Introduction
The efficacy of exposure therapy (‘exposure’) for anxiety disorders has been well-established, yet it remains among the least utilized evidence-based interventions (EBI) in community settings (e.g. Thomassin et al., Reference Thomassin, Marchette and Weisz2019). It has been posited that the large practice gap for exposure is associated with the unique therapist- and organization-level requirements for its delivery (Becker-Haimes et al., Reference Becker-Haimes, Byeon, Frank, Williams, Kratz and Beidas2020). Exposure calls for patients to confront anxiety-provoking situations in a graded manner to gather new learning about the safety and tolerability of feared situations. Exposure therapists must be willing to encourage patients to encounter feared situations and to tolerate temporary escalations in patient distress. Consequently, only 10–30% of therapists endorse using exposure in routine clinical care (Becker et al., Reference Becker, Zayfert and Anderson2004; Borntrager et al., Reference Borntrager, Chorpita, Higa-McMillan, Daleiden and Starace2013; Trask et al., Reference Trask, Fawley-King, Garland and Aarons2016; Wolitzky-Taylor et al., Reference Wolitzky-Taylor, Zimmermann, Arch, De Guzman and Lagomasino2015), and patients consistently report difficulty accessing this frontline treatment (Merikangas et al., Reference Merikangas, He, Burstein, Swendsen, Avenevoli, Case, Georgiades, Heaton, Swanson and Olfson2011). Recent efforts to enhance the dissemination of exposure have included evaluations of practice barriers and the development of targeted training strategies (Farrell et al., Reference Farrell, Kemp, Blakey, Meyer and Deacon2016; Frank et al., Reference Frank, Becker-Haimes, Rifkin, Norris, Ollendick, Olino, Kratz, Beidas and Kendall2020). Progress in the development of exposure-specific training strategies requires ongoing evaluation of therapists’ perceptions of training and their experiences of implementing exposure following training and consultation. Accordingly, this paper evaluates therapists’ perceptions of an experientially focused training approach and their efforts to implement exposure following training.
Exposure poses a unique set of implementation challenges given its complexity and tendency to evoke distress in providers new to its delivery (Garcia, Reference Garcia2017; Pittig et al., Reference Pittig, Kotter and Hoyer2018). Implementation frameworks, such as the Consolidated Framework for Implementation Research (CFIR; Damschroder et al., Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009), can help identify the breadth of constructs associated with implementation success. In addition to therapist-level factors (i.e. characteristics of individuals involved), the CFIR highlights the importance of considering the inner setting (e.g. organizational culture), the outer setting (e.g. patient needs and resources), characteristics of the intervention itself, and the implementation process. Influences at each of these levels interact (Becker-Haimes et al., Reference Becker-Haimes, Williams, Okamura and Beidas2019), such that the success of a therapist in implementing an intervention will be affected by the therapists’ own beliefs, their clients’ characteristics, organizational factors of their practice setting, and the context of the region in which they work (Beidas et al., Reference Beidas, Stewart, Adams, Fernandez, Lustbader, Powell, Aarons, Hoagwood, Evans, Hurford, Rubin, Hadley, Mandell and Barg2016; Williams, Reference Williams2016).
Most assessments of organizational determinants of exposure use have centered on broad aspects of organizational culture and climate (Cook et al., Reference Cook, Dinnen, Thompson, Ruzek, Coyne and Schnurr2015; Sayer et al., Reference Sayer, Rosen, Bernardy, Cook, Orazem, Chard, Mohr, Kehle-Forbes, Eftekhari and Crowley2017) that are key to the implementation of EBIs in general (Becker-Haimes et al., Reference Becker-Haimes, Williams, Okamura and Beidas2019). One evaluation of therapists trained in exposure found that factors such as the perceived acceptance of exposure in the organization and available supervisor support were implementation facilitators (Ringle et al., Reference Ringle, Read, Edmunds, Brodman, Kendall, Barg and Beidas2015). In contrast, other surveys of community mental health (CMH) providers have found little association between perceived organizational barriers and exposure usage (Becker-Haimes et al., Reference Becker-Haimes, Okamura, Wolk, Rubin, Evans and Beidas2017; Wolitzky-Taylor et al., Reference Wolitzky-Taylor, Chung, Bearman, Arch, Grossman, Fenwick, Lengnick-Hall and Miranda2019). Less research has explored the specific organizational capacities necessary to support exposure use. In a recent survey of anxiety specialty clinic leaders, Becker-Haimes and colleagues (Reference Becker-Haimes, Byeon, Frank, Williams, Kratz and Beidas2020) found a consensus on the facilitative importance of supervisor knowledge and support, therapist comfort seeking support from colleagues, and flexibility to change the setting and duration of exposure sessions. Taken together, these findings suggest a need to better understand exposure-specific organizational determinants across a variety of clinical settings.
