Introduction
It is estimated that 264,000 or 0.75% of the Canadian population are living with the effects of stroke.1 Ischemic strokes are 10 times more common than hemorrhagic strokes.Reference Andersen, Olsen, Dehlendorff and Kanmesgaard2 Although hemorrhagic strokes have a higher mortality in the acute phase, it has been shown that outcomes of both hemorrhagic and ischemic strokes in patients discharged from a rehabilitation setting are similar.Reference Scrutinio, Monitollo and Guido3 It is established that early in-patient rehabilitation for stroke patients is associated with improvement, better outcomes, and a higher percentage who return home.Reference Jörgensen, Nakayama, Raaschou, Larsen, Hübbe and Olsen4–Reference Rollnik, Bertram and Bucka8 However, some patients are more likely to benefit than others; to maximize the use of scarce and expensive resources, some stratification and selection of patients are necessary.
The functional independence measure (FIM) is an 18-item assessment of physical, psychological, and social functioning. The AlphaFIM, introduced in 2014 in Ontario, is more specifically designed for indices of stroke severity (using eating, grooming, bowel management, toilet transfers, expression, and memory) while patients are in the acute stroke units.Reference Scrutinio, Monitollo and Guido3, Reference Ween, Alexander, D’Esposito and Roberts9, Reference Ring, Feder, Schwartz and Samuels10 In general, values between 40 and 80 for AlphaFIM are commonly used to select patients for rehabilitation: values above 80 can usually be managed in the community and values below 40 are often selected for “slow stream” rehabilitation or long-term care (LTC) from discharge from the acute stroke unit.Reference Ween, Alexander, D’Esposito and Roberts9, Reference Hakkennes, Brock and Hill11, Reference Rayegani, Raeissadat, Alikhani, Bayat, Bahrami and Karimzadeh12
Because of the higher incidence of ischemic stroke and since ischemic and hemorrhagic strokes often have different pathogeneses and comorbidities, we chose to study ischemic stroke patients who were admitted to our rehabilitation unit.Reference Andersen, Olsen, Dehlendorff and Kammersgaard13 We selected patients admitted to our rehabilitation unit as there was a more comprehensive capture of variables than were obtained during the acute phase from referring hospitals.
The purpose of our study was to use a broad approach, weighing all the variables at our disposal to determine which were the most likely to be associated with transfer to LTC versus discharge home.
Methods
Records of all patients with acute ischemic stroke as the principal diagnosis who were discharged from our general rehabilitation unit at Grey Bruce Health Services in Owen Sound, Ontario, between January 1, 2005 and December 31, 2015 were reviewed and the following information was extracted: age at onset of stroke, sex, FIM, and AlphaFIM scores prior to admission and FIM scores at admission and at discharge from rehabilitation, difference in FIM between admission and discharge to rehabilitation. (FIM change), residence (living at home versus chronic care facility), independent activities of daily living, right versus left versus both cerebral hemispheres, bladder incontinence while in rehabilitation, bowel incontinence while in rehabilitation, dysphagia while in rehabilitation, aphasia, Berg Balance Scale score on admission and at discharge, change in Berg Balance Scale score from admission to discharge, ability to transfer at discharge, Montreal Cognitive Assessment (MoCA) score (done within 3 days of admission to rehabilitation), hemianopsia (assessed by a qualified neurologist), the presence of caregiver and having independent financial support for care. Additionally, any comorbidities were recorded in a free text field. This free text field was mined at the data analysis step to identify the most common comorbidities for assessment. These were diabetes mellitus, atrial fibrillation, previous stroke, coronary artery disease (CAD), smoking, dyslipidemia, CHF, hemiparesis, previous coronary bypass graft (CABG), benign prostatic hypertrophy (BPH) with urinary symptoms, chronic obstructive pulmonary disease, and obesity.
