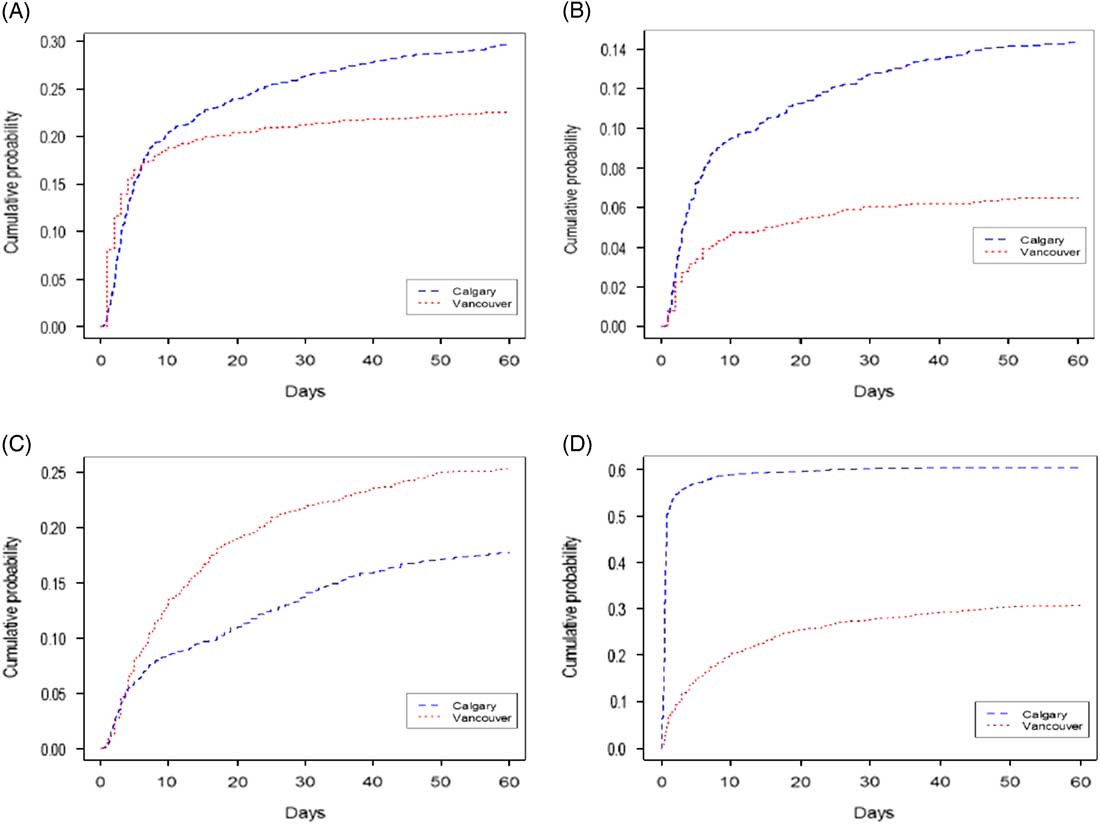
Figure 2 Sixty-day event rates by city (Kaplan-Meier plots). Figure 2A shows time to renal colic-related ED revisit in days. Figure 2B shows time to renal colic-related hospital readmission occurring after discharge from the index ED encounter or hospitalization. Figure 2C shows time to rescue intervention in days (note that more patients in Vancouver were eligible for an intervention based on low index intervention rates). Figure 2D shows time to intervention for all interventions including those performed during the index encounter.
Table 4 Sixty-day outcomes stratified by city
CI=confidence interval; Diff=difference.
* Refers to patients requiring inpatient care after discharge from the index ED-hospital encounter. Rescue procedures were unplanned interventions (ureteroscopy or ESWL) occurring after discharge from the index encounter, which excluded interventions performed during the index encounter.
† Any procedure refers to all patients who had a procedure during the index encounter or 60-day follow-up period.