In addition to implementation barriers at the organization level, there are also therapist-level barriers that influence the implementation and quality delivery of exposure. Therapist-level determinants warrant focus because they are most proximal to implementation and because, as noted by Damschroder and colleagues (Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009), ‘individuals are carriers of cultural, organizational, professional, and individual mindsets, norms, interests, and affiliations’. Thus, targeting therapist-level beliefs and behaviours holds promise to eventually extend to broader organizational and contextual change. The most salient therapist-level barrier is therapists’ negative beliefs about exposure, which include fears that exposure may be harmful or intolerable for therapists and their patients (Deacon et al., Reference Deacon, Lickel, Farrell, Kemp and Hipol2013c; Gola et al., Reference Gola, Beidas, Antinoro-Burke, Kratz and Fingerhut2015; Meyer et al., Reference Meyer, Farrell, Kemp, Blakey and Deacon2014; Olatunji et al., Reference Olatunji, Deacon and Abramowitz2009; Rosqvist, Reference Rosqvist2005). Specifically, therapists worry that implementing exposure will damage therapeutic alliance, lead to client attrition, cause damage to emotionally fragile clients, and lead to symptom exacerbation (Deacon et al., Reference Deacon, Lickel, Farrell, Kemp and Hipol2013c; Gola et al., Reference Gola, Beidas, Antinoro-Burke, Kratz and Fingerhut2015; Meyer et al., Reference Meyer, Farrell, Kemp, Blakey and Deacon2014; Olatunji et al., Reference Olatunji, Deacon and Abramowitz2009; Rosqvist, Reference Rosqvist2005). Despite clear research evidence to the contrary (Deacon et al., Reference Deacon, Lickel, Farrell, Kemp and Hipol2013c; Foa et al., Reference Foa, Zoellner, Feeny, Hembree and Alvarez-Conrad2002; Kendall et al., Reference Kendall, Comer, Marker, Creed, Puliafico, Hughes, Martin, Suveg and Hudson2009; Olatunji et al., Reference Olatunji, Deacon and Abramowitz2009), these beliefs persist. Specifically, community therapists have been shown to endorse negative beliefs about exposures (Deacon et al., Reference Deacon, Kemp, Dixon, Sy, Farrell and Zhang2013b), and these negative beliefs are associated with overly cautious delivery of therapy (Farrell et al., Reference Farrell, Deacon, Kemp, Dixon and Sy2013). However, training approaches that specifically address therapists’ negative beliefs about exposures have shown promise in improving attitudes (Farrell et al., Reference Farrell, Kemp, Blakey, Meyer and Deacon2016; Waller et al., Reference Waller, D’Souza Walsh and Wright2016).
Attempts to target therapist attitudes about exposure during training have included both explicit and implicit techniques. Explicit strategies consist of providing therapists with empirical evidence to recalibrate their perceptions of the likelihood and severity of feared patient outcomes, as well as expert testimonials on the safety and tolerability of exposure (Farrell et al., Reference Farrell, Deacon, Kemp, Dixon and Sy2013). Explicit means are capable of reducing negative beliefs during training, but do not fully address therapists’ concerns about the process of delivering exposures (Farrell et al., Reference Farrell, Kemp, Blakey, Meyer and Deacon2016). Implicit techniques have included simulated self-exposures to provide therapists with insight into what their patients might experience during exposure (Farrell et al., Reference Farrell, Kemp, Blakey, Meyer and Deacon2016). Simulated exposure facilitates parallel processing during training and may allow therapists to implicitly test their assumptions about the safety and tolerability of exposure for their patients. Parallel processing refers to: (1) therapists undergoing the same procedural experience as clients and (2) therapists experiencing a reduction in their anxiety about using exposure in the same way that clients typically experience a reduction in anxiety following exposure. Including simulated exposures in training is attributed to greater negative belief reduction, above and beyond explicit didactic approaches (Farrell et al., Reference Farrell, Kemp, Blakey, Meyer and Deacon2016). Thus, the inclusion of experiential training tasks, such as simulated exposure, may be an effective strategy for reducing therapists’ concerns about exposure and consequently increasing therapists’ success implementing exposure following training.
This study evaluated the experiences of therapists who recently completed an experientially focused training (Frank et al., Reference Frank, Becker-Haimes, Rifkin, Norris, Ollendick, Olino, Kratz, Beidas and Kendall2020), which used exposure techniques to enhance therapist training. We sought to understand beliefs about exposure and experiential training, as well as barriers and facilitators of exposure delivery. Specifically, qualitative interviews were used to examine therapists’ perceptions of experiential training (Aim 1), including how experiential training affected beliefs about exposure. A secondary aim (Aim 2) was to assess determinants of exposure use following experiential training and to consider how these determinants compared with prior research. Mixed methods analyses examined how responses about determinants varied by practice setting (i.e. private practice (PP) versus CMH) and exposure use. A mixed methods approach is ideally suited to examine the complex interactions between organizational, therapist, and patient factors that influence exposure implementation.