Patients were categorized as being either discharged home or to LTC, which we defined as any type of chronic care facility ranging from assisted living to higher level care where all activities of daily living and feeding are provided, as the dependent variable. Univariable logistic regression models were run for each of the independent variables to assess their relationship with the discharge destination. Correlation among the independent variables was assessed using Pearson and Spearman’s correlation coefficients, where appropriate for variable types. Where pairs of variables were found to be highly correlated (p > |0.8|), variables with higher recording consistency, or deemed more biologically plausible were retained for further modeling. Variables with a p-value of <0.2 were used to build a multivariable logistic model using a manual backwards selection approach, maintaining variables with a p-value of ≤0.05. A priori rules for model building were set as follows: (1) a cut-off of 30% was used to assess confounding during the model building process, where variables that produced a >30% change in other significant coefficients would be forced into the model. (2) Linear variables were visualized using locally weighted scatterplot smoothing with the log odds of the discharge destination in order to identify curvilinear relationships. Quadratic terms were introduced to the model where appropriate, or variables were categorized using logical groupings based upon cut-offs found in the literature. (3) Biologically significant interaction terms were assessed using a p-value cut-off of 0.05.
Variables modeled as linear were age and change in Berg score from admission to discharge. Variables that were not well modeled in a linear manner and were therefore categorized were Berg scores at admission and discharge, categorized into <20, 20–<40, and 40+; and change in FIM was categorized to 1–4 and 5+. These categorizations allowed for more appropriate modeling and to separate those with severe disabilities from those with less marked deficits. Additionally, location of stroke was modeled as categorical (left, right, and both hemispheres).
Results
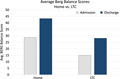
Table 1 lists the variables, numbers of patients with data recorded for each variable, the odds ratios, and p-values for univariable analysis against the destination of being discharged to LTC or home. All of the ischemic strokes are involved in the cerebral hemispheres except one pontine stroke. We eliminated that case from our review. The following were significant predictors of LTC disposition: age, admission, and discharge FIM scores (allowing determination of improvement in scores, Figure 1), AlphaFIM score, change in AlphaFIM score, dependency and site of accommodation before the stroke (which are likely to be closely related), presence of a caregiver, urinary and bowel incontinence, the Berg Balance Scale score (Figure 2), MoCA, and ability to transfer. Interestingly, the following did not reach significance: sex, dysphagia, aphasia, hemianopsia, and various comorbidities (diabetes mellitus type 2, atrial fibrillation, previous stroke, CAD, CHF, smoking, dyslipidemia, hemiparesis, BPH, and CABG).
Table 1: Univariable results for all predictor variables against the outcome of being discharged to LTC versus home
A fib, atrial fibrillation; BPH, benign prostatic hyperplasia; CABG, previous coronary bypass graft; CAD, coronary artery disease; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; Delta Alpha, difference in AlphaFIM score between admission and discharge; Delta Berg, change in Berg score between admission and discharge; FIM, functional independence measure; MoCA, Montreal Cognitive Assessment score; T2DM, type 2 diabetes mellitus.
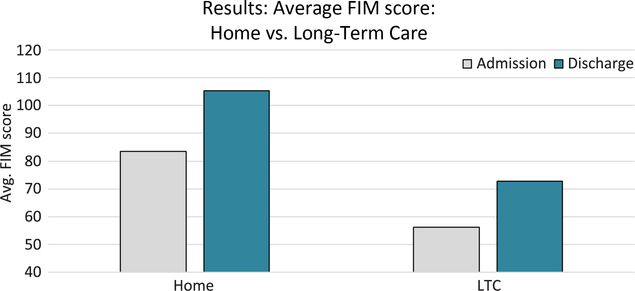
Figure 1: Average FIM score at admission and discharge for ischemic stroke patients discharged to home and LTC from the rehabilitation unit at Grey Bruce Health Services in Owen Sound, Ontario, between January 1, 2005 and December 31, 2015.