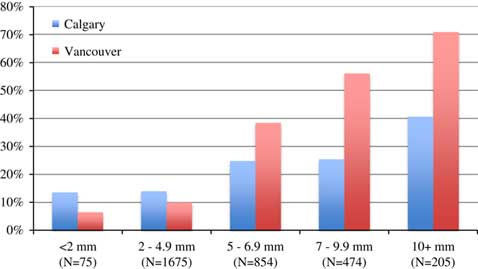
Table 5 stratifies patients by stone size, showing that 2.3%, 51%, 26%, 14.4%, and 6.3% of the patients had stone size categories of <2, 2.0–4.9, 5.0–6.9, 7.0–9.9, and ≥10 mm, respectively. The size distributions were similar in the two cities, but patients in Calgary had more stones in the 7–9.9 mm category than patients in Vancouver (16.1% v. 12.0%, respectively). Figure 3 shows that the Calgary index intervention rates were higher in all stone size categories. Table 5 and Figure 4 indicate that a 60-day readmission or rescue intervention occurred significantly less often in Vancouver for stones under 5 mm. Conversely, for stones over 5 mm, a 60-day readmission or rescue intervention occurred less often in Calgary, although this finding was tempered by the fact that more patients in Calgary than in Vancouver (75% v. 15%, respectively) with these larger stones had already undergone a stone removal.
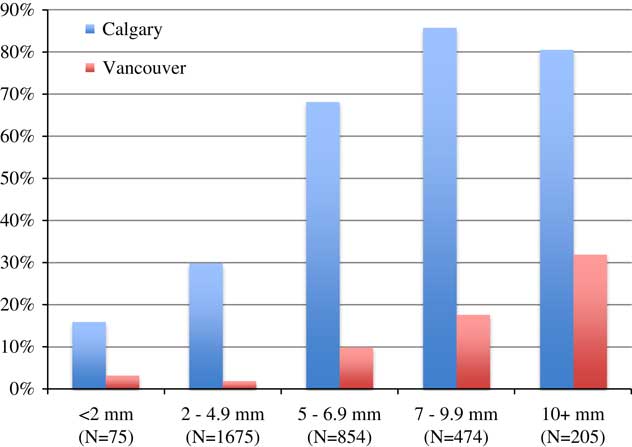
Figure 3 Index visit intervention stratified by stone size.
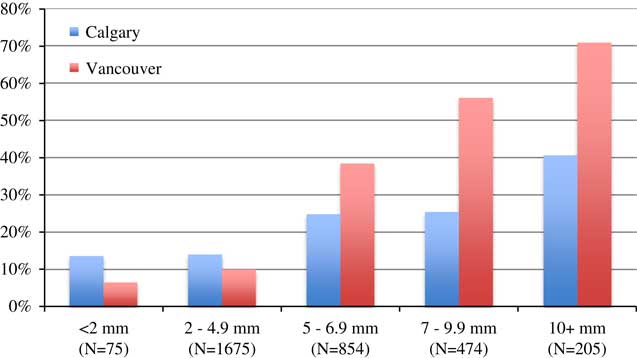
Figure 4 Sixty-day rescue intervention or readmission stratified by stone size.
Table 5 Management and 60-day outcomes stratified by stone size
CI=confidence interval; ED=emergency department.
* Readmission and readmit or intervention* refer to hospitalizations and procedures occurring after discharge from the index encounter, thus, excluding the index visit hospitalizations and procedures. Interventions were limited to rescue interventions and did not include planned follow-up procedures (i.e., cystoscopy for stent removal).
DISCUSSION
This population-based study assessed all patients in two comparable health regions who had an incident renal colic ED visit with a well-characterized ureteral stone during a one-year period. Our data indicated profoundly different management approaches, suggesting a lack of clarity in defining the patient populations who would most likely benefit from early intervention, as well as the need for a more standardized approach to referral and intervention. Our analyses were stratified by region rather than by intervention and, therefore, did not clearly define the association between treatment and outcome; however, the data showed that an early interventional approach was associated with a 50% higher cumulative probability of an ED revisit and double the rates of readmission and intervention.