Method
Participants
Therapist participants (N=12) were mental health therapists practising in the northeastern United States who received training in exposure (Frank et al., Reference Frank, Becker-Haimes, Rifkin, Norris, Ollendick, Olino, Kratz, Beidas and Kendall2020). Inclusion criteria were: (1) having an advanced degree in a mental health field; (2) working in a clinical setting; (3) treating at least one client who would benefit from exposure; and (4) ability to read and speak English. Participants who had previously attended a prior full-day workshop on exposure were not eligible. Participants included therapists who were randomized to the experiential training condition in a pilot study examining the feasibility and acceptability of this training approach (Frank et al., Reference Frank, Becker-Haimes, Rifkin, Norris, Ollendick, Olino, Kratz, Beidas and Kendall2020). The experiential training required therapists themselves to complete exposures to spiders after attending lecture-style teaching about exposure therapy. Participants completed a modified version of a one-session phobia treatment (Kashdan et al., Reference Kashdan, Adams, Read and Hawk2012; Ollendick et al., Reference Ollendick, Öst, Reuterskiöld, Costa, Cederlund, Sirbu, Davis and Jarrett2009), which allowed them to complete an entire exposure protocol over the course of an afternoon. Specifically, participants were partnered with another therapist who exhibited a similar level of fear of spiders (based on a quantitative measure). They were instructed to complete four phases of ‘treatment’ with their partner, including psychoeducation/rationale, assessment/hierarchy building, implementing exposures, and homework/relapse prevention.
Procedures
This study was approved by the Temple University IRB; ClinicalTrials.gov Identifier: NCT03354975.
Qualitative interviews
After completion of all other study procedures (i.e. training, consultation calls, and quantitative questionnaires), participants who received experiential training were contacted by email to ask if they would be willing to complete qualitative interviews. Data collection was ongoing until data saturation (i.e. new data are redundant; Saunders et al., Reference Saunders, Sim, Kingstone, Baker, Waterfield, Bartlam, Burroughs and Jinks2018) was reached. One participant declined and did not specify a reason; all other participants who were contacted agreed to participate, yielding a final sample of 12 participants. A semi-structured qualitative interview guide (see Appendix in Supplementary material) included questions about therapists’ perceptions of experiential training and exposure. Participants were also asked about factors that affect their use of exposures. Participants were interviewed once individually for 30–60 minutes. Interviews were conducted and audio recorded via Webex, a video conferencing platform. They were transcribed by undergraduate research assistants and spot-checked by the first author. Interviews were conducted, coded, and analysed by two female doctoral students with advanced training in exposure (L.S.R. and H.E.F.) who were also involved in therapist training and consultation. L.S.R. and H.E.F. attended a three-day intensive workshop on qualitative methods prior to this study. Participants received $20 for completing qualitative interviews.
Quantitative questionnaires
Measures were administered before training, after training, and at three monthly follow-ups. Participants received links via email to complete follow-up questionnaires online.
Demographics and background questionnaire
The demographics questionnaire assessed participants’ age, gender, race, and education. It also assessed topics related to participants’ work setting, theoretical orientation, and level of familiarity with exposure.
Exposure Therapy Clinical Use Survey (Harned et al., Reference Harned, Dimeff, Woodcock, Kelly, Zavertnik, Contreras and Danner2014)
This survey measured therapist-reported use of exposure over the past month. Frequency of exposure use was assessed by the sum of in vivo, imaginal, and interoceptive exposures used in the past month. For mixed methods analyses, participants were classified as having either used exposures some or none at 1-month follow-up.
Qualitative and mixed method analyses
Qualitative analyses followed the consolidated criteria for reporting qualitative research (COREQ) (Tong et al., Reference Tong, Sainsbury and Craig2007) to ensure methodological rigor.
Analyses were conducted in NVivo using an integrated approach (Bradley et al., Reference Bradley, Curry and Devers2007), which included a priori codes specific to the CFIR (i.e. a deductive approach), while allowing for additional codes to emerge from the data (i.e. an inductive approach). A priori CFIR codes included intervention characteristics, inner setting, outer setting, characteristics of individuals involved (i.e. therapists), and implementation process. Two advanced doctoral students (L.S.R. and H.E.F.) collaboratively reviewed three transcripts to develop initial definitions for each a priori code and to identify and define potential inductive codes. Through discussion, coders agreed on two inductive codes that were not fully captured by the deductive (a priori) codes. Coders then independently applied all codes to three transcripts to determine inter-rater reliability (kappa=0.79). Disagreements were resolved through discussion informed by memos and examples, which informed the creation of a revised codebook. Then, both coders independently coded all transcripts using the codebook. Final codes were determined through discussion and consensus (kappa=0.78; ‘substantial’ agreement; DeSantis and Ugarriza, Reference DeSantis and Ugarriza2000; Hill et al., Reference Hill, Knox, Thompson, Williams, Hess and Ladany2005; Viera and Garrett, Reference Viera and Garrett2005).
Responses for each code were exported into separate Excel files and reviewed by the first author (H.E.F.) and a bachelor’s-level research assistant (K.S.) who was not directly involved in the training. Mixed methods analyses were conducted to identify how themes differed by quantitative variables. The structure of the mixed methods analyses was sequential, with quantitative data gathered prior to qualitative data. The function of the analysis was complementarity (i.e. using qualitative data to elaborate on quantitative findings), and the process was connecting (i.e. using qualitative data to build on quantitative data; Creswell et al., Reference Creswell, Klassen, Plano Clark and Smith2011; Palinkas et al., Reference Palinkas, Aarons, Horwitz, Chamberlain, Hurlburt and Landsverk2011). Analyses focused on identifying how perceptions of training and exposure varied by practice setting and exposure use at 1-month follow-up. Mixed methods analyses were conducted by dividing each qualitative code into subgroups by quantitative codes. H.E.F. and K.S. collaboratively created brief written summaries for each subgroup and identified differences between responses by practice setting and exposure use.