Figure 2: Average Berg Balance Scores at admission and discharge for ischemic stroke patients discharged to home and LTC from the rehabilitation unit at Grey Bruce Health Services in Owen Sound, Ontario, between January 1, 2005 and December 31, 2015.
Multivariable analysis showed the following five factors to have the most prominent associations with LTC disposition: age, bowel incontinence, residence prior to stroke, laterality of the stroke, and caregiver availability (Table 2). Patients were more likely to be discharged to LTC if they were older, living outside of the home before the stroke, had a right hemisphere stroke, suffered from bowel incontinence, and had no caregiver available.
Table 2: Multivariable results for logistic regression analyses of predictors associated with being discharged to LTC
Discussion
Our study focused on those patients who were discharged from a rehabilitation unit after acute ischemic stroke and differs from some earlier studies that examined patients in stroke units.Reference Hakkennes, Brock and Hill11, Reference Dutrieux, van Eijk, Marloes, van Heugen, Visser-Meily and Achterberg14–Reference Mirkowski, McClure, Speechly and Teasell20 Thus, our study had a selection bias, usually eliminating those patients with early mortality and AlphaFIM scores >80 and <40 (criteria for admission to rehabilitation after 2014). Our study was more inclusive of more independent variables than many earlier studies with respect to discharge destination from rehabilitation after acute ischemic stroke.
We found discharge destination to be associated with numerous variables at the univariable level: Berg balance score, indicating risk of falling (recently shown by Louie and EngReference Louie and Eng21 as a strong predictor of regaining unassisted ambulation), age (as shown previously by Scrutinio et al., Glader et al., and Bindawas et al.),Reference Scrutinio, Monitollo and Guido3, Reference Glader, Stegmayr, Terént, Huter-Åsberg, Wester and Asplund18, Reference Bindawas, Vennu, Mawajdeh and Alhaidary22 FIM score and improvement in FIM score during the stay on rehabilitation (as shown by Scrutinio et al. and Thorpe et al.),Reference Scrutinio, Monitollo and Guido3, Reference Thorpe, Garrett, Smith, Reneker and Phillips23 bladder and bowel incontinence (bladder incontinence was also shown to be related to LTC discharge by John et al.),Reference John, Bardini, Mégevand, Combescure and Dallenbach15 ability to transfer (not previously explored), and MoCA score (as shown by Chan et al.).Reference Chan, Altendorf, Healy, Werring and Cippolotti24 The self-perceived functional improvement, dependency for indoor functioning and social relations with family members/caregivers are also determinants in participation and eventual autonomy,Reference Törnbom, Hadartz and Sunnerhagen25 but this was not examined in our study.
Not surprisingly, patients who were already in LTC prior to their stroke would be unlikely to go home after a stroke, which would produce even greater disability. Similarly, the presence of a caregiver already in place would greatly enhance the chances of being discharged home, as others have shown.Reference Dutrieux, van Eijk, Marloes, van Heugen, Visser-Meily and Achterberg14, Reference Mirkowski, McClure, Speechly and Teasell20, Reference Pereira, Foley and Salter26 Some variables are inter-related, for example, younger patients are more likely to have a caregiver at home than older patients.Reference Dutrieux, van Eijk, Marloes, van Heugen, Visser-Meily and Achterberg14 It is of interest that comorbidities were not statistically associated with discharge destination. Some neurological deficits, for example, hemianopsia, aphasia, dysphagia also did not impact on discharge destination, as was shown by Dromerick and Reding,Reference Dromerick and Reding19 even though they may pose serious social and care challenges.Reference Wray and Clarke27 However, multiple, coexisting comorbidities at least in acute settings, can affect disposition.Reference Dromerick and Reding19, Reference Dutta, Thornton and Bowen28 This is especially important in the elderly, where treatment of acute complications can make a difference in outcome.Reference Kim, Lee and Sohn29
Our study had similar results to the larger Canadian Institute of Health Information (CIHI) study published in 2009.30 Motor function on admission was the strongest predictor of discharge destination, followed by whether or not the patient lived with someone prior to the stroke. There were some differences between our study and the CIHI report, in that all types of hemorrhagic strokes were included and comorbidities, continence, and Berg scores were not specifically included in the CIHI study. More detail was paid in the CIHI study to cognitive factors. A recent meta-analysisReference Burton, Ferguson and Barugh31 confirmed the importance of stroke severity and age as strong predictors of discharge to LTC. There was considerable heterogeneity among the 18 included papers, which were not comprehensive in including all possible variables; potentially modifiable (risk) factors were rarely examined.