Higher adverse event rates in a more interventional setting are surprising in that early definitive stone management would be expected to reduce the need for subsequent unplanned ED visits and hospital-based care. It is not surprising to see ED revisit and hospitalization rates of 22.6% and 6.5%, respectively, in a system in which early intervention rarely occurs. It is surprising to find rates of 29.7% for ED revisits and 14.3% for readmission at 60 days in a system (Calgary) that provides early definitive intervention for most patients with significant stones. There are several possible explanations for this finding. During an acute stone episode, many patients have ongoing symptoms. Access to operating room (OR) time is more limited in Vancouver that could have led to inappropriately low rescue intervention rates. Conversely, Calgary has limited access to outpatient urology resources but better access to urgent OR time; hence, urologists may be more likely to “do something” if patients return to EDs with ongoing pain. The observational experience of physicians at the study sites is that patients who return to the hospital after having a stone removal procedure do so as a result of a clot or stent pain, postoperative ureteral edema or spasm causing an obstruction, incomplete stone removal, infection, or even ongoing post-procedural pain that was unexpected (because patients expected the pain to resolve immediately after stone removal). In some cases, access-related difficulties in scheduling stent removal caused patients to reappear in EDs with ongoing stent pain. The ED revisit and readmission rates seen in this study demonstrated that the ureteral stone experience does not always end when the intervention is complete for a variety of reasons. They also highlighted the need for research into optimal stenting practice, notably, patient selection, duration of stenting, discharge education resources, and outpatient follow-up support for stented patients.
The finding of lower rescue intervention rates for patients who had immediate intervention was not surprising. We assumed that patients whose stone had been removed during ureteroscopy had no further need for repeat ureteroscopy unless the stone was incompletely treated. As the stone-free outcomes for modern day ureteroscopy with holmium:YAG lithotripsy and/or a stone basketing approach have been nearly 100% for ureteral stones,Reference Teichman, Rao, Rogenes and Harris 28 early intervention would make sense if there were clinical factors that would help predict failure of spontaneous passage.Reference Ordon, Andonian and Blew 5 Our data suggest that current processes for identifying patients who would likely benefit from early intervention are highly variable and imperfect in terms of sensitivity and specificity and that the ideal rate of intervention probably falls between these two divergent practices.
The main finding of this study was that 60-day adverse event rates were not distributed equally across the spectrum of stone sizes. Figure 4 shows that an early interventional approach was associated with higher adverse event rates (readmission or rescue intervention) for the subgroup of patients with stones of <5 mm and that a non-interventional approach was associated with higher adverse event rates for patients with stones of >5 mm. Prior research also showed an inverse relationship between stone size and spontaneous passage rates, although studies have been limited by a small sample size with broad CIs around passage estimates. Segura et al. reported passage rates of 25%–53% for stones >5 mm and 71%–98% for smaller stones.Reference Segura, Preminger and Assimos 29 Ueno et al. documented an overall 53% passage rate for 520 patients with ureteral calculi and recommended intervention for stones of >8 mm based on size-related passage.Reference Ueno, Kawamura, Ogawa and Takayasu 30 Papa et al. found that a stone size of >6 mm was highly associated with the need for intervention,Reference Papa, Stiell and Wells 31 and a meta-analysis of five studies with a total of 224 patients described passage rates of 47% for stones of >5 mm and 68% for smaller stones.Reference Preminger, Tiselius and Assimos 6 Size alone is not sufficient to predict passage accurately, and stone location may be a more powerful determinant. Coll et al. reported passage rates of 48%, 60%, 75%, and 79% for proximal, middle, distal, and ureterovesical (UV) junction stones, respectively, regardless of size.Reference Coll, Varanelli and Smith 7 If size were used as the determinant for intervention, the CT transverse diameter would be the preferred measure, because US examinations can lead to size overestimates, particularly for small stones.Reference Ray, Ghiculete, Pace and Honey 32