Results
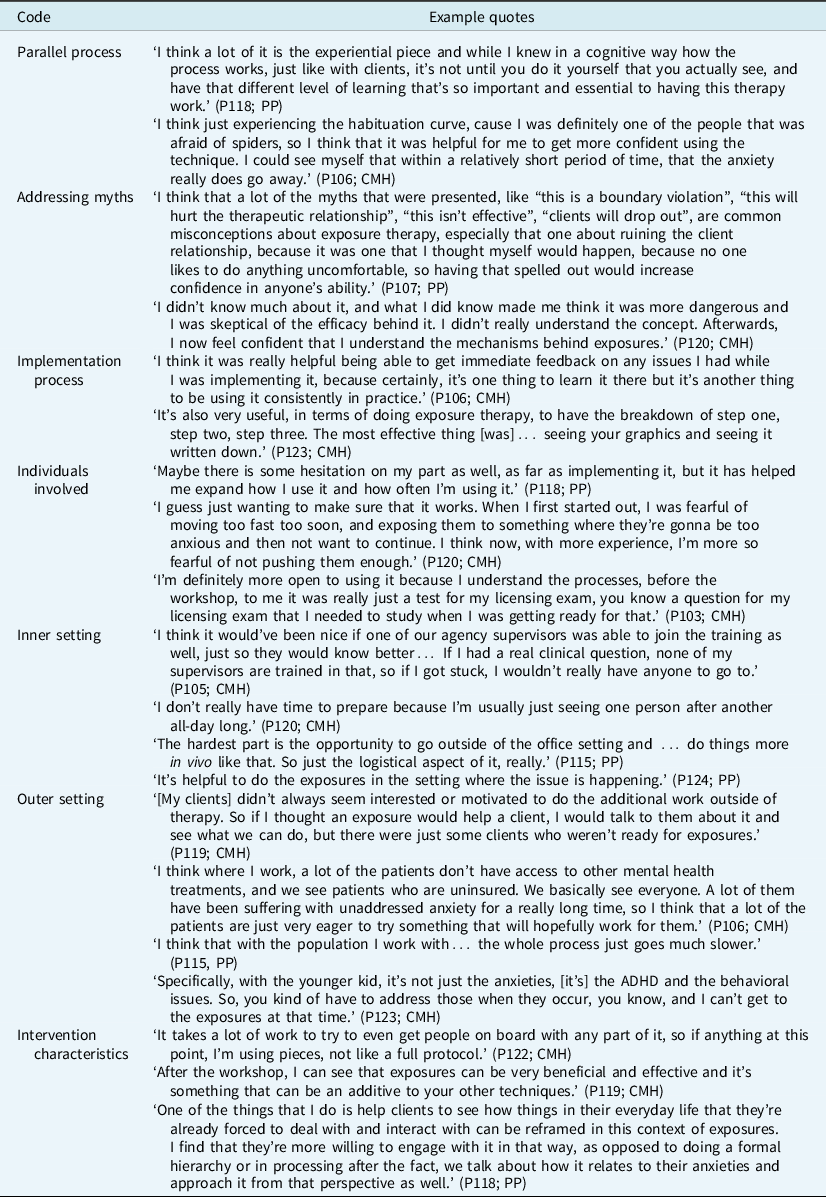
Participant demographics are shown in Table 1. Representative quotes for each of the qualitative codes are presented in Table 2.
Table 1. Characteristics of study participants (n=12)
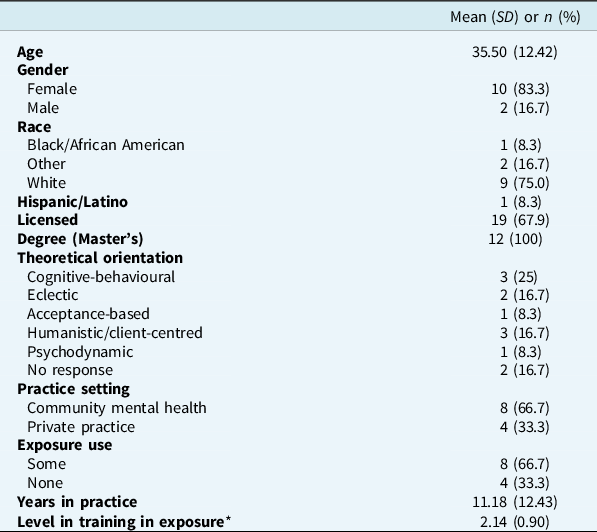
* Measured with a 1–5 point Likert scale, with 1 being no training and 5 being extensive training.
Table 2. Qualitative interview codes and quotes
Aim 1: Perceptions of experiential training
The first aim of this study was to assess therapists’ perceptions of experiential training, including its impact on beliefs about exposure. In addition to the a priori code, implementation process, we identified two inductive codes related to this theme, including how the training functioned as a parallel process for therapists and addressed myths about exposure.
Parallel process
Parallel process was a code that arose out of several therapists’ descriptions of how their experience interacting with spiders during the training was consistent with what a client experiences during exposures, including a reduction in anxiety. Many described this process as being helpful to ‘gain empathy for clients’ (P118) and to address their negative beliefs about exposures. Participants also noted that doing exposures ‘changed [their] initial thoughts and perceptions [about exposure]’ (P120) especially if they experienced anxiety themselves during the exposure practice. In addition, the experiential practice helped therapists better understand the logistical aspects of exposures and feel more confident using exposures with clients.