Multivariable analysis revealed the five main variables that together were best able to predict the discharge destination: age, residence prior to stroke, right hemisphere site of stroke, bowel continence, and presence of caregiver. While increasing age, bowel incontinence, and the absence of a caregiver are logically expected to be linked to discharge to LTC (and were found to be statistically linked in our study), our finding that right hemispheric stroke patients are more likely to go to LTC than those with left or bilateral hemispheric strokes seems at odds with earlier papers.Reference Hedna, Bodhit and Ansan32 Prior research has suggested that left hemispheric strokes do worse than right hemispheric strokes, but these studies related to those with acute strokes: patients with left-middle cerebral artery strokes were more likely to show early mortality and an initially lower Glasgow Coma Scale score and higher National Institutes of Health Stroke Scale (NIHSS).Reference Hedna, Bodhit and Ansan32 However, the selective nature of our study eliminates these early differences and produces a more “even playing field”. Thus, a more direct comparison of right versus left hemispheric damage in the post-acute phase was possible.
Enduring unilateral spatial neglect (USN) is defined as “failure to report, respond, or orient to novel or meaningful stimuli presented to the side opposite the brain lesion when this failure cannot be attributed to either sensory or motor deficits.”Reference Heilman, Watson, Valenstein, Heilman and Valenstein33 While the hospital charts did not consistently mention USN, this is a feature of right hemisphere lesions, in contrast with left hemisphere lesions that have more language-related deficits.Reference Katz, Hartneb-Maeir, Ring and Soroker34–Reference Zoccolotti, Antonucci, Judica, Monenero, Pizzamiglio and Razzano37 Patients with USN do not improve as much in motor or sensory function or activities of daily living during the period of acute hospitalization and rehabilitation as those without USN, in comparison with those patients with hemiparesis but without neglect.Reference Katz, Hartneb-Maeir, Ring and Soroker34, Reference Spaccavento, Cellamare, Falcone, Loverre and Nardilli38 Thus, those right hemisphere-damaged patients with neglect tend to show less improvement and would probably be more likely to require LTC.Reference Klinke, Hjaltoson, Berg, Tryggvadóttirt and Jónsdóttirt39 Most patients (87%) with right hemisphere strokes showed USN in the series of Klinke et al.Reference Klinke, Hjaltoson, Berg, Tryggvadóttirt and Jónsdóttirt39 The relative lack of improvement during rehabilitation in right hemisphere damaged (RHD) compared to left hemisphere damaged (LHD) stroke patients was also noted by Ween et al.Reference Ween, Alexander, D’Esposito and Roberts9 We suggest that neglect and other deficits should be further explored with advanced techniques, such as fMRI, to explore how brain networks are affected and ultimately therapy can be targeted accordingly.Reference Riestra and Barrett40
While lower MoCA scores increase the probability of LTC destination, this may apply primarily to left hemispheric strokes. It has been shown that the MoCA lacks sensitivity and specificity in the detection of overall cognitive deficiency, processing speed, executive functions, and nonverbal memory for patients with right hemisphere strokes compared with those with left hemispheric strokes, when patients were assessed with comprehensive neuropsychological testing.Reference Wray and Clarke27 This could create a problem in designing rehabilitative strategies for patients with right hemispheric strokes when MoCA is used as the main cognitive screening tool. It is noteworthy that MoCA scores were similar in discharge destination from acute stroke units in the study by Dutrieux et al.Reference Dutrieux, van Eijk, Marloes, van Heugen, Visser-Meily and Achterberg14 More in-depth cognitive assessment indicates that visuospatial, executive function, memory, and language function were the most important vascular cognitive impairments in determining functional outcomes.Reference Park, Sohn, Jee and Yang41 Also, pre-stroke dementia did not alter the functional outcome of elderly patients with ischemic stroke; both the demented and nondemented groups (using MoCA scoring criteria) made similar motor gains on FIM scoring.Reference Mizrahi, Arad and Adunsky17 Similarly, the NIHSS has been shown to be more predictive of outcome for LHD than RHD ischemic strokes.Reference Yoo, Romero and Nogueiro42