Our findings suggest that an interventional approach leads to better outcomes for stones of >5 mm, and this finding is relatively robust given the sample size of more than 3000 patients studied in diverse settings. These findings are compatible with recent Canadian guidelines, which state that stones of >5 mm are less likely to pass spontaneously and that patients with these stones should be counselled on their options.Reference Ordon, Andonian and Blew 5 Our data illustrated substantial practice variability and seemingly high intervention rates in one setting but also show that one-third of patients in the less interventional setting ultimately required stone removal, likely enduring a significant period of potentially avoidable morbidity. Conceptually, the area under the Vancouver Kaplan-Meier plot (Figure 2D) reflects patients who needed an intervention but had not yet had one, and the area between the curves represents patients who had a procedure but would not have done so if they were treated in the alternate setting. Therefore, the higher adverse event rates for patients in Calgary with small stones and higher adverse event rates for patients in Vancouver with large stones suggested that an overly interventional approach for small stones and a non-interventional approach for larger stones were both associated with patient morbidity and that outcome events were driven in part by overtreatment of stones in one setting and undertreatment of stones in the other. If patients who ultimately require intervention could be identified more accurately at the index visit, patient disability could be mitigated using a more specifically targeted intervention.
The outcomes studied, ED visits, hospitalizations, and follow-up procedures were chosen because they were reliably captured in health system data and because the investigators viewed them as proxies for treatment failure. Our premise was that unplanned ED visits and hospital readmissions were indicators of patients in distress and that rescue interventions usually represented a diversion from a chosen path of care or failure of a treatment strategy. However, these outcomes were sometimes driven by factors other than treatment failure. For example, many patients who have had a prior stone removal learned that the treatment for stones was an intervention, not spontaneous passage, and insisted on intervention if they developed another symptomatic stone. Within an interventional culture, many physicians feel that early stone removal is preferable to the uncertainty of spontaneous passage and that intervention is the approach they would want for themselves. In such settings, ED physicians would be more likely to refer marginal patients with smaller stones or even patients with mild to moderate ongoing symptoms who might not require intervention. Such referrals may generate patient expectations for current and future intervention, as well as convey a message to the surgeon that the patient has failed medical management and requires a surgical approach. These patient and physician interactions are less likely in a setting that defaults overwhelmingly to spontaneous passage.
LIMITATIONS
The most important limitation of this study was that it assessed population-level outcomes, not patient-level responses to a therapeutic strategy. Our outcomes were measures of treatment failure, not treatment success. We did not directly measure stone passage or assess patient experience, quality of life, lost productivity, or symptom severity. It is possible that some patients experienced significant morbidity but did not seek hospital-based care or require intervention during the follow-up period; therefore, the absence of an outcome event does not mean that patients had optimal care or the best possible experience. It is possible that ED revisit rates might relate to differences in primary care access or postdischarge care (e.g., adequacy of analgesic prescription). The findings in this study are applicable to patients with well-characterized ureteral stones; they do not apply to all cases of renal colic or patients with a clinical diagnosis of renal colic. We did not capture outpatient office or clinic visits and cannot comment on the community care that was available, required, or delivered in the two cities. Further, there were undoubtedly patients who did not require hospital-based care during the 60-day follow-up period but who experienced exacerbations requiring intervention after 60 days; therefore, we cannot say that we captured all outcome events in the two populations. Future studies should assess cost effectiveness and measure patient-reported outcomes such as disability, pain, quality of life, and functional status in contrasting systems or interventional approaches.
CONCLUSIONS
This study demonstrated high variability in the management of ureteral colic and the need for a more standardized approach to referral and intervention. We found that an early interventional approach was associated with higher health system utilization in the form of cumulative ED revisit, hospitalization, and intervention rates. If these events are markers of patient disability, then a less interventional approach to small stones and earlier definitive management of large stones may reduce health system utilization and improve outcomes for patients presenting with an index ED visit for acute ureteral colic.
Competing interests: This study was funded by the MSI Foundation.