Addressing myths
Addressing myths was a code that included descriptions of how the training addressed misconceptions that participants had about exposures prior to the training. Several participants reported that they had negative associations with exposure prior to the training (e.g. thinking it was ‘unethical’ (P105)). However, these beliefs were dispelled in the training by talking about the myths directly and learning how exposure works (e.g. ‘It addressed my fears of being seen as the mean and horrible therapist’ (P103)). Overall, many reported that addressing these myths improved their attitudes towards exposure and their willingness to use exposures with clients.
Implementation process
Implementation process was a CFIR-informed code referring to the process of learning about and applying the intervention in clinical practice. Participants said that they felt capable of addressing clients’ concerns and explaining the rationale and procedures of exposure after training. Participants noted being ‘floored with how quickly [patients] progressed with exposure therapy’ (P106). However, some therapists reported that they did not have enough knowledge and confidence to proceed with exposures after one day of training. One person described that ‘none of my supervisors are trained in [exposure], so if I got stuck, I wouldn’t really have anyone to go to’ (P105). Participants described the group consultation calls as being useful and serving as a back-up to the training that addressed week-to-week difficulties with using exposure.
Aim 2: Determinants of exposure use following training
This aim focused on understanding therapists’ experiences implementing exposure following experiential training, including barriers and facilitators across the CFIR dimensions.
Characteristics of individuals involved
This CFIR-informed code refers to therapists who attended the training and their knowledge, beliefs, and attitudes about exposure. Many participants reported that they attended the workshop because they were interested in learning new therapeutic strategies. Following the training, several participants described feeling excited and motivated to implement exposure with their clients. Many reported a shift in attitudes about exposures after the workshop, including feeling more positive and/or more informed about exposures. Exposure was described as more broadly applicable than they initially realized; some therapists were left with new ideas of how to use it with their clients. Some people had positive associations with exposure prior to the workshop but never really used it (e.g. it was ‘glossed over’ (P105) in their training). Others were resistant to exposure and had perceptions that it could be damaging to their clients prior to training. One participant said, ‘It was something that I thought, “oh these are the type of therapists that will take you into an elevator even if you don’t want to”, and that was my first impression. I never thought that I myself would use exposures with my clients, and after the training, I got a little more comfortable using exposures’ (P119). Participants who had previous negative associations reported that understanding the theory behind exposure helped them feel more confident and comfortable using it.
Differences by setting
Therapists in PP more explicitly noted how the training improved their confidence in using exposures, whereas CMH therapists described continuing to feel anxious about exposure. CMH therapists specifically discussed experiencing a change toward more positive in beliefs about exposure following the training.
Differences by exposure use
Therapists who did not use exposures identified several reasons for this, including therapist anxiety and client symptoms that would benefit from exposures primarily outside of the office. Related to this, participants who did not use exposures described being open to the idea of using exposures but expressed hesitancy about doing so in practice. They described concerns that for many clients, it was not the right technique or that it could result in damage or harm (e.g. liability, client terminating therapy).
Inner setting
This CFIR-informed code refers to wherever the therapist works and how it relates to implementation of exposures. A commonly stated barrier to implementation was that participants’ supervisors or co-workers did not have training in exposure. Another barrier was short appointment times – one participant said, ‘I’d love to do it with some of my clients, but I can’t… We generally don’t spend… longer than 20–30 minutes with a client’ (P110). Similarly, infrequent sessions were described as a barrier to implementing exposures consistently. Some participants mentioned that their patients’ priorities may not be conducive to using exposure during these infrequent, short sessions, where time is spent addressing more pressing issues than anxiety. Participants described that ‘within an agency setting where you have a high case load and don’t really have time to prepare worksheets’ (P118), it can be challenging to implement exposure. In addition, people reported that there were ‘rules about staying within the confines of the building’ (P119) that limited the scope of exposures that could be completed. Some participants noted that attending the consultation calls was difficult because they could not get time off during the work week to attend the calls. Facilitators related to inner setting included having supervisors who knew about exposures and provided support for implementing them.
Differences by setting
Participants who worked in CMH settings mentioned that aspects of their organization made it more difficult to use exposure. They more often endorsed that having infrequent appointments, high caseloads, and complex clinical presentations made it difficult to prepare for and prioritize exposures. CMH therapists also often mentioned difficulties related to office constraints, such as not being able to leave the office or offer rewards. PP therapists had more mixed responses about office constraints, with some having more flexibility (e.g. being able to go to clients’ homes).
Differences by exposure use
Participants who used exposure mentioned that it would be helpful for their co-workers and supervisors to receive training, but that their workplaces were open to using new interventions such as exposure. They also described overcoming the barrier of short sessions by using components of exposure (e.g. planning for exposures). Those who did not use exposure reported a lack of co-workers who were knowledgeable about exposure.