We found no significant differences between men and women for discharge to LTC. Other studies had variable results, some showing that men were more likely to require institutional care than women or that there were no sex differences in disposition.Reference Holroyd-Leduc, Kapral, Austin and Tu43–Reference Sharma, Fletcher and Vassallo46 The largest study, involving thousands of patients in the Swedish stroke registry found women fared worse than men, but women had more unfavorable predisposing factors.Reference Glader, Stegmayr, Terént, Huter-Åsberg, Wester and Asplund18 It is possible that our study was underpowered to show a sex difference. This may be worth examining in a larger, future study, as there may be gender differences in ability to cope independently or in the availability of a spouse being available to act as caregiver.
Our study has several other limitations. These largely relate to its selection bias and retrospective nature, prone to have missing data, and imprecision for localization and classification of stroke. Some data were missing in our retrospective review, although our calculations took this into account. From the review of charts and neuro-imaging (mainly CT images) it was not always possible to separate small vessel/lacunar strokes from larger vessel or cardioembolic strokes. Most of our cases were large vessel rather than lacunar strokes; only three were obviously lacunar in nature and none were recognized as brainstem infarcts. While our study is not representative of the case mix of patients admitted for stroke rehabilitation in most centres, the severity of strokes as measured by preadmission AlphaFIM and FIM scores during rehabilitation is probably similar. As Ween et al.Reference Ween, Alexander, D’Esposito and Roberts9 pointed out the lesion site and lesion type (large vessel versus small vessel strokes) may have confounding effects on discharge destination, having predominantly large vessel ischemic strokes in our series allows for a more direct comparison of lesion site.
The probability of discharge home versus LTC is best understood by considering multiple variables, as in our study.Reference Everink, van Haastregt, van Hoof, Schols and Kempen47, Reference Itaya, Murakami, Nomura, Fukushima and Nishigaki48 Using grouped data to make decisions about individual patient discharge destination has limitations. Among individual cases, there will be different weightings of variables dependent on caregivers, affect, motivation, and other factors that require individual consideration.Reference Nelson, Hanna, Hall and Calvert49 This is not to deny that any improvement gained in rehabilitation (Figures 1 and 2) and continued outreach care is worth the effort in many patients destined for LTC, as the subsequent level of care required, resource implications, and quality of life can benefit from the gains made in rehabilitation. Attention should be given to the modifiable risk factors that respond to the rehabilitative effort. Clearly, more work is needed to model the variables in clusterReference Simpson, Wilmskoetter and Hong50, Reference Duncan, Bushnell and Rosamond51 or multivariable analysis in a larger sample size, preferably in a prospective study,Reference Duncan, Bushnell and Rosamond51 for timely, projected effects of rehabilitation strategies on patients with ischemic strokes on the full spectrum of outcomes.Reference Cameron, O’Connell and Foley52 While such population studies will help us to pay more attention to modifiable variables, each patient requires individual attention, as the importance or weighting of the various factors will vary with each case.
Statement of Authorship
Each author contributed to the design and authorship of the article. AS collected and tabulated the data; SG-K performed the statistical analysis; and GBY performed literature searches and contributed to the discussion.
Disclosures
The authors declare no conflicts of interest.