Outer setting
This CFIR-informed code refers to characteristics of the larger context in which treatment is being implemented, as well as factors related to the population receiving treatment. Factors that were identified as improving patient engagement in exposures included consistency with session attendance, homework completion, and extent of caregiver involvement in treatment (for youth). Participants identified concerns that ‘there are just some clients who aren’t ready for exposures’ (P119). Others noted that the process of engaging clients in exposure is slow and gradual, which is sometimes a barrier. Practical challenges for families, such as financial barriers to accessing treatment, were also noted. Another common theme was the presence of comorbid conditions that may interfere with the use of exposures, such as ADHD (‘it would be really great for him to do exposure therapy, except he has limited self-awareness and no attention span’ (P123)), autism (causing a lack of social motivation), trauma (‘so many [clients] have such significant trauma underlying their issues’ (P124)), and complex cases with multiple diagnoses. Some participants mentioned that, after training, they had an increased willingness to provide referrals to an exposure therapist if they believed that their clients would benefit from seeing a specialist.
Differences by setting
CMH therapists noted that anxiety is not always at the top of the hierarchy of needs for patients, and that other basic needs (e.g. food, housing) may need to be addressed first. CMH therapists discussed how specific client characteristics (e.g. comorbid diagnoses) made it more difficult to use exposures. CMH therapists also expressed that some patients were excited about a new type of treatment like exposure, while others were resistant to the idea of introducing a new intervention. PP therapists noted that progress with exposures was slower than they expected.
Differences by exposure use
Therapists who used exposure talked about using exposure components (e.g. psychoeducation) flexibly but facing competing issues and concerns such as poor attendance when trying to implement exposures in session. They also noted that it is especially challenging and time consuming to do exposures with clients who have comorbid diagnoses. However, therapists who used exposure were able to overcome client barriers by flexibly implementing exposures. Those who did not use exposure described having more clients for whom exposure may not be a priority due to case management issues or lack of treatment compliance. They also described more diagnostic complexity within their cases and difficulty identifying appropriate clients for exposure given the lack of clear anxiety diagnoses.
Intervention characteristics
This CFIR-informed code included perceptions of the intervention itself. Some participants reported liking that exposure is ‘pretty clear-cut and structured’ (P115), while others described being ‘more flexible with implementing it’ (P118). Participants reported liking that the exposure process can be broken into small steps and is intuitive once the rationale is understood. Several people reported using the psychoeducation component of exposure (i.e., describing the importance of approach rather than avoidance behaviors) and connecting it to the client’s life. However, others stated that buy-in for exposures can be hard. Some described only using parts of the intervention, such as identifying core fears, the cycle of avoidance, and the fear hierarchy, but not being able to use exposures consistently in session.
Differences by setting
Therapists in both settings noted the benefits of exposure being a flexible intervention, but CMH therapists noted the importance of this flexibility to allow them to address time constraints and use adjunctive interventions. PP therapists noted that the flexibility of exposure is useful to address multiple presenting problems. CMH therapists more often discussed using parts of exposure rather than all aspects of it. They noted that the psychoeducation part of exposure often resonates with clients.
Differences by exposure use
Therapists who used exposure provided more detail about exactly how they used the intervention flexibly. For example, they talked about an emphasis on assessment (e.g. building fear hierarchies). They also described completing informal or ‘smaller scale mini-exposures’ (P107) based on current treatment goals or life stressors. Those who did not use exposures also mentioned that exposures were used flexibly, but they stated that exposures take a lot of time, which limits their ability to complete them in session.
Discussion
The present study identified how experiential training influenced therapists’ attitudes towards and use of exposure. Furthermore, results highlight the multi-level contextual factors that influence exposure implementation, and how these factors varied by clinical setting and exposure use. Although participants reported improved attitudes towards exposure following experiential training, as well as generally positive experiences during training, structural barriers persisted in limiting the delivery of exposure in many cases. Furthermore, participants’ readiness to use exposure following training varied. This provides support for the potential benefits of experiential training for improving therapist attitudes towards exposure while also highlighting the need to consider broader contextual factors that influence implementation. Differences in perceptions of exposure by clinical setting and self-reported exposure use indicate future directions for research focused on improving implementation and sustained use of exposure.
Results from this study expand on the emerging research identifying organizational determinants of exposure. Although organizational culture and climate are well-documented as influencing EBI implementation broadly (Proctor et al., Reference Proctor, Landsverk, Aarons, Chambers, Glisson and Mittman2009), few studies have specifically examined the role of organizational factors in exposure implementation for anxiety disorders (Becker-Haimes et al., Reference Becker-Haimes, Byeon, Frank, Williams, Kratz and Beidas2020; Frank et al., Reference Frank, Milgram, Freeman and Benito2022; Milgram et al., Reference Milgram, Freeman, Benito, Elwy and Frank2022). In the present study, comparisons between therapists in CMH and PP settings indicated that organizational factors were much more commonly identified as contributing to difficulty implementing exposure by CMH therapists. Such challenges persisted even among therapists who had positive attitudes towards exposure following experiential training. These results are consistent with prior research indicating that therapists in CMH and PP settings have less organizational support for exposure than therapists in anxiety specialty clinics (Becker-Haimes et al., Reference Becker-Haimes, Byeon, Frank, Williams, Kratz and Beidas2020; Frank et al., Reference Frank, Milgram, Freeman and Benito2022). This may be particularly pronounced among CMH therapists, who reported not having co-workers or supervisors who were trained in or able to assist with exposures. Previous research (Ringle et al., Reference Ringle, Read, Edmunds, Brodman, Kendall, Barg and Beidas2015; Wolitzky-Taylor et al., Reference Wolitzky-Taylor, Fenwick, Lengnick-Hall, Grossman, Bearman, Arch, Miranda and Chung2018) has highlighted that lack of supervisors trained in CBT is a barrier to exposure use in CMH settings. Results suggest that even weekly group-based expert consultation was not sufficient to meet therapists’ needs, and that there was a desire for clinic-based supervision to support exposure implementation. This underscores the importance of identifying sustainable approaches to consultation/supervision that both provide an adequate dose and meet therapists’ preferences to receive support within their organization.
CMH therapists also indicated other inner setting barriers to exposure use that persisted following experiential training, such as short appointment times and full caseloads. The high burden of seeing many patients over a short period of time in CMH settings may make it difficult to implement new interventions; this is likely to be especially true for an intervention like exposure that may require advance planning and elicit distress from a patient. Short appointments decrease the time a therapist can wait for a client’s distress to come back down as they adjust to an exposure. This may lead to multiple consequences, including increased therapist anxiety about sending a patient home feeling distressed, as well as limited opportunities for patients to learn that they can sit with and tolerate that distress. This is especially notable as therapists’ hesitancy to elicit distress is a known barrier to exposure implementation (Deacon et al., Reference Deacon, Farrell, Kemp, Dixon, Sy, Zhang and McGrath2013a; Deacon et al., Reference Deacon, Lickel, Farrell, Kemp and Hipol2013c). Although experiential training may address clinician hesitancy, other challenges such as being unable to leave the office for exposures and working with patients with multiple needs can further contribute to limited exposure delivery. To address these barriers, training should focus on how to use exposure flexibly in the contexts in which therapists work (i.e. where leaving the office is not feasible or appointment times are brief). Guidance should be given throughout training on how to deliver treatment flexibility while also maintaining fidelity to treatment (Kendall and Frank, Reference Kendall and Frank2018). Efforts to improve therapist self-efficacy in the flexible delivery of exposure may require use of innovative strategies such as on-demand consultation with experts (Stewart et al., Reference Stewart, Williams, Byeon, Buttenheim, Sridharan, Zentgraf, Jones, Hoskins, Candon and Beidas2019) or implementing stepped care models of delivery (Bower and Gilbody, Reference Bower and Gilbody2005), where additional consultation is available for therapists who need it. Strategies such as learning collaboratives or peer-to-peer consultation that include members across an organization (or across multiple PPs) to address barriers collaboratively may also be effective to address organizational-level barriers (Hanson et al., Reference Hanson, Saunders, Ralston, Moreland, Peer and Fitzgerald2019).
When participants reflected on the useful components of the training they received, they highlighted that, as suggested by Farrell and colleagues (Reference Farrell, Kemp, Blakey, Meyer and Deacon2016), directly addressing myths and negative beliefs about exposure was beneficial. The experiential training explicitly identified and debunked myths about exposure, while also incorporating an implicit training approach in which therapists underwent exposures themselves. Using explicit and implicit techniques in tandem may be especially likely to change therapists’ attitudes towards exposure. This is consistent with research on the self-practice/self-reflection (SP/SR) training technique, which also harnesses an experiential approach for clinician training in CBT and likely operates on an implicit process that extends beyond traditional (explicit) CBT training (Bennett-Levy and Lee, Reference Bennett-Levy and Lee2014). The SP/SR approach has demonstrated evidence for increasing clinician confidence in delivering CBT, which researchers have suggested is due to participants’ deeper understanding of theory and techniques through experiential personal practice (Scott et al., Reference Scott, Yap, Bunch, Haarhoff, Perry and Bennett-Levy2021). Both SP/SR and experiential training highlight the value of therapists’ personal engagement with therapeutic processes to extend learning of CBT skills.
Also similar to SP/SR, therapists who received experiential training identified that the parallel process of experiencing what a client experiences during exposure was one of the most effective aspects of training. Future work should continue to examine the effectiveness of this approach on changing therapist behaviour. Furthermore, there is a need to identify the mechanisms of change that were engaged with experiential training. One potential mechanism is that therapists may experience exposure as less scary than they originally thought and find that the outcomes they feared did not come to fruition. In this case, the mechanism of action engaged by training may be reducing therapist anxiety. Another possible mechanism is that being the recipient of exposure makes therapists more comfortable using and explaining it. In this case, a function of engaging in exposures during training may be to increase self-efficacy. In addition to testing these distinctions empirically, this also highlights other potential applications of using exposure as a training tool. For instance, if addressing therapist anxiety is a primary mechanism, experiential training should be studied with other interventions that evoke therapist distress, such as suicide risk assessments (Becker-Haimes et al., Reference Becker-Haimes, Klein, Frank, Oquendo, Jager-Hyman, Brown and Barnettsubmitted). Such extensions of this work will require consideration of ethical and legal concerns. Interestingly, although ethical concerns about exposure are quite common (e.g. competence, confidentiality; Gola et al., Reference Gola, Beidas, Antinoro-Burke, Kratz and Fingerhut2015), no participants identified such concerns during experiential training. However, future applications of experiential training may surface ethical concerns when exposure is used more broadly with therapists. Thus, careful consideration must be given to ethical issues during training, such as the informed consent process, privacy when therapists disclose feared topics, and the availability of therapy referrals if clinically significant symptoms arise during training.
Overall, participants reported that training was effective in altering attitudes, improving confidence, and increasing motivation to use exposure. However, there were still participants who did not use exposure. Results point to several potentially contributing factors to the non-use of exposure following training. As noted above, inner setting factors are known to predict implementation success. Those who did not use exposure reported being unable to rely on colleagues or supervisors for feedback on using exposure. Although attitudes towards exposure were more positive following training, it is likely that therapist anxiety combined with limited support at work had an additive effect of decreasing the likelihood of implementing exposure. This is consistent with prior work suggesting the need for ‘synergy between organizational and therapist constructs’ to predict therapist outcomes (Becker-Haimes et al., Reference Becker-Haimes, Williams, Okamura and Beidas2019), and the inclusion of multiple levels of determinants in most implementation science frameworks (e.g. CFIR; Damschroder et al., Reference Damschroder, Aron, Keith, Kirsh, Alexander and Lowery2009).
Limitations
Limitations include the fact that participants were a small sample of therapists from one geographical region, reducing variability in outer contextual factors. In addition, qualitative interviews were only conducted with participants in one condition of the study, meaning that we could not compare responses across conditions. Limited quantitative data were collected on inner context factors, such as organizational culture and implementation climate, which may influence attitudes toward exposure (Woodard et al., Reference Woodard, Triplett, Frank, Harrison, Robinson and Dorsey2021) and exposure use (Becker-Haimes et al., Reference Becker-Haimes, Byeon, Frank, Williams, Kratz and Beidas2020). Another limitation is the use of therapist self-report measures of exposure use, which may be inflated relative to observer ratings (Nakamura et al., Reference Nakamura, Selbo-Bruns, Okamura, Chang, Slavin and Shimabukuro2014). Finally, although participants were encouraged to provide honest responses during qualitative interviews, social desirability bias may have led them to provide more positive responses, especially when being interviewed by the study’s principal investigator.
Conclusion
Overall, this study demonstrates that experiential learning is an acceptable approach for training therapists to use exposure, and that it improves perceptions of and intentions to use exposure. However, this may not always lead directly to increased exposure use. Causal theories, such as the theory of planned behavior (Ajzen and Driver, Reference Ajzen and Driver1991; Fishman et al., Reference Fishman, Beidas, Reisinger and Mandell2018; Fishman et al., Reference Fishman, Lushin and Mandell2020), posit that intentions predict behaviour when one is able to act. Thus, there is a need to specifically consider contextual determinants, such as inner setting characteristics, that moderate the relationship between intentions and behavior (Frank et al., Reference Frank, Last, Alrabiah, Fishman, Rudd, Kratz, Harker, Fernandez-Marcote, Jackson, Comeau, Shoyinka and Beidas2021). In summary, experiential training may be an especially effective implementation strategy when combined with strategies that also address inner setting barriers.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1352465822000728
Data availability statement
The dataset generated and analysed during the current study is not publicly available due to the sensitive nature of interview transcript data. Publication of entire transcripts risks identifying research participants.
Acknowledgements
We are grateful to the many people who contributed to this project, including the graduate students who assisted with training and consultation, the research assistants who provided data entry and transcript support, our community advisory board members, the grant consultants and dissertation committee members who supported this project, and the therapists who participated in this study.
Author contributions
Hannah Frank: Conceptualization (lead), Data curation (lead), Formal analysis (lead), Funding acquisition (lead), Investigation (lead), Methodology (lead), Project administration (lead), Supervision (equal), Writing – original draft (lead), Writing – review & editing (lead); Lara Rifkin: Data curation (supporting), Formal analysis (supporting), Writing – review & editing (supporting); Kate Sheehan: Formal analysis (supporting), Writing – original draft (supporting), Writing – review & editing (supporting); Emily Becker-Haimes: Conceptualization (supporting), Methodology (supporting), Writing – review & editing (supporting); Margaret Crane: Data curation (supporting), Writing – review & editing (supporting); Katherine Phillips: Data curation (supporting), Writing – review & editing (supporting); Sophie Palitz: Data curation (supporting), Writing – review & editing (supporting); Joshua Kemp: Conceptualization (supporting), Writing – original draft (supporting), Writing – review & editing (supporting); Kristen Benito: Writing – review & editing (supporting); Philip Kendall: Conceptualization (supporting), Funding acquisition (supporting), Investigation (supporting), Methodology (supporting), Resources (lead), Supervision (equal), Writing – review & editing (supporting).
Financial support
This work was supported by the National Institutes of Health (F31MH112211; T32MH019927; F31MH124346). The funding source did not have any direct involvement in the study design, data collection, analysis, or writing of this report.
Conflicts of interest
Dr Kendall receives author royalties from the sales of treatment materials (Guilford, Oxford University Press and Workbook Publishing); his spouse has a financial interest in and is affiliated with Workbook Publishing. No other authors report any conflicts of interests.
Ethical standards
This study was approved by the Temple University IRB (Protocol 2448) and conformed to the Declaration of Helsinki. All participants completed informed consent procedures prior to participating in this study.





Comments
No Comments have been published for this article.